Survival Guide for Long-Term Care Providers Update Since SB
43 Slides883.00 KB
Survival Guide for Long-Term Care Providers Update Since SB 1202 Presentation by the Agency for Health Care Administration September/October 2002 Agency for Health Care Administration Division of Managed Care & Health Quality
Updates & Recent Activities SB 1202 Questions & Answers – Adverse Incidents Liability Claims and Insurance 2002 Legislative Changes Nursing Home Staffing Alzheimer’s Training Gold Seal Program Agency for Health Care Administration Division of Managed Care & Health Quality
New Slides Blue Background Underlined Text Added to Presentation Not in Handout Post on AHCA Web Site Agency for Health Care Administration Division of Managed Care & Health Quality
SB 1202 Emphasis on Adverse Incidents Asked Quality of Care Monitors Definition of Adverse Incidents Questions and Answers Published: February 2002 May 2002 Agency for Health Care Administration Division of Managed Care & Health Quality
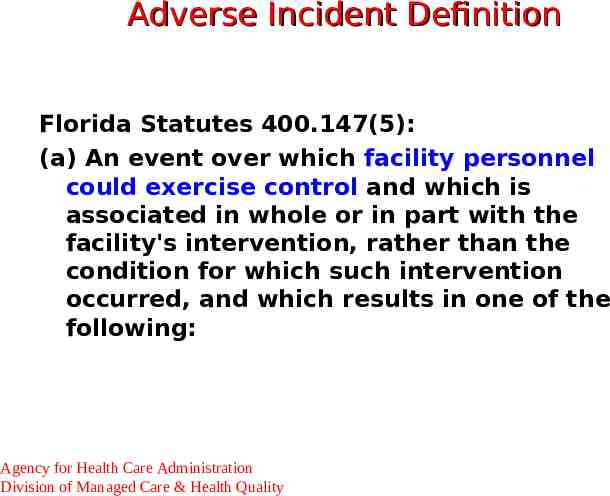
Adverse Incident Definition Florida Statutes 400.147(5): (a) An event over which facility personnel could exercise control and which is associated in whole or in part with the facility's intervention, rather than the condition for which such intervention occurred, and which results in one of the following: Agency for Health Care Administration Division of Managed Care & Health Quality
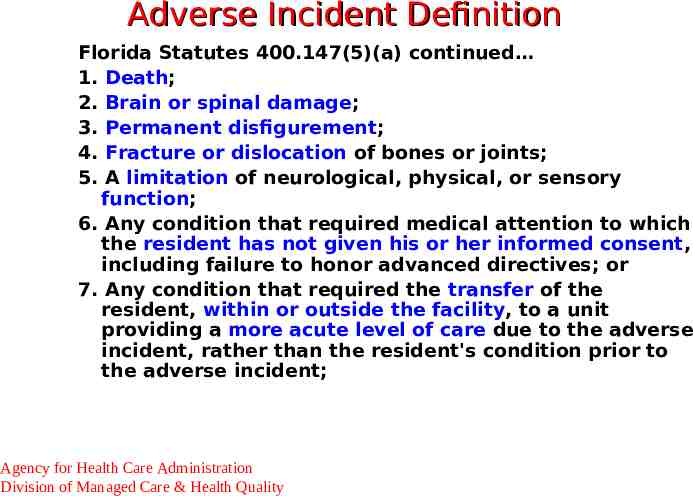
Adverse Incident Definition Florida Statutes 400.147(5)(a) continued 1. Death; 2. Brain or spinal damage; 3. Permanent disfigurement; 4. Fracture or dislocation of bones or joints; 5. A limitation of neurological, physical, or sensory function; 6. Any condition that required medical attention to which the resident has not given his or her informed consent, including failure to honor advanced directives; or 7. Any condition that required the transfer of the resident, within or outside the facility, to a unit providing a more acute level of care due to the adverse incident, rather than the resident's condition prior to the adverse incident; Agency for Health Care Administration Division of Managed Care & Health Quality
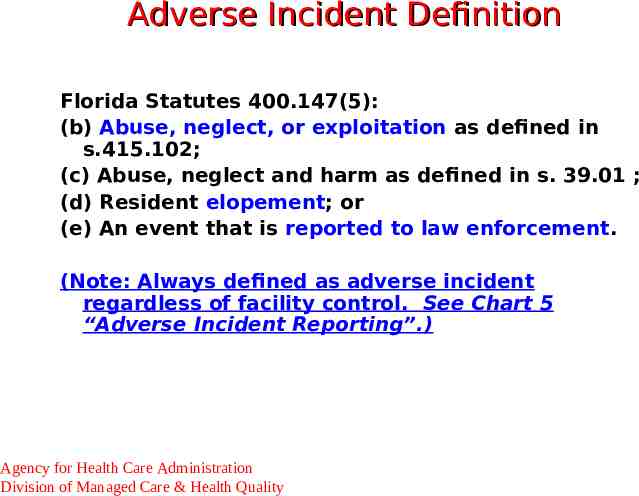
Adverse Incident Definition Florida Statutes 400.147(5): (b) Abuse, neglect, or exploitation as defined in s.415.102; (c) Abuse, neglect and harm as defined in s. 39.01 ; (d) Resident elopement; or (e) An event that is reported to law enforcement. (Note: Always defined as adverse incident regardless of facility control. See Chart 5 “Adverse Incident Reporting”.) Agency for Health Care Administration Division of Managed Care & Health Quality
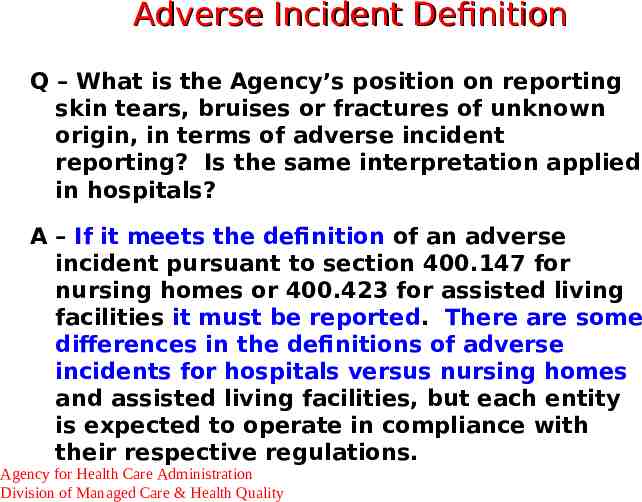
Adverse Incident Definition Q – What is the Agency’s position on reporting skin tears, bruises or fractures of unknown origin, in terms of adverse incident reporting? Is the same interpretation applied in hospitals? A – If it meets the definition of an adverse incident pursuant to section 400.147 for nursing homes or 400.423 for assisted living facilities it must be reported. There are some differences in the definitions of adverse incidents for hospitals versus nursing homes and assisted living facilities, but each entity is expected to operate in compliance with their respective regulations. Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incident - Elopement Q - How is “elopement” defined for the purposes of adverse incident reporting? A - Elopement is when a resident leaves the facility without following facility policies and procedures for signing out. Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incidents – Baker Act Q – Baker Act referrals and risk management reporting requirements: Does a facility have to report a call for law enforcement transportation as an adverse incident? Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incidents – Baker Act A – Events reported to law enforcement for investigation are considered adverse incidents pursuant to sections 400.147(5)(e), F.S. A call to law enforcement for something other than investigation, e.g.: transportation only, would not alone meet the definition of an adverse incident. However, a Baker Act situation must be reviewed independently to determine if it meets one of the definitions of an adverse incident. Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incident Reporting Q – If, prior to the required report date, facility staff determine that an incident does not meet the definition of an adverse incident as specified in statute, is a report to the Agency still required? Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incident Reporting A – Only those incidents that meet the definition of an Adverse Incident must be reported to the Agency. If the facility is able to determine that the incident does not meet the definition, prior to the required report date, then a report is not required. However, if the facility has not yet determined if the incident meets the adverse incident definition the incident must be reported on the 1-Day report. After the facility investigation is complete and if it is determined that the incident does not meet the definition of an adverse incident, then the facility staff may report on the 15-Day report that the incident was determined not to be an adverse incident. Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incident Report Q – What should a facility provide in the adverse incident report? A - All the questions on the Adverse Incident Report forms should be answered. The description of the incident should include answers to basic questions like Who, What, Where, When, Why, allows AHCA reviewers to determine appropriate action. Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incident Confidentiality Q – Are a facility’s risk management and quality assurance records protected from public disclosure once they are sent to the Agency, such as with a plan of correction? A – All documents received by the agency are considered public records unless there is a specific public record exemption in law. Only the adverse incident reports themselves are protected from public record. Any documents submitted with a plan of correction are not protected from public disclosure, however, resident unique identifying information remains protected and redacted from documents prior to the release of the records. Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incident Confidentiality Adverse Incident Reports (1-Day and 15Day) are Exempt from Public Disclosure The 5-Day Report of the Status of an Abuse, Neglect or Exploitation Not Specifically Exempt from Public Disclosure Accept the 15-Day Report by the 5th Day to Meet Federal 5-Day Requirement Agency for Health Care Administration Division of Managed Care & Health Quality
Adverse Incidents Role of Risk Management Process – Identification of Incidents – Affect Compliance with Regulations Role of Quality-of-Care Monitor – Risk Management Program – Adverse Incident Identification Role in the Survey Process – Regulatory Compliance Related to Occurrences – Current Non-Compliance Except Egregious Agency for Health Care Administration Division of Managed Care & Health Quality
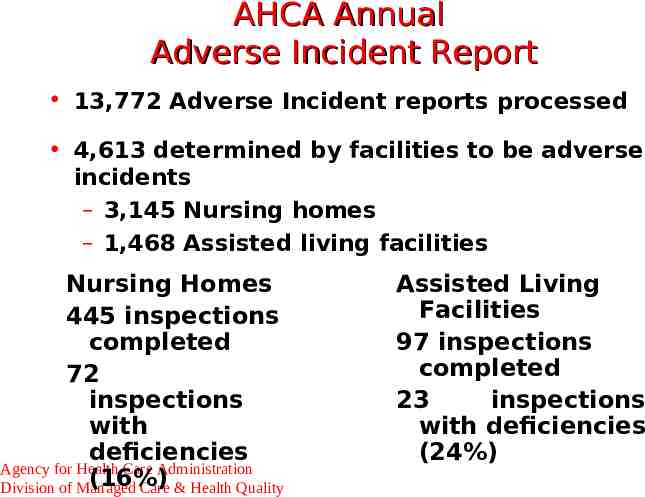
AHCA Annual Adverse Incident Report 13,772 Adverse Incident reports processed 4,613 determined by facilities to be adverse incidents – 3,145 Nursing homes – 1,468 Assisted living facilities Nursing Homes 445 inspections completed 72 inspections with deficiencies Agency for Health Care Administration (16%) Division of Managed Care & Health Quality Assisted Living Facilities 97 inspections completed 23 inspections with deficiencies (24%)
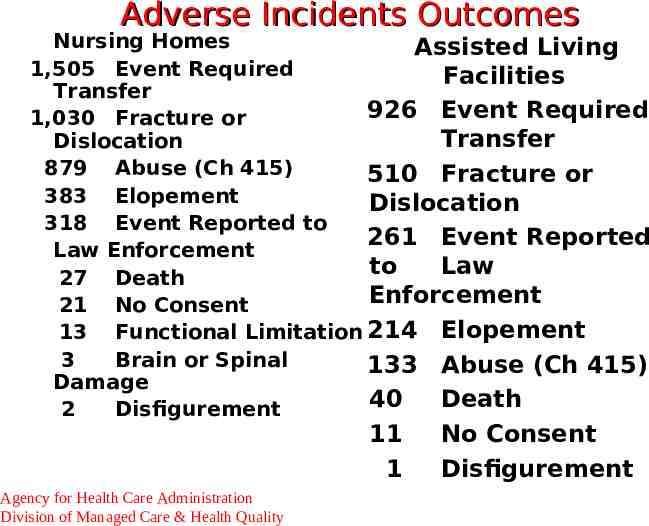
Adverse Incidents Outcomes Nursing Homes Assisted Living 1,505 Event Required Facilities Transfer 926 Event Required 1,030 Fracture or Transfer Dislocation 879 Abuse (Ch 415) 510 Fracture or 383 Elopement Dislocation 318 Event Reported to 261 Event Reported Law Enforcement to Law 27 Death Enforcement 21 No Consent 13 Functional Limitation 214 Elopement 3 Brain or Spinal 133 Abuse (Ch 415) Damage 40 Death 2 Disfigurement 11 1 Agency for Health Care Administration Division of Managed Care & Health Quality No Consent Disfigurement
Practitioner Review Medical Quality Assurance Investigates Practitioners for Violations of Practice Acts Review All Adverse Incident Reports Practitioners Being Investigated Receive a Copy of the Adverse Incident Report – Other Staff Names are Removed Agency for Health Care Administration Division of Managed Care & Health Quality
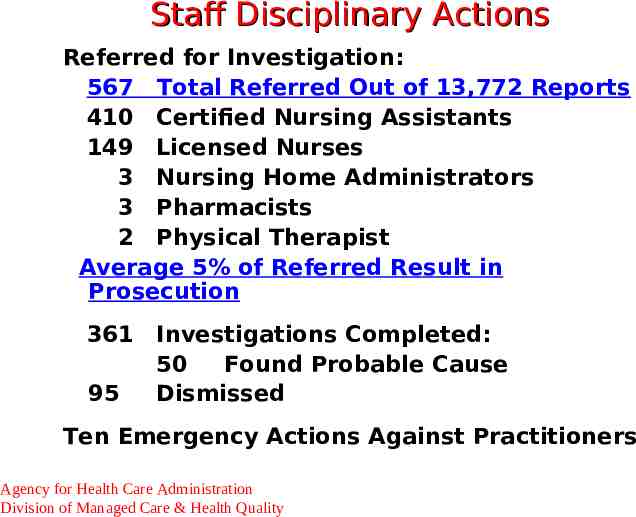
Staff Disciplinary Actions Referred for Investigation: 567 Total Referred Out of 13,772 Reports 410 Certified Nursing Assistants 149 Licensed Nurses 3 Nursing Home Administrators 3 Pharmacists 2 Physical Therapist Average 5% of Referred Result in Prosecution 361 Investigations Completed: 50 Found Probable Cause 95 Dismissed Ten Emergency Actions Against Practitioners Agency for Health Care Administration Division of Managed Care & Health Quality
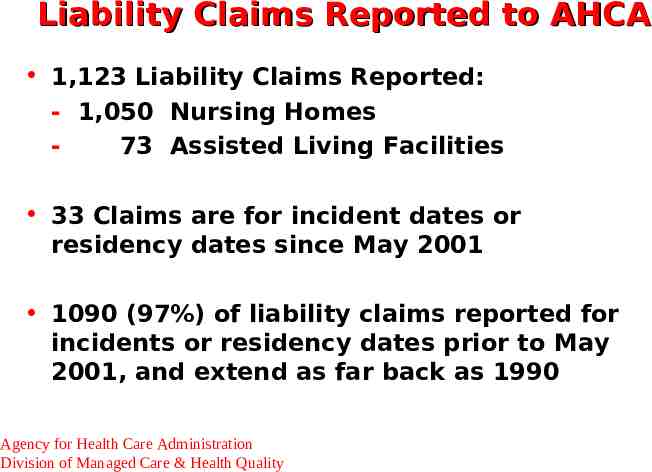
Liability Claims Reported to AHCA 1,123 Liability Claims Reported: - 1,050 Nursing Homes 73 Assisted Living Facilities 33 Claims are for incident dates or residency dates since May 2001 1090 (97%) of liability claims reported for incidents or residency dates prior to May 2001, and extend as far back as 1990 Agency for Health Care Administration Division of Managed Care & Health Quality
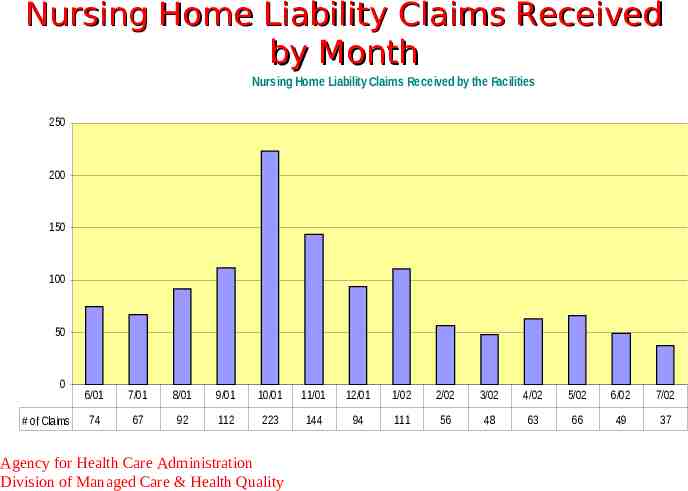
Nursing Home Liability Claims Received by Month Nursing Home Liability Claims Received by the Facilities 250 200 150 100 50 0 # of Claims 6/01 7/01 8/01 9/01 10/01 11/01 12/01 1/02 2/02 3/02 4/02 5/02 6/02 7/02 74 67 92 112 223 144 94 111 56 48 63 66 49 37 Agency for Health Care Administration Division of Managed Care & Health Quality

Top Reasons for Claims Reported Nursing Homes: Assisted Living: 260 Other 159 Death 133 Fracture 89 Abuse 75 Transfer Involved 13 Other 13 Fracture 12 Death 10 Transfer Involved 4 Abuse Other for Nursing Homes: Pressure Sores, Illness (Pneumonia, UTI), Falls, Weight Loss (non-terminal residents), Restraints, Unnecessary Medications Agency for Health Care Administration Division of Managed Care & Health Quality
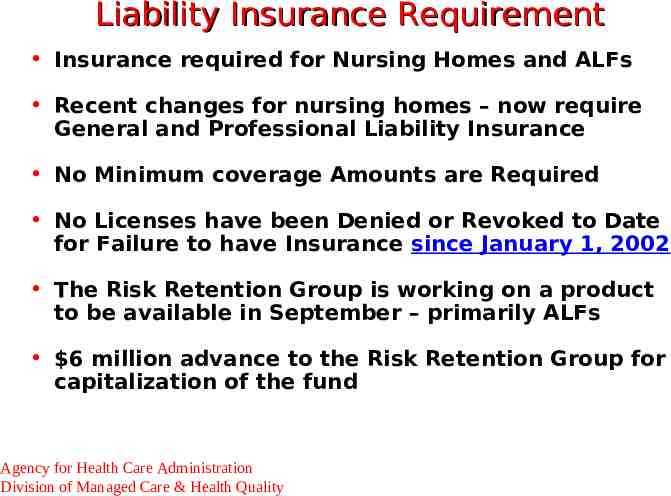
Liability Insurance Requirement Insurance required for Nursing Homes and ALFs Recent changes for nursing homes – now require General and Professional Liability Insurance No Minimum coverage Amounts are Required No Licenses have been Denied or Revoked to Date for Failure to have Insurance since January 1, 2002 The Risk Retention Group is working on a product to be available in September – primarily ALFs 6 million advance to the Risk Retention Group for capitalization of the fund Agency for Health Care Administration Division of Managed Care & Health Quality
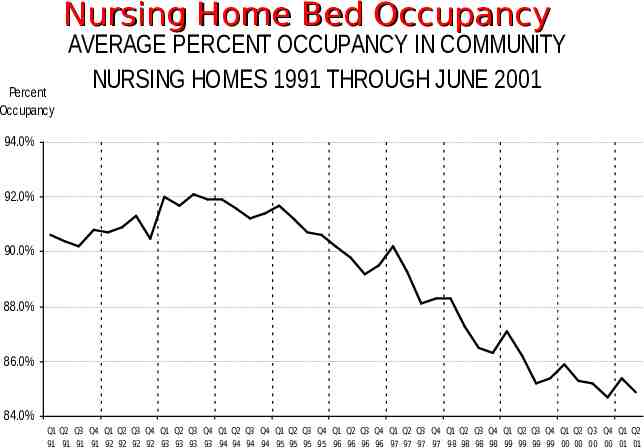
Nursing Home Bed Occupancy Percent Occupancy AVERAGE PERCENT OCCUPANCY IN COMMUNITY NURSING HOMES 1991 THROUGH JUNE 2001 94.0% 92.0% 90.0% 88.0% 86.0% 84.0% Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 91 91 91 91 92 92 92 92 93 93 93 93 94 94 94 94 95 95 95 95 96 96 96 96 97 97 97 97 98 98 98 98 99 99 99 99 00 00 00 00 01 01
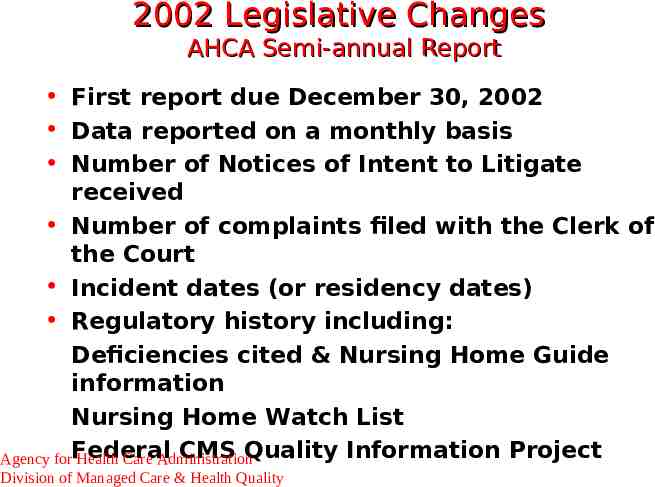
2002 Legislative Changes AHCA Semi-annual Report First report due December 30, 2002 Data reported on a monthly basis Number of Notices of Intent to Litigate received Number of complaints filed with the Clerk of the Court Incident dates (or residency dates) Regulatory history including: Deficiencies cited & Nursing Home Guide information Nursing Home Watch List CMS Quality Information Project Agency forFederal Health Care Administration Division of Managed Care & Health Quality
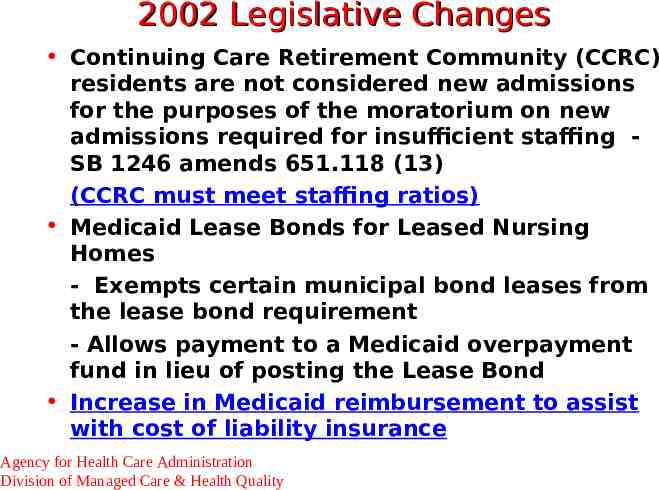
2002 Legislative Changes Continuing Care Retirement Community (CCRC) residents are not considered new admissions for the purposes of the moratorium on new admissions required for insufficient staffing SB 1246 amends 651.118 (13) (CCRC must meet staffing ratios) Medicaid Lease Bonds for Leased Nursing Homes - Exempts certain municipal bond leases from the lease bond requirement - Allows payment to a Medicaid overpayment fund in lieu of posting the Lease Bond Increase in Medicaid reimbursement to assist with cost of liability insurance Agency for Health Care Administration Division of Managed Care & Health Quality
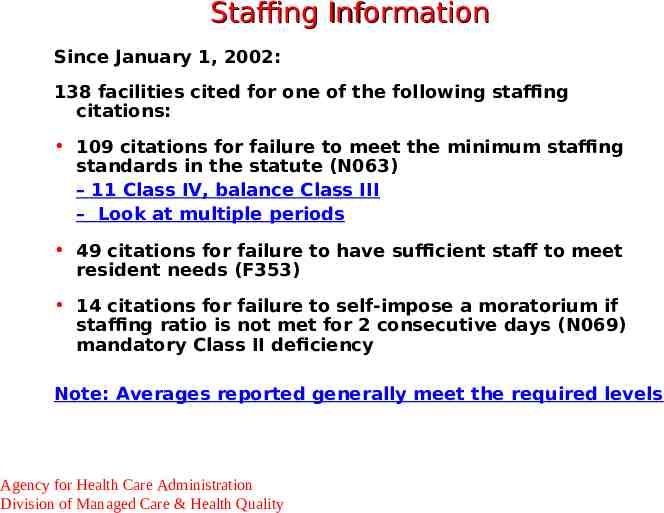
Staffing Information Since January 1, 2002: 138 facilities cited for one of the following staffing citations: 109 citations for failure to meet the minimum staffing standards in the statute (N063) – 11 Class IV, balance Class III – Look at multiple periods 49 citations for failure to have sufficient staff to meet resident needs (F353) 14 citations for failure to self-impose a moratorium if staffing ratio is not met for 2 consecutive days (N069) mandatory Class II deficiency Note: Averages reported generally meet the required levels Agency for Health Care Administration Division of Managed Care & Health Quality
Report Staffing Information Nursing Homes AHCA collects semi-annual reporting of staff ratios, turnover and stability Next report: - Will be sent to all facilities in September, 2002 - Due October 20, 2002 - Anticipate on-line submission of staffing reports and monthly bed vacancy by October, 2002 Centers for Medicare and Medicaid Services (CMS) also posts staffing data on Nursing Home Compare - From the CMS 671 form (provider completes during annual survey) Agency for Health Care Administration Division of Managed Care & Health Quality
Nursing Home Information Know What Others See About Your Facility Reconcile Information – IDR Online – Federal and State Public File Public Information Office (850) 4146044 Agency for Health Care Administration Division of Managed Care & Health Quality
Alzheimer’s Disease Training Department of Elder Affairs Rule is finalized, mailed to nursing homes in May - 58A-4.001(2), F.A.C. http://elderaffairs.state.fl.us/doea/mark.html (see Nursing Home Alzheimer’s Training) Nursing Home Training Provider Certification and Curriculum Approval maintained by the Florida Policy Exchange Center on Aging at USF at www.fpeca.usf.edu Recent Questions and Answers from the Department of Elder Affairs – Attached Teaching Nursing Home – CD-ROM Alzheimer’s Training for LPNs – Contact LTC Unit – Richard Kelly Agency for Health Care Administration Division of Managed Care & Health Quality

Legal Activity Conditional Licenses Fines for Deficiencies Late Fines Fine for Failure to Report Monthly Bed Vacancy Adhere to Timeframes Informal Hearing 40 Facilities Eligible for a 6-month Survey Cycle Agency for Health Care Administration Division of Managed Care & Health Quality

Other Legislative Updates Medicaid Up or Out Monitor Facilities with Lowest NH Guide Scores Improve or Terminate from Medicaid Funding Cut Consumer Satisfaction Survey Resident Interviews and Family Questionnaire Tool & Survey Questions in Rule 59A-4 Unable to Secure Contractor Funding Cut AHCA Still Required to Conduct Survey Gold Seal and Nursing Home Guide Agency for Health Care Administration Division of Managed Care & Health Quality

Gold Seal Award Recipients River Garden Hebrew Home for the Aged, Jacksonville The Pavilion for Health Care, Penney Farms John Knox Village Medical Center, Tampa Florida Presbyterian Homes, Lakeland Memorial Manor, Pembroke Pines Menorah Manor, St. Petersburg Presentation made by Lt. Governor Brogan on July 24, 2002 Agency for Health Care Administration Division of Managed Care & Health Quality

Gold Seal Criteria Facility Must Be Licensed For 30 Months Quality of Care Standards: Consider Past 30 Months Top 25% In Quality of Care Rank (LTC Unit Contact – Richard Kelly) No Conditional Licenses No Class I or II Deficiencies Free of Bankruptcy Proceedings For 30 Months (Including Agency for Health CarePast Administration Division of Managed Care & Health Quality Parent Company)

Gold Seal Financial Criteria Meet a Combination of Financial Thresholds over Past Three Years: Positive Current Ratio of At Least One [current assets (due in 1 year) greater than current liabilities (cash equivalent within 1 year)] Positive Tangible Net Worth (total assets exceed total liabilities) Time Interest Earned Ratio of At Least 115% (profit margin is at least 15% of the interest expense) Agency for Health Care Administration Division of Managed Care & Health Quality
Gold Seal Financial Criteria Note: candidates must submit audited financial statements and a one-year set of pro-forma financial statements and meet two of three thresholds on the pro-forma and a) Two of three financial thresholds for two of the three most recent years (one of which must be the most recent year), or b) All three thresholds for the most recent year Agency for Health Care Administration Division of Managed Care & Health Quality
Gold Seal Criteria Staff Stability Turnover Rate of Not More Than 85% A Stability Rate of At Least 50% Evidence of Efforts To Maintain Stable Workforce Outstanding Ombudsman Complaint History Evidence of Family And Community Involvement Targeted In-Service Training Programs Agency for Health Care Administration See Statute 400.235 Division of Managed Care & Health Quality and rule 59A-4 for
Gold Seal Process Applications received (minimum of five) Staff review for regulatory then financial criteria Ombudsman review Initial Panel review and site visit selection Site visits conducted Final Panel review, site visit reports, facility presentations, and decision regarding recommendation to Governor Final decision by Governor Gold Seal Awards presented Agency for Health Care Administration Division of Managed Care & Health Quality
Current Gold Seal Reviews Meeting July 26 in Tampa Four Facilities Recommended Governor’s Decision Agency for Health Care Administration Division of Managed Care & Health Quality

Gold Seal Benefits Facility Marketing Agency’s NH Guide Web-site and in the Next Hard-copy Publication Public Inquiries –Legislative Future Benefits Nursing Home Licenses Gold Seal Facility Best Practices Request an Extended Survey Cycle Agency for Health Care Administration Division of Managed Care & Health Quality
Resources AHCA Web Site: www.fdhc.state.fl.us AHCA Annual Report on Adverse Incidents Gold Seal Applications Licensure Applications and Forms Nursing Home Guide Nursing Home Watch Lists Florida Health Stats – Locate Facilities/Providers Long-Term Care Unit (850) 488-5861 Agency for Health Care Administration Division of Managed Care & Health Quality