Module 5: Management of Hypertension in Nondiabetes Patients with
51 Slides943.00 KB
Module 5: Management of Hypertension in Nondiabetes Patients with Chronic Kidney Disease This program meets the accreditation criteria of The College of Family Physicians of Canada and has been accredited for up to 1.0 Mainpro-M1 credits. 1
Case Development & Disclosures Case Author: Sheldon W. Tobe Associate Professor of Medicine, Sunnybrook Health Sciences Centre, University of Toronto Specialty: Nephrology Additional Contributor: Marcel Ruzicka, MD, PhD, FRCPC Assistant Professor, University of Ottawa Director of Renal Hypertension Program, Division of Nephrology, The Ottawa Hospital Continuing Education Committee Sol Stern, MD MCFP David Dannenbaum, MD CCFP John Hickey MD, CCFP Karen Mann, BN, MSc, PhD Case Series Editor: Sheldon W. Tobe, MD, MScCH HPTE, FRCPC, FACP, FASH, 2
Conflict Disclosure Information Presenter 1: – Grants/Research Support: – Speakers Bureau/Honoraria: – Consulting Fees: – Other: 3
Outline of Today’s Activity Introduction Case Presentation Key Learnings & Questions Wrap Up 4
Module 5: Management of Hypertension in Non-diabetes Patients with Chronic Kidney Disease Gerald An 78-year-old man with a 20 year history of hypertension is found to have a creatinine of 140 umol/L on his most recent blood tests 5
Learning Objectives Upon completion of this activity, participants will be able to: State the new BP target for patients with non-DM CKD and understand the rationale for this change Identify the risk of developing CKD from HTN is graded based on race and comorbidities Understand that presence of non-DM CKD in hypertensive patients increases risk for cardiovascular outcomes 6
Statement of Need “My greatest challenge as a health care provider in the management of patients with hypertension is ” 7
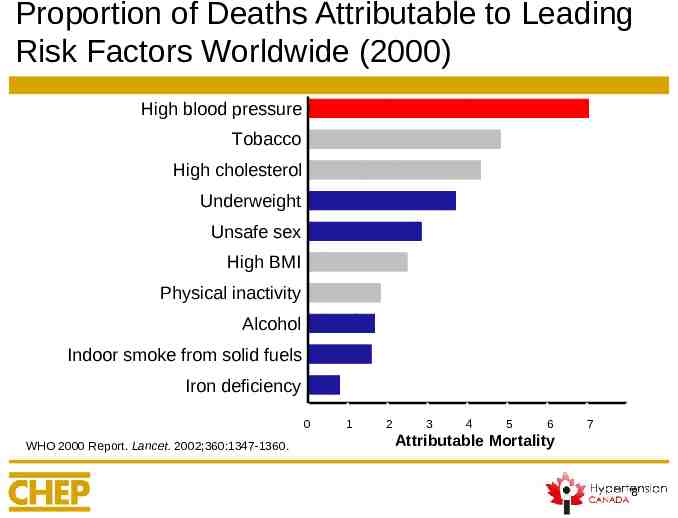
Proportion of Deaths Attributable to Leading Risk Factors Worldwide (2000) High blood pressure Tobacco High cholesterol Underweight Unsafe sex High BMI Physical inactivity Alcohol Indoor smoke from solid fuels Iron deficiency 0 WHO 2000 Report. Lancet. 2002;360:1347-1360. 1 2 3 4 5 6 7 8 Attributable Mortality 8
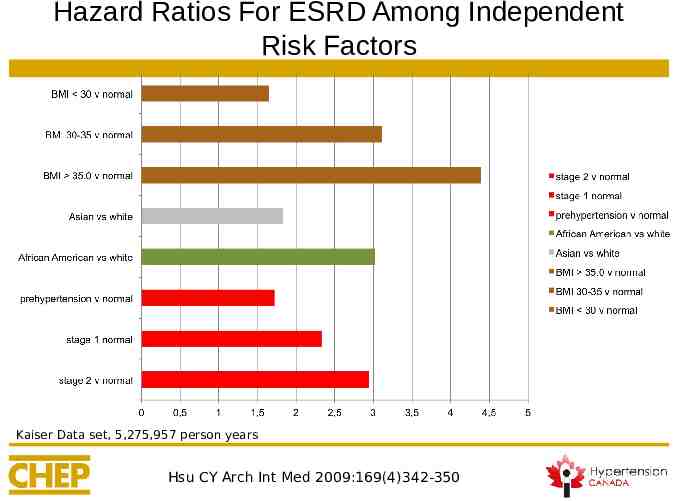
Hazard Ratios For ESRD Among Independent Risk Factors Kaiser Data set, 5,275,957 person years Hsu CY Arch Int Med 2009:169(4)342-350
Hypertension as a Risk Factor Hypertension is a significant risk factor for: – cerebrovascular disease – coronary artery disease – congestive heart failure – renal failure – peripheral vascular disease – dementia – atrial fibrillation 10
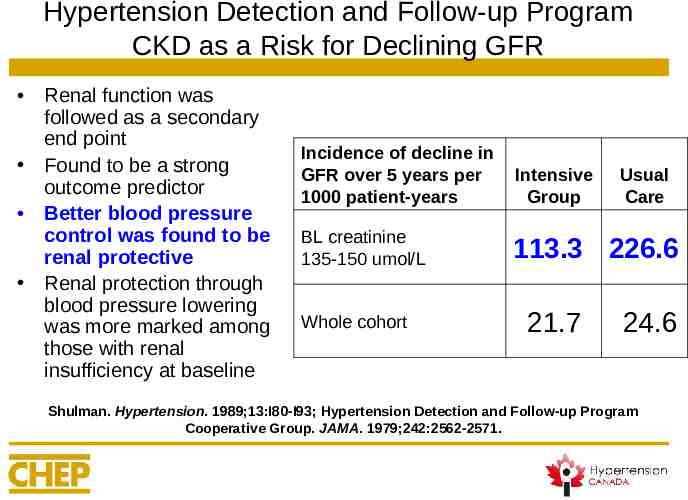
Hypertension Detection and Follow-up Program CKD as a Risk for Declining GFR Renal function was followed as a secondary end point Found to be a strong outcome predictor Better blood pressure control was found to be renal protective Renal protection through blood pressure lowering was more marked among those with renal insufficiency at baseline Incidence of decline in GFR over 5 years per 1000 patient-years Intensive Group BL creatinine 135-150 umol/L 113.3 226.6 Whole cohort 21.7 Usual Care 24.6 Shulman. Hypertension. 1989;13:I80-I93; Hypertension Detection and Follow-up Program Cooperative Group. JAMA. 1979;242:2562-2571.
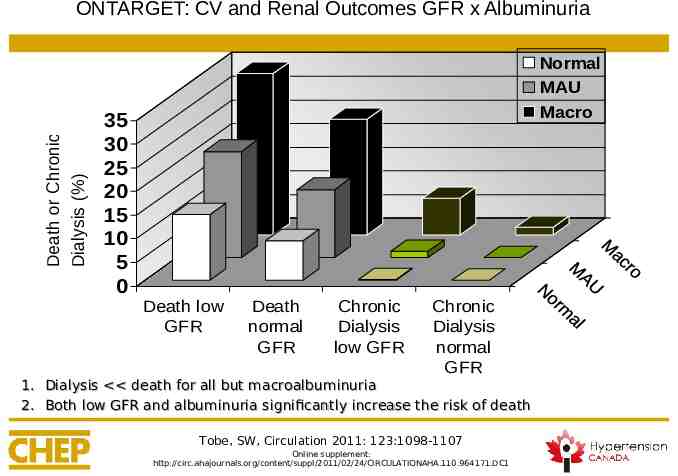
Death or Chronic Dialysis (%) ONTARGET: CV and Renal Outcomes GFR x Albuminuria 1. 2. 35 30 25 20 15 10 5 0 Normal MAU Macro Death low GFR Death normal GFR Chronic Dialysis low GFR Chronic Dialysis normal GFR Dialysis death for all but macroalbuminuria Both low GFR and albuminuria significantly increase the risk of death Tobe, SW, Circulation 2011: 123:1098-1107 Online supplement: http://circ.ahajournals.org/content/suppl/2011/02/24/CIRCULATIONAHA.110.964171.DC1
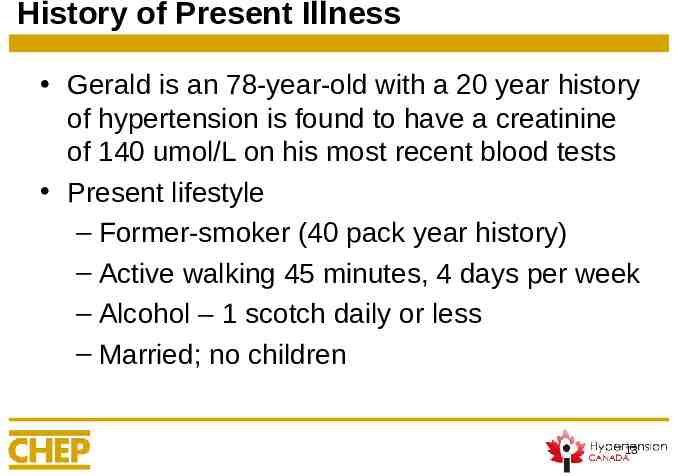
History of Present Illness Gerald is an 78-year-old with a 20 year history of hypertension is found to have a creatinine of 140 umol/L on his most recent blood tests Present lifestyle – Former-smoker (40 pack year history) – Active walking 45 minutes, 4 days per week – Alcohol – 1 scotch daily or less – Married; no children 13
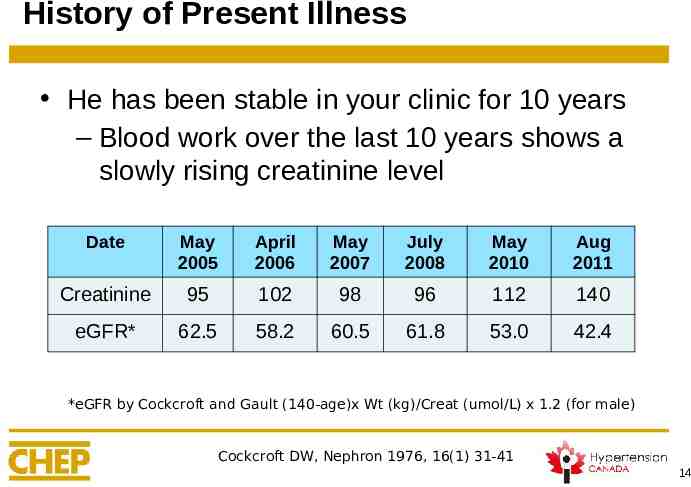
History of Present Illness He has been stable in your clinic for 10 years – Blood work over the last 10 years shows a slowly rising creatinine level Date May 2005 April 2006 May 2007 July 2008 May 2010 Aug 2011 Creatinine 95 102 98 96 112 140 eGFR* 62.5 58.2 60.5 61.8 53.0 42.4 *eGFR by Cockcroft and Gault (140-age)x Wt (kg)/Creat (umol/L) x 1.2 (for male) Cockcroft DW, Nephron 1976, 16(1) 31-41 14
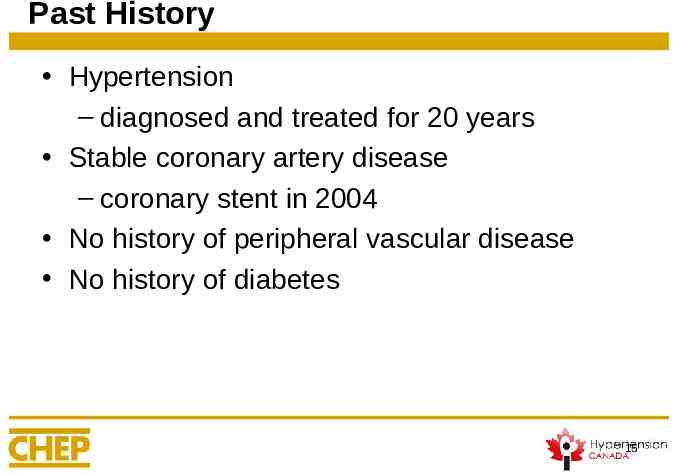
Past History Hypertension – diagnosed and treated for 20 years Stable coronary artery disease – coronary stent in 2004 No history of peripheral vascular disease No history of diabetes 15
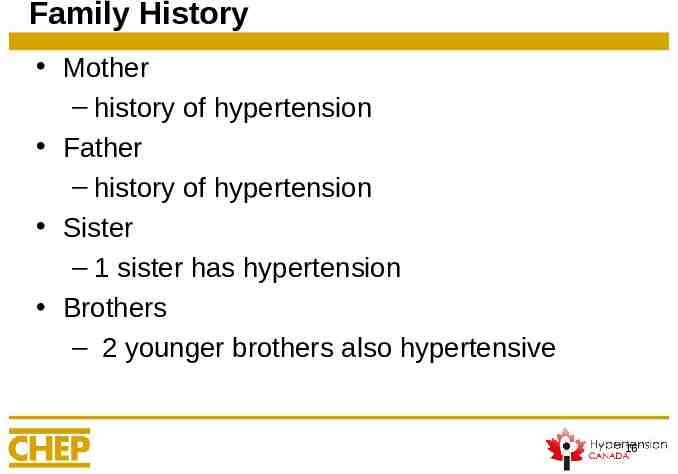
Family History Mother – history of hypertension Father – history of hypertension Sister – 1 sister has hypertension Brothers – 2 younger brothers also hypertensive 16
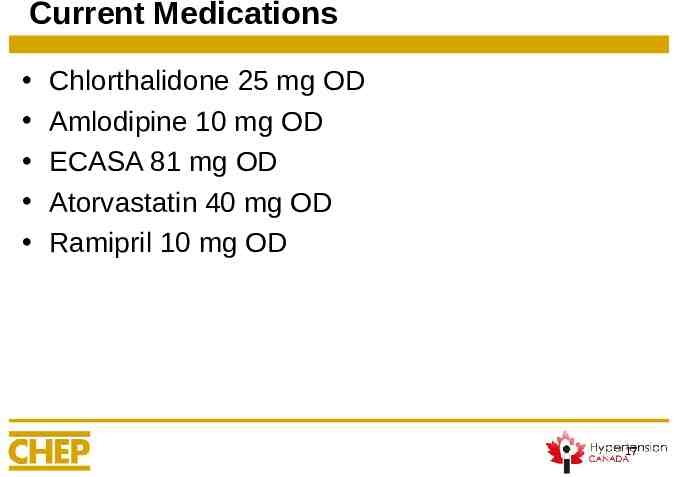
Current Medications Chlorthalidone 25 mg OD Amlodipine 10 mg OD ECASA 81 mg OD Atorvastatin 40 mg OD Ramipril 10 mg OD 17
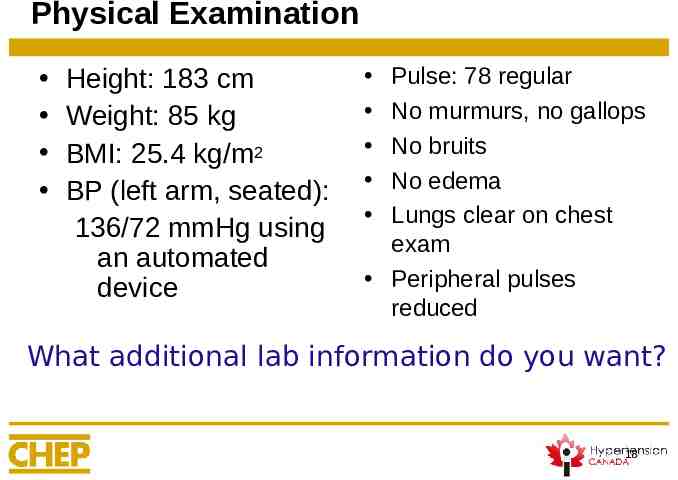
Physical Examination Height: 183 cm Weight: 85 kg BMI: 25.4 kg/m2 BP (left arm, seated): 136/72 mmHg using an automated device Pulse: 78 regular No murmurs, no gallops No bruits No edema Lungs clear on chest exam Peripheral pulses reduced What additional lab information do you want? 18
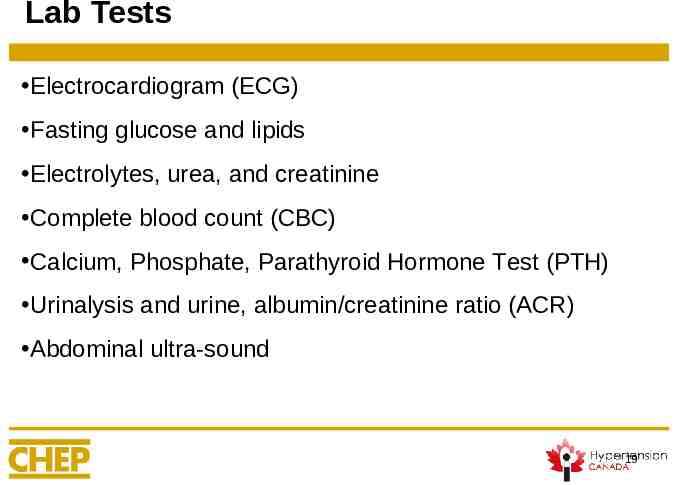
Lab Tests Electrocardiogram (ECG) Fasting glucose and lipids Electrolytes, urea, and creatinine Complete blood count (CBC) Calcium, Phosphate, Parathyroid Hormone Test (PTH) Urinalysis and urine, albumin/creatinine ratio (ACR) Abdominal ultra-sound 19
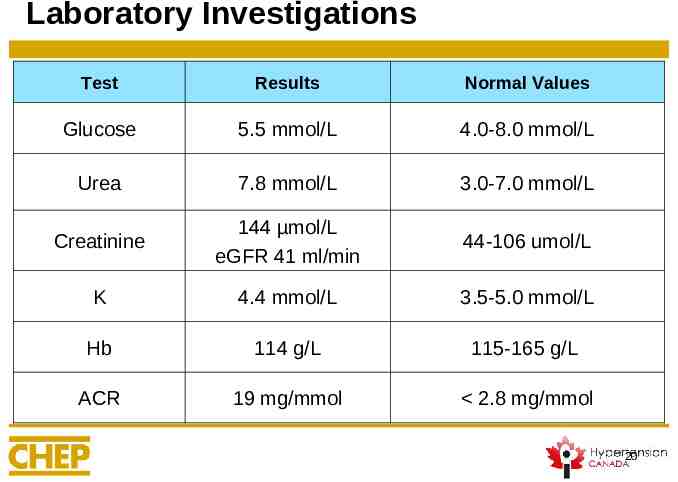
Laboratory Investigations Test Results Normal Values Glucose 5.5 mmol/L 4.0-8.0 mmol/L Urea 7.8 mmol/L 3.0-7.0 mmol/L Creatinine 144 µmol/L eGFR 41 ml/min 44-106 umol/L K 4.4 mmol/L 3.5-5.0 mmol/L Hb 114 g/L 115-165 g/L ACR 19 mg/mmol 2.8 mg/mmol 20

Laboratory Investigations Test Results Normal Values LDL 2.2 mmol/L 2.50 mmol/L Total Chol 3.8 mmol/L 5.20 mmol/L TG 2.2 mmol/L 1.70 mmol/L HDL 1.1 mmol/L 0.99 mmol/L TC:HDL 3.75 High risk target: 4.0 Mod risk target: 5.0 Low risk target: 6.0 21
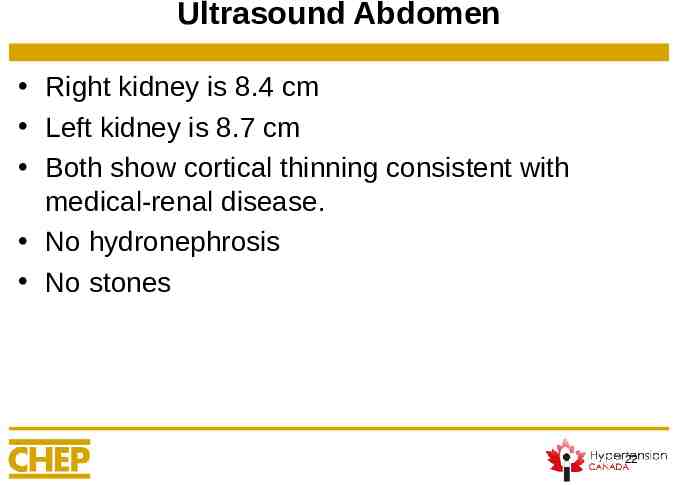
Ultrasound Abdomen Right kidney is 8.4 cm Left kidney is 8.7 cm Both show cortical thinning consistent with medical-renal disease. No hydronephrosis No stones 22
Discussion Question 1 What is the blood pressure target for Gerald? 23
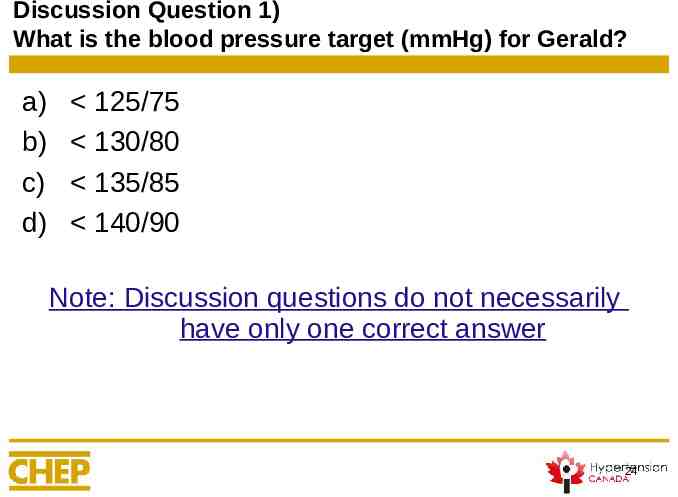
Discussion Question 1) What is the blood pressure target (mmHg) for Gerald? a) b) c) d) 125/75 130/80 135/85 140/90 Note: Discussion questions do not necessarily have only one correct answer 24
a) 125/75 Incorrect This is no longer the BP target for any patient with HTN. 25
b) 130/80 Incorrect in this case 130/80 mmHg is the BP target for people with diabetes with or without CKD 26
C) 135/85 Incorrect This is the correct answer if you use home BP readings or an automated device in your office, such as BpTRU 27
d) 140/90 Correct This is the new BP target for people with chronic kidney disease and no diabetes 28
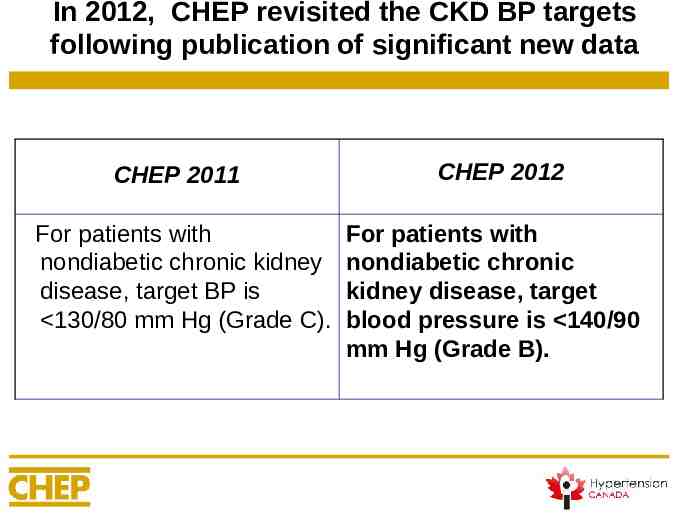
In 2012, CHEP revisited the CKD BP targets following publication of significant new data CHEP 2011 For patients with nondiabetic chronic kidney disease, target BP is 130/80 mm Hg (Grade C). CHEP 2012 For patients with nondiabetic chronic kidney disease, target blood pressure is 140/90 mm Hg (Grade B).
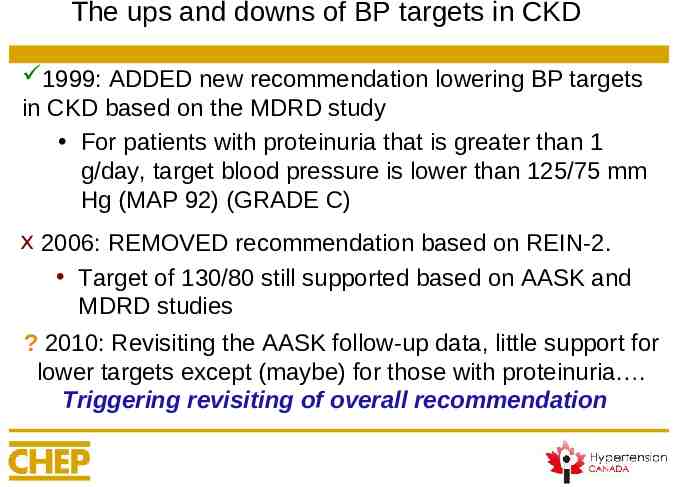
The ups and downs of BP targets in CKD 1999: ADDED new recommendation lowering BP targets in CKD based on the MDRD study For patients with proteinuria that is greater than 1 g/day, target blood pressure is lower than 125/75 mm Hg (MAP 92) (GRADE C) x 2006: REMOVED recommendation based on REIN-2. Target of 130/80 still supported based on AASK and MDRD studies ? 2010: Revisiting the AASK follow-up data, little support for lower targets except (maybe) for those with proteinuria . Triggering revisiting of overall recommendation
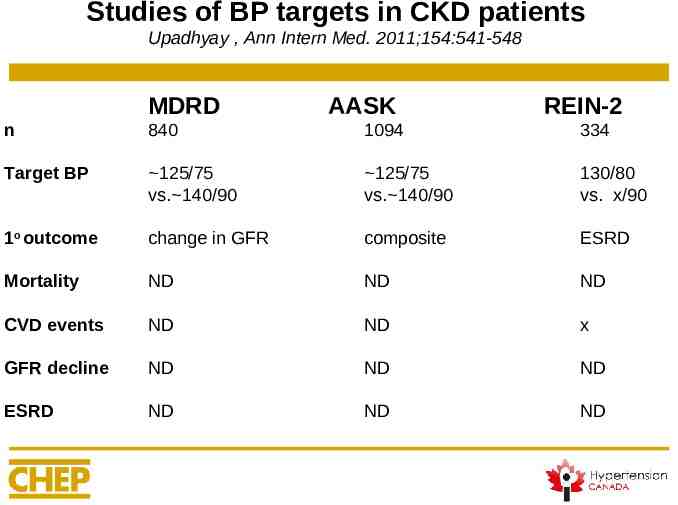
Studies of BP targets in CKD patients Upadhyay , Ann Intern Med. 2011;154:541-548 MDRD AASK REIN-2 n 840 1094 334 Target BP 125/75 vs. 140/90 125/75 vs. 140/90 130/80 vs. x/90 1o outcome change in GFR composite ESRD Mortality ND ND ND CVD events ND ND x GFR decline ND ND ND ESRD ND ND ND
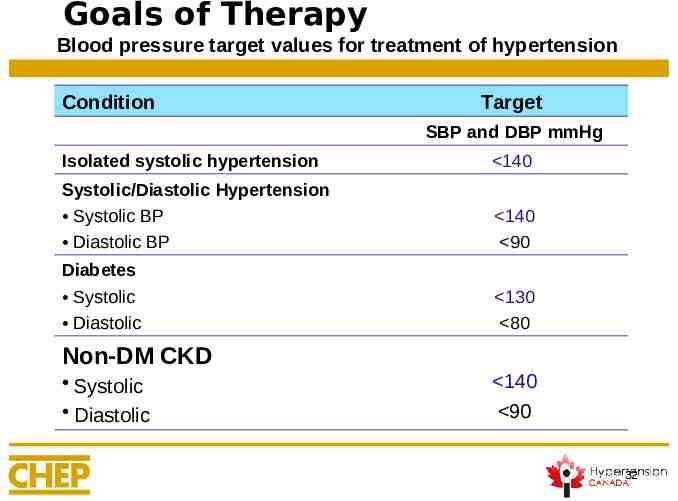
Goals of Therapy Blood pressure target values for treatment of hypertension Condition Target SBP and DBP mmHg Isolated systolic hypertension 140 Systolic/Diastolic Hypertension Systolic BP Diastolic BP 140 90 Diabetes Systolic Diastolic 130 80 Non-DM CKD Systolic Diastolic 140 90 32
Discussion Question 2 What other factors would you consider in optimization of BP control? 33
What other factors would you consider in optimization of BP control? a) b) c) d) RAAS blockade 24-hr ABPM Low sodium diet Avoid NSAIDS/Aminoglycosides/nephrotoxic drugs Note: Discussion questions do not necessarily have only one correct answer 34
a) RAAS blockade The patient is taking ramipril 10 mg/day 35
b) 24-hr ABPM Determine whether to patient has masked HTN (prevalence 20%) Determine whether nocturnal HTN – consider longer acting ACE inhibitor 36
c) Low sodium diet High dietary sodium is an key contributor to high blood pressure. To decrease blood pressure, consider reducing sodium intake towards 2,000 mg (5g of salt or 87mmol of sodium) per day. 37
d) Avoid NSAIDS/Aminoglycosides/nephrotoxic drugs Nephrotoxic drugs can cause hemodynamic compromise of kidney in patients with CKD Examples of nephrotoxic drugs – – – – – – – – – Aminoglycosides Nonsteroidal anti-inflammatory drugs (NSAIDs) Acyclovir Amphotericin B Lithium Phenytoin Sulfonamides Vancomycin Zoledronic acid Baumgarten, Gehr. Am Fam Physician 2011;84:1138-48 38
Discussion Question 3 How would you manage Gerald’s global cardiovascular risk associated with HTN and CKD? 39
How would you manage Gerald’s global cardiovascular risk associated with HTN and CKD? a) b) c) d) LDL 2.0 mmol/L Cholesterol Control: TC/HDL 4.0 Smoking cessation Diet and exercise (BMI 25 kg/m2) Note: Discussion questions do not necessarily have only one correct answer 40
a) LDL 2.0 Primary lipid targets for adults with diabetes at high risk for CVD 2.0 mmol/L Achievable with statin monotherapy 41
b) Cholesterol Control High risk for CVD, secondary target TC/HDL of 4.0 42
c) Smoking cessation Maintain present lifestyle of non-smoking (former smoker with 40 pack year history)
d) Diet and exercise (BMI 25 kg/m2) Lifestyle changes are a critical component of hypertension management and prevention An accumulation of 30-60 minutes of dynamic exercise of moderate intensity four to seven days per week in addition to the routine activities of daily living.
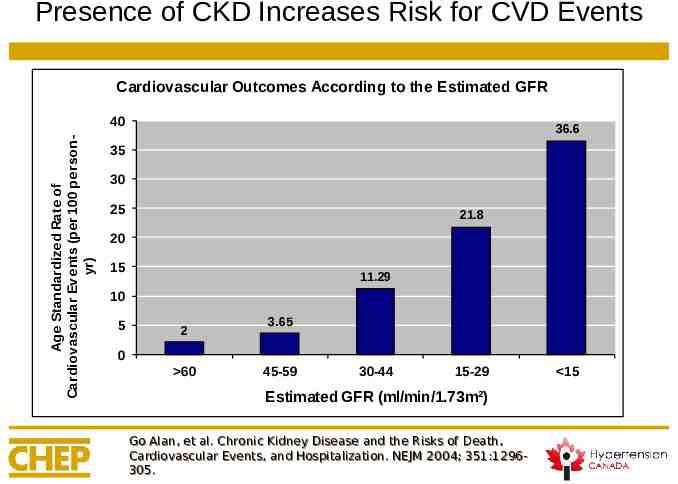
Presence of CKD Increases Risk for CVD Events Cardiovascular Outcomes According to the Estimated GFR Age Standardized Rate of Cardiovascular Events (per 100 person yr) 40 36.6 35 30 25 21.8 20 15 11.29 10 5 2 3.65 0 60 45-59 30-44 15-29 Estimated GFR (ml/min/1.73m²) Go Alan, et al. Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization. NEJM 2004; 351:1296305. 15
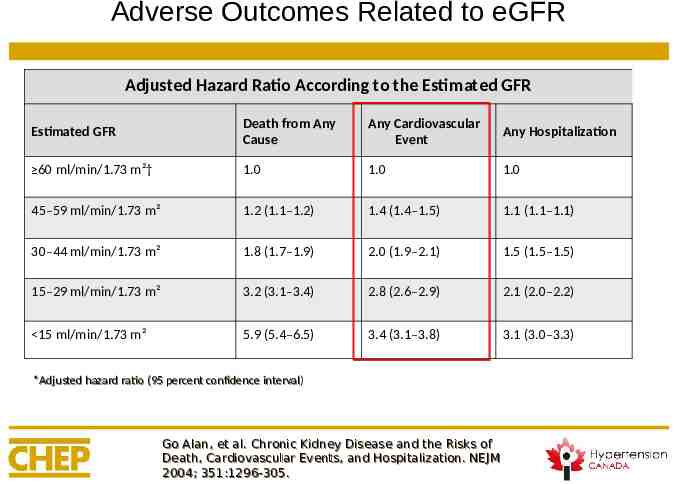
Adverse Outcomes Related to eGFR Adjusted Hazard Ratio According to the Estimated GFR Estimated GFR Death from Any Cause Any Cardiovascular Event Any Hospitalization 60 ml/min/1.73 m²† 1.0 1.0 1.0 45–59 ml/min/1.73 m² 1.2 (1.1–1.2) 1.4 (1.4–1.5) 1.1 (1.1–1.1) 30–44 ml/min/1.73 m² 1.8 (1.7–1.9) 2.0 (1.9–2.1) 1.5 (1.5–1.5) 15–29 ml/min/1.73 m² 3.2 (3.1–3.4) 2.8 (2.6–2.9) 2.1 (2.0–2.2) 15 ml/min/1.73 m² 5.9 (5.4–6.5) 3.4 (3.1–3.8) 3.1 (3.0–3.3) *Adjusted hazard ratio (95 percent confidence interval) Go Alan, et al. Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization. NEJM 2004; 351:1296-305.
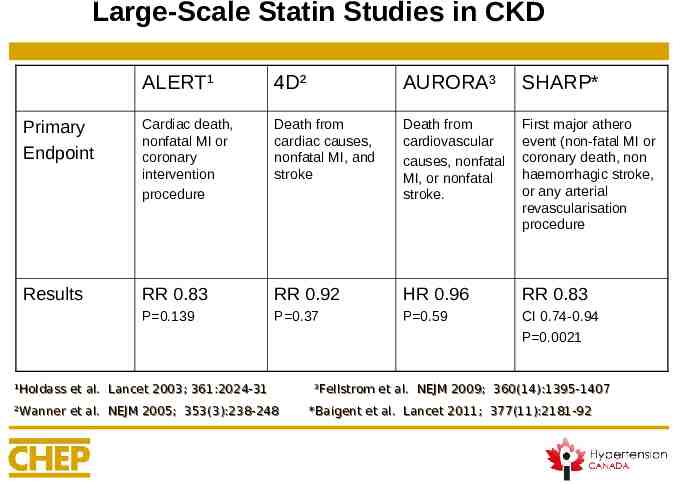
Large-Scale Statin Studies in CKD ALERT¹ 4D² AURORA³ SHARP* Primary Endpoint Cardiac death, nonfatal MI or coronary intervention procedure Death from cardiac causes, nonfatal MI, and stroke Death from cardiovascular causes, nonfatal MI, or nonfatal stroke. First major athero event (non-fatal MI or coronary death, non haemorrhagic stroke, or any arterial revascularisation procedure Results RR 0.83 RR 0.92 HR 0.96 RR 0.83 P 0.139 P 0.37 P 0.59 CI 0.74-0.94 P 0.0021 ¹Holdass et al. Lancet 2003; 361:2024-31 ²Wanner et al. NEJM 2005; 353(3):238-248 ³Fellstrom et al. NEJM 2009; 360(14):1395-1407 *Baigent et al. Lancet 2011; 377(11):2181-92
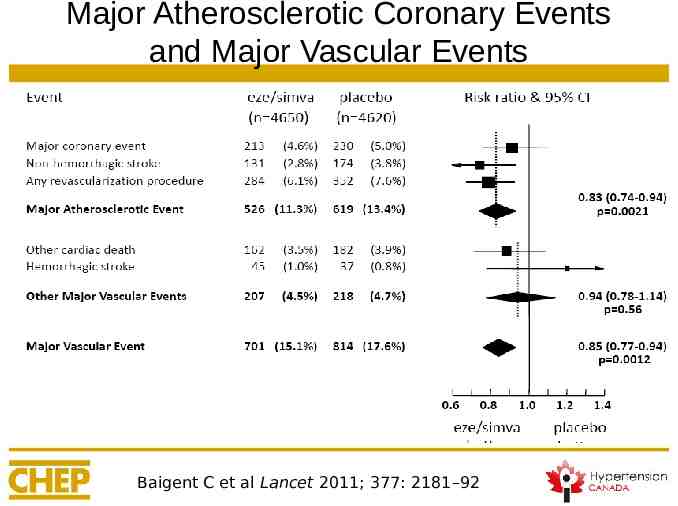
Major Atherosclerotic Coronary Events and Major Vascular Events Baigent C et al Lancet 2011; 377: 2181–92
Case Progression After the tests are completed and reviewed with Gerald, he asks about his blood pressure control. You describe that his BP target is 140/90 mmHg and that he is at his target. You also discuss the need for ongoing global cardiovascular risk reduction strategies and give him positive feedback for achieving optimal medical therapy including: being on a RAAS blocker and BP at target regular exercise careful diet good LDL control with a statin maintaining a smoke free lifestyle 49
Key Learnings For patients with nondiabetic chronic kidney disease, target blood pressure should be 140/90 mmHg Maintaining a healthy lifestyle and weight lowers blood pressure and prevents hypertension Promote: reducing dietary sodium and increased physical activity
The full slide set of the 2015 CHEP Recommendations is available at www.hypertension.ca 51