Recovery and Psychiatric Rehabilitation Prepared by Mohamed Z. Aish
48 Slides3.09 MB
Recovery and Psychiatric Rehabilitation Prepared by Mohamed Z. Aish Hisham M. El-Mudallal Supervised by Dr. Ashraf Aljedi
Tertiary Prevention In Psychiatric Care Goal of tertiary prevention is to limit the amount of disability and maladaptive functioning resulting from an illness. Concepts of tertiary prevention relevant to patients with serious mental illness. 1 in 17 adults in USA have a serious mental illness. Nurses care for these people in a variety of settings: Private and public psychiatric hospitals. Psychiatric and medical-surgical units in general hospitals. Emergency rooms. Community-based treatment and rehabilitation programs. Primary care settings. Patients homes.
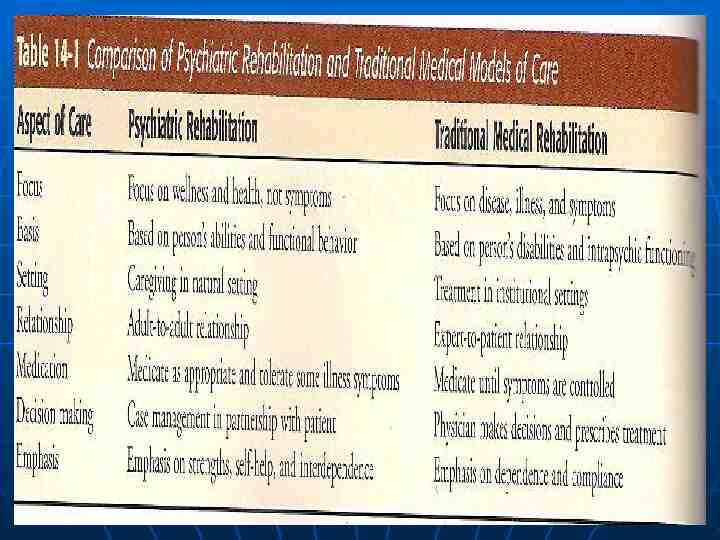
Rehabilitation Tertiary prevention is carried out through activities identified as rehabilitation, which is the process of helping the person return to the highest possible level of functioning. Psychiatric rehabilitation is a combination of services incorporating social, educational, occupational, behavioral, and cognitive interventions aimed at long-term recovery and maximization of self-sufficiency. Psychiatric rehabilitation grew out of a need to create opportunities for people diagnosed with severe mental illness to live, learn, and work in their own communities. Psychiatric rehabilitation uses a person-centered, people-topeople approach that differs from the traditional medical model of care ( Table 14-1 ).
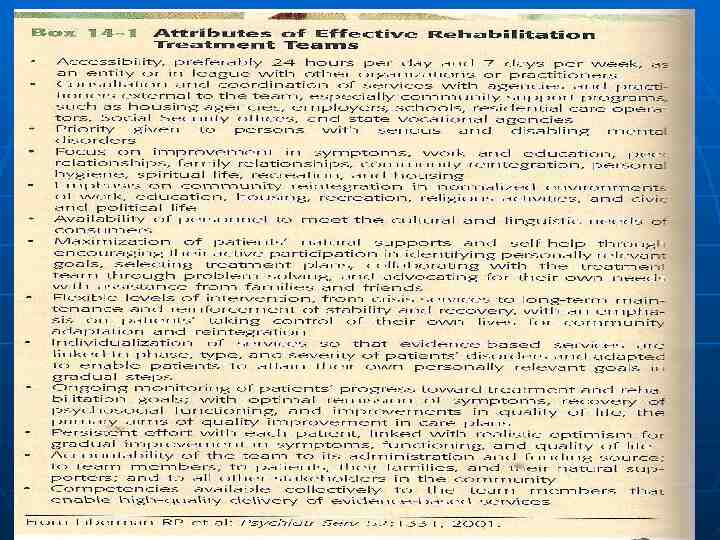
Although research has reported that certain interventions effectively assist people who have serious mental illnesses function productively in their communities. The first group of disseminated evidence-based practices that support and enhance psychiatric rehabilitation included the following: assertive community treatment, supported employment, illness management and recovery, integrated treatment for co-occurring mental illness and substance abuse, family psycho-education, and medication management. Rehabilitative psychiatric nursing takes place in the context of a multidisciplinary treatment team. Other team members may include: psychiatrists, psychologists, social workers, occupational therapists, rehabilitation counselors, case managers, consumer team members, family advocates, employment specialists, or job coaches.
Rehabilitative psychiatric nursing also must be studied in the contexts of the patient, family, and social system . This requires the nurse to focus on 3 elements: 1- The individual. 2- The family. 3- The community. The nursing care of people with serious mental illnesses is related to these 3 elements and the activities of assessment, planning and implementation, and evaluation. The psychiatric rehabilitation philosophy is consistent with the goal of recovery.
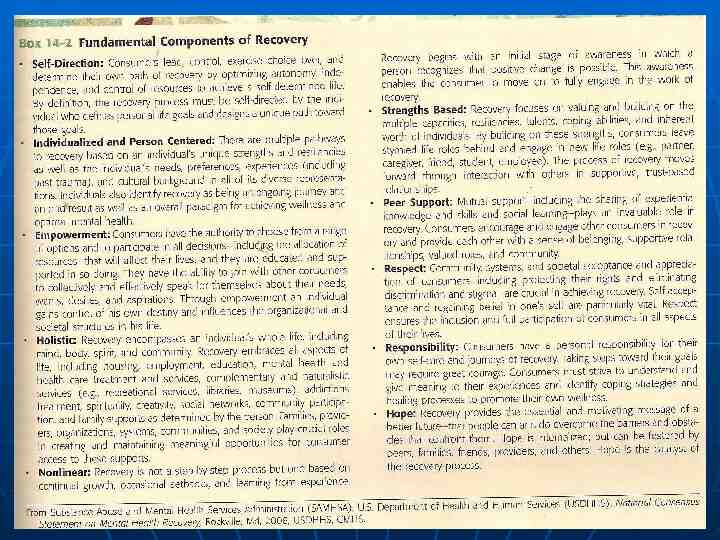
Recovery Recovery is the process in which people are able to live, work, learn, and participate fully in their communities. Recovery is a journey of healing and transformation enabling a person with a mental health problem to live a meaningful life in a community of his or her choice while striving to achieve his or her full potential.
Assessment The Individual: Assessment of the need for rehabilitation and recovery begins with the initial contact between the nurse and the patient. A comprehensive psychiatric nursing assessment provides information that enables the nurse to help the patient achieve maximum possible functioning. Nurses are expected to identify and reinforce strengths as one means of helping the patient cope. When conducting an initial assessment, the nurse needs to assist the patient to plan for recovery by identifying the individuals life goals and strengths and discussing services available from the health care system and the persons social support network that will support strengths and assist in goal achievement.
Characteristics of Serious Mental Illness People who have SMI are likely to have primary and secondary symptoms. Primary symptoms are directly caused by the illness. For example, hallucinations and delusions are primary symptoms of schizophrenia, and elation and hyperactivity are primary symptoms of bipolar disorder. Secondary symptoms, such as loneliness and social isolation, are caused by the person response to the illness or its treatment. Behaviors related to primary symptoms may violate social norms and be considered deviant. Society tries to protect itself from the persons norm violation. As behavior problems become more serious, people increasingly identify themselves as mentally ill. They begin to relate to society in terms of this identity rather than others, such as wife, mother, husband, father, or worker. The persons acceptance of mentally ill status and adjustment to society in terms of this role are accompanied by the secondary symptoms of SMI.
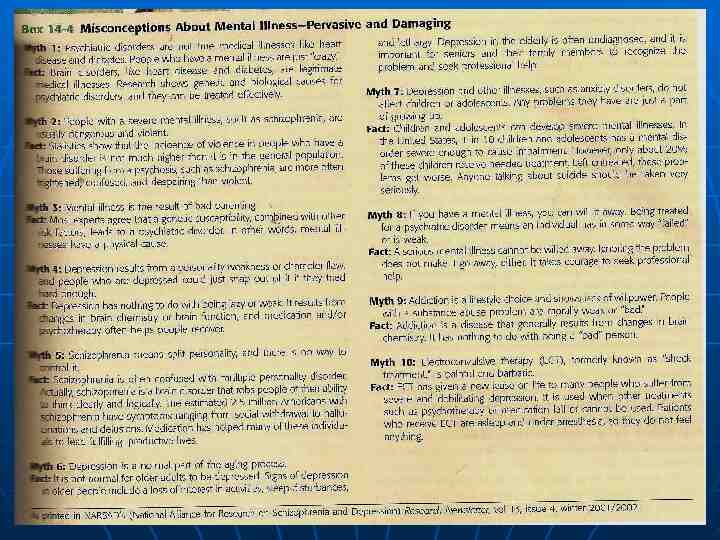
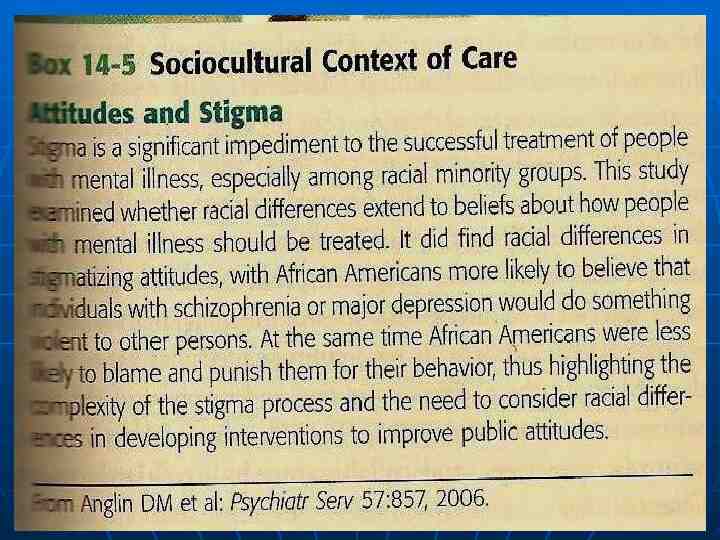
Behaviors related to serious mental illness Blocks to recovery of individuals with SMI include poverty, victimization, and stigma. People with SMI are often unemployed, less likely to be involved in close relationships, and tend to have fewer financial resources than their peers. Stigma experienced by those who are mentally ill has been linked to self-esteem. A study of women with mental illness found that when there was low perception of discrimination and the women did not believe that discrimination was legitimate, they had higher self-esteem. Thus the effects of stigma, poverty and victimization should be included in patient assessment and treatment planning.
Activities of daily living: Are skills that are necessary to live independently, such as housekeeping, shopping, food preparation, money management, and hygiene. A major goal of recovery is to help the person develop independent living skills. Interpersonal relations: People who have SMI are apathetic, withdrawn, and socially isolated. These behaviors create serious problems in establishing close relationships. Nonetheless, formal and informal networks are needed by the seriously ill. Low self-esteem: is the feeling of self-worth or regard for oneself. Lack of ability to maintain employment, live independently, marry, and have children contributes to low selfesteem. Motivation :Fear of failure often results in reluctance to try new experiences. Lack of motivation may be caused by low energy related to the biological effect of the illness or to medication.
Strengths: An emphasis on strengths provides hope that improved functioning is possible. Strengths may be related to recreational and leisure activities, work skills, educational accomplishments, self-care skills, special interests, talents and abilities, and positive interpersonal relationships. Non-adherence: Failure to take medication is a common cause of re-hospitalization. Assess the reasons for non-adherence as denial of the illness, lack of understanding of the reason for treatment regimen, side effects of medication. Living skills assessment: The nursing assessment of a patient with a SMI should include an analysis of the physical, emotional, and intellectual components of the skills needed for living, learning, and working in the community.
The Family Components of family assessment The nurse who assesses the family as part of a rehabilitation plane should consider the following aspects of family dynamics: Family structure, including developmental stage, roles, responsibilities, norms, and values. Family attitudes toward the mentally ill member. The emotional climate of the family (fearful, angry, depressed, anxious, calm). The social supports available to the family, including extended family, friends, financial support, religious involvement, and community contacts. Past family experiences with mental health services. The family s understanding of the patient s problem and the plan of care. The nurse should plan on regular contacts with family members and inclusion of them as part of the treatment team.
Family Burden The mental illness of a family member affects the entire family. The most burden was related to worry about the future, poor concentration, upset household routines, feeling guilty about not doing enough, feeling trapped, and being upset by changes in their family member. Burden may be objective or subjective. Objective burden is related to the patients behavior, role performance, adverse effects on the family, need for support, and financial costs of the illness. Subjective burden is the persons own feeling of being burdened; it is individual and not consistently related to the elements of objective burden. Several responses are frequently noted in families who have members with SMI:
Grief: Is common and is related to the loss of the person they knew before the illness, as well as loss of the future that they expected to share with the ill family member. Guilt: Is common for those who are close to a person with SMI to wonder whether they could have done something to prevent it. Parents of a depressed woman may believe that they could prevented her depression if they had not shared their own worries with her. Anger: May be directed toward the patient, other family members, mental health care providers, or the entire health care system. Powerlessness and fear: Often result from families realization that they are dealing with a long-term recurrent illness.
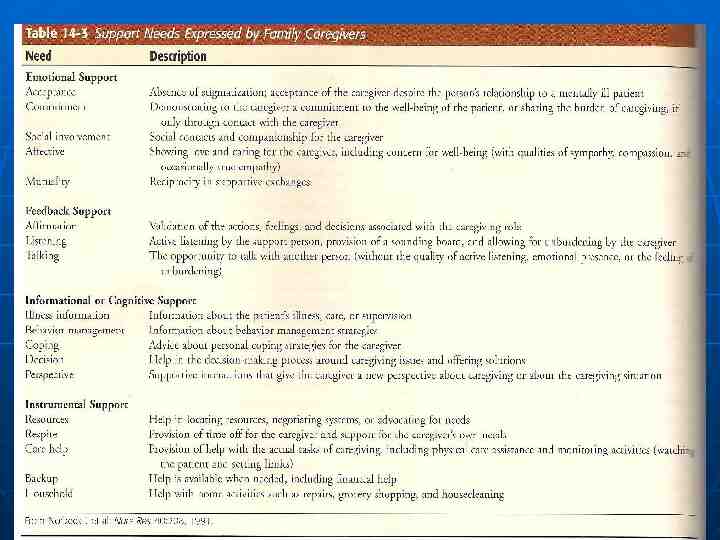
Social Support Needs Families who are providing care for members who have SMI often feel isolated and alone in dealing with the challenges of care giving. Previous sources of social support may be lost or limited because of the demands of attending to the mentally ill family member. Caregivers may be embarrassed about the illness or fear that the person with mental illness will behave inappropriately in the presence of others. Nurses can play an important role in offering family members opportunities to discuss their concerns and taking action to meet their needs whenever possible. Table 14-3 lists support needs expressed by family caregivers.
The community The community greatly influences the rehabilitation and recovery of its mentally ill members. Mental health professionals have a unique role in the community because they are community member and also advocates for people with mental illness and their families at the same time . care providers, including nurses , should assume a leadership role in assessing the adequacy and effectiveness of community resources and in recommending change to improve access and quality of mental health care .
Nurses in all setting must be familiar with the community agencies that provide services to people with mental illnesses . Most communities have asocial and medical services directory that can to consult for basic information , such as location , type ,and cost of services provided . Most agencies serve people who come from a particular geographic area, such as one part of a city or, in a rural area , one or several counties. Nurses should pay attention to patient evaluation of the agencies from which they receive services. This information helps to identify agencies that are responsive and helpful as opposed to those that are difficult for patients to approach.
The nurse also can provide emotional support of the patient feels insecure in anew situation. Nurse should introduce them selves to the staff of the agency and explain that they. As well as the patient, would like to learn more about the services. Collaboratetive relationships between mental health care providers and community agencies ate essential if rehabilitation is to succeed. A wide range of community services must be available to patients. Those that are directed toward basic needs include provisions for shelter, food and clothing; activities; and mobility and transportation.
. Other services provide for special needs that may differ from one person the next, such as general medical services, mental Health services, habilitation and rehabilitation programs. Vocational service, and social services. A third group of services coordinates the system. These include patient identification and outreach, individual assessment and service planning, case management, advocacy and community organization, community information, and support.
Planning and implementation The individual Treatment planning and intervention in Recovery-focused psychiatric nursing aim to foster independence by maximizing the per-sons strengths. Specially, the nurse helps the individual to do the following: Develop strengths and potential. Learn living skills. Manage one’s illness. Access environmental supports.
The nursing treatment plan should be organized be organized around very specific behavioral goals that ate bases on a comprehensive assessment of the person's living skills. These goals should building in those that are developed during the acute phase of the illness. This part of the nursing care plan may be called the discharge be developed in community care setting. Discharge plans also should be developed in community care setting. This will remind the nurses and patient that the expected outcome of nursing care is independent functioning.
The nurse and patient must decide together on the desired level of functioning. If the patient is unwilling to take on activities that the nurses thinks would be helpful. It is important to determined why. Sometimes nurses try to push a patient ahead too rapidly. Behavior that has developed gradually over time cannot be changed quickly. Learning new behavior patterns and giving up old ones are frightening and cause anxiety.
The nurse must be sure that the patients coping skills are adequate to deal with the stress of growth. Feedback must be requested to be sure that the rehabilitation plan continues to address the patient’s needs. Its is a problem if the plan assumes greater important than the patient. The nurse must prevent this from happening.
Developing strengths and potential The development of the patient’s strengths and potential is critically important. Nursing interventions that develop strengths and potentials can help patients develop independent living skills, interpersonal relationships, and coping resources and thus help meet their special needs. Ultimately, the expected outcome of such intervention is change in the patient’s self-concept and an increase in self-esteem. The negative self-concept and low selfesteem that characterize people who have serious mental illnesses interfere with their ability to see the themselves as individuals with strengths and potentials.
Learning living skills Learning living skills. Social skills uses cognitive and behavioral techniques to help people gain the knowledge and skills they need to live in the community. Persons participating in social skills training should be assisted to express their problems as positive goals. For example, instead o the negative “I’m tires of watching television al the time.” encourage-age the positive “I an going to see at least one friend every week” social skills training program typically use videos. Role playing, practice and homework assignments centered on practical problems.
Another important aspect of psychiatric rehabilitation and recovery relates to promoting the physical well-being of those with serious mental illness. problems such as high tobacco use, low exercise level, poor oral health, high-risk sexual behavior, and limited contact with physicians and dentists ate common among people who have serious mental illnesses.
illness management . Illness management is an evidencebased practice that focus on assisting the patient to assume control over the illness and function at the highest possible level of independent . Four intervention that have been identified to support illness management in persons recovery from psychiatric illness are as follows :
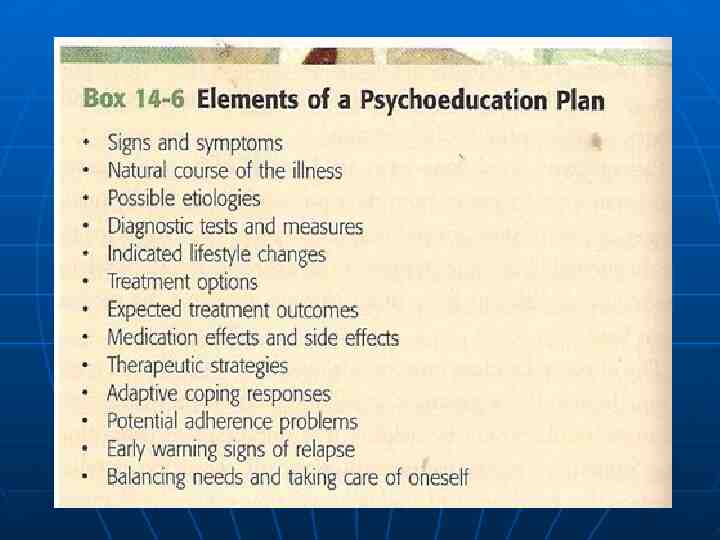
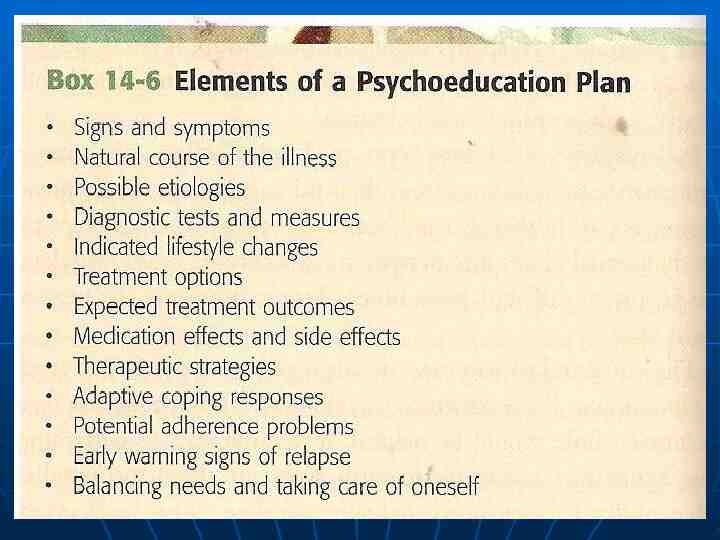
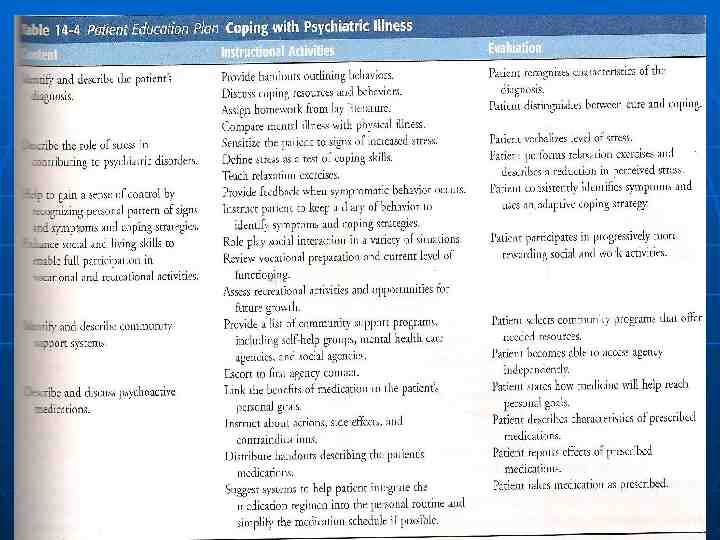
psychoeducation: an approach that -1 support the rehabilitation process by teaching the patient and family about the mental illness and the coping skills that will help with successful community living .(box 14-6) behavior tailoring for medication: -2 developing strategies with the patient that integrate medication regimens into the persons daily routine and Simplifying the .medication schedule
training in relapse prevention : -3 most people who have serious mental illnesses can learn to recognize signs and .symptoms of an approaching relapse coping skill training : teaching the -4 person techniques for coping with persistent symptoms of mental illness , person who has auditory hallucination can be trained to listen to music use .headphone
Accessing environmental support support people who have mental illness in community setting requires the development of a wide array of community support programs. Some of these are rehabilitation center. Housing services , employment opportunities , education , crisis intervention and .outreach and case management
Rehabilitation programs psychiatric rehabilitation programs were developed in response to the plight of people who had been discharged from state mental hospital lacking the skill and resources needed to live independently several models are presented here as an over-view of some of the psychiatric rehabilitation approaches that have .evidence supporting their effectiveness
Residential services Housing is consistently identified as a critical element of successful recovery and rehabilitation services . Appropriate housing must be safe , affordable, and acceptable to the consumer early housing program tended to focus on existing supervised living situation , such as foster care more recently , an array of housing option has been developed under the leadership of consumer and psychiatric rehabilitation professional .
Employment services An extensive of the literature has identified a number of barriers to employment for person with psychiatric disabilities and recommended action that would help to overcome the barriers : . These are summarized below Ongoing health insurance for medical care ,mental health care ,and medication regardless of employment status. Integration and coordination of clinical and vocational services .
Access to educational program . Benefits planning and assistance with financial management . Development of assets through special saving program for low-income individuals. Safe ,affordable , and stable housing that will not be jeopardized by a higher income . Peer support and self-help.
Evaluation Evaluation of psychiatric rehabilitations services usually covers the impact on the patient and family and the effectiveness of the community service system. Patient evaluation: Evaluation of the services provider to patient and family member must focus on the achievement of the expected outcome of the intervention . Most psychiatric rehabilitation evaluation program rely on both objective and subjective measure of outcome.
Objective measures are general related to the following question : Is the person living in the housing of personal choice? Have days of hospitalization in the last years decrease ? How many emergency room visits has the person made? How often does the person have contact with family members? Who are they? Can the person identify people to provide support in a crisis? Is the person involved in a community activities ? Is the person enrolled in an adult education course? In an academic education program ?
Program evaluation Program evaluation is conducted to inform administration about the relevance and costeffectiveness of the services they offer . It is often required by funding , regulatory, and licensure agencies to confirm that public mental health dollars are being spent wisely. Outcome measurement is an approach to evaluation that provide information about the effectiveness of services to individuals with mental illness and can also be used to analyze the impact of funding initiatives.