EDCBH-SUDS Provider Training Resolving Common Deficiencies Found
36 Slides567.92 KB
EDCBH-SUDS Provider Training Resolving Common Deficiencies Found During Provider Monitoring Medical Director Policies & Standards
Today’s Training Department of Health Care Services (DHCS) findings after completing FY 17/18 DMC-ODS county and provider monitoring. We will focus on findings related to the Medical Director Review what the regulations say Review the roles and responsibilities of the Medical Director Review changes under DMC-ODS regarding roles.
DHCS Monitoring During Fiscal Year 2017-2018, DHCS performed annual monitoring of counties for DMC-ODS and SAPT requirements. Upon review of all the monitoring conducted, DHCS determined what the most commonly cited deficiencies at the provider level were. DHCS recommends that counties make sure to monitor providers in these identified areas
DHCS Findings DHCS found there were: 1. Providers do not have Medical Director Policies and Standards (procedures) developed 2. Verification of required 5 Continuing Medical Education credits (CMEs) for the Medical Director not found 3. Beneficiary not placed in level of care according to ASAM or ASAM appears inaccurate 4. Counselors determining the diagnosis
El Dorado County Findings During EDCBH-SUDS FY 18-19 annual compliance monitoring the team found that provider’s did not have Medical Director Polices & Standards or they did not meet the minimum standards as described in 22 CCR. We also found that the majority of programs were unable to show that their Medical Directors received the minimum 5 hours of continuing education in addiction medicine.
Today’s Focus Today we will be focusing on the role of the SUD Medical Director and first two DHCS findings: 1. Providers do not have Medical Director policies and procedures developed 2. Verification of required 5 Continuing Medical Education credits (CMEs) for the medical director not found
Under DMC ODS Title 22 of the California Code of Regulations and DHCS DMC-ODS Intergovernmental Agreement Section III.PP.5.i. Describe which standards the Medical Director’s Policies & Standards must meet.
What does Title 22 say? “For a provider to receive reimbursement for Drug Medi-Cal substance use disorder services, those services shall be provided by or under the direction of a physician” - 22 CCR § 51341.1 (h) DMC physician must be licensed by the Medical Board Of California or the Osteopathic Medical Board of California - 22 CCR § 51341.1 (b)(21)
What does the I/A say? We will get to this later
Medical Director Roles and Responsibilities Each DMC or DMC-ODS provider must have a Medical Director who has medical responsibility for all clients of the program Duties of a Medical Director may vary, but at a minimum, they are responsible for:
Medical Director Roles and Responsibilities Reviewing each beneficiary’s personal, medical and substance abuse history Documenting the basis for the SUD diagnosis in the beneficiary’s individual chart. Physician must indicate that they reviewed each client’s personal, medical, and substance abuse history Determining whether SUD services are medically necessary record/chart. The DMC physician MUST determine and document whether SUD services are medically necessary Ensuring physical exam requirements are met Physical exam requirements must be me within 30 days
Medical Necessity Medical necessity is about the quality of services provided to beneficiaries. It primarily relates to what programs must do, not what beneficiaries must do (Taubman 2019). The key issues in establishing medical necessity is to demonstrate whether or not services provided to a Medi-Cal beneficiary were needed to address a medical problem (Taubman 2019).
How is Medical Necessity Established What must happen under DMC for medical necessity to be established?
Establishing Medical Necessity To establish medical necessity: The beneficiary is determined by qualified personnel to meet criteria for at least one diagnosis, and The beneficiary is placed into services that meet the ASAM criteria definition of medical necessity for services.
How Does the ASAM Define Medical Necessity ASAM uses the general definition of medical necessity which is: 1. Services requested are needed to identify or treat an illness that has been diagnosed or suspected. 2. Treatment services are consistent with: a. the diagnosis and treatment of the condition (‘experimental treatments’ are disallowed) b. the standards of good medical practice 3. Treatment services required are for other than convenience.
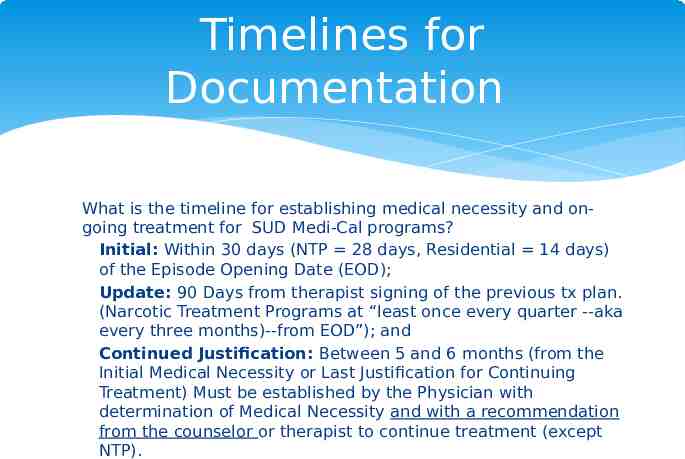
Timelines for Documentation What is the timeline for establishing medical necessity and ongoing treatment for SUD Medi-Cal programs? Initial: Within 30 days (NTP 28 days, Residential 14 days) of the Episode Opening Date (EOD); Update: 90 Days from therapist signing of the previous tx plan. (Narcotic Treatment Programs at “least once every quarter --aka every three months)--from EOD”); and Continued Justification: Between 5 and 6 months (from the Initial Medical Necessity or Last Justification for Continuing Treatment) Must be established by the Physician with determination of Medical Necessity and with a recommendation from the counselor or therapist to continue treatment (except NTP).
Medical Director Further Roles and Responsibilities Reviewing, approving and signing the treatment plan & treatment plan Determining if continuing services and medically necessary Between 5 and 6 months from date of admission Completing Continuing Services Justification or, Documenting if services are no longer medically necessary and discharge is appropriate There will be changes with ODS implementation still the Medical Director is ultimately responsible for this process
Medical Director Roles and Responsibilities Medical Directors shall also ensure: Medical care provided meets standard of care Physicians are not delegating the duties they are specifically responsible for Medical personnel follow medical policies and standards Medical decisions are not influenced by fiscal considerations Physicians are adequately trained to perform diagnosis of SUD, and determine medical necessity Delegated duties to physicians are properly performed
Medical Policies & Standards As a way of ensuring that the roles and responsibilities of the Medical Director are clearly known and in accordance with Title 22 and the I/A and common medical practice standards, the Medical Director must: Develop the required Medical Policies and Standards for the SUD treatment program. Implement, monitor, review, and update the Medical Policies and Standards that fall under their scope of practice.
Medical Policies & Standards Question? Since the roles and responsibilities are written in regulation or contract for all SUD Medical Directors do they have to be included in the Medical Policies & Standards developed by the Medical Director? Yes, not only did DHCS find that some SUD providers did not have Medical Policies and Standards at all, but some did have them but they did not contain all the required roles and responsibilities
Additional Information to Include Disease Prevention On-site injury prevention On-site injure response Medication dosing procedures Infectious diseases protocols Overdose procedure Medical emergency procedure Requirements for physical exam Procedure for when client is under the influence
But wait. What does the I/A say?
Finally! The Suspense Is Killing Me Does the implementation of the Organized Delivery System change the Medical Director’s responsibilities to be outlined in the Policies and Standards? YES!
Intergovernmental Agreement The DHCS DMC-ODS Intergovernmental Agreement Section III.PP.5.i. Allows medical directors to delegate certain responsibilities to qualified LPHA’s working within their scope of practice.
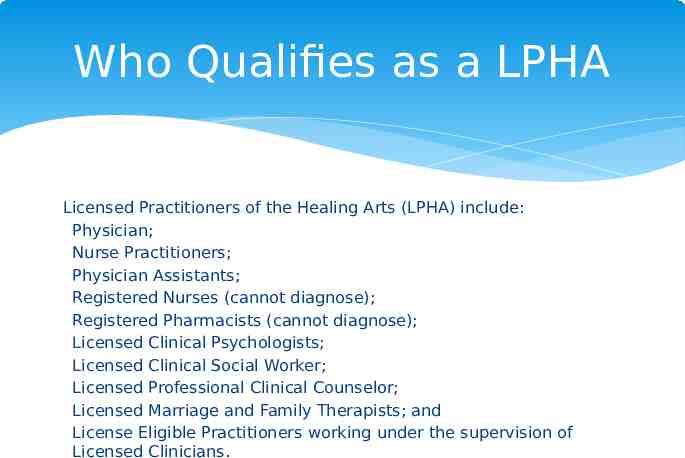
Who Qualifies as a LPHA Licensed Practitioners of the Healing Arts (LPHA) include: Physician; Nurse Practitioners; Physician Assistants; Registered Nurses (cannot diagnose); Registered Pharmacists (cannot diagnose); Licensed Clinical Psychologists; Licensed Clinical Social Worker; Licensed Professional Clinical Counselor; Licensed Marriage and Family Therapists; and License Eligible Practitioners working under the supervision of Licensed Clinicians.
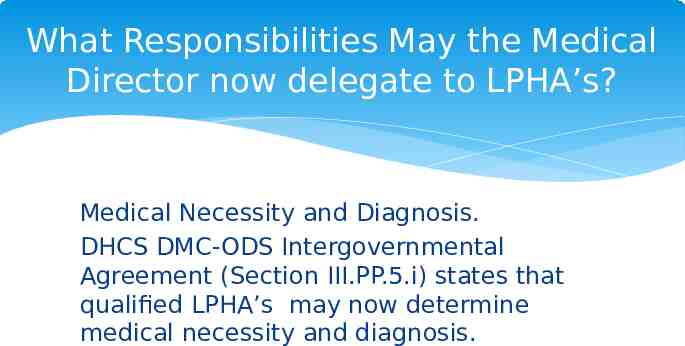
What Responsibilities May the Medical Director now delegate to LPHA’s? Medical Necessity and Diagnosis. DHCS DMC-ODS Intergovernmental Agreement (Section III.PP.5.i) states that qualified LPHA’s may now determine medical necessity and diagnosis.
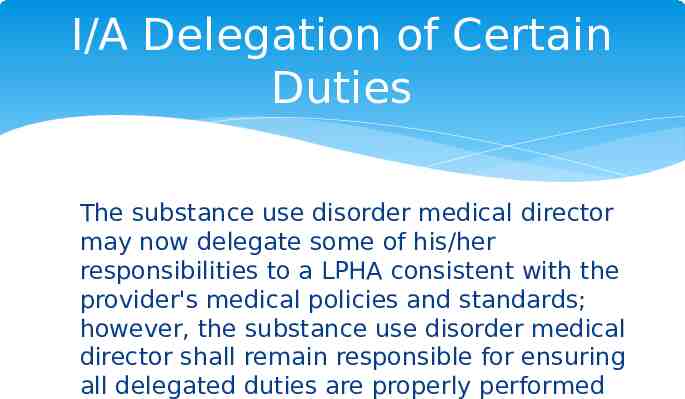
I/A Delegation of Certain Duties The substance use disorder medical director may now delegate some of his/her responsibilities to a LPHA consistent with the provider's medical policies and standards; however, the substance use disorder medical director shall remain responsible for ensuring all delegated duties are properly performed
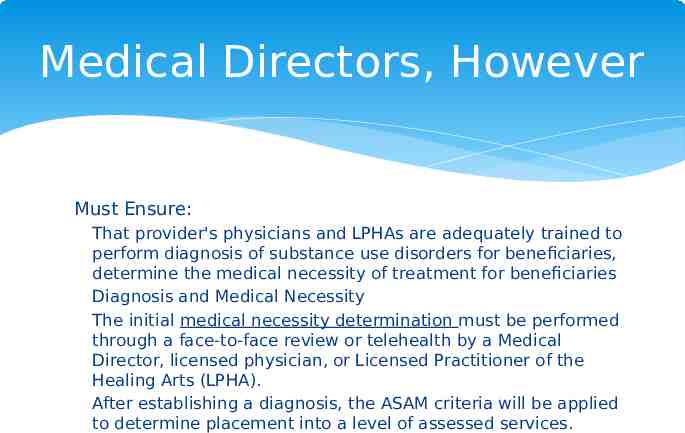
Medical Directors, However Must Ensure: That provider's physicians and LPHAs are adequately trained to perform diagnosis of substance use disorders for beneficiaries, determine the medical necessity of treatment for beneficiaries Diagnosis and Medical Necessity The initial medical necessity determination must be performed through a face-to-face review or telehealth by a Medical Director, licensed physician, or Licensed Practitioner of the Healing Arts (LPHA). After establishing a diagnosis, the ASAM criteria will be applied to determine placement into a level of assessed services.
I/A Delegation of Certain Duties Does the implementation of the Organized Delivery System Change any other responsibilities? No!
Responsibilities Under I/A In fact, the I/A reaffirms that Medical Director’s responsibilities shall, at a minimum, include the following: Ensure that physicians, registered nurse practitioners, and physician assistants follow the provider's medical policies and standards. Ensure that the medical decisions made by physicians are not influenced by fiscal considerations. Ensure that care provided by physicians, registered nurse practitioners, and physician assistants and meets the applicable standard of care. Ensure that physicians do not delegate their duties to non-physician personnel. Ensure that provider's physicians are adequately trained to perform other physician duties

And Develop and implement medical policies and standards for the provider.
DHCS Findings #2 The second commonly found deficiency is: Verification of the required five (5) Continuing Medical Education (CME) credits in addiction medicine each year
DHCS 22 CCR 51341.1(b)(28)(A)(iii) also requires that the Medical Director participate and provide documentation showing 5 hours of continuing education in addiction medicine each year.
Citations and Resources DHCS Technical Assistance Webinar September 6, 2018 The DHCS DMC-ODS Intergovernmental Agre ement Section III.PP.5.i. Title 22CCR 513.41(b) Title 22 CCR 51341.1. (h) DHCS Title 22 Drug Medi-Cal FAQ
Citations and Resources Public Policy Statement on Managed Care, A ddiction Medicine and Parity: Supplement for Physicians and Others on the Step-by-step U tilization Review Process Taubman Ph.D, S.,Dr. (2019, January 9). Drug Medi-CAL Organized Delivery System Quality Assurance Toolkit [PDF]. Sacramento: California Institute for Behavioral Health Solutions.
Questions/Comments Should you ever have any questions please feel free to contact EDCBH-SUDS QA/UR Supervisor at 530-621-6146 or at [email protected] For general information and questions or being added to the provider or stakeholder lists you may contact SUDS at [email protected]