The current policy environment for occupational health Nick Pahl, CEO
30 Slides1.16 MB

The current policy environment for occupational health Nick Pahl, CEO
Contents 1 Current Issues 2 Recent Reports, Infographics, Reports and Policy activity 3 Green Paper on Work/ Health and Disability 4 Role of Occupational Health 5 Questions 6 Vision for the future

1 Current Issues
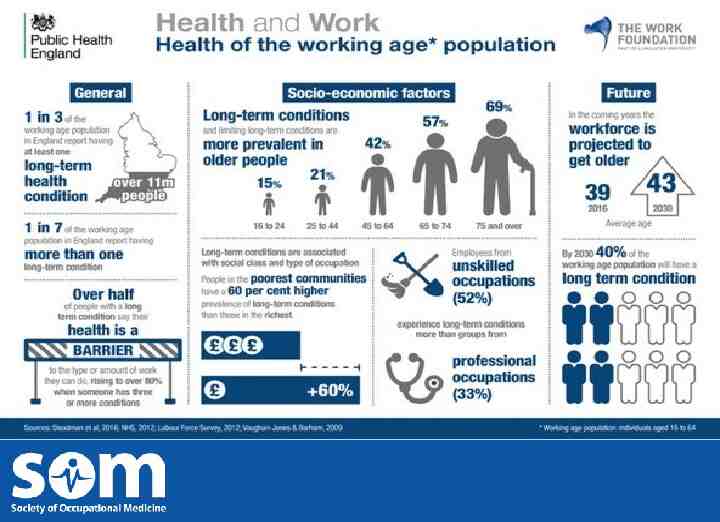
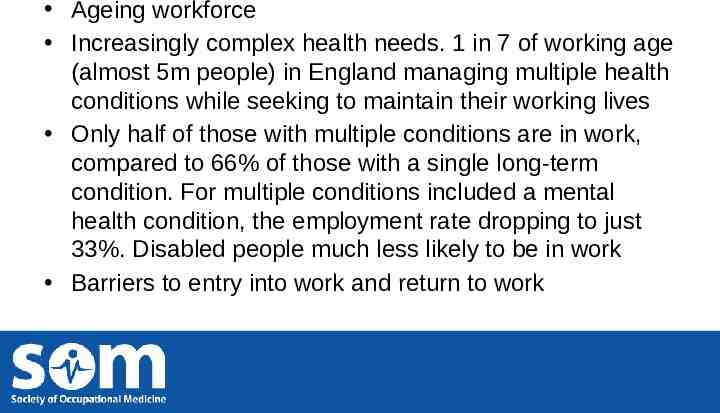
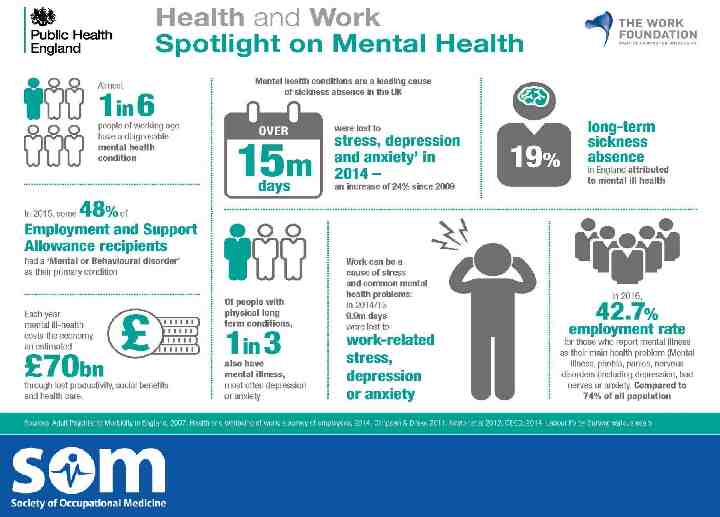
Ageing workforce Increasingly complex health needs. 1 in 7 of working age (almost 5m people) in England managing multiple health conditions while seeking to maintain their working lives Only half of those with multiple conditions are in work, compared to 66% of those with a single long-term condition. For multiple conditions included a mental health condition, the employment rate dropping to just 33%. Disabled people much less likely to be in work Barriers to entry into work and return to work
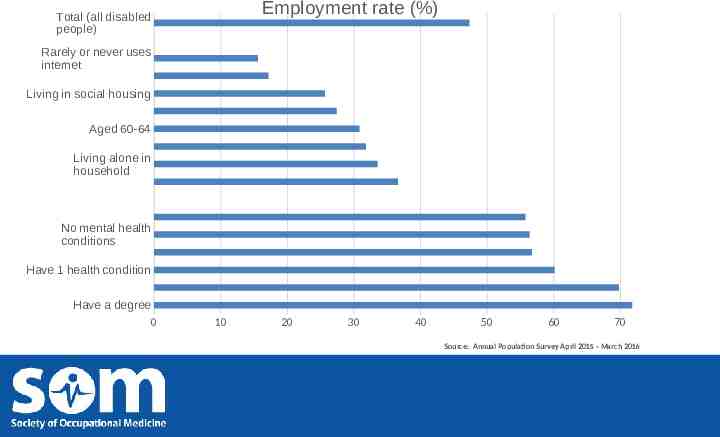
Employment rate (%) Total (all disabled people) Rarely or never uses internet Living in social housing Aged 60-64 Living alone in household No mental health conditions Have 1 health condition Have a degree 0 10 20 30 40 50 60 70 Source: Annual Population Survey April 2015 - March 2016
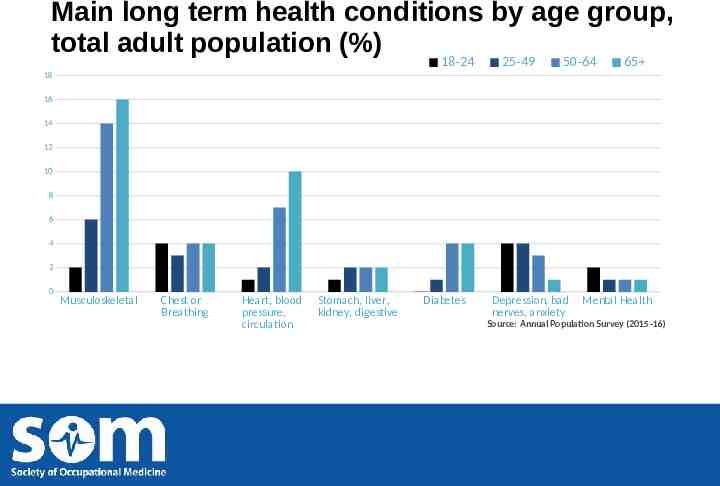
Main long term health conditions by age group, total adult population (%) 18-24 25-49 50-64 65 18 16 14 12 10 8 6 4 2 0 Musculoskeletal Chest or Breathing Heart, blood pressure, circulation Stomach, liver, kidney, digestive Diabetes Depression, bad nerves, anxiety Mental Health Source: Annual Population Survey (2015-16)
Cancer Cancer survivors are 1.4 times more likely to be unemployed than general population 65% of cancer survivors think it’s important to continue to work Key issues – reasonable adjustments, coping at work, discrimination and unhelpful and unsympathetic employers Materials from Macmillan available (stand 70)
Occupational health and medicine Significant gaps in provision of occupational health – particularly for small business Training posts for specialist occupational physicians are at an all-time low, down from 216 in 2002 to just 74 in 2015. Ageing specialty; 64% of all doctors working in occupational medicine are aged 50 or over, and half of all specialists could retire within a decade.
2 Recent reports/ toolkits / info graphics / guidance and Policy Activity
Reports / toolkits / info graphics MSK - Employer toolkit - BITC/ ARMA/PHE Health and Safety Executive – new health strategy focus on work-related stress, MSK PHE – infographics Ageing – infographic - Centre for Ageing

Reports Health, work and worklessness - Local Government Association Inequality in Access to Quality Work – Carnegie Foundation Arthritis in the workplace – Arthritis Research UK Retention - Resolution Foundation Disability and employment - Cardiff University Social Prescribing/ MS/ working with multiple health conditions – Work Foundation Reducing long term sickness absence - IPRR
Quality standards / advice . Healthy workplaces: improving employee mental and physical health and wellbeing – NICE quality standard Advice on the menopause - FOM

Coming up. Devolving spend 2017 e.g. to London Independent Review of Employment Practices in the Modern Economy - commissioned by the PM Oct 2016. Matthew Taylor (the Chief Executive of the Royal Society of the Arts) taking forward. PM also asked CEO of MIND and Lord Stevenson to look at mental health in the workplace NHS England publication on Hearing loss in workplace Centre for Social Justice report – end of this month What Works Centre for Wellbeing Strategic Council
3 Green Paper on Work, health and disability
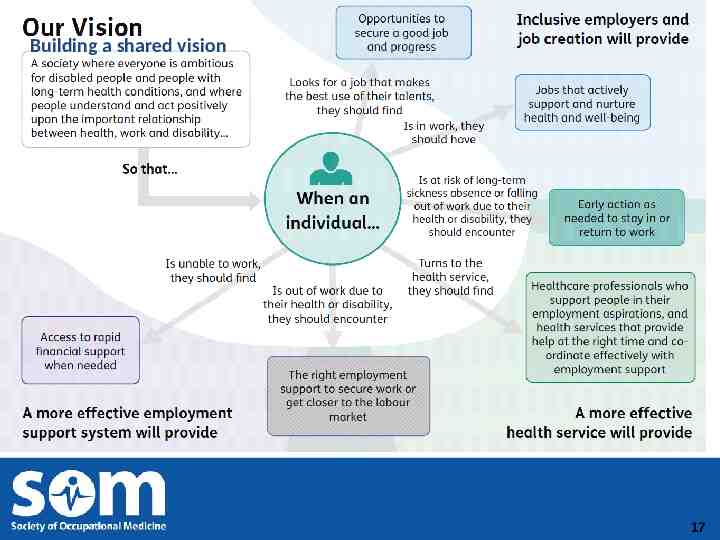
Building a shared vision 17
Action occurring already New personal support within Jobcentre Plus Investment in skills and capabilities for work coaches to help people with disabilities Reform of the Work Capability Assessment, including separating decisions on financial support and employment support Further improvements to simplify the assessment process for a small proportion of claimants with the most severe, life-long conditions
Questions in Green Paper Should other health professionals be able to issue fit notes? If so, who and what qualifications / training would we expect them to undertake? Can the fit for work service be improved – or does something very different need to replace it? How can occupational health and medicine professionals be part of the solution?
Green Paper on work, health and disability – SOM involvement Parliamentary roundtable hosted by SOM Patron, Lord Blunkett - November SOM/FOM Consultation event for 70 health professionals in York – January SOM/FOM Submission to DWP/DH unit - February Campaign to increase understanding health and work: http://www.whyoccupationalhealth.co.uk/content/why-occ upational-health/
Concerns target is over – ambitious. On current trends it will take to 2065 to close the gap! assumes the UK economy can deliver these jobs, and disabled people can access these jobs. employers, particularly small employers, need to get the right support at the right time. workforce capacity of occupational health professionals need to be expanded to deliver the new occupational health models that are required.
4 Occupational Health
Occupational health professionals have unique training, expertise and perspective to understand the link between health and work; as well as how to help injured, ill and ageing workers remain productive and at work. provide preventive services for the entire workforce; support services for individual employees; and competent professional support to management. help employers to ensure a healthy workplace culture and properly organised and healthy work.

Role of occupational health individuals need conversations with trusted health professionals who understand their medical needs, which may be complex, and can refer to a range of support services; medical and non-medical employers need direct, individualised and concise advice on how to support disabled people and people with longterm health conditions in the workplace OH professionals are ideally placed to ‘join-up’ service access and advice between individuals, their health care professionals and their employers
Occupational health – the evidence base Evidence demonstrates that there is a rounded business case for investment in occupational health services Well-integrated and supported workplace health initiatives improve employee health and productivity Research supports the proposition that investments in occupational health add value through reduced costs associated with the prevention of ill health, improved productivity and a range of intangible benefits. Employers state the reasons they provide occupational health service are: Financial – to reduce costs or add value to the business Legal – to comply with health and safety laws and regulations Moral – it is the right/ethical/socially responsible thing to do
Occupational health awareness and training Need pool of well trained and competent OH professionals e.g. in each CCG OH needs to be added into the undergraduate curriculum for health, education and social care professionals and other specialist curriculums
Vision for the future
Work in 2030 Preventive approaches that help people stay in work and stay well Greater flexibility in where, when and how we work When people do develop health conditions, both employers and health professionals do much more to help them stay in touch with work, and identify the adaptations they might need to return .not everyone will be able to stay in work – and that sometimes it will be best for them to stop. benefits system needs to support people in this situation

SAVE THE DATE 26TH - 28TH June 2017 Come and join us at the NEW multi- for all Occupational Health Professionals in the fantastic location of Leeds
Questions? [email protected]