Risk Capture & HCC CodingCardiovascular Disease Momen Wahidi, MD, MBA
18 Slides1.21 MB
Risk Capture & HCC CodingCardiovascular Disease Momen Wahidi, MD, MBA Dev Sangvai, MD, MBA
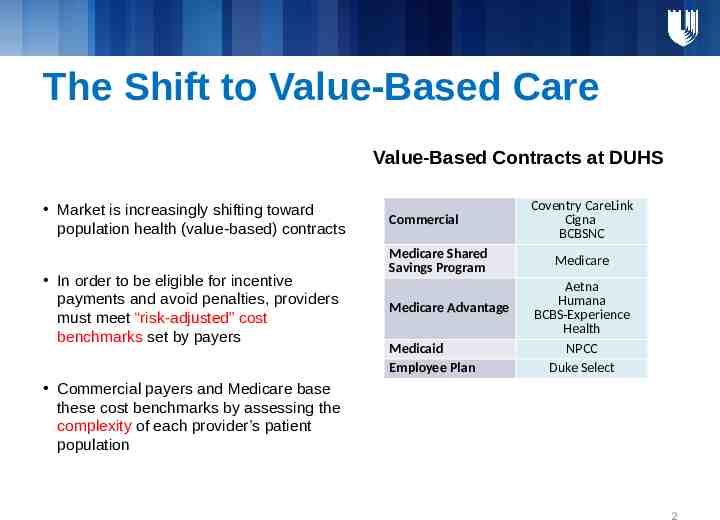
The Shift to Value-Based Care Value-Based Contracts at DUHS Market is increasingly shifting toward population health (value-based) contracts In order to be eligible for incentive payments and avoid penalties, providers must meet “risk-adjusted” cost benchmarks set by payers Commercial Medicare Shared Savings Program Medicare Advantage Medicaid Employee Plan Coventry CareLink Cigna BCBSNC Medicare Aetna Humana BCBS-Experience Health NPCC Duke Select Commercial payers and Medicare base these cost benchmarks by assessing the complexity of each provider’s patient population 2
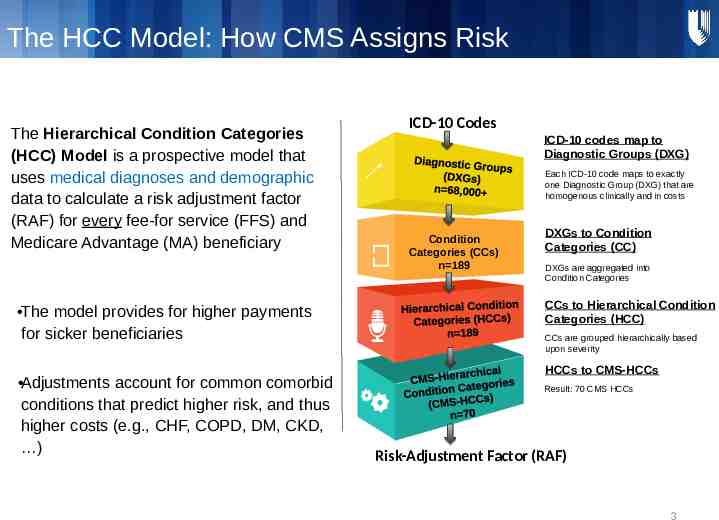
The HCC Model: How CMS Assigns Risk The HCC Model: How CMS Assigns Risk The Hierarchical Condition Categories (HCC) Model is a prospective model that uses medical diagnoses and demographic data to calculate a risk adjustment factor (RAF) for every fee-for service (FFS) and Medicare Advantage (MA) beneficiary The model provides for higher payments for sicker beneficiaries Adjustments account for common comorbid conditions that predict higher risk, and thus higher costs (e.g., CHF, COPD, DM, CKD, ) ICD-10 Codes ICD-10 codes map to Diagnostic Groups (DXG) Each ICD-10 code maps to exactly one Diagnostic Group (DXG) that are homogenous clinically and in costs Condition Categories (CCs) n 189 DXGs to Condition Categories (CC) DXGs are aggregated into Condition Categories CCs to Hierarchical Condition Categories (HCC) CCs are grouped hierarchically based upon severity HCCs to CMS-HCCs Result: 70 CMS HCCs Risk-Adjustment Factor (RAF) 3
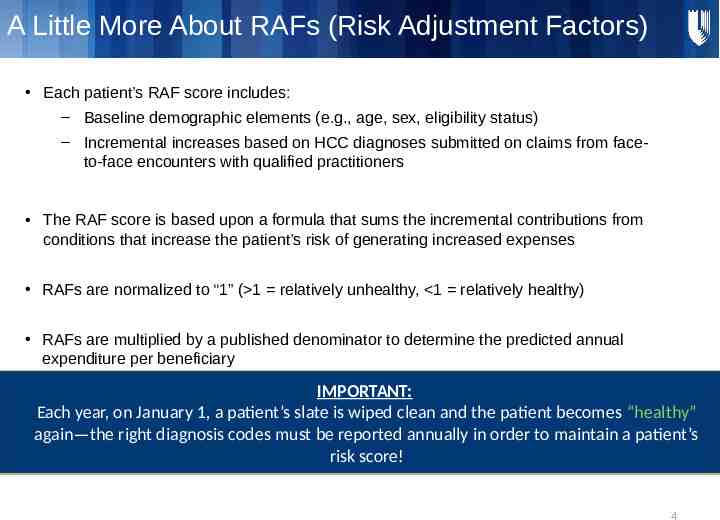
A Little More About RAFs (Risk Adjustment Factors) Each patient’s RAF score includes: A Little More About RAFs (Risk Adjustment Factors) – Baseline demographic elements (e.g., age, sex, eligibility status) – Incremental increases based on HCC diagnoses submitted on claims from faceto-face encounters with qualified practitioners The RAF score is based upon a formula that sums the incremental contributions from conditions that increase the patient’s risk of generating increased expenses RAFs are normalized to “1” ( 1 relatively unhealthy, 1 relatively healthy) RAFs are multiplied by a published denominator to determine the predicted annual expenditure per beneficiary IMPORTANT: Each year, on January 1, a patient’s slate is wiped clean and the patient becomes “healthy” again—the right diagnosis codes must be reported annually in order to maintain a patient’s risk score! 4
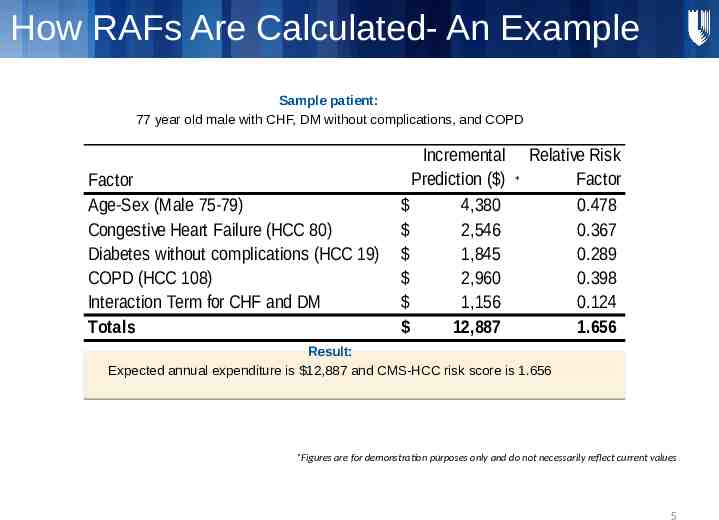
How RAFs Are Calculated- An Example Sample patient: 77 year old male with CHF, DM without complications, and COPD Factor Age-Sex (Male 75-79) Congestive Heart Failure (HCC 80) Diabetes without complications (HCC 19) COPD (HCC 108) Interaction Term for CHF and DM Totals Incremental Prediction ( ) 4,380 2,546 1,845 2,960 1,156 12,887 * Relative Risk Factor 0.478 0.367 0.289 0.398 0.124 1.656 Result: Expected annual expenditure is 12,887 and CMS-HCC risk score is 1.656 *Figures are for demonstration purposes only and do not necessarily reflect current values 5
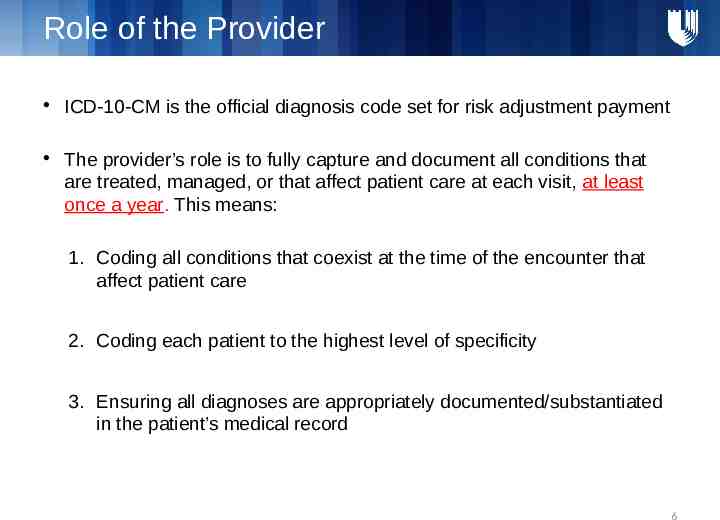
Role of the Provider Role of the ICD-10-CM is theProvider official diagnosis code set for risk adjustment payment The provider’s role is to fully capture and document all conditions that are treated, managed, or that affect patient care at each visit, at least once a year. This means: 1. Coding all conditions that coexist at the time of the encounter that affect patient care 2. Coding each patient to the highest level of specificity 3. Ensuring all diagnoses are appropriately documented/substantiated in the patient’s medical record 6
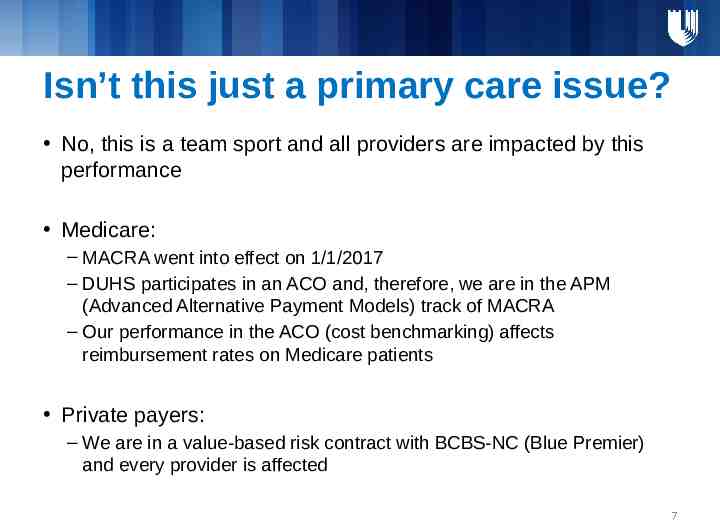
Isn’t this just a primary care issue? No, this is a team sport and all providers are impacted by this performance Medicare: – MACRA went into effect on 1/1/2017 – DUHS participates in an ACO and, therefore, we are in the APM (Advanced Alternative Payment Models) track of MACRA – Our performance in the ACO (cost benchmarking) affects reimbursement rates on Medicare patients Private payers: – We are in a value-based risk contract with BCBS-NC (Blue Premier) and every provider is affected 7
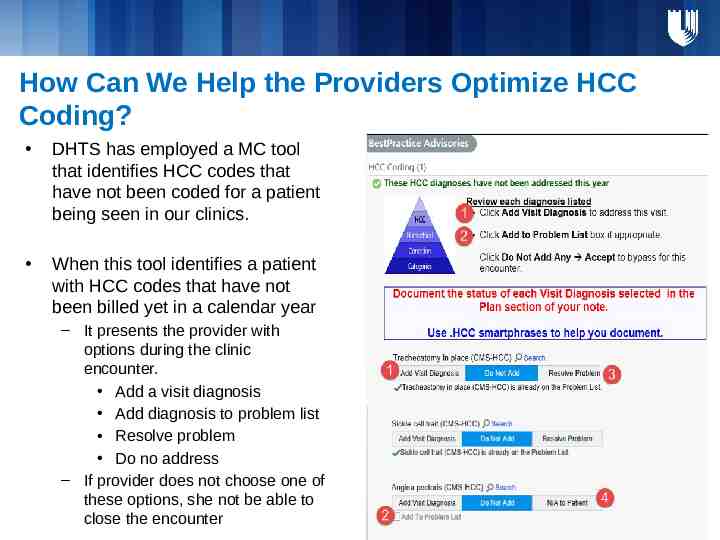
How Can We Help the Providers Optimize HCC Coding? DHTS has employed a MC tool that identifies HCC codes that have not been coded for a patient being seen in our clinics. When this tool identifies a patient with HCC codes that have not been billed yet in a calendar year – It presents the provider with options during the clinic encounter. Add a visit diagnosis Add diagnosis to problem list Resolve problem Do no address – If provider does not choose one of these options, she not be able to close the encounter
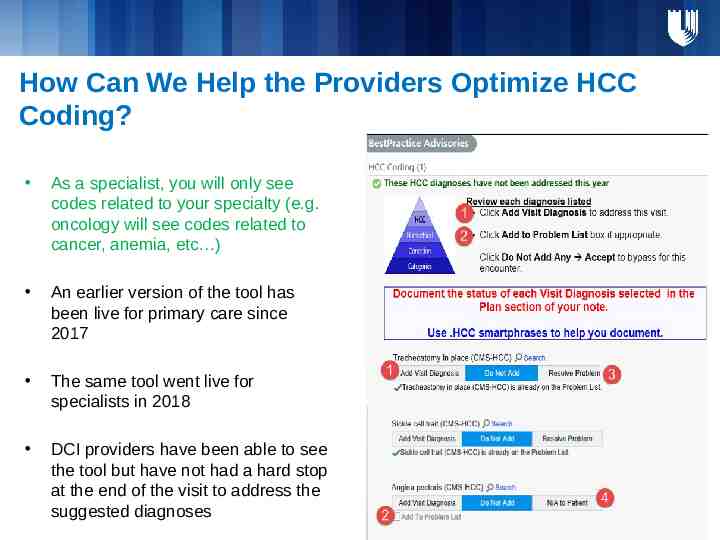
How Can We Help the Providers Optimize HCC Coding? As a specialist, you will only see codes related to your specialty (e.g. oncology will see codes related to cancer, anemia, etc ) An earlier version of the tool has been live for primary care since 2017 The same tool went live for specialists in 2018 DCI providers have been able to see the tool but have not had a hard stop at the end of the visit to address the suggested diagnoses
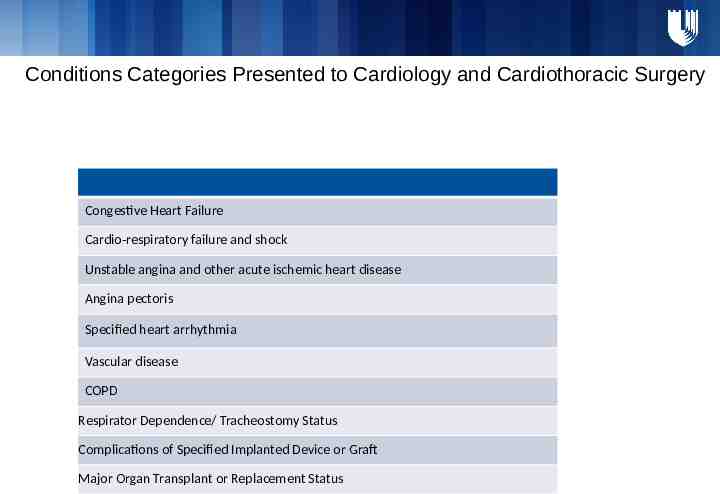
Conditions Categories Presented to Cardiology and Cardiothoracic Surgery Congestive Heart Failure Cardio-respiratory failure and shock Unstable angina and other acute ischemic heart disease Angina pectoris Specified heart arrhythmia Vascular disease COPD Respirator Dependence/ Tracheostomy Status Complications of Specified Implanted Device or Graft Major Organ Transplant or Replacement Status
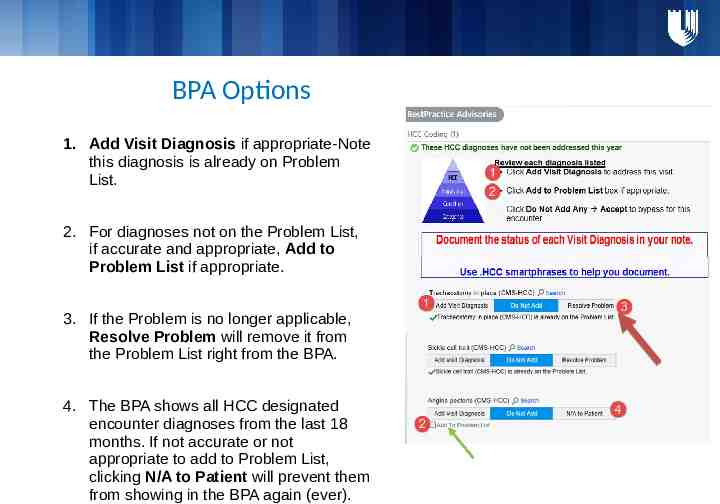
BPA Options 1. Add Visit Diagnosis if appropriate-Note this diagnosis is already on Problem List. 2. For diagnoses not on the Problem List, if accurate and appropriate, Add to Problem List if appropriate. 3. If the Problem is no longer applicable, Resolve Problem will remove it from the Problem List right from the BPA. 4. The BPA shows all HCC designated encounter diagnoses from the last 18 months. If not accurate or not appropriate to add to Problem List, clicking N/A to Patient will prevent them from showing in the BPA again (ever).

Conditions Specific Documentation Opportunities
A M B U L ATO RY D O C U M E N TAT I O N A N D CO D I N G I N A M B U L ATO R Y D O C U M E N TAT I O N A N D C O D I N G AMBULATORY DOCUMENTATION AND CODING I N I T I AT I V E INITIATIVE Ambulatory Documentation and Coding Operations (ADCO) Team – Helps support clinics and providers through real time education and feedback Paula Allard, Director Coding Operations Brittainy McKinney, Manager ADCO Kimberly Telesco, ADCO Educator Bobette Haley, ADCO Educator ADCI Clinical Leadership Team Dr. John Paat and Dr. Momen Wahidi, PDC Dr. John Anderson, DPC Population Health Management Office (PHMO) PDC and DUHS Compliance Many More . 13
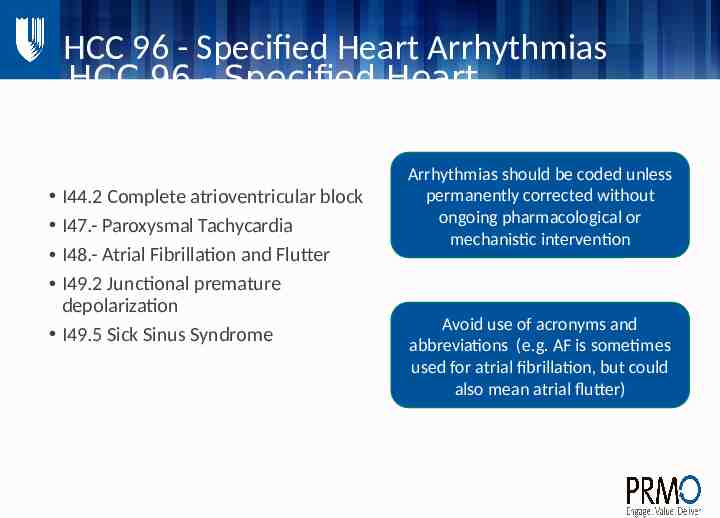
HCC 96 - Specified Heart Arrhythmias HCC 96 - Specified Heart Arrhythmias I44.2 Complete atrioventricular block I47.- Paroxysmal Tachycardia I48.- Atrial Fibrillation and Flutter I49.2 Junctional premature depolarization I49.5 Sick Sinus Syndrome Arrhythmias should be coded unless permanently corrected without ongoing pharmacological or mechanistic intervention Avoid use of acronyms and abbreviations (e.g. AF is sometimes used for atrial fibrillation, but could also mean atrial flutter)
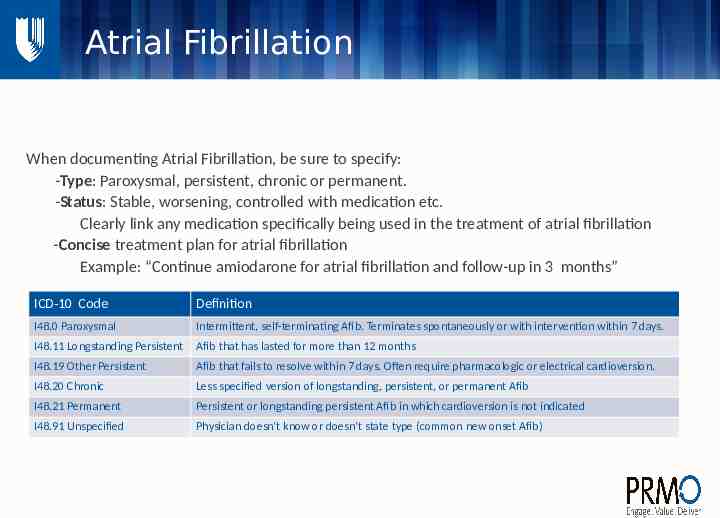
Atrial Fibrillation Atrial Fibrillation When documenting Atrial Fibrillation, be sure to specify: -Type: Paroxysmal, persistent, chronic or permanent. -Status: Stable, worsening, controlled with medication etc. Clearly link any medication specifically being used in the treatment of atrial fibrillation -Concise treatment plan for atrial fibrillation Example: “Continue amiodarone for atrial fibrillation and follow-up in 3 months” ICD-10 Code Definition I48.0 Paroxysmal Intermittent, self-terminating Afib. Terminates spontaneously or with intervention within 7 days. I48.11 Longstanding Persistent Afib that has lasted for more than 12 months I48.19 Other Persistent Afib that fails to resolve within 7 days. Often require pharmacologic or electrical cardioversion. I48.20 Chronic Less specified version of longstanding, persistent, or permanent Afib I48.21 Permanent Persistent or longstanding persistent Afib in which cardioversion is not indicated I48.91 Unspecified Physician doesn’t know or doesn’t state type (common new onset Afib)
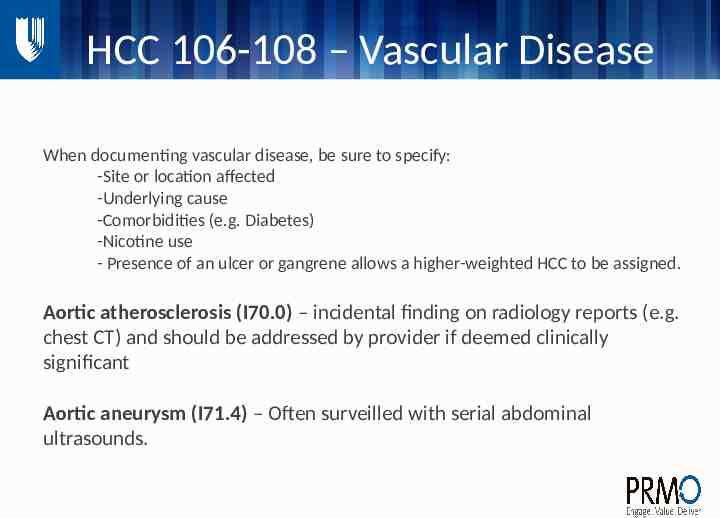
HCC 106-108 – Vascular Disease HCC 106-108 – Vascular Disease When documenting vascular disease, be sure to specify: -Site or location affected -Underlying cause -Comorbidities (e.g. Diabetes) -Nicotine use - Presence of an ulcer or gangrene allows a higher-weighted HCC to be assigned. Aortic atherosclerosis (I70.0) – incidental finding on radiology reports (e.g. chest CT) and should be addressed by provider if deemed clinically significant Aortic aneurysm (I71.4) – Often surveilled with serial abdominal ultrasounds.
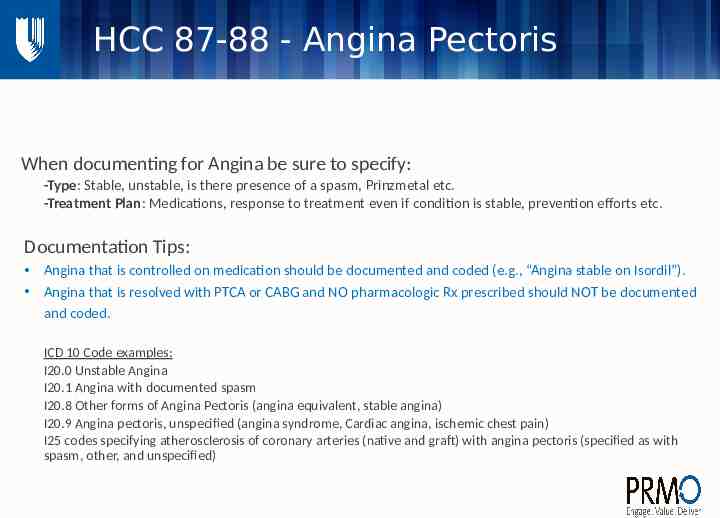
HCC 87-88 - Angina Pectoris HCC 87-88 - Angina Pectoris When documenting for Angina be sure to specify: -Type: Stable, unstable, is there presence of a spasm, Prinzmetal etc. -Treatment Plan: Medications, response to treatment even if condition is stable, prevention efforts etc. Documentation Tips: Angina that is controlled on medication should be documented and coded (e.g., “Angina stable on Isordil”). Angina that is resolved with PTCA or CABG and NO pharmacologic Rx prescribed should NOT be documented and coded. ICD 10 Code examples: I20.0 Unstable Angina I20.1 Angina with documented spasm I20.8 Other forms of Angina Pectoris (angina equivalent, stable angina) I20.9 Angina pectoris, unspecified (angina syndrome, Cardiac angina, ischemic chest pain) I25 codes specifying atherosclerosis of coronary arteries (native and graft) with angina pectoris (specified as with spasm, other, and unspecified)
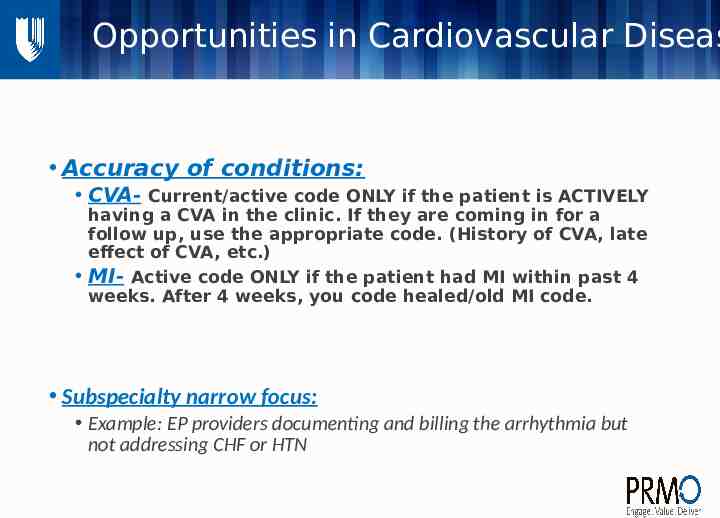
Opportunities in Cardiovascular Diseas MI and CVA coding in clinic Accuracy of conditions: CVA- Current/active code ONLY if the patient is ACTIVELY having a CVA in the clinic. If they are coming in for a follow up, use the appropriate code. (History of CVA, late effect of CVA, etc.) MI- Active code ONLY if the patient had MI within past 4 weeks. After 4 weeks, you code healed/old MI code. Subspecialty narrow focus: Example: EP providers documenting and billing the arrhythmia but not addressing CHF or HTN