The Low FODMAP Diet for IBS Lauren Van Dam, MS, RD Senior GI
28 Slides4.62 MB
The Low FODMAP Diet for IBS Lauren Van Dam, MS, RD Senior GI Dietitian Division of Gastroenterology Please consider the environment before printing this PowerPoint
Overview What are FODMAPs? Mechanisms Supporting data Which foods contain FODMAPs? Nutrition counseling approach
Patient referrals & the low FODMAP diet Majority of referrals ( 70%) are for IBS/FODMAP diet Who else may benefit from low FODMAP diet: IBD (in remission), high ileostomy output Celiac disease (commonly overlapped with IBS; negative serologies/biopsy)* Gastroparesis/IBS overlap* SIBO *along with other dietary modifications
FODMAPs Fermentable Oligosaccharides – few simple sugars linked together (fructans, galactans) Disaccharides – double sugar (lactose) Monosaccharides – single sugar (fructose) And Polyols – sugar alcohols (sorbitol, mannitol, isomalt, xylitol, glycerol)
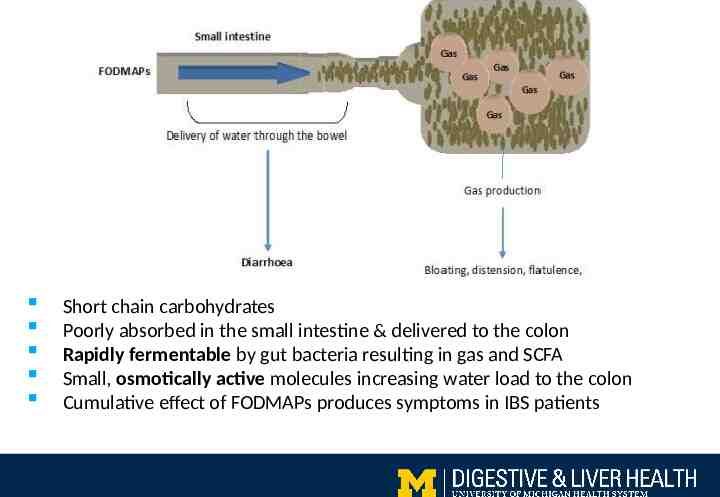
Short chain carbohydrates Poorly absorbed in the small intestine & delivered to the colon Rapidly fermentable by gut bacteria resulting in gas and SCFA Small, osmotically active molecules increasing water load to the colon Cumulative effect of FODMAPs produces symptoms in IBS patients
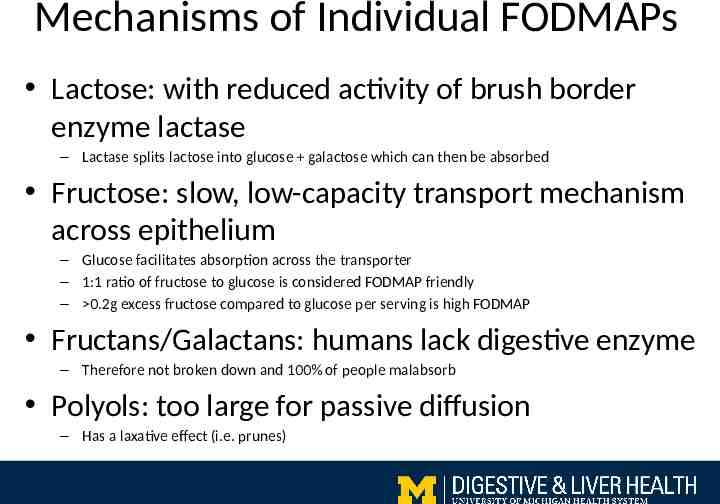
Mechanisms of Individual FODMAPs Lactose: with reduced activity of brush border enzyme lactase – Lactase splits lactose into glucose galactose which can then be absorbed Fructose: slow, low-capacity transport mechanism across epithelium – Glucose facilitates absorption across the transporter – 1:1 ratio of fructose to glucose is considered FODMAP friendly – 0.2g excess fructose compared to glucose per serving is high FODMAP Fructans/Galactans: humans lack digestive enzyme – Therefore not broken down and 100% of people malabsorb Polyols: too large for passive diffusion – Has a laxative effect (i.e. prunes)
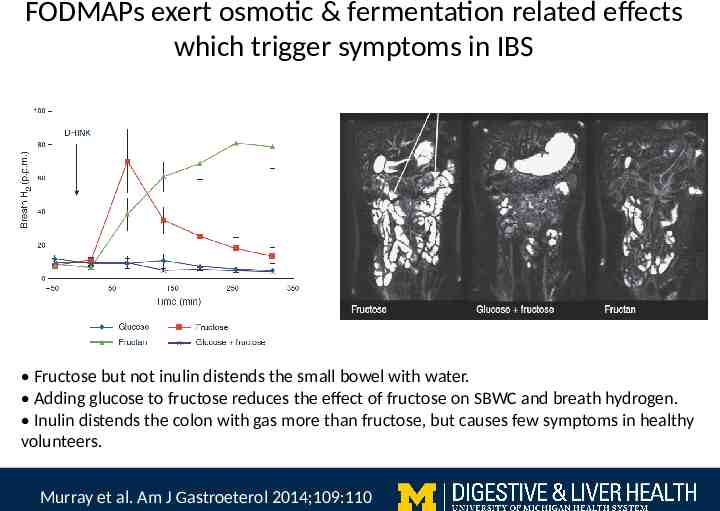
FODMAPs exert osmotic & fermentation related effects which trigger symptoms in IBS Fructose but not inulin distends the small bowel with water. Adding glucose to fructose reduces the effect of fructose on SBWC and breath hydrogen. Inulin distends the colon with gas more than fructose, but causes few symptoms in healthy volunteers. Murray et al. Am J Gastroeterol 2014;109:110
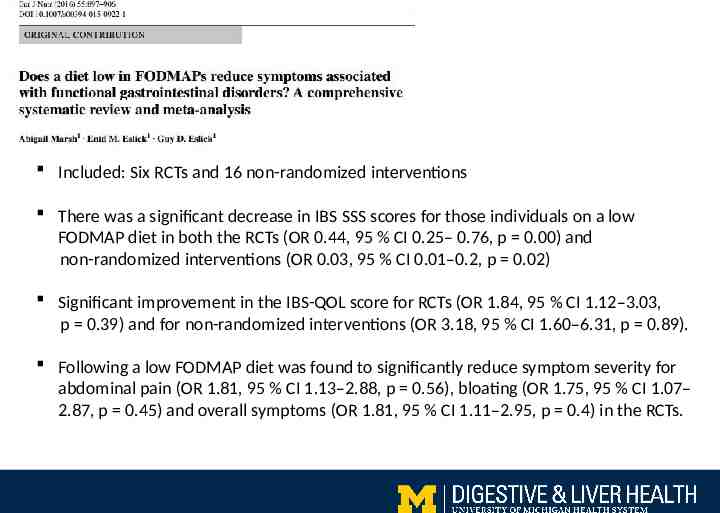
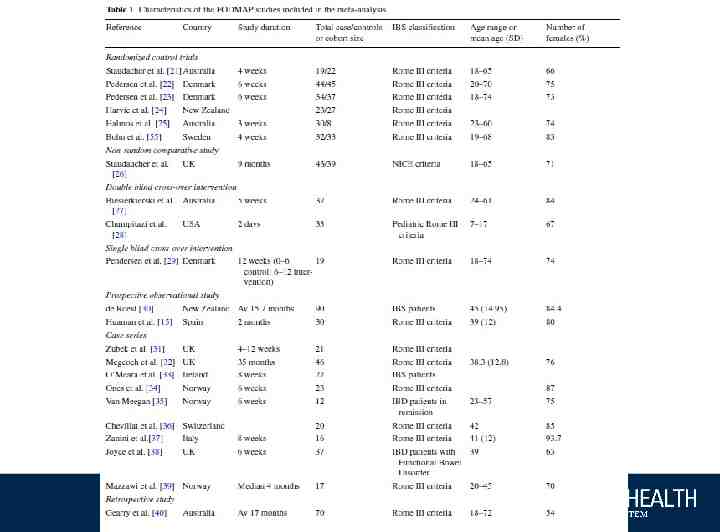
Included: Six RCTs and 16 non-randomized interventions There was a significant decrease in IBS SSS scores for those individuals on a low FODMAP diet in both the RCTs (OR 0.44, 95 % CI 0.25– 0.76, p 0.00) and non-randomized interventions (OR 0.03, 95 % CI 0.01–0.2, p 0.02) Significant improvement in the IBS-QOL score for RCTs (OR 1.84, 95 % CI 1.12–3.03, p 0.39) and for non-randomized interventions (OR 3.18, 95 % CI 1.60–6.31, p 0.89). Following a low FODMAP diet was found to significantly reduce symptom severity for abdominal pain (OR 1.81, 95 % CI 1.13–2.88, p 0.56), bloating (OR 1.75, 95 % CI 1.07– 2.87, p 0.45) and overall symptoms (OR 1.81, 95 % CI 1.11–2.95, p 0.4) in the RCTs.
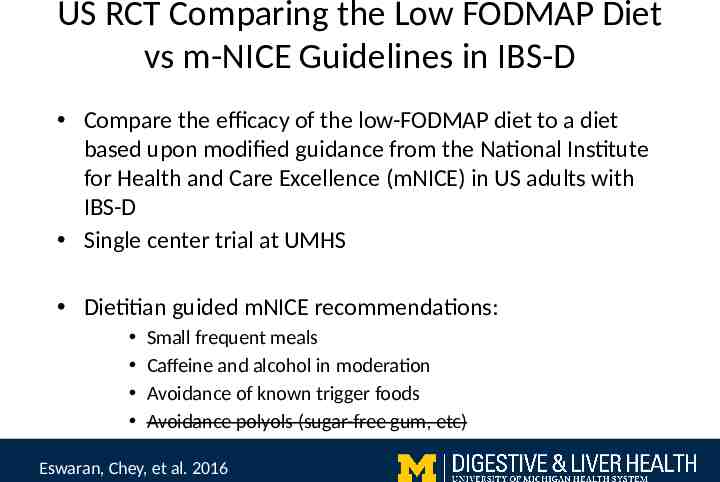
US RCT Comparing the Low FODMAP Diet vs m-NICE Guidelines in IBS-D Compare the efficacy of the low-FODMAP diet to a diet based upon modified guidance from the National Institute for Health and Care Excellence (mNICE) in US adults with IBS-D Single center trial at UMHS Dietitian guided mNICE recommendations: Small frequent meals Caffeine and alcohol in moderation Avoidance of known trigger foods Avoidance polyols (sugar-free gum, etc) Eswaran, Chey, et al. 2016
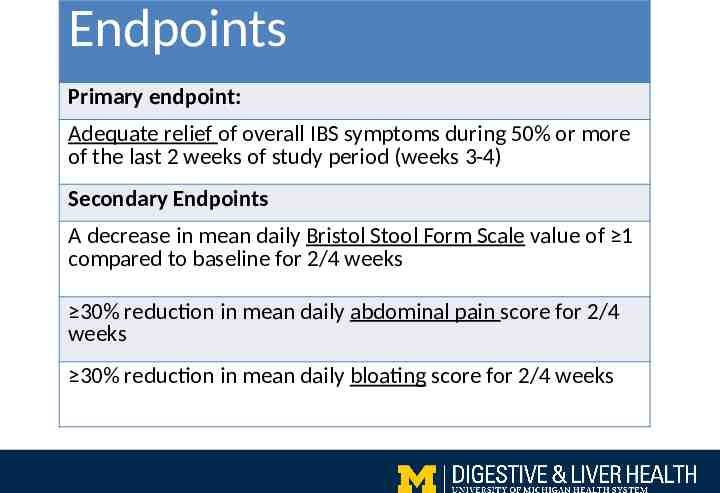
Endpoints Primary endpoint: Adequate relief of overall IBS symptoms during 50% or more of the last 2 weeks of study period (weeks 3-4) Secondary Endpoints A decrease in mean daily Bristol Stool Form Scale value of 1 compared to baseline for 2/4 weeks 30% reduction in mean daily abdominal pain score for 2/4 weeks 30% reduction in mean daily bloating score for 2/4 weeks
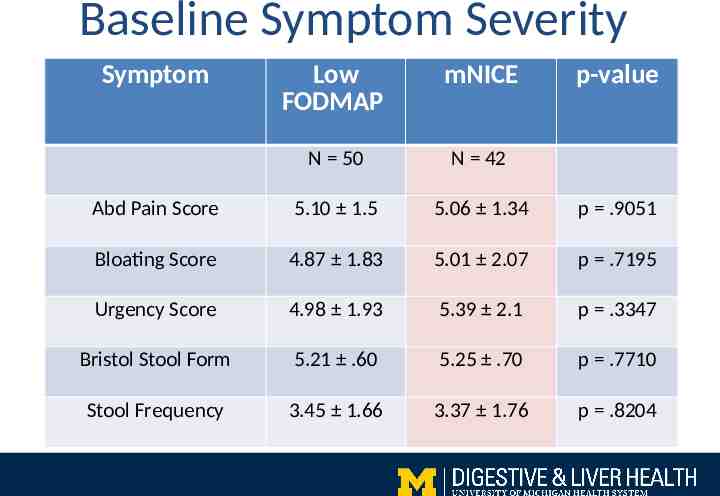
Baseline Symptom Severity Symptom Low FODMAP mNICE p-value N 50 N 42 Abd Pain Score 5.10 1.5 5.06 1.34 p .9051 Bloating Score 4.87 1.83 5.01 2.07 p .7195 Urgency Score 4.98 1.93 5.39 2.1 p .3347 Bristol Stool Form 5.21 .60 5.25 .70 p .7710 Stool Frequency 3.45 1.66 3.37 1.76 p .8204 Baseline Characteristics
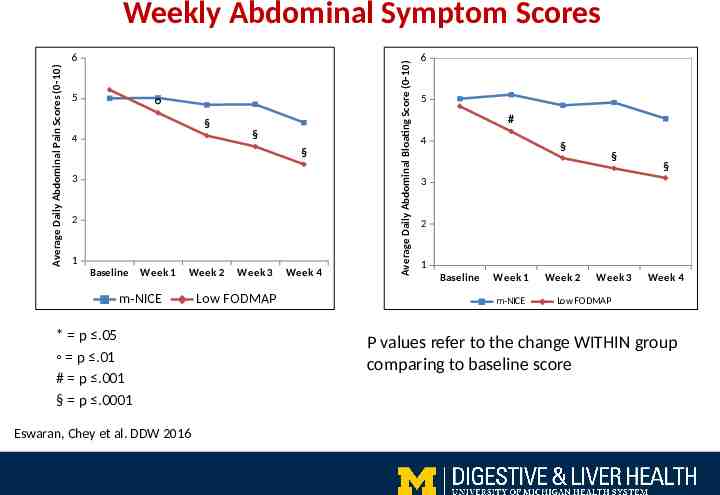
Average Daily Abdominal Pain Scores (0-10) 6 Urgency 5 § 4 § § 3 2 1 Baseline Week 1 Week 2 m-NICE * p .05 p .01 # p .001 § p .0001 Eswaran, Chey et al. DDW 2016 Week 3 Low FODMAP Week 4 Average Daily Abdominal Bloating Score (0-10) Weekly Abdominal Symptom Scores 6 5 # 4 § § § 3 2 1 Baseline Week 1 m-NICE Week 2 Week 3 Week 4 Low FODMAP P values refer to the change WITHIN group comparing to baseline score
Overall IBS- QOL Scores p .0015 p .0001 80 p .03 69.3 70 60 59.4 54.3 53.4 50 Mean Value 40 30 20 10 Baseline 0 Week 4 m-NICE Baseline Week 4 Low FODMAP
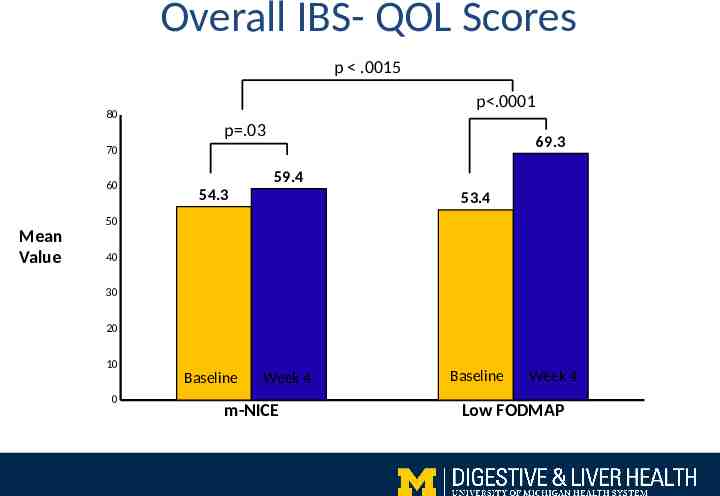
Study Conclusions Both dietitian-taught interventions improved IBS symptoms The low FODMAP diet led to significantly greater improvements in abdominal symptoms Abdominal pain Bloating Modest improvements in stool consistency Benefits extend beyond GI symptoms This study supports a role for low FODMAP diet in the treatment of IBS-D patients
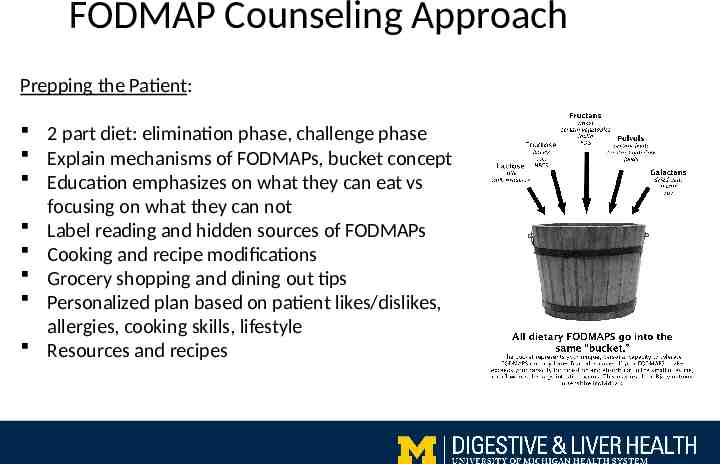
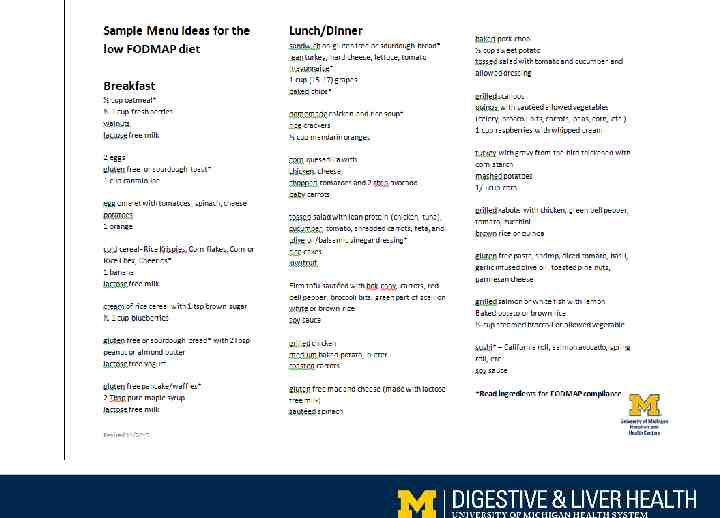
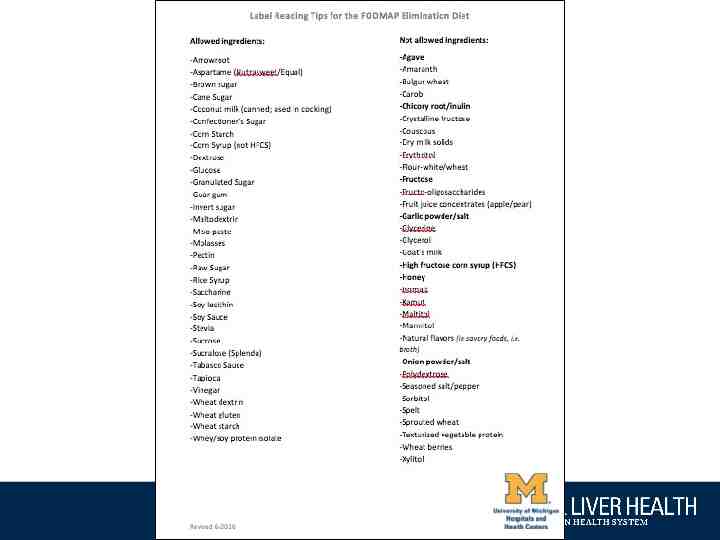
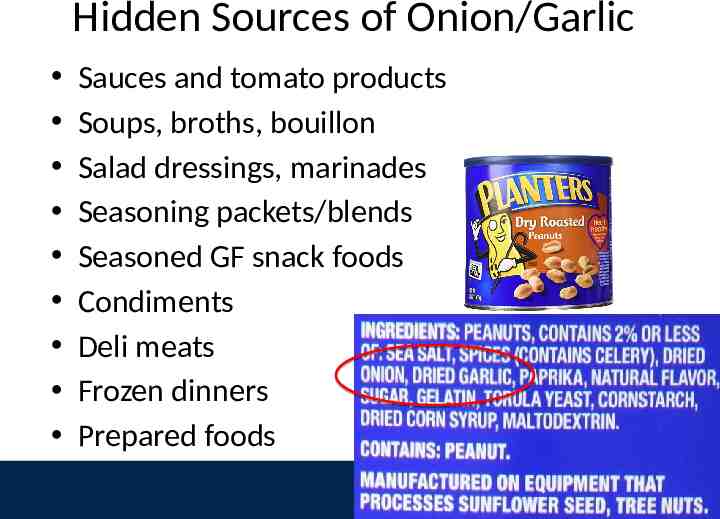
FODMAP Counseling Approach Prepping the Patient: 2 part diet: elimination phase, challenge phase Explain mechanisms of FODMAPs, bucket concept Education emphasizes on what they can eat vs focusing on what they can not Label reading and hidden sources of FODMAPs Cooking and recipe modifications Grocery shopping and dining out tips Personalized plan based on patient likes/dislikes, allergies, cooking skills, lifestyle Resources and recipes
Hidden Sources of Onion/Garlic Sauces and tomato products Soups, broths, bouillon Salad dressings, marinades Seasoning packets/blends Seasoned GF snack foods Condiments Deli meats Frozen dinners Prepared foods

http://www.myginutrition.com https://www.pinterest.com/UMGIdie titians/
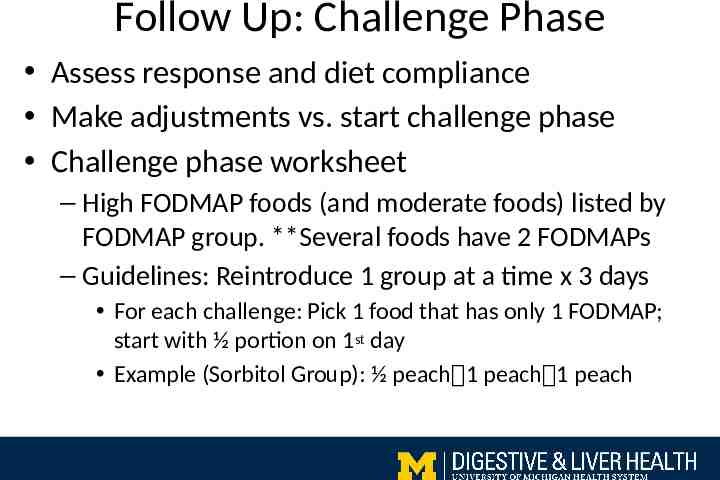
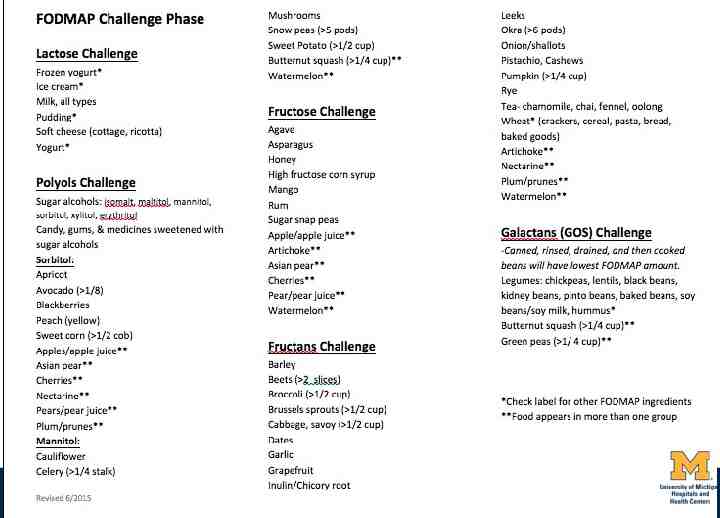
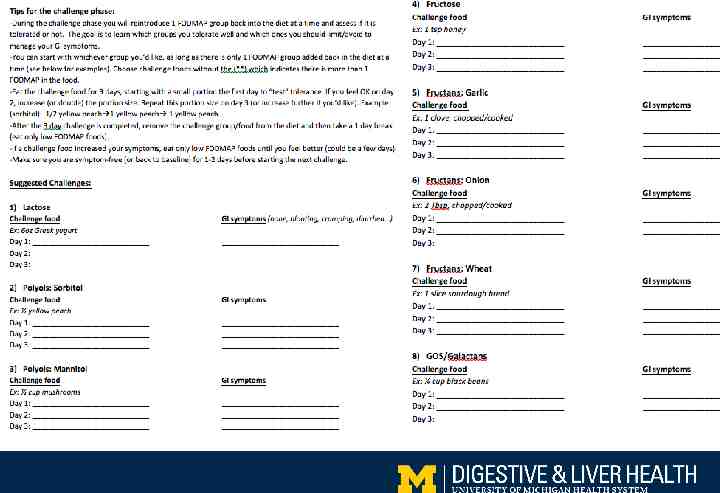
Follow Up: Challenge Phase Assess response and diet compliance Make adjustments vs. start challenge phase Challenge phase worksheet – High FODMAP foods (and moderate foods) listed by FODMAP group. **Several foods have 2 FODMAPs – Guidelines: Reintroduce 1 group at a time x 3 days For each challenge: Pick 1 food that has only 1 FODMAP; start with ½ portion on 1st day Example (Sorbitol Group): ½ peach 1 peach 1 peach
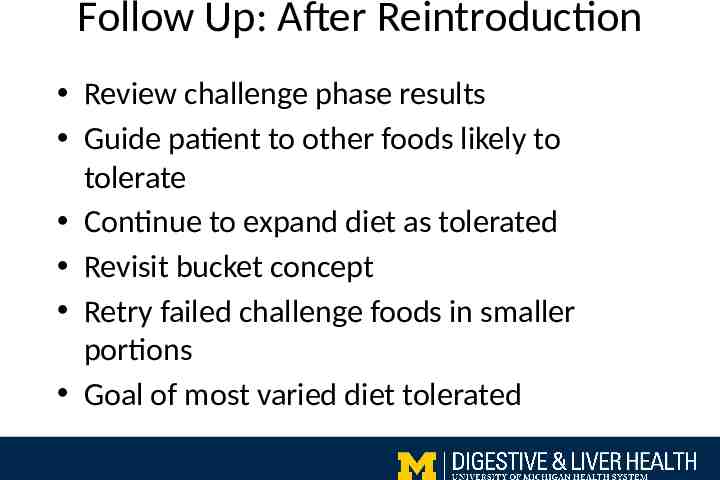
Follow Up: After Reintroduction Review challenge phase results Guide patient to other foods likely to tolerate Continue to expand diet as tolerated Revisit bucket concept Retry failed challenge foods in smaller portions Goal of most varied diet tolerated
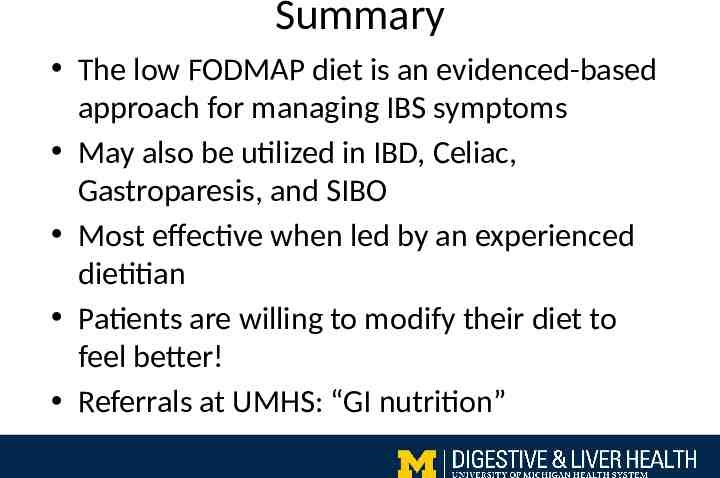
Summary The low FODMAP diet is an evidenced-based approach for managing IBS symptoms May also be utilized in IBD, Celiac, Gastroparesis, and SIBO Most effective when led by an experienced dietitian Patients are willing to modify their diet to feel better! Referrals at UMHS: “GI nutrition”
Thank you! Questions