2015 National Training Program Module 10 Medicare and Medicaid
48 Slides2.37 MB
2015 National Training Program Module 10 Medicare and Medicaid Fraud and Abuse Prevention
Session Objectives This session should help you Define fraud and abuse Identify causes of improper payments Discuss how CMS fights fraud and abuse Explain how you can fight fraud and abuse Recognize sources of additional information October 2015 Medicare and Medicaid Fraud and Abuse Prevention 2
Lesson 1—Fraud and Abuse Overview Definition of fraud and abuse Protecting the Medicare Trust Funds and other public resources Examples of Medicare and Medicaid fraud Who commits fraud? Causes of improper payments Quality of care concerns October 2015 Medicare and Medicaid Fraud and Abuse Prevention 3
Definition of Fraud and Abuse Fraud When someone intentionally executes or attempts to execute a scheme to obtain money or property of any health care benefit program Abuse When health care providers or suppliers perform actions that directly or indirectly result in unnecessary costs to any health care benefit program The primary difference between fraud and abuse is intention. October 2015 Medicare and Medicaid Fraud and Abuse Prevention 4
Protecting Taxpayer Dollars CMS must Protect Medicare Trust Funds Medicare Hospital Insurance (Part A) Trust Fund Supplementary Medical Insurance (Part B) Trust Fund Protect the public resources that fund the Medicaid programs Manage the careful balance between Paying claims quickly and limiting burden on the provider community with conducting reviews that prevent and detect fraud October 2015 Medicare and Medicaid Fraud and Abuse Prevention 5
Examples of Fraud Medicare or Medicaid is billed for Services you never received Equipment you never got or was returned Documents are altered to gain a higher payment Misrepresentation of dates, descriptions of furnished services, or the identity of the beneficiary Someone uses your Medicare or Medicaid card with or without your permission A company uses false information to mislead you into joining a Medicare plan For recent examples of fraud by region visit, medic-outreach.rainmakerssolutions.com/fraud-in-the-news/ . October 2015 Medicare and Medicaid Fraud and Abuse Prevention 6
Consequences of Sharing a Medicaid Card or Number Medicaid-specific lock-in program Limits you to certain doctors/drug stores/hospitals For activities like ER visits for non-emergency care and using multiple doctors that duplicate treatment/medication Your medical records could be wrong You may have to pay money back or be fined You could be arrested You might lose your Medicaid benefits October 2015 Medicare and Medicaid Fraud and Abuse Prevention 7
Who Commits Fraud? Most individuals and organizations that work with Medicare and Medicaid are honest However, anyone can commit fraud Doctors and health care practitioners Suppliers of durable medical equipment Employees of doctors or suppliers Employees of companies that manage Medicare billing People with Medicare and Medicaid October 2015 Medicare and Medicaid Fraud and Abuse Prevention 8
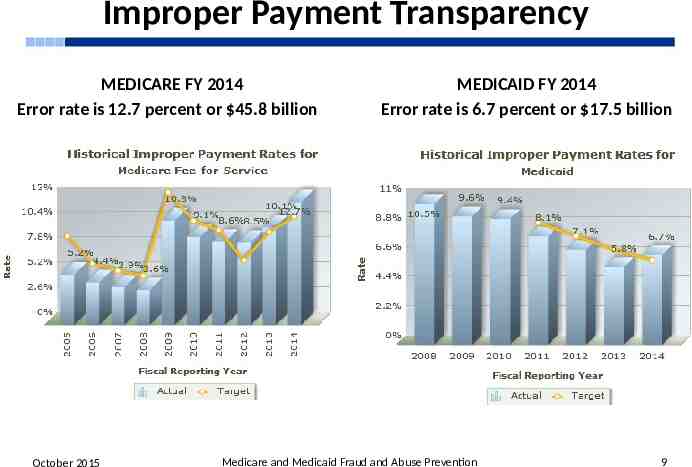
Improper Payment Transparency MEDICARE FY 2014 Error rate is 12.7 percent or 45.8 billion October 2015 MEDICAID FY 2014 Error rate is 6.7 percent or 17.5 billion Medicare and Medicaid Fraud and Abuse Prevention 9
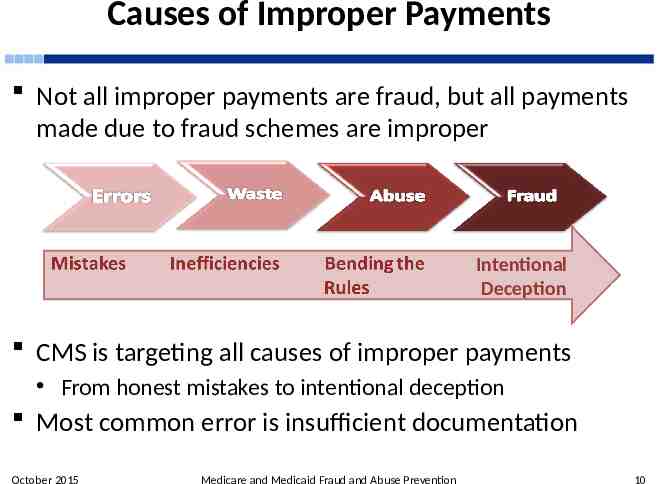
Causes of Improper Payments Not all improper payments are fraud, but all payments made due to fraud schemes are improper Intentional Deception CMS is targeting all causes of improper payments From honest mistakes to intentional deception Most common error is insufficient documentation October 2015 Medicare and Medicaid Fraud and Abuse Prevention 10
Preventing Fraud in Medicare Parts C and D Plan agents and brokers must follow CMS’s Marketing Guidelines. Examples of what plans can’t do include Send you unwanted emails Come to your home uninvited to get you to join Call you unless you're already a member Offer you cash to join their plan Give you free meals while trying to sell you a plan Talk to you about their plan in areas where you get health care If you think a Medicare plan broke the rules Call 1-800-MEDICARE (1-800-633-4227) TTY users should call 1-877-486-2048 October 2015 Medicare and Medicaid Fraud and Abuse Prevention 11
Telemarketing and Fraud— Durable Medical Equipment (DME) DME telemarketing rules DME suppliers can’t make unsolicited sales calls Potential DME scams Calls or visits from people saying they represent Medicare Telephone or door-to-door selling techniques Equipment or service is offered free and you’re then asked for your Medicare number for “record keeping purposes” You’re told that Medicare will pay for the item or service if you provide your Medicare number October 2015 Medicare and Medicaid Fraud and Abuse Prevention 12
Quality of Care Concerns Patient quality of care concerns aren’t necessarily fraud Medication errors Change in condition not treated Discharged from the hospital too soon Incomplete discharge instructions and/or arrangements Contact your Beneficiary and Family-Centered Care Quality Improvement Organization Visit Medicare.gov/contacts and click on Find Helpful Contacts Call 1-800-MEDICARE (1-800-633-4227) TTY users should call 1-877-486-2048 October 2015 Medicare and Medicaid Fraud and Abuse Prevention 13
Check Your Knowledge—Question 1 Those who commit Medicare fraud can include a. People with Medicare b. Suppliers of durable medical equipment c. Doctors and health care practitioners d. All of the above October 2015 Medicare and Medicaid Fraud and Abuse Prevention 14
Check Your Knowledge—Question 2 It’s considered fraud if someone else uses your Medicare card with your permission a. True b. False October 2015 Medicare and Medicaid Fraud and Abuse Prevention 15
Lesson 2—CMS Fraud and Abuse Strategies The Center for Program Integrity CMS Program Integrity Contractors CMS Administrative Actions Law Enforcement Actions The Health Care Fraud Prevention Partnership Health Care Fraud Prevention and Enforcement Action (HEAT) Team The Fraud Prevention Toolkit at CMS.gov/Medicare-Medicaid-Coordination/Fraud-Preven tion/Medicaid-Integrity-Education/fwa.html Provider and Beneficiary Education Medicare and Medicaid Fraud and Abuse Prevention October 2015 16
CMS Center for Program Integrity Consolidates CMS anti-fraud components Authorities from the Affordable Care Act More rigorous screenings for health care providers Reciprocal termination of providers from Medicare, Medicaid, and the Children’s Health Insurance Program May temporarily stop enrollment in high-risk areas Used first in July 2013 and extended into 2015 Temporarily stop payments in cases of suspected fraud October 2015 Medicare and Medicaid Fraud and Abuse Prevention 17
CMS Program Integrity Contractors A nationally coordinated Medicare/Medicaid program integrity strategy that cuts across regions Zone Program Integrity Contractors (ZPIC) National Benefit Integrity Medicare Drug Integrity Contractor (NBI MEDIC) Recovery Audit Program Outreach & Education MEDIC (O&E MEDIC) Medicaid Integrity Contractors October 2015 Medicare and Medicaid Fraud and Abuse Prevention 18
Zone Program Integrity Contractors (ZPICs) Investigate leads generated by the new Fraud Prevention System (FPS) and a variety of other sources Provide feedback to CMS to improve the FPS Perform data analysis to identify and investigate cases of suspected fraud, waste, and abuse Make recommendations to CMS for appropriate administrative actions to protect Medicare Trust Fund dollars Make referrals to law enforcement for potential prosecution Provide support for ongoing law enforcement investigations Identify improper payments to be recovered by Medicare Administrative Contractors October 2015 Medicare and Medicaid Fraud and Abuse Prevention 19

Zone Program Integrity Contractor Map Zone 6 EA-BISC NEBISC and PA-BISC October 2015 Medicare and Medicaid Fraud and Abuse Prevention 20

National Benefit Integrity Medicare Drug Integrity Contractor (NBI MEDIC) Monitors fraud, waste, and abuse in the Part C and Part D programs in all 50 states, the District of Columbia, and U.S. Territories Works with law enforcement and other stakeholders Key responsibilities include Investigate potential fraud, waste, and abuse Receive complaints Resolve beneficiary fraud complaints Perform proactive data analyses Identify program vulnerabilities Refer potential fraud cases to law enforcement agencies The Outreach and Education MEDIC provides tools to combat Part C and Part D fraud, waste and abuse October 2015 Medicare and Medicaid Fraud and Abuse Prevention 21
Recovery Audit Program Recovery Audit Program’s mission Reduce improper Medicare payments by Detecting and collecting overpayments Identifying underpayments Implementing actions to prevent future improper payments Ensure that each Medicare Advantage Plan under Part C and Prescription Drug Plan under Part D has an anti-fraud plan in effect States and territories establish Medicaid Recovery Audit Contractors Identify overpayments and underpayments Coordinate efforts with federal and state auditors October 2015 Medicare and Medicaid Fraud and Abuse Prevention 22
Outreach & Education MEDIC (O&E MEDIC) Created the CMS O&E MEDIC website on behalf of the CMS Center for Program Integrity To help those committed to stopping Parts C/D fraud, waste, and abuse, by providing October 2015 Outreach and education materials Professional education Regulation and guidance Fraud - fighting resources General news Medicare and Medicaid Fraud and Abuse Prevention 23
Medicaid Integrity Contractors (MICs) Support, not replace, state Medicaid program integrity efforts Conduct post-payment audits of Medicaid providers Identify overpayments, and refer to the state for collection of the overpayments Doesn’t adjudicate appeals, but supports state adjudication process Three types of MICs: review, audit, and education October 2015 Medicare and Medicaid Fraud and Abuse Prevention 24
CMS Administrative Actions When CMS suspects fraud, administrative actions include the following: Automatic denials of payment Payment suspensions Prepayment edits Civil monetary penalties Revocation of billing privileges Referral to law enforcement Overpayment determinations October 2015 Medicare and Medicaid Fraud and Abuse Prevention 25
Law Enforcement Actions When law enforcement finds fraudulent activities, enforcement actions include Providers/companies are barred from the programs Providers/companies can’t bill Medicare, Medicaid, or Children’s Health Insurance Plan (CHIP) Providers/companies are fined Arrests and convictions occur Corporate Integrity Agreements may be negotiated October 2015 Medicare and Medicaid Fraud and Abuse Prevention 26
Health Care Fraud Prevention Partnership Includes the federal government, state officials, private health insurance organizations, and other health care anti-fraud groups Shares information and best practices Improves detection Prevents payment of fraudulent health care billings across public and private payers Enables the exchange of data and information among the partners October 2015 Medicare and Medicaid Fraud and Abuse Prevention 27
Health Care Fraud Prevention and Enforcement Action (HEAT) Team Joint initiative between U.S. Department of Health & Human Services and U.S. Department of Justice Improve interagency collaboration on reducing and preventing fraud in federal health care programs Increase coordination, data sharing, and training among investigators, agents, prosecutors, analysts, and policymakers October 2015 Medicare and Medicaid Fraud and Abuse Prevention 28
Medicare Fraud Strike Force Teams Medicare Fraud Strike Force Teams Located in fraud “hot spot” locations Use advanced data analysis to identify high-billing levels in health care fraud hot spots Coordinate national takedowns CMS supports Strike Force takedowns Perform data analysis Suspends payment October 2015 Medicare and Medicaid Fraud and Abuse Prevention 29
Fraud Prevention Toolkit Visit CMS.gov to access the Fraud Prevention Toolkit that includes The 4Rs brochure Fact sheets on preventing and detecting fraud Frequently Asked Questions CMS.gov also has information about the Center for Program Integrity and fraud prevention efforts in Medicare fee-for-service, Parts C and D, and Medicaid October 2015 Medicare and Medicaid Fraud and Abuse Prevention 30
Provider and Beneficiary Education Provider education helps correct vulnerabilities Maintain proper documentation Reduce inappropriate claims submission Protect patient and provider identity information Establish a broader culture of compliance Beneficiary education helps identify and report suspected fraud October 2015 Medicare and Medicaid Fraud and Abuse Prevention 31
Check Your Knowledge―Question 3 a. All of the above When CMS detects fraud, administrative actions may include the following: b. Civil monetary penalties c. Revocation of billing privileges d. Referral to law enforcement October 2015 Medicare and Medicaid Fraud and Abuse Prevention 32
Lesson 3—How You Can Fight Fraud 4Rs for Fighting Medicare Fraud stopmedicarefraud.gov Medicare Summary Notices MyMedicare.gov 1-800-MEDICARE Senior Medicare Patrol Protecting Personal Information and ID Theft Reporting Medicaid Fraud Helpful Resources October 2015 Medicare and Medicaid Fraud and Abuse Prevention 33
4Rs for Fighting Medicare Fraud You’re the first line of defense against Medicare fraud and abuse. Here are some ways you can protect yourself from fraud: 1. Record appointments and services 2. Review services provided Compare services actually received with services on your Medicare Summary Notice 3. Report suspected Fraud 4. Remember to protect personal information, such as your Medicare card and bank account numbers October 2015 Medicare and Medicaid Fraud and Abuse Prevention 34

STOPMedicareFraud.gov Learn about fraud Find resources Report fraud online Access videos See recent Health Care Fraud Prevention and Enforcement Action Team HEAT Task Force results by state October 2015 Medicare and Medicaid Fraud and Abuse Prevention 35
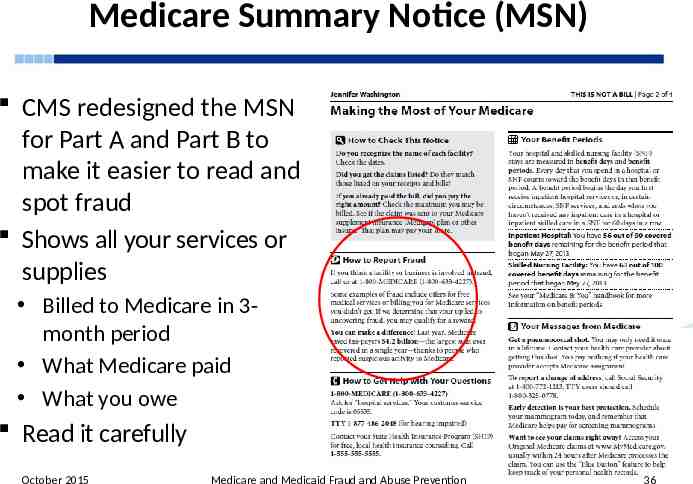
Medicare Summary Notice (MSN) CMS redesigned the MSN for Part A and Part B to make it easier to read and spot fraud Shows all your services or supplies Billed to Medicare in 3month period What Medicare paid What you owe Read it carefully October 2015 Medicare and Medicaid Fraud and Abuse Prevention 36
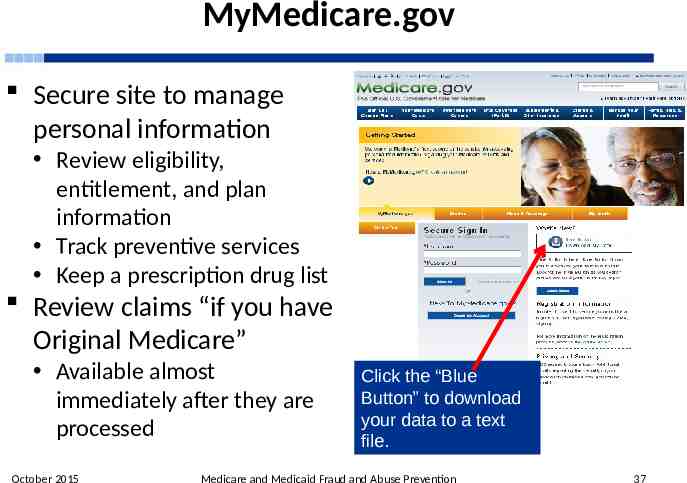
MyMedicare.gov Secure site to manage personal information Review eligibility, entitlement, and plan information Track preventive services Keep a prescription drug list Review claims “if you have Original Medicare” Available almost immediately after they are processed October 2015 Click the “Blue Button” to download your data to a text file. Medicare and Medicaid Fraud and Abuse Prevention 37
1-800-MEDICARE (TTY 1-877-486-2048) Beneficiary fraud complaints received Help target certain providers/suppliers for review Show where fraud scams are heating up Using the Interactive Voice Response System Access up to 15 months of claims Check for proper dates, services, and supplies received If not checking claims on MyMedicare.gov October 2015 Medicare and Medicaid Fraud and Abuse Prevention 38
Learning Activity John has concerns and wants to discuss his Medicare Summary Notice with you. What are some things that might indicate fraud? October 2015 Medicare and Medicaid Fraud and Abuse Prevention 39
Learning Activity What Might Indicate Fraud? Was he charged for any medical services he didn’t get? Do the dates of services look unfamiliar? Was he billed for the same thing twice? Does his credit report show any unpaid bills for medical services or equipment you didn’t receive? Has he received any collection notices for medical services or equipment he didn’t receive? October 2015 Medicare and Medicaid Fraud and Abuse Prevention 40
Fighting Fraud Can Pay You may get a reward if you meet all of these conditions: You call either 1-800-HHS-TIPS (1-800-447-8477) or call 1-800-MEDICARE (1-800-633-4227) to report suspected fraud. TTY users should call 1-877486-2048. The suspected Medicare fraud you report must be investigated and validated by CMS’s contractors. The reported fraud must be formally referred to the Office of Inspector General for further investigation. You aren’t an excluded individual. The person or organization you're reporting isn’t already under investigation by law enforcement. Your report leads directly to the recovery of at least 100 of Medicare money. October 2015 Medicare and Medicaid Fraud and Abuse Prevention 41
The Senior Medicare Patrol Education and prevention program aimed at educating beneficiaries on preventing, identifying, and reporting health care fraud Active programs in all states, the District of Columbia, Puerto Rico, Guam, and U.S. Virgin Islands Seeks volunteers to represent their communities Nationwide toll-free number: 1-877-808-2468 October 2015 Medicare and Medicaid Fraud and Abuse Prevention 42
Protecting Personal Information Only share with people you trust Doctors, other health care providers, and plans approved by Medicare Insurers who pay benefits on your behalf Trusted people in the community who work with Medicare, like your State Health Insurance Assistance Program (SHIP) or Social Security Call 1-800-MEDICARE (1‑800‑633‑4227) if you aren’t sure if a provider is approved by Medicare TTY users should call 1‑877‑486‑2048 October 2015 Medicare and Medicaid Fraud and Abuse Prevention 43
Identity Theft Identity theft is a serious crime Someone else uses your personal information, like your Social Security or Medicare number If you think someone is using your information Call your local police department Call the Federal Trade Commission’s ID Theft Hotline at 1-877-438-4338 If your Medicare card is lost or stolen, report it right away Call Social Security at 1-800-772-1213 TTY users should call 1-800-325-0778 October 2015 Medicare and Medicaid Fraud and Abuse Prevention 44
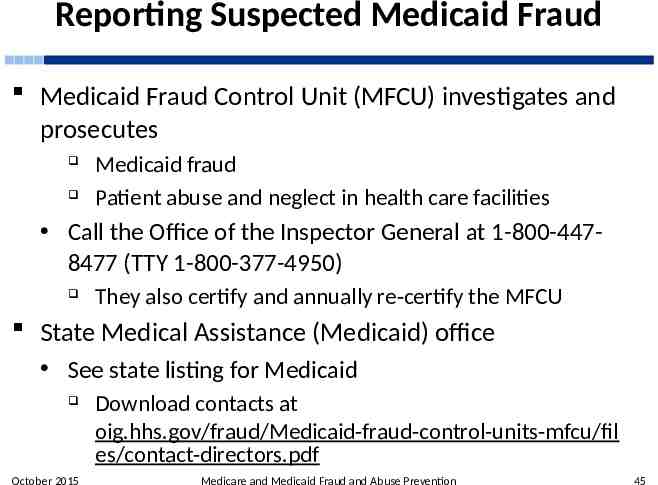
Reporting Suspected Medicaid Fraud Medicaid Fraud Control Unit (MFCU) investigates and prosecutes Medicaid fraud Patient abuse and neglect in health care facilities Call the Office of the Inspector General at 1-800-4478477 (TTY 1-800-377-4950) They also certify and annually re-certify the MFCU State Medical Assistance (Medicaid) office See state listing for Medicaid October 2015 Download contacts at oig.hhs.gov/fraud/Medicaid-fraud-control-units-mfcu/fil es/contact-directors.pdf Medicare and Medicaid Fraud and Abuse Prevention 45
Key Points to Remember The key difference between fraud and abuse is intention Improper payments are often mistakes CMS fights fraud and abuse with support from Program Integrity Contractors You can fight fraud and abuse with the 4Rs: Record, Review, Report, Remember There are many sources of additional information October 2015 Medicare and Medicaid Fraud and Abuse Prevention 46
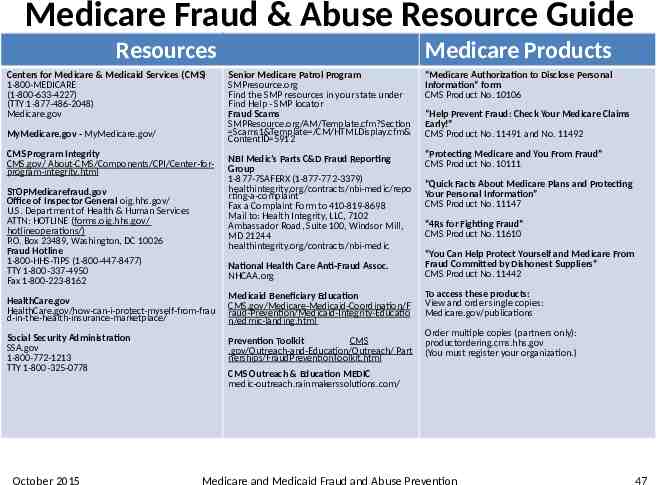
Medicare Fraud & Abuse Resource Guide Resources Centers for Medicare & Medicaid Services (CMS) 1-800-MEDICARE (1-800-633-4227) (TTY 1-877-486-2048) Medicare.gov MyMedicare.gov - MyMedicare.gov/ CMS Program Integrity CMS.gov/ About-CMS/Components/CPI/Center-forprogram-integrity.html STOPMedicarefraud.gov Office of Inspector General oig.hhs.gov/ U.S. Department of Health & Human Services ATTN: HOTLINE (forms.oig.hhs.gov/ hotlineoperations/) P.O. Box 23489, Washington, DC 10026 Fraud Hotline 1-800-HHS-TIPS (1-800-447-8477) TTY 1-800-337-4950 Fax 1-800-223-8162 Resources Medicare Products Senior Medicare Patrol Program SMPresource.org Find the SMP resources in your state under Find Help - SMP locator Fraud Scams SMPResource.org/AM/Template.cfm?Section Scams1&Template /CM/HTMLDisplay.cfm& ContentID 5912 “Medicare Authorization to Disclose Personal Information” form CMS Product No. 10106 NBI Medic’s Parts C&D Fraud Reporting Group 1-877-7SAFERX (1-877-772‑3379) healthintegrity.org/contracts/nbi-medic/repo rting-a-complaint Fax a Complaint Form to 410-819-8698 Mail to: Health Integrity, LLC, 7102 Ambassador Road, Suite 100, Windsor Mill, MD 21244 healthintegrity.org/contracts/nbi-medic “Protecting Medicare and You From Fraud” CMS Product No. 10111 National Health Care Anti-Fraud Assoc. NHCAA.org HealthCare.gov HealthCare.gov/how-can-i-protect-myself-from-frau d-in-the-health-insurance-marketplace/ Medicaid Beneficiary Education CMS.gov/Medicare-Medicaid-Coordination/F raud-Prevention/Medicaid-Integrity-Educatio n/edmic-landing.html Social Security Administration SSA.gov 1-800-772-1213 TTY 1-800-325-0778 Prevention Toolkit CMS .gov/Outreach-and-Education/Outreach/ Part nerships/FraudPreventionToolkit.html October 2015 “Help Prevent Fraud: Check Your Medicare Claims Early!” CMS Product No. 11491 and No. 11492 “Quick Facts About Medicare Plans and Protecting Your Personal Information” CMS Product No. 11147 “4Rs for Fighting Fraud” CMS Product No. 11610 “You Can Help Protect Yourself and Medicare From Fraud Committed by Dishonest Suppliers” CMS Product No. 11442 To access these products: View and order single copies: Medicare.gov/publications Order multiple copies (partners only): productordering.cms.hhs.gov (You must register your organization.) CMS Outreach & Education MEDIC medic-outreach.rainmakerssolutions.com/ Medicare and Medicaid Fraud and Abuse Prevention 47
CMS National Training Program (NTP) To view all available NTP training materials, or to subscribe to our email list, visit CMS.gov/Outreach-and-Education/Training/ CMS NationalTrainingProgram/index.html For questions about training products, email [email protected]