The Michigan Upper Peninsula Critical Access Hospital HIT Network
24 Slides1.32 MB
The Michigan Upper Peninsula Critical Access Hospital HIT Network Implementation Project Donald A. Wheeler, FACHE Primary Investigator Moving Community Health To the 21st Century AHRQ 2006 Annual Patient Safety & Health Information Technology Conference June 5, 2006
Critical Access Hospital HIT Network Implementation Project Participants 10 Critical Access Hospitals Marquette General Health System (MGHS) Upper Peninsula Health Care Network (UPHCN) A 10-year history of working cooperatively Developing shared services and information systems
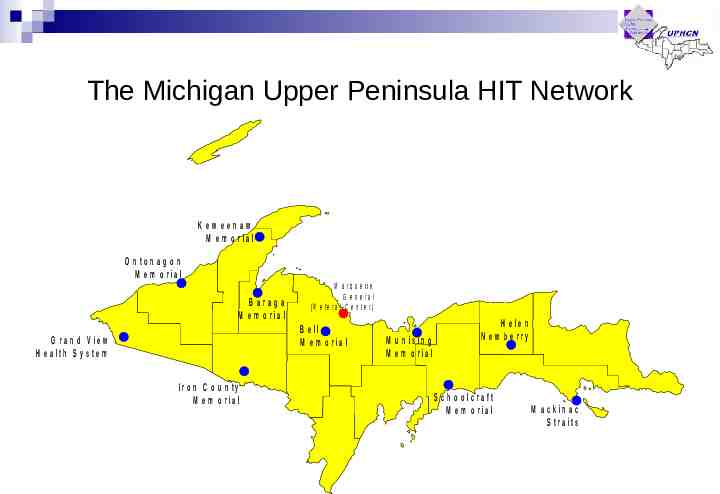
The Michigan Upper Peninsula HIT Network Kew eenaw M e m o r ia l O n to n a g o n M e m o r ia l B a ra g a M e m o r ia l M a rq u e tte G e n e ra l (R e fe ra l C e n te r ) B e ll M e m o r ia l G r a n d V ie w H e a lth S y s te m Ir o n C o u n ty M e m o r ia l M u n is in g M e m o r ia l H e le n N e w b e rry S c h o o lc ra ft M e m o r ia l M a c k in a c S tra its
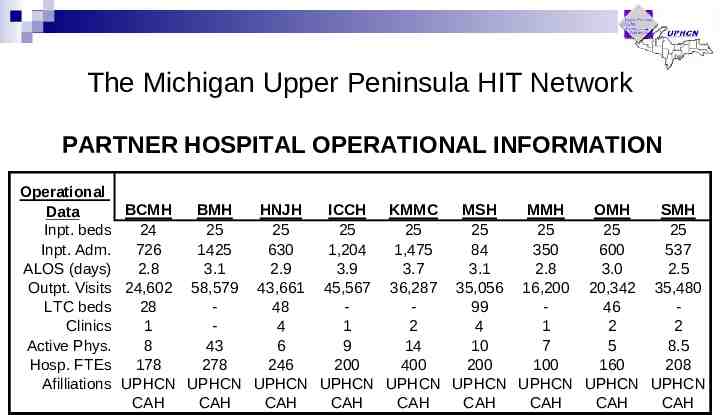
The Michigan Upper Peninsula HIT Network PARTNER HOSPITAL OPERATIONAL INFORMATION Operational BCMH BMH HNJH ICCH KMMC MSH MMH OMH SMH Data Inpt. beds 24 25 25 25 25 25 25 25 25 Inpt. Adm. 726 1425 630 1,204 1,475 84 350 600 537 ALOS (days) 2.8 3.1 2.9 3.9 3.7 3.1 2.8 3.0 2.5 Outpt. Visits 24,602 58,579 43,661 45,567 36,287 35,056 16,200 20,342 35,480 LTC beds 28 48 99 46 Clinics 1 4 1 2 4 1 2 2 Active Phys. 8 43 6 9 14 10 7 5 8.5 Hosp. FTEs 178 278 246 200 400 200 100 160 208 Afilliations UPHCN UPHCN UPHCN UPHCN UPHCN UPHCN UPHCN UPHCN UPHCN CAH CAH CAH CAH CAH CAH CAH CAH CAH
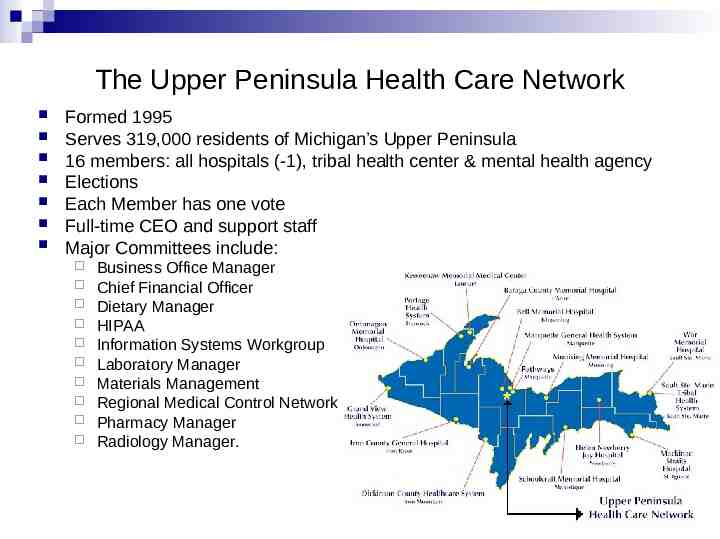
The Upper Peninsula Health Care Network Formed 1995 Serves 319,000 residents of Michigan’s Upper Peninsula 16 members: all hospitals (-1), tribal health center & mental health agency Elections Each Member has one vote Full-time CEO and support staff Major Committees include: Business Office Manager Chief Financial Officer Dietary Manager HIPAA Information Systems Workgroup Laboratory Manager Materials Management Regional Medical Control Network Pharmacy Manager Radiology Manager.
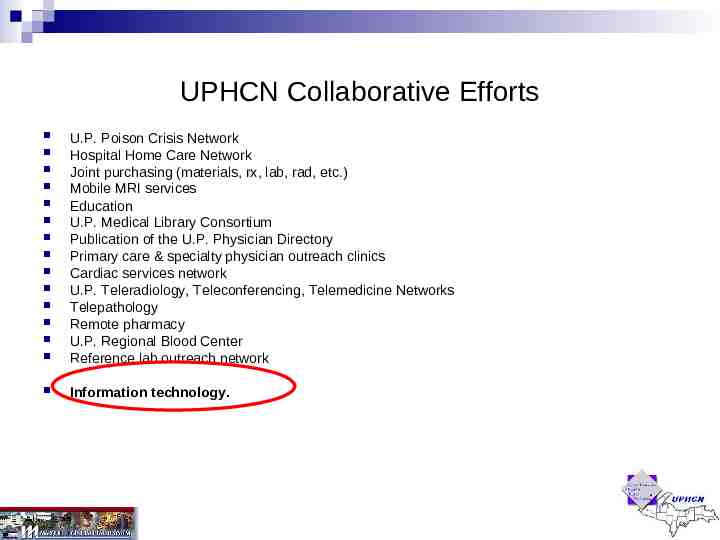
UPHCN Collaborative Efforts U.P. Poison Crisis Network Hospital Home Care Network Joint purchasing (materials, rx, lab, rad, etc.) Mobile MRI services Education U.P. Medical Library Consortium Publication of the U.P. Physician Directory Primary care & specialty physician outreach clinics Cardiac services network U.P. Teleradiology, Teleconferencing, Telemedicine Networks Telepathology Remote pharmacy U.P. Regional Blood Center Reference lab outreach network Information technology.
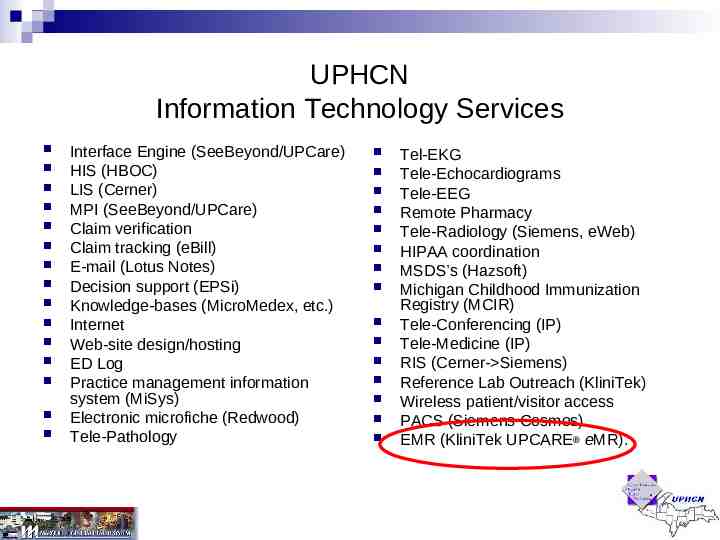
UPHCN Information Technology Services Interface Engine (SeeBeyond/UPCare) HIS (HBOC) LIS (Cerner) MPI (SeeBeyond/UPCare) Claim verification Claim tracking (eBill) E-mail (Lotus Notes) Decision support (EPSi) Knowledge-bases (MicroMedex, etc.) Internet Web-site design/hosting ED Log Practice management information system (MiSys) Electronic microfiche (Redwood) Tele-Pathology Tel-EKG Tele-Echocardiograms Tele-EEG Remote Pharmacy Tele-Radiology (Siemens, eWeb) HIPAA coordination MSDS’s (Hazsoft) Michigan Childhood Immunization Registry (MCIR) Tele-Conferencing (IP) Tele-Medicine (IP) RIS (Cerner- Siemens) Reference Lab Outreach (KliniTek) Wireless patient/visitor access PACS (Siemens Cosmos) EMR (KliniTek UPCARE eMR).
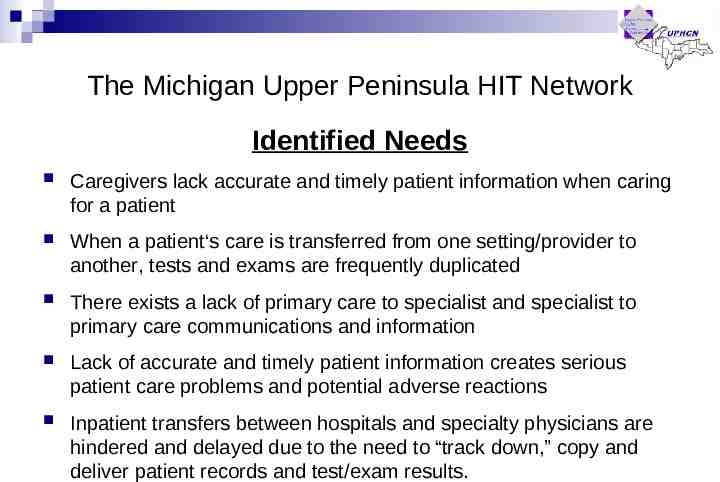
The Michigan Upper Peninsula HIT Network Identified Needs Caregivers lack accurate and timely patient information when caring for a patient When a patient‘s care is transferred from one setting/provider to another, tests and exams are frequently duplicated There exists a lack of primary care to specialist and specialist to primary care communications and information Lack of accurate and timely patient information creates serious patient care problems and potential adverse reactions Inpatient transfers between hospitals and specialty physicians are hindered and delayed due to the need to “track down,” copy and deliver patient records and test/exam results.
The Michigan Upper Peninsula HIT Network Purpose “To Improve patient safety and quality of care through the regional planning, development, and implementation of Health Information Technologies.”
The Michigan Upper Peninsula HIT Network Long-Term Goals 1. Assess quality of patient care, patient safety, and outcomes through consolidated patient clinical and care measures data collected by the Network HIT applications 2. Provide clinical data sharing among participating entities through high-speed connectivity and data compatibility across the Network Partners I.T. applications to support optimal care delivery.
The Michigan Upper Peninsula HIT Network Desired Outcomes Provide caregivers with as much information as possible when caring for the patient Eliminate/reduce number of duplicate tests and exams when a patient‘s care is transferred from one setting/provider to another Enhance primary care- specialist and specialist- primary care communications and information Improve care provided in Partner hospital emergency departments Improve inpatient transfers between Partner hospitals, Marquette General Hospital, and specialty physicians Enable the conduct of medication reconciliation when patients are transferred between facilities, emergency departments, and specialty and primary care physicians Eliminate hard-copy reports, paperwork, courier deliveries, and most types of handwritten clinical data by the end of the decade!
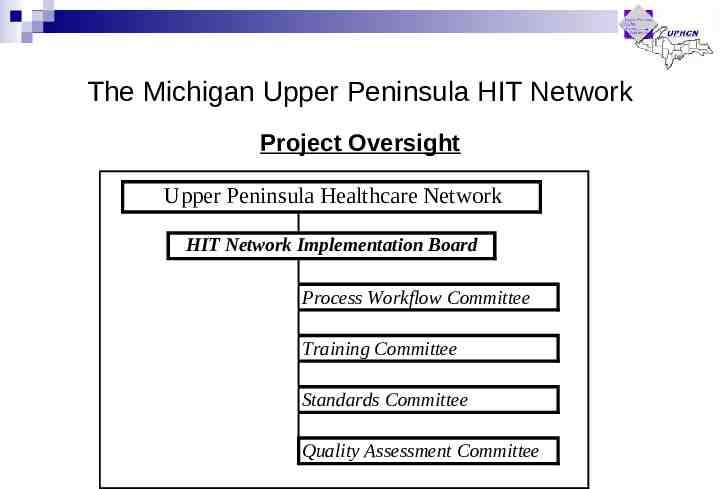
The Michigan Upper Peninsula HIT Network Project Oversight Upper Peninsula Healthcare Network HIT Network Implementation Board Process Workflow Committee Training Committee Standards Committee Quality Assessment Committee
The Michigan Upper Peninsula HIT Network Structuring the Solution UPHCN provides the organizational structure to solve technical issues relative to sharing patient information Across disparate systems Between independently owned/operated organizations Hospitals use their own Health Information Technology (HIT) within their facility: Registration Scheduling Results Order management Clinical documentation, etc Hospitals use UPCARE eMR at their facility to view clinical results on their patient from other participating facilities, including their own.
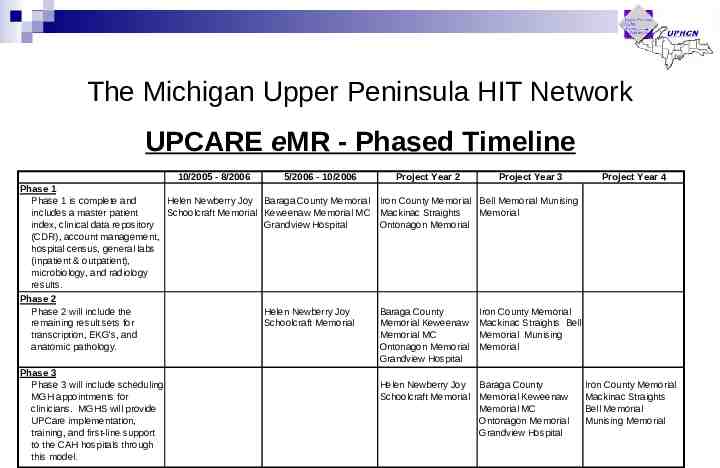
The Michigan Upper Peninsula HIT Network UPCARE eMR - Phased Timeline 10/2005 - 8/2006 Phase 1 Phase 1 is complete and Helen Newberry Joy includes a master patient Schoolcraft Memorial index, clinical data repository (CDR), account management, hospital census, general labs (inpatient & outpatient), microbiology, and radiology results. Phase 2 Phase 2 will include the remaining result sets for transcription, EKG's, and anatomic pathology. Phase 3 Phase 3 will include scheduling MGH appointments for clinicians. MGHS will provide UPCare implementation, training, and first-line support to the CAH hospitals through this model. 5/2006 - 10/2006 Project Year 2 Project Year 3 Project Year 4 Baraga County Memorial Iron County Memorial Bell Memorial Munising Keweenaw Memorial MC Mackinac Straights Memorial Grandview Hospital Ontonagon Memorial Helen Newberry Joy Schoolcraft Memorial Baraga County Memorial Keweenaw Memorial MC Ontonagon Memorial Grandview Hospital Iron County Memorial Mackinac Straights Bell Memorial Munising Memorial Helen Newberry Joy Baraga County Schoolcraft Memorial Memorial Keweenaw Memorial MC Ontonagon Memorial Grandview Hospital Iron County Memorial Mackinac Straights Bell Memorial Munising Memorial
UPHCN Information Technology In the beginning 1995 No connectivity between Members MGHS “Best of Breed” w/interface engine Upgrading clinical and financial systems Demand for expanding I.T. resulted in growing I.T. staff Other Members “Best of Breed” w/o interface engine Integrated “IBM 36” type systems for financials – no clinical systems Little or no I.T. staff Demand for I.T., but lacked capital and I.T. talent MGHS packaged their I.T. services and systems and offered to Members Many early adopters Installed everything from networks to clinical and billing systems Developed much of the data connectivity in use today Established long-term trust and working relations.
UPHCN Information Technology Today Hi-speed, private, secure network 70 physical sites (more than just UPHCN Members) Connects U.P. hospitals, providers, payers, patients Data needs Video needs 9100 user accounts Managed through MGHS-IT department Created working model, cost effective mechanism to access and share a host of systems and services Provide the foundation to build Local Health Information Technology (HIT) Regional Health Information Organization (RHIO).
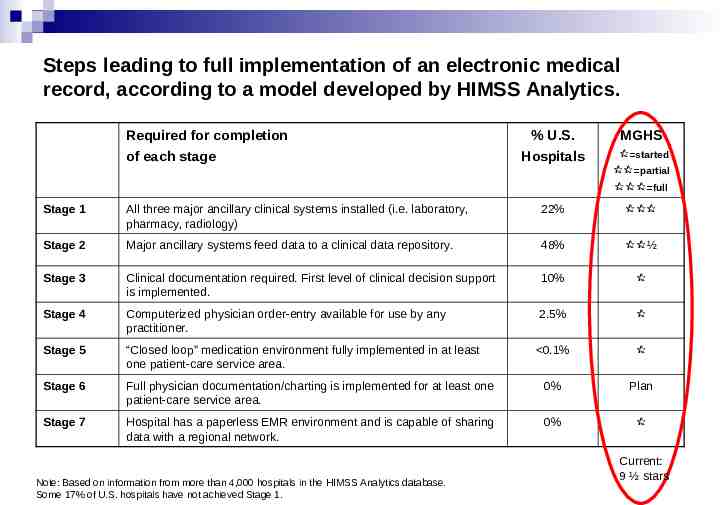
Steps leading to full implementation of an electronic medical record, according to a model developed by HIMSS Analytics. Required for completion of each stage % U.S. Hospitals MGHS started partial full Stage 1 All three major ancillary clinical systems installed (i.e. laboratory, pharmacy, radiology) 22% Stage 2 Major ancillary systems feed data to a clinical data repository. 48% ½ Stage 3 Clinical documentation required. First level of clinical decision support is implemented. 10% Stage 4 Computerized physician order-entry available for use by any practitioner. 2.5% Stage 5 “Closed loop” medication environment fully implemented in at least one patient-care service area. 0.1% Stage 6 Full physician documentation/charting is implemented for at least one patient-care service area. 0% Plan Stage 7 Hospital has a paperless EMR environment and is capable of sharing data with a regional network. 0% Note: Based on information from more than 4,000 hospitals in the HIMSS Analytics database. Some 17% of U.S. hospitals have not achieved Stage 1. Current: 9 ½ stars
EMR Development & MGHS Conclusions Big vendor systems costly: 10’s millions dollars Installations are not complete, therefore total costs unknown Technology platforms tend to be “closed” vs. “open” Limited by what vendor decides to do with product, i.e., little to no control over how product is developed Purchase 80% of what you don’t need or can’t use and only 20% of what you can use.
EMR Development & MGHS Direction Buy “Best-of-Suite”, Develop, and Integrate option Purchase clinical ancillary systems Build a Clinical Data Repository (CDR) Interface ancillary systems to the CDR Develop web-based user interface/application to access data in CDR Develop web-based order management & other EMR functions MGH aligned w/KliniTek to develop an EMR that would work across the U.P. Live on first version of UPCARE eMR 6/04 Today MGH has signed-up 65% physicians/allied health professionals 80% nursing professionals 1,219 UPCARE eMR users 10 Critical Access Hospitals 2 Pilots in-progress.
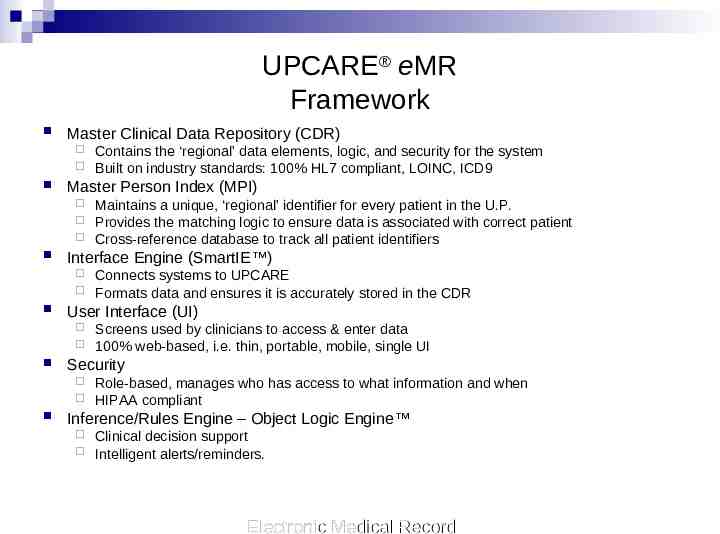
UPCARE eMR Framework Master Clinical Data Repository (CDR) Master Person Index (MPI) Screens used by clinicians to access & enter data 100% web-based, i.e. thin, portable, mobile, single UI Security Connects systems to UPCARE Formats data and ensures it is accurately stored in the CDR User Interface (UI) Maintains a unique, ‘regional’ identifier for every patient in the U.P. Provides the matching logic to ensure data is associated with correct patient Cross-reference database to track all patient identifiers Interface Engine (SmartIE ) Contains the ‘regional’ data elements, logic, and security for the system Built on industry standards: 100% HL7 compliant, LOINC, ICD9 Role-based, manages who has access to what information and when HIPAA compliant Inference/Rules Engine – Object Logic Engine Clinical decision support Intelligent alerts/reminders. Electronic Medical Record
UPCARE eMR Functionality Patient census Results Order management Common registration Enterprise procedures Office appointment Account Maintenance Bridge IP & OP settings Provide common account number for same visit to store results Scheduling General/nursing CPOE Ensuring results are associated with correct patient 100% Web-based Single UI Ultra-thin client Fast Portable & mobile. Electronic Medical Record
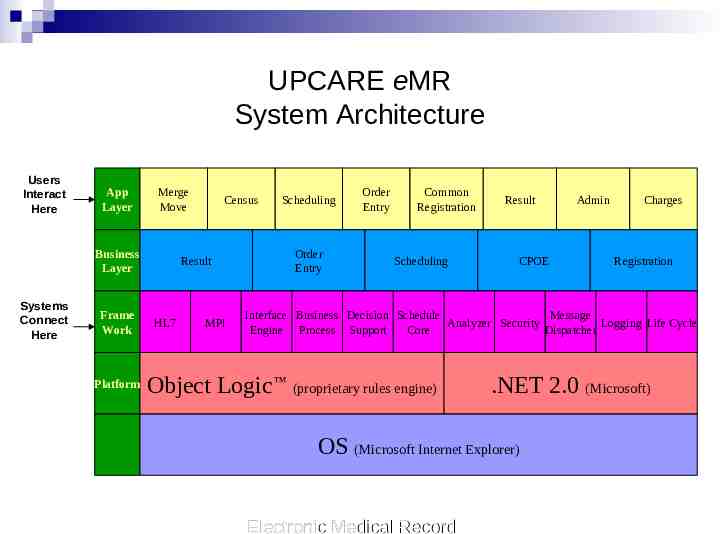
UPCARE eMR System Architecture Users Interact Here App Layer Merge Move Business Layer Systems Connect Here Frame Work Platform Census Result HL7 MPI Scheduling Order Entry Order Entry Common Registration Scheduling Result CPOE Admin Charges Registration Interface Business Decision Schedule Message Analyzer Security Logging Life Cycle Engine Process Support Core Dispatcher Object Logic (proprietary rules engine) .NET 2.0 (Microsoft) OS (Microsoft Internet Explorer) Electronic Medical Record
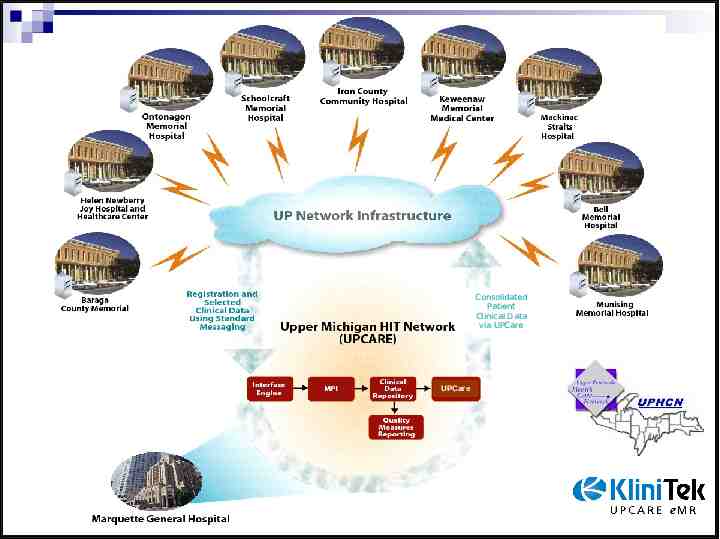
Consolidated Patient Clinical Data via UPCare UPCare
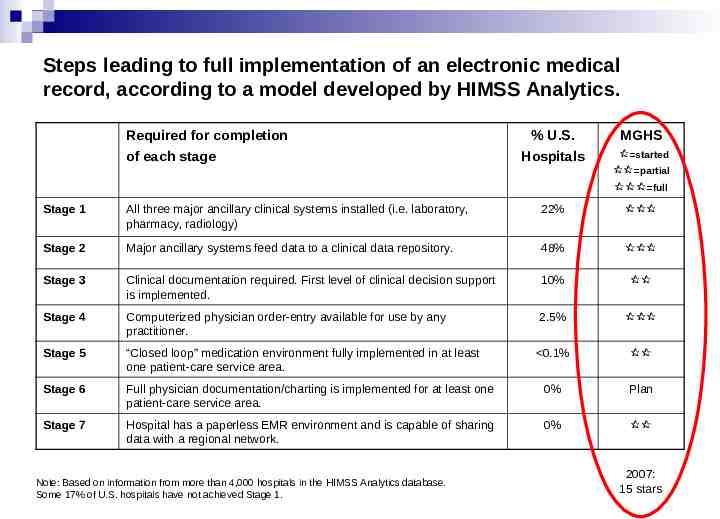
Steps leading to full implementation of an electronic medical record, according to a model developed by HIMSS Analytics. Required for completion of each stage % U.S. Hospitals MGHS started partial full Stage 1 All three major ancillary clinical systems installed (i.e. laboratory, pharmacy, radiology) 22% Stage 2 Major ancillary systems feed data to a clinical data repository. 48% Stage 3 Clinical documentation required. First level of clinical decision support is implemented. 10% Stage 4 Computerized physician order-entry available for use by any practitioner. 2.5% Stage 5 “Closed loop” medication environment fully implemented in at least one patient-care service area. 0.1% Stage 6 Full physician documentation/charting is implemented for at least one patient-care service area. 0% Plan Stage 7 Hospital has a paperless EMR environment and is capable of sharing data with a regional network. 0% Note: Based on information from more than 4,000 hospitals in the HIMSS Analytics database. Some 17% of U.S. hospitals have not achieved Stage 1. 2007: 15 stars