Rheumatoid Arthritis Osteoarthritis & Systemic Lupus Erythematosus
62 Slides4.25 MB
Rheumatoid Arthritis Osteoarthritis & Systemic Lupus Erythematosus By Brianne O’Neill And Lynn Bates
Objectives Understand the pathophysiology of RA,OA, & SLE. Review signs and symptoms of RA, OA, & SLE. Understand how these conditions affects a persons everyday life. Understand the treatments available for RA, OA, & SLE.

Arthritis “arthr” joint “itis” inflammation “Arthritis can affect babies and children, as well as people in the prime of their lives” Osteoarthritis Rheumatoid Arthritis Systemic Lupus Erythematosus Gout Childhood Arthritis (Juvenile Idiopathic Arthritis) (The Arthritis Society, 2012)
Facts Leading cause of disability in Canada Affects 1 in 6 individuals Costs Canadians 33 billion each year 2/3 individuals with arthritis are women One of the most prevalent chronic diseases of Aboriginal peoples Skeletal remains from humans living 4500BC show signs of arthritis By 2031 approximately 7 million people will be living with Arthritis Has caused more deaths than melanoma, asthma, or HIV/AIDS Only 1.3% of research is dedicated to arthritis. (The Arthritis Society , 2012; Statistics Canada, 2012; Canadian Arthritis Network, 2007)
Myths # 1: Arthritis isn’t serious #2: Arthritis is an old person’s disease #3:Arthritis is a normal part of aging #4: Not much can be done for those living with arthritis #5: People with arthritis can’t exercise (Arthritis Foundation, 2012)
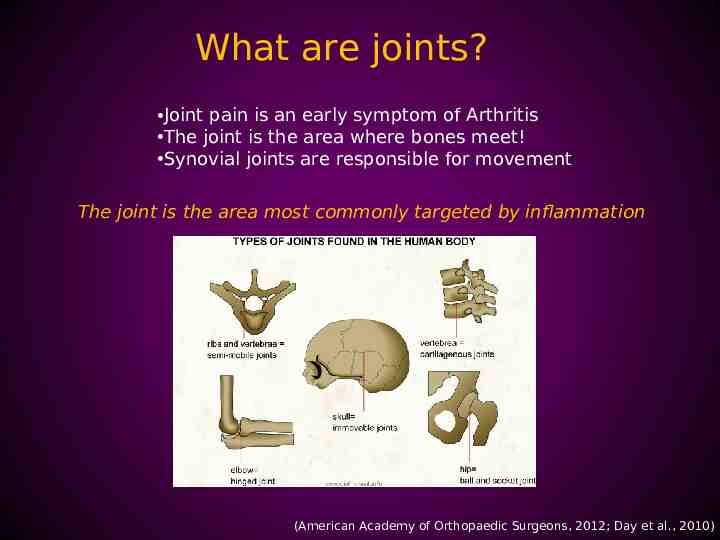
What are joints? Joint pain is an early symptom of Arthritis The joint is the area where bones meet! Synovial joints are responsible for movement The joint is the area most commonly targeted by inflammation (American Academy of Orthopaedic Surgeons, 2012; Day et al., 2010)
http://www.youtube.com/watch? v nCL-Xm7k DE&feature related
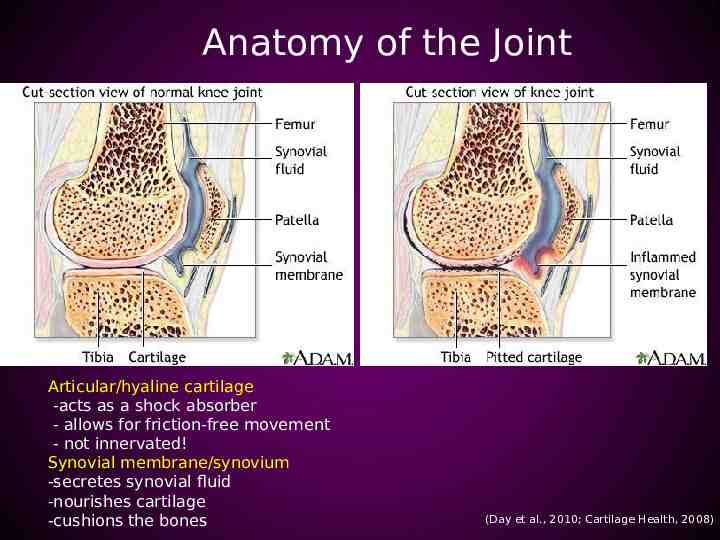
Anatomy of the Joint Articular/hyaline cartilage -acts as a shock absorber - allows for friction-free movement - not innervated! Synovial membrane/synovium -secretes synovial fluid -nourishes cartilage -cushions the bones (Day et al., 2010; Cartilage Health, 2008)
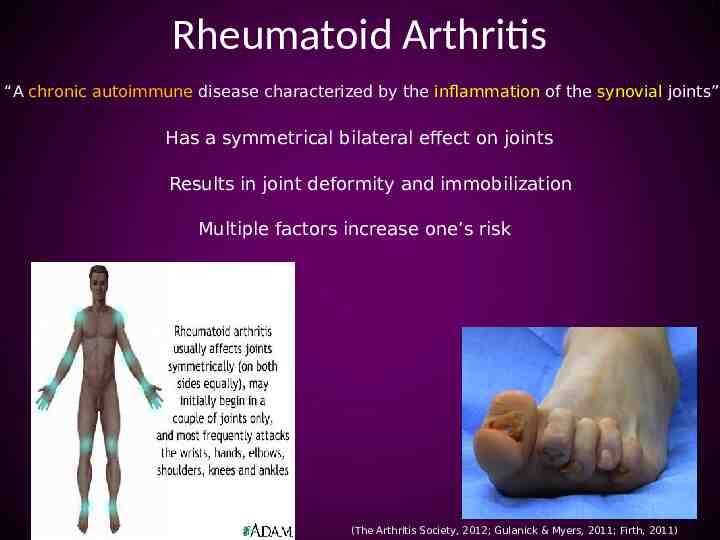
Rheumatoid Arthritis “A chronic autoimmune disease characterized by the inflammation of the synovial joints” Has a symmetrical bilateral effect on joints Results in joint deformity and immobilization Multiple factors increase one’s risk (The Arthritis Society, 2012; Gulanick & Myers, 2011; Firth, 2011)

Symptoms Morning stiffness lasting more than half an hour Simultaneous symmetrical joint swelling Not relieved by rest Fever Weight loss Fatigue Anemia Lymph node enlargement Nodules Raynaud’s phenomenon (The Arthritis Society, 2012; Firth, 2011; Oliver, 2010; Day et al., 2010)
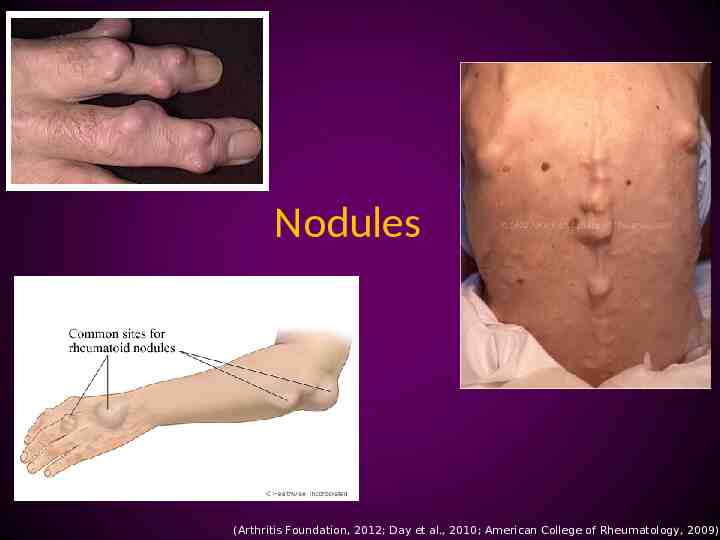
Nodules (Arthritis Foundation, 2012; Day et al., 2010; American College of Rheumatology, 2009)

Diagnosis No single test is specific to Rheumatoid Arthritis CBC Radiographs of involved joints CT/MRI scans Direct arthroscopy Synovial/Fluid aspirate Synovial membrane biopsy Arthrocentesis (National Institute of Arthritis and Musculoskeletal and Skin Diseases, 2012)
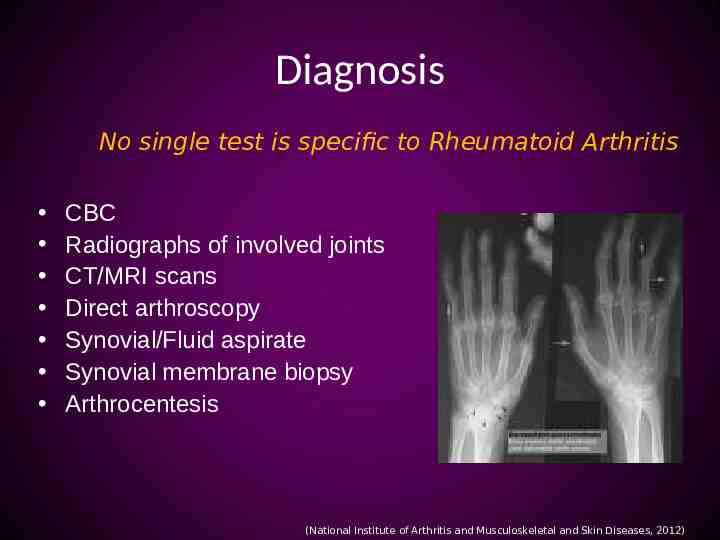
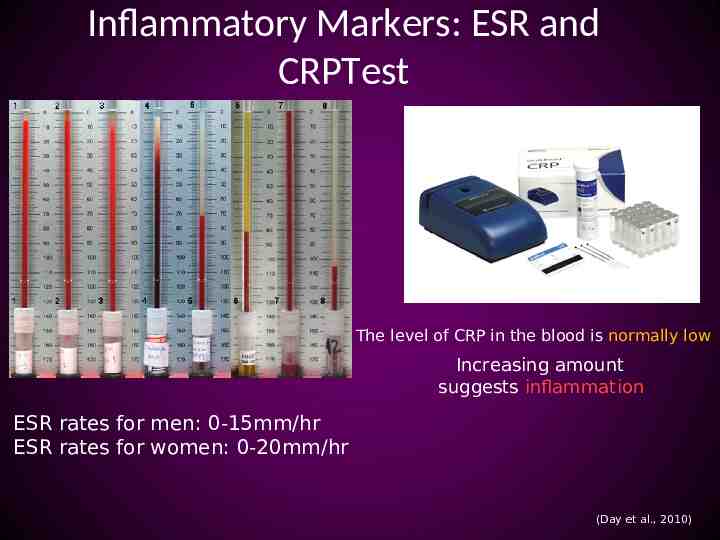
Inflammatory Markers: ESR and CRPTest The level of CRP in the blood is normally low Increasing amount suggests inflammation ESR rates for men: 0-15mm/hr ESR rates for women: 0-20mm/hr (Day et al., 2010)
Antibody Tests: Rheumatoid Factor Test and CCP Other blood tests check for the presence of antibodies that are not normally present in the human body (National Rheumatoid Arthritis Society, 2012; Day et al., 2010)
Direct arthroscopy Benefits Minimally invasive Less tissue damage Fewer complications Reduced pain Quicker recovery time Outpatient basis (American Academy of Orthopaedic Surgeons, 2012; Day et al., 2010)

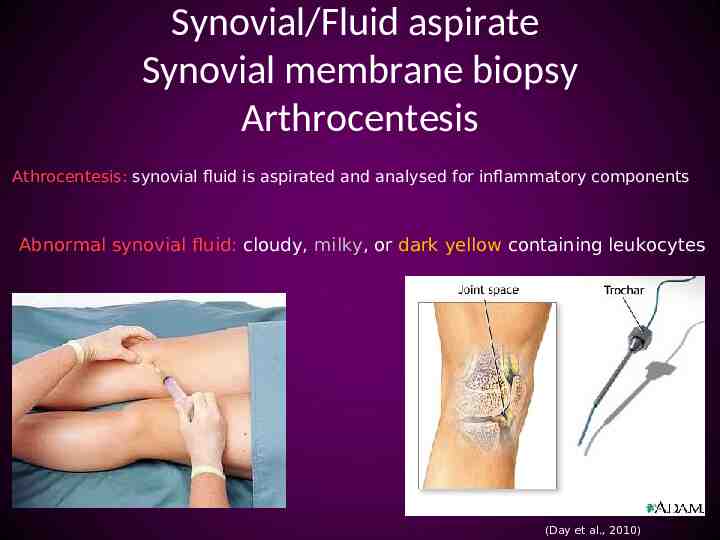
Synovial/Fluid aspirate Synovial membrane biopsy Arthrocentesis Athrocentesis: synovial fluid is aspirated and analysed for inflammatory components Abnormal synovial fluid: cloudy, milky, or dark yellow containing leukocytes (Day et al., 2010)
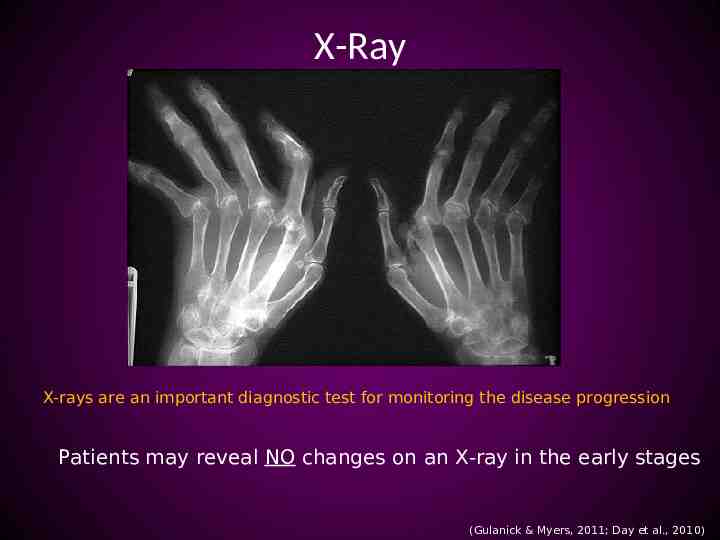
X-Ray X-rays are an important diagnostic test for monitoring the disease progression Patients may reveal NO changes on an X-ray in the early stages (Gulanick & Myers, 2011; Day et al., 2010)
Arthography A radiopaque substance or air is injected into the joint, which outlines soft tissue structures surrounding the joint http://www.youtube.com/watch? v 2YJsuDxxNJE&feature related (Day et al, 2010)
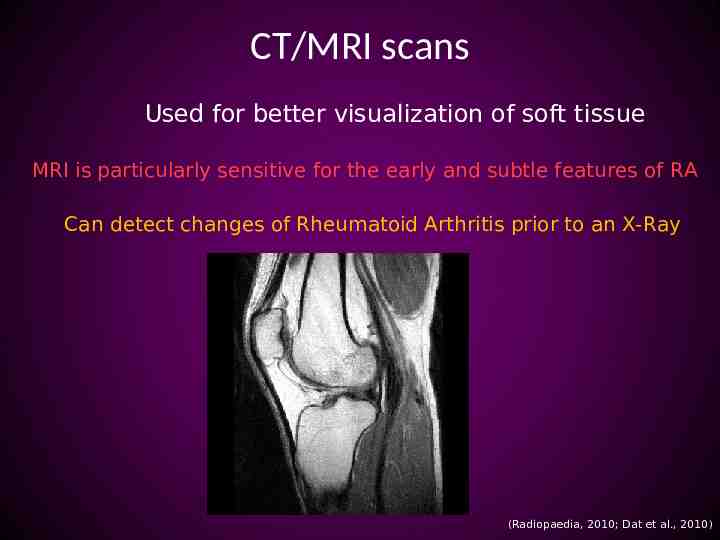
CT/MRI scans Used for better visualization of soft tissue MRI is particularly sensitive for the early and subtle features of RA Can detect changes of Rheumatoid Arthritis prior to an X-Ray (Radiopaedia, 2010; Dat et al., 2010 )
Newly Diagnosed The major goal is to relieve pain and inflammation and prevent further joint damage Anxiety, depression, and a low self esteem commonly accompanies Rheumatoid Arthritis (Walker, 2012; Gulanick & Myers, 2011; The Arthritis Society, 2011; Firth, 2011)

Medications There are four types of medications used to treat RA: – Non-steroidal anti-inflammatory drugs (NSAIDs) – Disease-modifying anti-rheumatic drugs(DMARDS). – Corticosteroids – Biologic Response Modifiers (“Bioligics”) (Arthritis Foundation, 2012; Gulanick & Myers 2011)
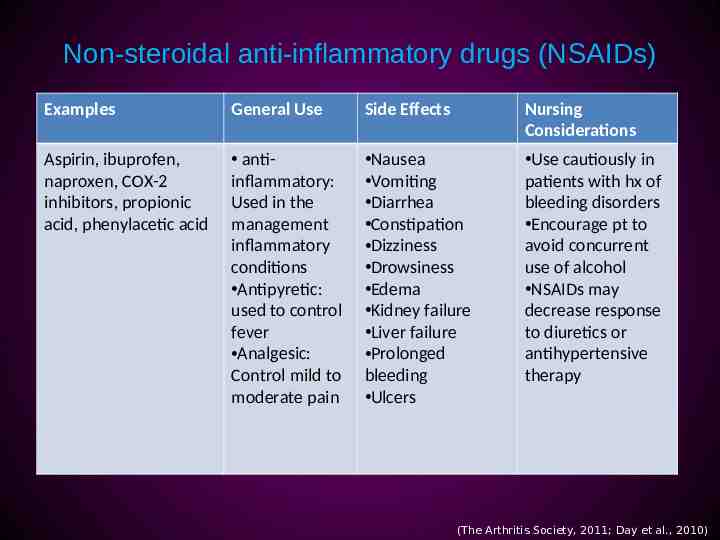
Non-steroidal anti-inflammatory drugs (NSAIDs) Examples General Use Side Effects Nursing Considerations Aspirin, ibuprofen, naproxen, COX-2 inhibitors, propionic acid, phenylacetic acid antiinflammatory: Used in the management inflammatory conditions Antipyretic: used to control fever Analgesic: Control mild to moderate pain Nausea Vomiting Diarrhea Constipation Dizziness Drowsiness Edema Kidney failure Liver failure Prolonged bleeding Ulcers Use cautiously in patients with hx of bleeding disorders Encourage pt to avoid concurrent use of alcohol NSAIDs may decrease response to diuretics or antihypertensive therapy (The Arthritis Society, 2011; Day et al., 2010)
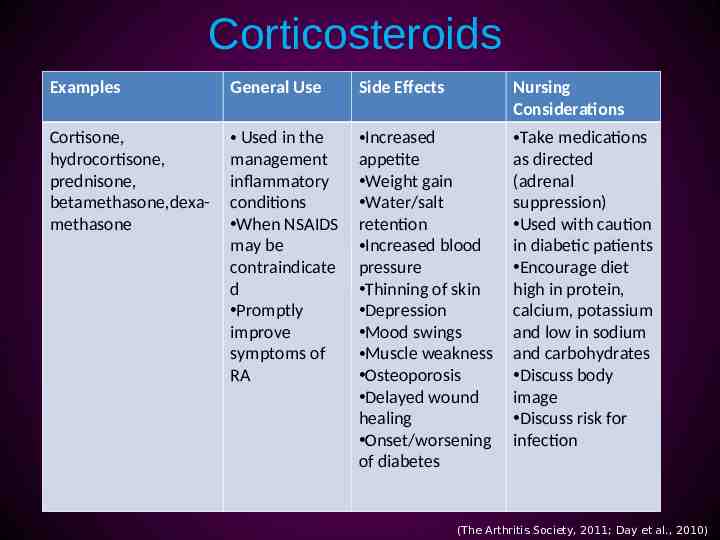
Corticosteroids Examples General Use Side Effects Nursing Considerations Cortisone, hydrocortisone, prednisone, betamethasone,dexamethasone Used in the management inflammatory conditions When NSAIDS may be contraindicate d Promptly improve symptoms of RA Increased appetite Weight gain Water/salt retention Increased blood pressure Thinning of skin Depression Mood swings Muscle weakness Osteoporosis Delayed wound healing Onset/worsening of diabetes Take medications as directed (adrenal suppression) Used with caution in diabetic patients Encourage diet high in protein, calcium, potassium and low in sodium and carbohydrates Discuss body image Discuss risk for infection (The Arthritis Society, 2011; Day et al., 2010)
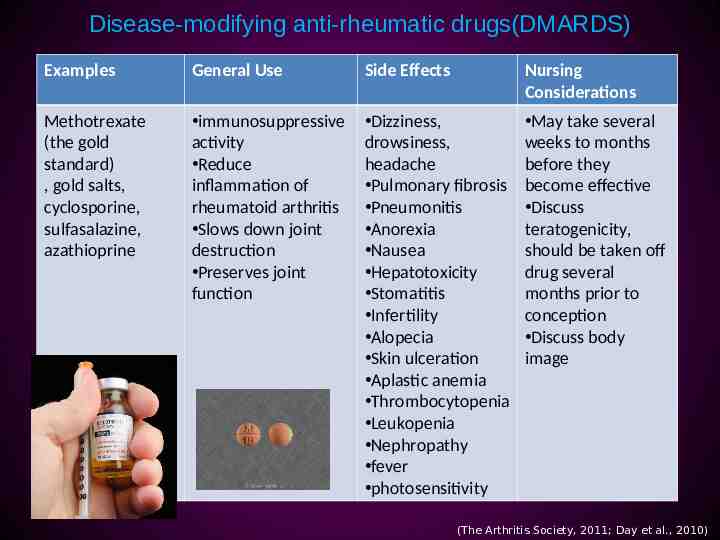
Disease-modifying anti-rheumatic drugs(DMARDS) Examples General Use Side Effects Nursing Considerations Methotrexate (the gold standard) , gold salts, cyclosporine, sulfasalazine, azathioprine immunosuppressive activity Reduce inflammation of rheumatoid arthritis Slows down joint destruction Preserves joint function Dizziness, drowsiness, headache Pulmonary fibrosis Pneumonitis Anorexia Nausea Hepatotoxicity Stomatitis Infertility Alopecia Skin ulceration Aplastic anemia Thrombocytopenia Leukopenia Nephropathy fever photosensitivity May take several weeks to months before they become effective Discuss teratogenicity, should be taken off drug several months prior to conception Discuss body image (The Arthritis Society, 2011; Day et al., 2010)
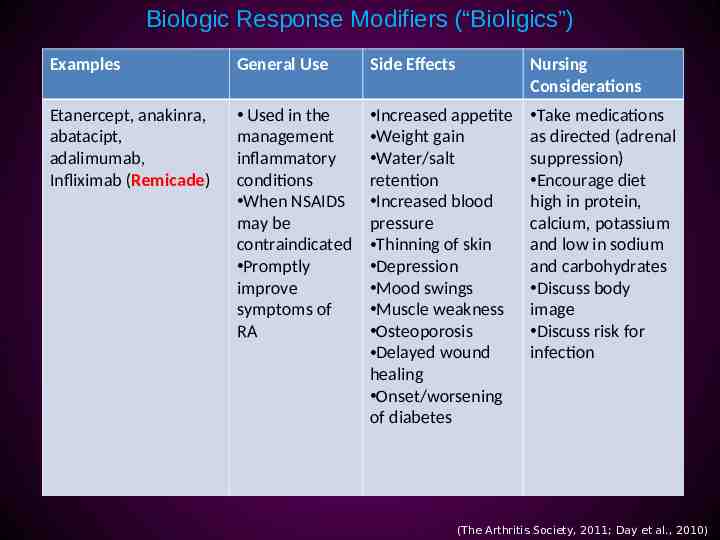
Biologic Response Modifiers (“Bioligics”) Examples General Use Side Effects Nursing Considerations Etanercept, anakinra, abatacipt, adalimumab, Infliximab (Remicade) Used in the management inflammatory conditions When NSAIDS may be contraindicated Promptly improve symptoms of RA Increased appetite Weight gain Water/salt retention Increased blood pressure Thinning of skin Depression Mood swings Muscle weakness Osteoporosis Delayed wound healing Onset/worsening of diabetes Take medications as directed (adrenal suppression) Encourage diet high in protein, calcium, potassium and low in sodium and carbohydrates Discuss body image Discuss risk for infection (The Arthritis Society, 2011; Day et al., 2010)
Alternative Medicine Olive leaf extract Aloe Vera Green Tea Omega 3 Ginger Root Extract Cats Claw Omega 3 interferes with blood clotting drugs! (American College of Rheumatology, 2012)

Pain Pain is subjective and influenced by multiple factors Lack of control Helpless Stressful events can increase symptoms of arthritis Consider drugs such as Paxil, Elavil or Zoloft (Day et al., 2010; Canadian Psychological Association, 2009)

Exercise Being overweight strains joints and leads to further inflammation 4 times a week for 30 minutes Walking Light jogging Water aerobics Cycling Yoga Tai chi stretching (Arthritis Foundation, 2012)
Nutrition The most commonly observed vitamin and mineral deficiencies in patients with RA are: o folic acid o vitamin C o vitamin D o vitamin B6 o vitamin B12 o vitamin E o calcium o magnesium o zinc o selenium (Johns Hopkins Arthritis Center, 2012)

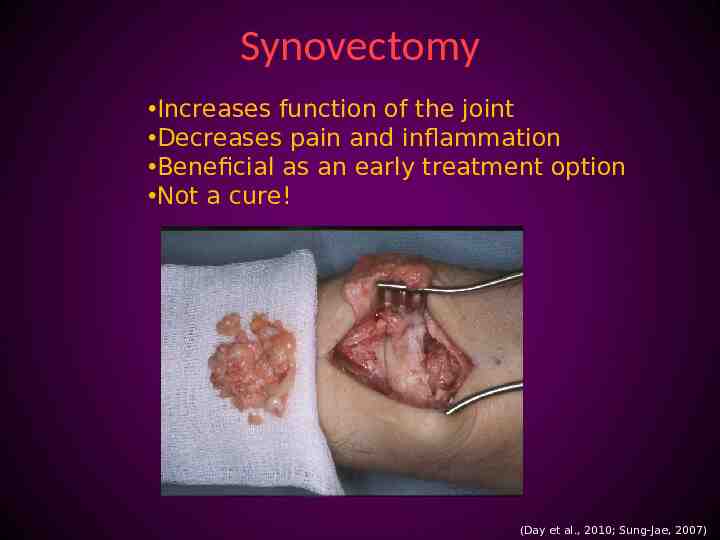
Synovectomy Increases function of the joint Decreases pain and inflammation Beneficial as an early treatment option Not a cure! (Day et al., 2010; Sung-Jae, 2007)
Braces/casts/splints Support injured joints and weak muscles Improve joint mobility and stability Help to alleviate pain, swelling and muscle spasm May prevent further damage and deformity (Johns Hopkins Arthritis Center, 2012)

Osteoarthritis Most common form of arthritis Over 3 million Canadians affected (1/10) Osteoarthritis is defined as “a degenerative joint disease characterized by destruction of the articular cartilage and overgrowth of bone” (Arthritis Society, 2011; Day et al., 2010)
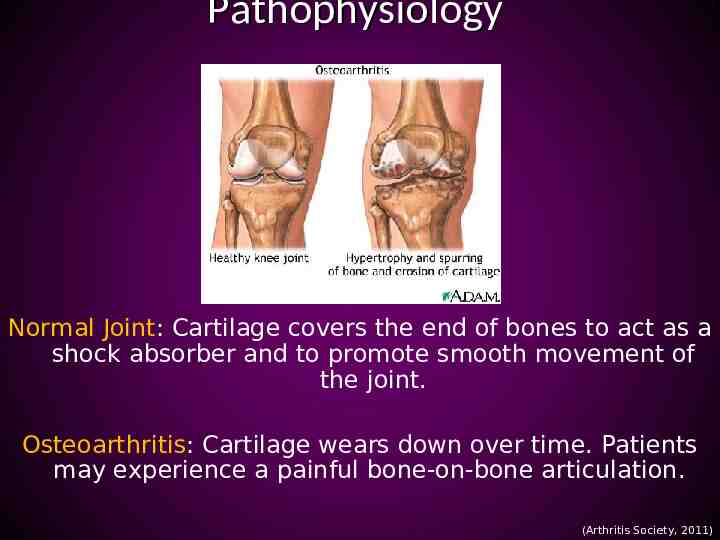
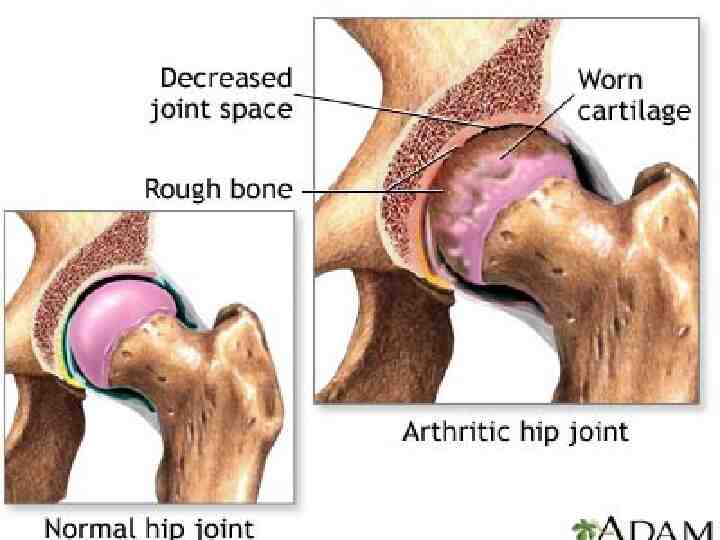
Pathophysiology Normal Joint: Cartilage covers the end of bones to act as a shock absorber and to promote smooth movement of the joint. Osteoarthritis: Cartilage wears down over time. Patients may experience a painful bone-on-bone articulation. (Arthritis Society, 2011)
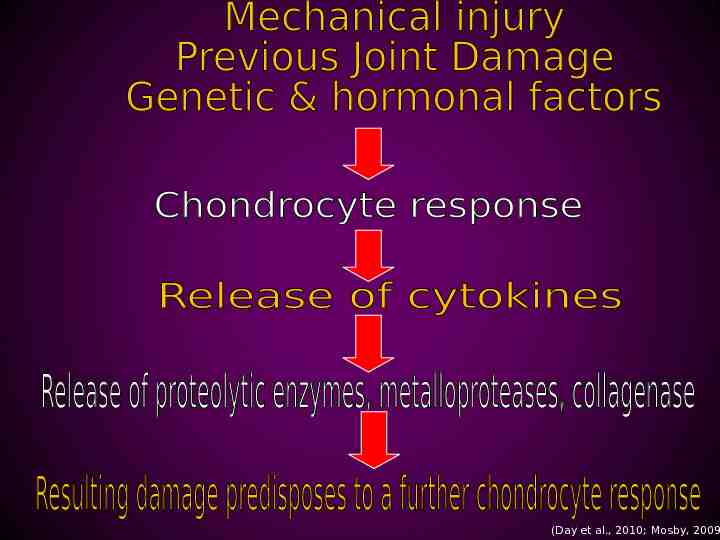
(Day et al., 2010; Mosby, 2009
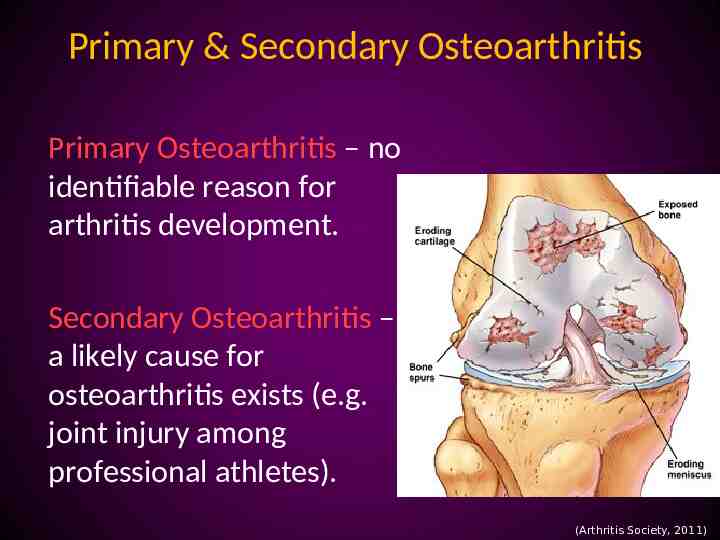
Primary & Secondary Osteoarthritis Primary Osteoarthritis – no identifiable reason for arthritis development. Secondary Osteoarthritis – a likely cause for osteoarthritis exists (e.g. joint injury among professional athletes). (Arthritis Society, 2011)
Risk Factors for OA Age Family History Excess weight Joint injury Complications of other types of arthritis MYTH – Normal wear and tear (Arthritis Society, 2011; Day et al., 2010)
Signs & Symptoms of OA Joint pain Feeling joints “locking” Joint “creaking” Stiff joints in the morning Joint swelling Loss of joint flexibility or strength (Arthritis Society, 2011)
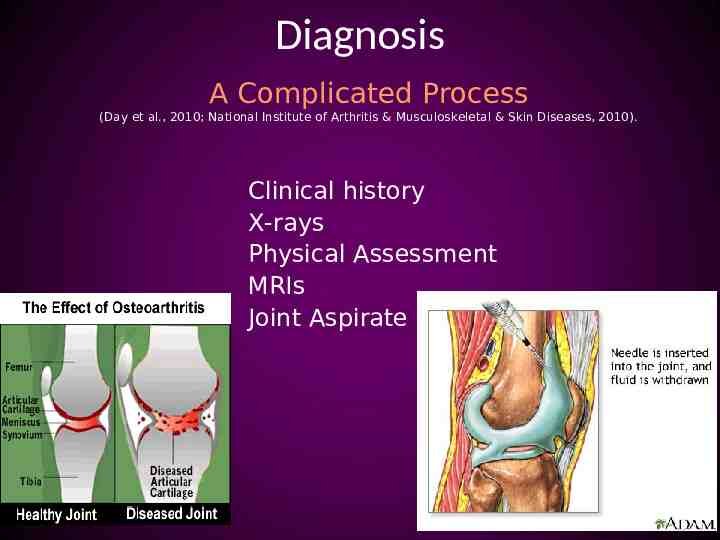
Diagnosis A Complicated Process (Day et al., 2010; National Institute of Arthritis & Musculoskeletal & Skin Diseases, 2010). Clinical history X-rays Physical Assessment MRIs Joint Aspirate
Non-Pharmacological Management Exercise Weight loss Heat & Cold Therapy Activity pacing Maintaining proper joint alignment Use of assistive devices Relaxation Exercises (Day et al., 2010; Arthritis Society, 2011; Walker, 2011)
Pharmacological Management Acetaminophen NSAIDs Opioids Corticosteroid injections Topical analgesics Glucosamine and chondroitin (Day et al., 2010; Arthritis Society, 2011)
Surgical Management Osteotomy Arthrodesis Arthroplasty – Total knee replacement – Total hip replacement (Day et al, 2010)
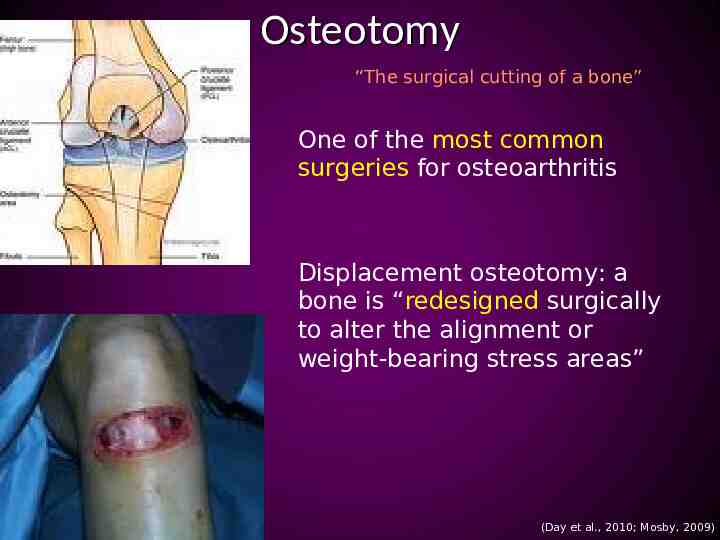
Osteotomy “The surgical cutting of a bone” One of the most common surgeries for osteoarthritis Displacement osteotomy: a bone is “redesigned surgically to alter the alignment or weight-bearing stress areas” (Day et al., 2010; Mosby, 2009)
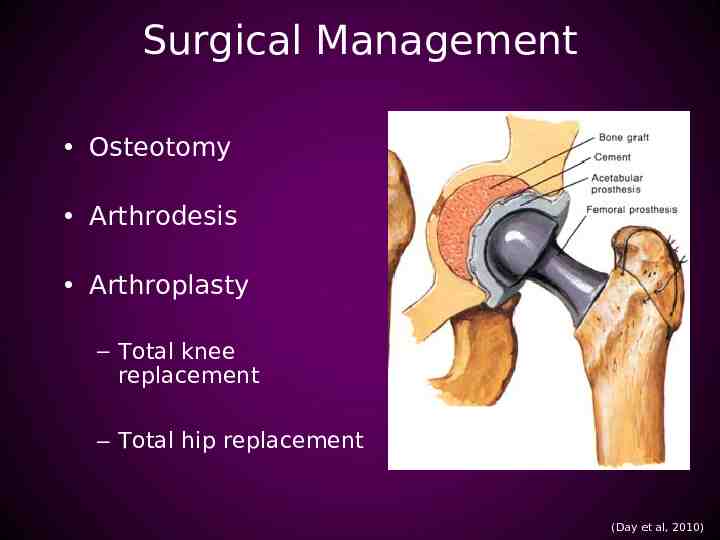
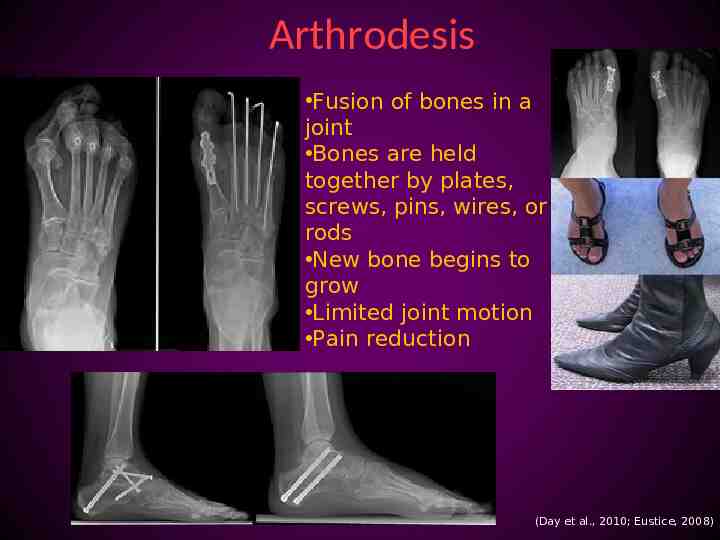
Arthrodesis Fusion of bones in a joint Bones are held together by plates, screws, pins, wires, or rods New bone begins to grow Limited joint motion Pain reduction (Day et al., 2010; Eustice, 2008)
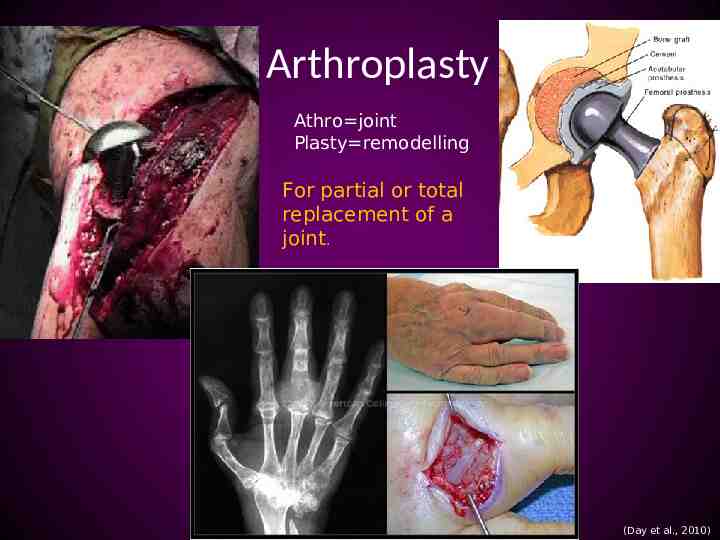
Arthroplasty Athro joint Plasty remodelling For partial or total replacement of a joint. (Day et al., 2010)
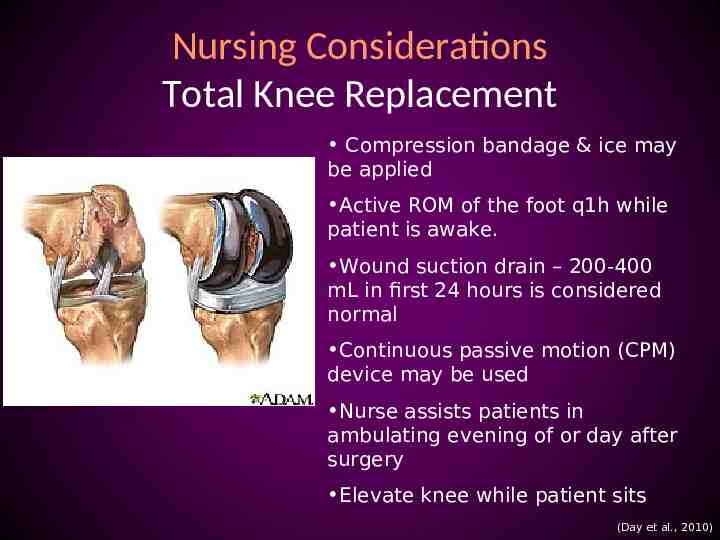
Nursing Considerations Total Knee Replacement Compression bandage & ice may be applied Active ROM of the foot q1h while patient is awake. Wound suction drain – 200-400 mL in first 24 hours is considered normal Continuous passive motion (CPM) device may be used Nurse assists patients in ambulating evening of or day after surgery Elevate knee while patient sits (Day et al., 2010)
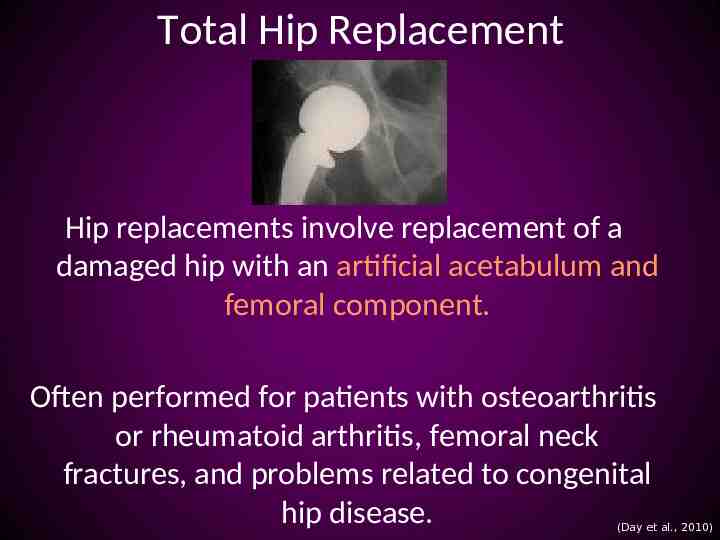
Total Hip Replacement Hip replacements involve replacement of a damaged hip with an artificial acetabulum and femoral component. Often performed for patients with osteoarthritis or rheumatoid arthritis, femoral neck fractures, and problems related to congenital hip disease. (Day et al., 2010)
Nursing Considerations Total Hip Replacement Hip precautions Monitor for dislodgement Abduct leg Keep HOB less than 60 degrees Use of fracture bedpan High-seat surfaces Sleep on unaffected side Avoid crossing legs No bending at the waist (Day et al., 2010)
Pre-op Care Educating Patient Discharge planning Evaluating patient risks (Walker, 2012)
Post-op Care Monitor VS Wound assessments Neurovascular assessments Monitor wound drainage Pain relief Infection/Osteomyelitis prevention Promote early ambulation Ensure physiotherapy is consulted (Walker, 2012; Day et al., 2010)
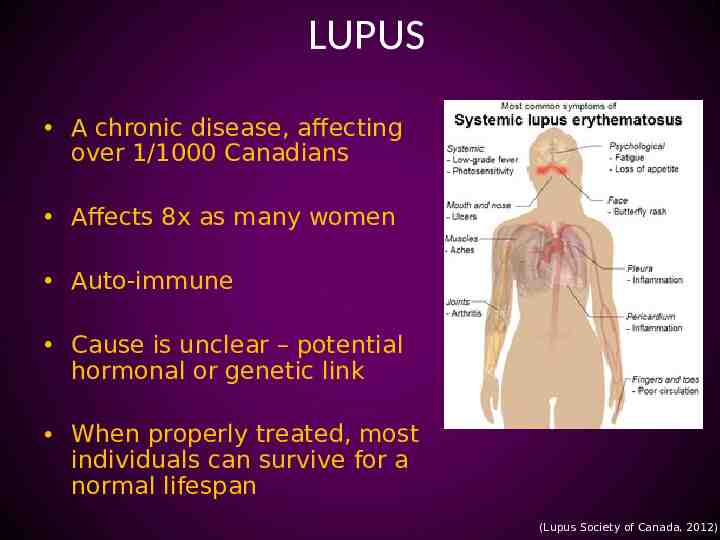
LUPUS A chronic disease, affecting over 1/1000 Canadians Affects 8x as many women Auto-immune Cause is unclear – potential hormonal or genetic link When properly treated, most individuals can survive for a normal lifespan (Lupus Society of Canada, 2012)
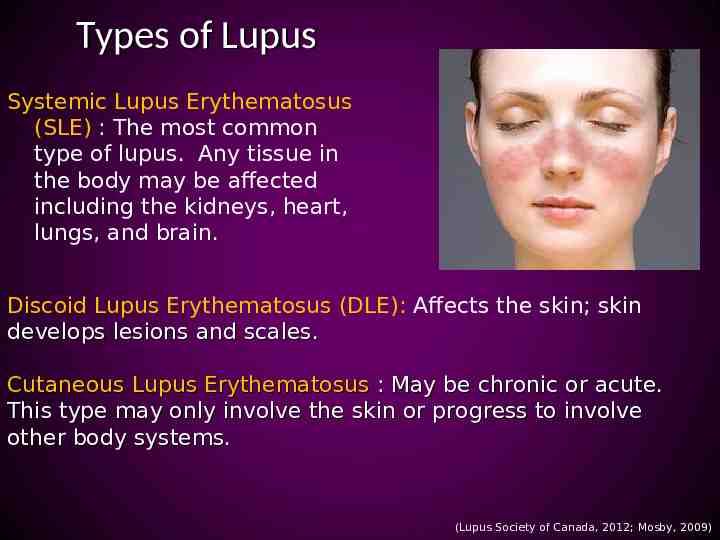
Types of Lupus Systemic Lupus Erythematosus (SLE) : The most common type of lupus. Any tissue in the body may be affected including the kidneys, heart, lungs, and brain. Discoid Lupus Erythematosus (DLE): Affects the skin; skin develops lesions and scales. Cutaneous Lupus Erythematosus : May be chronic or acute. This type may only involve the skin or progress to involve other body systems. (Lupus Society of Canada, 2012; Mosby, 2009)
(Lupus Society of Canada, 2012)
Manifestations of SLE (Mosby, 2009; Lupus Society of Canada, 2012)
Pharmacological Therapy Acetaminophen NSAIDs Corticosteroids Cytotoxic or Immunosuppressive drugs Antimalarial drugs (Lupus Society of Canada, 2012; Arthritis Society, 2010; Day et al, 2010)

Healthy Lifestyle (Arthritis Society, 2010)

Nursing Considerations Educate patient on lupus. Help patient identify factors that precipitate flare-ups. Assess patient’s medication knowledge. Provide adequate symptom management. MedicAlert bracelet Provide emotional and psychological support. A big one! (Mosby, 2009; Lupus Society of Canada, 2007)

Case Study Mrs. Sour Hip is a 66 year old female who has suffered from lupus for the past 30 years. Mrs. Sour Hip experiences many joint-related lupus symptoms, particularly in her right hip. She will be undergoing a right hip replacement surgery next week. Her medical history includes systemic lupus erythematosus, HTN, a. fib, pneumonia in winter 2010, and a history of pernicious anemia for which she receives Vitamin B12 s/c q2months. Her medications include long-term corticosteroid therapy to help manage her lupus.
Questions?
References American Academy of Orthopaedic Surgeons. (2012) . Arthritis. Retrieved from http://orthoinfo.aaos.org/menus/arthritis.cfm Arthritis Foundation. (2012). Common Myths. Retrieved from http://www.arthritis.org/aamcommon-myths.php Arthritis Society. (2010). Lupus. Retrieved from http://http://www.arthritis.ca/document.doc? id 327 Arthritis Society. (2011). Osteoarthritis: Know Your Options. Retrieved from http://www.arthritis.ca/document.doc?id 328 Arthritis Society. (2012). About Arthritis. Retrieved from http://www.arthritis.ca/aboutarthritis Canadian Arthritis Network. (2007). Arthritis Facts and Figures. Retrieved from http://www.arthritisnetwork.ca/home/Facts and Figures 2010.pdf Cartilage Health. (2008). What is articular cartilage? Retrieved from http://www.cartilagehealth.com/acr.html Canadian Psychological Association. (2012). Arthritis. Retrieved From http://www.cpa.ca/psychologyfactsheets/arthritis/ Day, R. A., Paul, P., Williams, B., Smeltzer, S. & Bare, B. (2007). Canadian textbook of medical surgical Nursing (1st Canadian Ed.). Philadelphia: Lippincott Williams & Watkins. Firth, J. (2011). Rheumatoid arthritis: diagnosis and multidisciplinary management. Nursing, 20(18), 1179-80.

References cont. Firth, J. (2011). Rheumatoid arthritis: diagnosis and multidisciplinary management. Nursing, 20(18), 1179-80. Gulanick, M. & Myers, J. (2011). Nursing Care Plans: Diagnoses, Interventions, and Outcomes (7th ed.). St.Louis, MO: Elsevier Mosby. John Hopkins Arthritis Center. (2012). Nutrition and Rheumatoid Arthritis. Retrieved from http://www.hopkinsarthritis.org/patient-corner/disease-management/rheumatoid-arthrtis-nutrition/ Lupus Society of Canada. (2007). Lupus Fact Sheet: Takling About Lupus. Retrieved from http://www.lupuscanada.org/pdfs/factsheets/Talk-Online.pdf Lupus Society of Canada. (2012). Living with Lupus: Lupus Overview. Retrieved from http://www.lupuscanada.org/english/living/lupus-overview.html Mosby. (2009). Mosby’s Dictionary of Medicine, Nursing, & Health Professions (8th ed.). St. Louis, MO: Author. Myers, J., Gulanick, M. (2011). Nursing Care Plans (7th ed.). Elsevier National Institute of Arthritis & Musculoskeletal & Skin Diseases. (2010). Handout on Health: Osteoarthritis. Retrieved from http://www.niams.nih.gov/Health Info/Osteoarthritis/default.asp Oliver, S. (2011). The role of the clinical nurse specialist in the assessment and management of biologic therapies. Musculoskeletal Care Journal. 9, 54-62. Sung-Jae, K., Kwang-Am, J. (2007). Arthroscopic Synovectomy in Rheumatoid Arthritis of Wrist. Clinical Medical Research, 5(4), 244-250. Walker, J. (2012). Care of patients undergoing joint replacements, Nursing Older People, 24(1), 14-20. Walker, J. (2011). Management of osteoarthritis. Nursing Older People, 23(9), 14-19.