Working Together Project Adjunct Professor Shane Crowe Executive
25 Slides1.20 MB
Working Together Project Adjunct Professor Shane Crowe Executive Director, Nursing & Midwifery Western Health
Working Together Pilot DH funded pilot project 12-month duration Western Health (14 teams) Northeast Health Wangaratta (7 teams) Independent evaluation by Deakin University 2
Pilot objectives Co-design, trial and evaluate improved nursing and midwifery workload allocation and management practices. Contribute to DH strategic priorities of providing person-centred care, sustainable services, improve workforce availability, capability, collaboration, leadership, wellbeing and engagement.
Pilot principles Adhere to co-design principles when developing strategies Keep within the requirements of The Act and The Agreement Consult key stakeholders Voluntary participation via EOI 4
Our journey Formal communication strategy UM engagement, empowerment, education and support – workshop, project lead Staff engagement – surveys, focus groups, UMs. Identified issues and strategies ANMF engagement Trialing of ideas – PDSA Evaluation 5
Pre-project interview themes Patient allocation ratios – “a blessing and a curse” Concerns about patient safety Difficult to provide high quality patient care Nurses/midwives feel “overworked”/ “burnt out” Patient care needs often missed (e.g. oral hygiene, pressure care 6
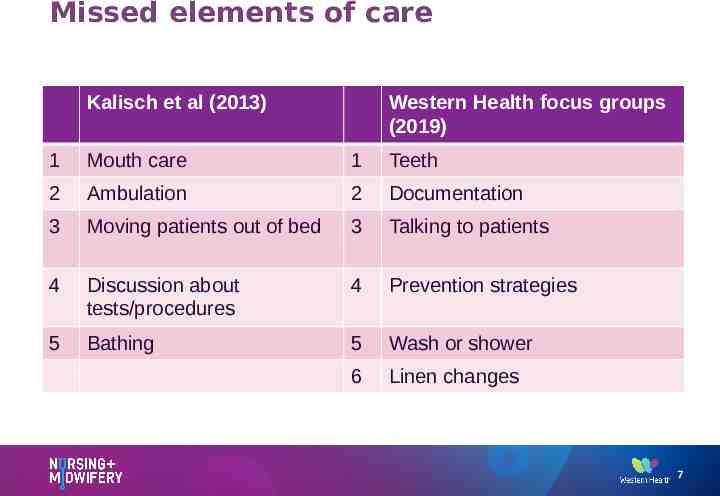
Missed elements of care Kalisch et al (2013) Western Health focus groups (2019) 1 Mouth care 1 Teeth 2 Ambulation 2 Documentation 3 Moving patients out of bed 3 Talking to patients 4 Discussion about tests/procedures 4 Prevention strategies 5 Bathing 5 Wash or shower 6 Linen changes 7
Why Co-design? Intentional Hypothesized that the workforce would feel more supported to choose and develop initiatives Higher chance of success Longer lasting impact and change Increase the likelihood of meeting the needs of nurses and midwives
Methodology - project Formal communication strategy ANMF engagement Focus groups identifying issues and strategies Co-design workshop confirming issues EDONM check-in session Piloting/trialing of strategies Support from project officer ‘Pulse check’ survey 9
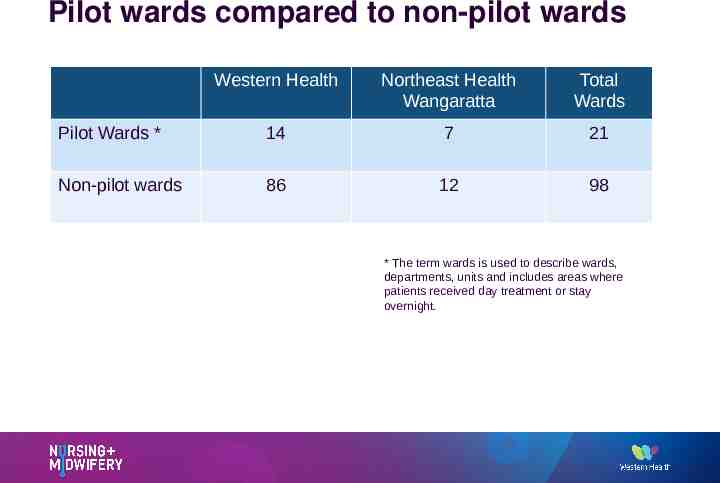
Pilot wards compared to non-pilot wards Western Health Northeast Health Wangaratta Total Wards Pilot Wards * 14 7 21 Non-pilot wards 86 12 98 * The term wards is used to describe wards, departments, units and includes areas where patients received day treatment or stay overnight.
Working Together is like a jigsaw 11
Key ‘border’ pieces Handover Staff allocation and reallocation Team nursing Intra-shift wellbeing checks Ensuring breaks occurred Leaving on time and together Proactive nursing Optimizing use of double staffing time 12
Key ‘middle’ pieces Staff ideas box Knowing who you are working with Standardized in charge shift Consistent use of patient beside communication boards Lean ward Staff wellness initiatives Department/team charter 13
‘Missing’ pieces New & innovative patient discharge solutions Managing tension between discharge time (access) and the nurse/patient plan Nursing & Midwifery lounge area / rest area for beaks sleep chairs Acuity tool to assist with patient allocation 14
Foundation or essential items Handover Staff allocation and reallocation during shift Team nursing In-charge responsibilities Proactive nursing Ideas and suggestion to Unit Managers Leaving on time and together Optimising use of double staffing time Ward meetings Staff wellness initiatives

Examples of ideas In charge led support Ward efficiency Handover AUM rounding & action Safe & tidy ward checks Start of shift intros Allocation model Patient booking system includes staff breaks ISBAR reinforced Leaving on time & together Sleep & rest strategies Team handover pt EMR AUM handover tool Code of conduct Team support Leader led support Uncategorized Informal debriefing and huddles Frequent ward meetings Bathroom toiletries Enhancing team Ideas boards/box Celebrating with food Staff identification methods Rotations ceased 16
Lessons learnt Co-design methodology works Reinforce nurse-led and midwife-led solutions Leadership was critical Time for staff to define what matters to them Don’t compromise the outcome to meet a timeline Collaborate and partner with others for expertise Changing long-held views - allow time for implementation and evaluation 17
Evaluation - methods Aim: To determine if the objectives of the project were achieved and inform decisions about expanding the project to other health services. Mixed methods (qualitative and quantitative) Data audit of key measures (Quantitative data) Pre and post implementation surveys (Quantitative data) Pre and post implementation interviews (Qualitative data)
Evaluation scope Time period - March 2019 to September 2020 Component 1: Data audit Components 2 & 3: Surveys & interviews Nurses/Midwives employed at WH & NHW Invited to complete survey and/or interview Prior and after implementation
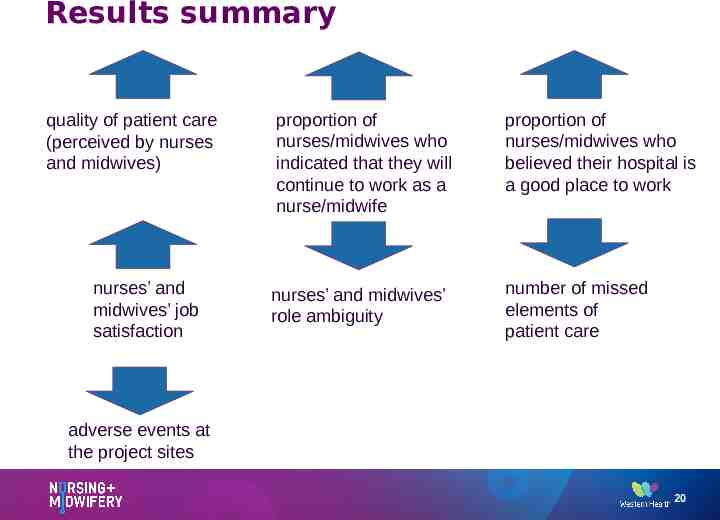
Results summary quality of patient care (perceived by nurses and midwives) nurses’ and midwives’ job satisfaction proportion of nurses/midwives who indicated that they will continue to work as a nurse/midwife proportion of nurses/midwives who believed their hospital is a good place to work nurses’ and midwives’ role ambiguity number of missed elements of patient care adverse events at the project sites 20
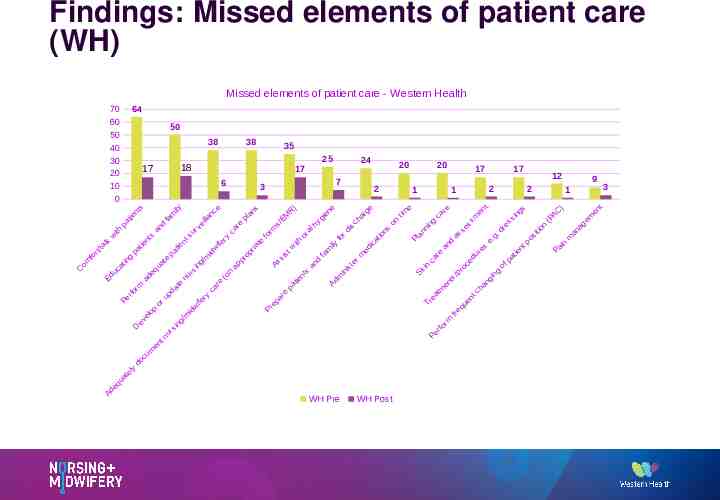
Findings: Missed elements of patient care (WH) Missed elements of patient care - Western Health 64 70 60 50 40 30 20 10 0 C om fo r t/ t k al w 50 38 p a g tin nt pa r fo Pe e at qu ly s tie rm D e Ad 25 s nt an eq ad ev op el cu do m d ua or fa te m tie pa d up tn en ily ur n e at ng si u ts n 24 17 6 ie at 35 18 17 ith uc Ed 38 rv s ur nc lla ei g in w id /m if /m y er 3 e w id ca ife re ry ( 7 ca on re p ap s an pl p ro ria te fo rm s M /E As ep Pr st si e ar R ) w ith or al s nt tie a p h an ne ie g y d m fa ily r fo 20 2 s di t is in m Ad ar ch e rm ic ed s on tim e an Pl ng ni in Sk c ca e ar t ea a nd e fo as s nt rm 12 2 re m r Pe WH Post 17 1 Tr WH Pre 17 1 ge n io at 20 se r /p fr e m ss oc q e en r du c nt ue t es ha e re .d g . g in ng 9 2 o gs in s s at fp n ie t s po 3 1 itio n AC (P ) in Pa an m a m ge en t
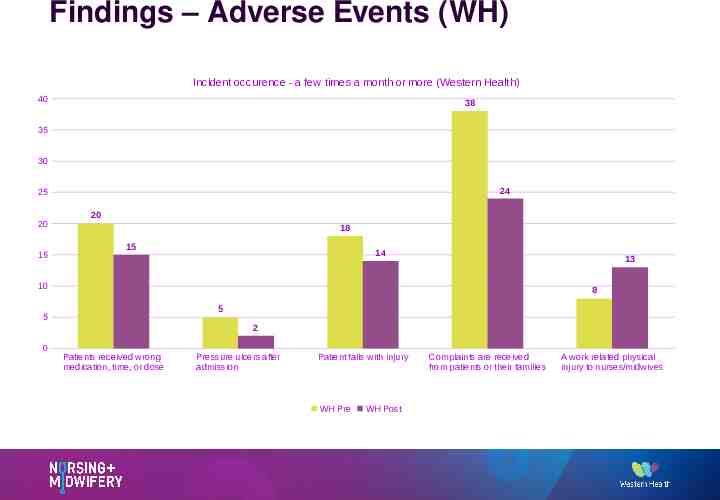
Findings – Adverse Events (WH) Incident occurence - a few times a month or more (Western Health) 40 38 35 30 24 25 20 15 20 18 15 14 13 10 8 5 5 2 0 Patients received wrong medication, time, or dose Pressure ulcers after admission Patient falls with injury WH Pre WH Post Complaints are received from patients or their families A work related physical injury to nurses/midwives
Limitations Project timeline (12 month duration) Complicating factors: o Effects of Bushfires (Dec 2019-Feb 2020) o Impact of COVID-19 pandemic (FebOctober 2020) 23
What's happening now? Concluded the ‘pilot’ Evaluation report submitted to DH Planning for WH wide roll out Co-design methodology perceived as positive ‘Working Together’ to understand and solve problems Will be encompassed in Western Health’s nursing and midwifery model of care Co-design principles embedded into future practice changes 24
Reading list 1. Bloom, S.L. & Farragher, B. (2013). Restoring Sanctuary. A new operating system for trauma-informed systems of care. Oxford: Oxford University Press. 2. Brasaite, I., Kaunonen, M. & Suominen, T. (2015). Healthcare professionals'’ knowledge, attitudes and skills regarding patient safety: a systematic literature review. Scandinavian Journal of Caring Sciences, 29(1), 30-50. 3. Havaei, F., MacPhee, M., & Dahinten, V.S. (2016). RNs and LPNs: emotional exhaustion and intention to leave. Journal of Nursing Management, 24(3), 393-399. 4. Kaiser, J.A. & Westers, J.B. (2018). Nursing Teamwork in a health system: A multisite study. Journal of Nursing Management, 26(5), 555-562. 5. Kalisch B.,J., Landstrom G.L. & Hinshaw, A.S (2009). Missed nursing care: A concept analysis. Journal of Advanced Nursing, 65(7),1509–1517. 6. Kalisch, B.J., Xie, B. & Dabney, B.W. (2013). Patient-reported missed nursing care correlated with adverse events. American Journal of Medical Quality, 29(5), 393-399. 7. Martin, A., Shann, C & LaMontagne, A. (2017). What works to promote workplace wellbeing? A rapid review of recent policy developments and intervention research. Retrieved from http://leadingwellvic.com.au/app/uploads/2018/02/What-Works-to-Promote-Workplace-Wellbeing.pdf 8. Nugus, P., Greenfield, D., Travaglia, J., Westbrook, J,. & Braithwaite, J. (2010). How and where clinicians exercise power: Interprofessional relations in health care. Social science & medicine (1982)71, 898-909. 9. Riskin, A. Erez, A, Foulk, T.A., Kugelman, A., Gover, A., Shoris, I., Riskin, K.S. , & Bamberger, P.A. (2015). The impact of rudeness on medical team performance: A randomised trial. Pediatrics, 136(3), 487-495 10. Ünver, G.T., & Seren, A.K.H. (2018). Defining the patient safety attitudes and influencing factors of health professionals working at maternity hospitals. Journal of Nursing Management, 26(5), 579–586. 11. Uttriainen, K., Ala-Mursula, L., & Kyngas, H. (2015). Hospital nurses’ wellbeing at work: a theoretical model. Journal of Nursing Management, 23(6),736-743. 25