Introducing the Last Days of Life toolkit: recognition of the dying
14 Slides1.26 MB

Introducing the Last Days of Life toolkit: recognition of the dying patient and management planning

How we care for dying patients Insert patient story here Insert local data around care and management of dying patients PRESENTATION NAME – MONTH YYYY PRESENTER NAME 2
Last Days of Life Toolkit The purpose of the toolkit is to provide clinicians with the tools and support to ensure that all dying patients are recognised early, receive optimal symptom control, have social, spiritual and cultural needs addressed, and that bereavement support for families and carers occurs.

In line with Relevant NSW Health Policy Medication Handling in NSW Public Health Facilities – PD2013 043 Using Resuscitation Plans in End of Life Decisions – PD2014 030 ACSQHC National Consensus Statement: Essential Elements for Safe & High Quality End of Life Care National Standards Standard 1 – Governance for Safety and Quality in Health Service Organisations Standard 2 – Partnering with Consumers Standard 4 – Medication Safety Standard 6 – Care Coordination Standard 9 – Recognising and Responding to Clinical Deterioration in Acute Health Care
The tools Tools to assist the recognition of the dying patient and development of individualised management plans: Initiating last days of life management plan Comfort Observation and Symptom Assessment chart Care after death in hospital
Initiating last days of life management plan Identify dying patient and commence management planning, includes: Signs & symptoms of dying Mandatory criteria around assessment, communication and documentation Care planning Why would you consider the patient is dying within hours to days? Is deterioration unexpected or a predictable consequence of a known illness? Is there any treatable problem that has caused this deterioration? Who is involved in recognising the patient may be dying? Discussion between multidisciplinary team caring for the patient. Communication with patient and family Meet with patient and/or family/carer as soon as possible.
Triggers for initiating last days of life management plan It is essential to identify the dying patient in order to allow them and their family/carers to reorient their priorities, achieve their goals, and so that appropriate last days of life care can be provided. There are various patterns of death trajectory at the end of life, however, with the exception of precipitous, unexpected fatal events (e.g., massive haemorrhage), certain signs tend to be present when patients are actively dying that are applicable to a variety of conditions. There are some prognostic tools that provide prompts to identify people at risk of deteriorating and dying from one or more advanced conditions for example the Gold Standards Framework Prognostic Indicator “surprise question” and the Supportive and Palliative Care Indicators Tool (SPICT ) Ultimately it is up to the multi-disciplinary team to make a thorough assessment of the patient and be in agreement that reversible causes for the current condition have been considered and that the patient is likely to die.
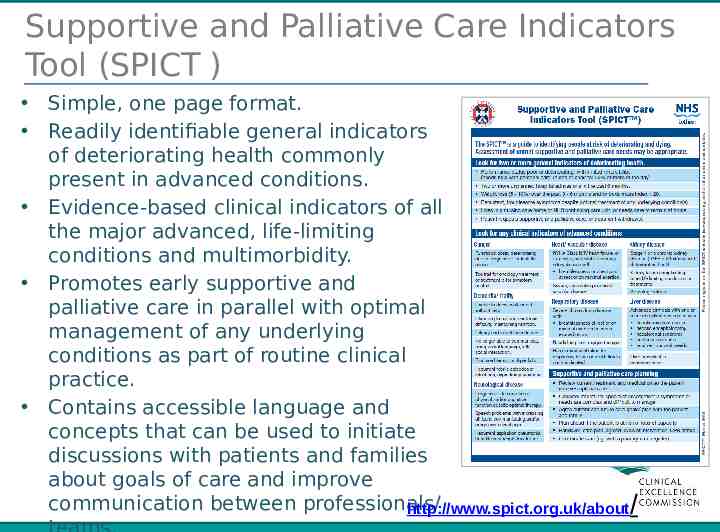
Supportive and Palliative Care Indicators Tool (SPICT ) Simple, one page format. Readily identifiable general indicators of deteriorating health commonly present in advanced conditions. Evidence-based clinical indicators of all the major advanced, life-limiting conditions and multimorbidity. Promotes early supportive and palliative care in parallel with optimal management of any underlying conditions as part of routine clinical practice. Contains accessible language and concepts that can be used to initiate discussions with patients and families about goals of care and improve communication between professionals/ http://www.spict.org.uk/about/
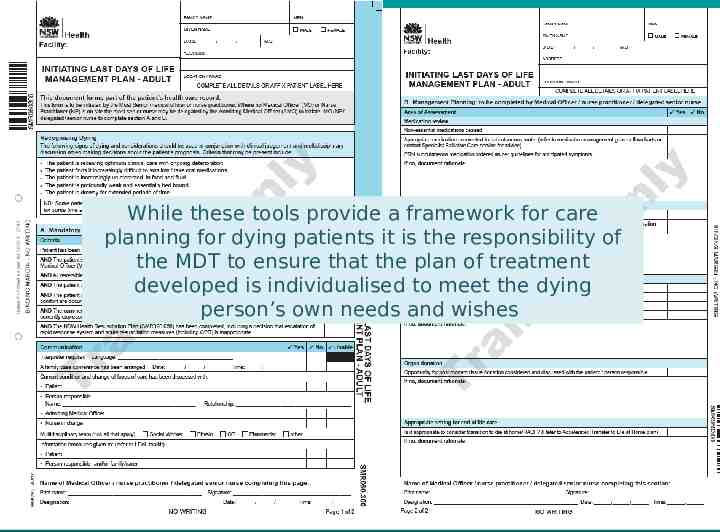
While these tools provide a framework for care planning for dying patients it is the responsibility of the MDT to ensure that the plan of treatment developed is individualised to meet the dying person’s own needs and wishes
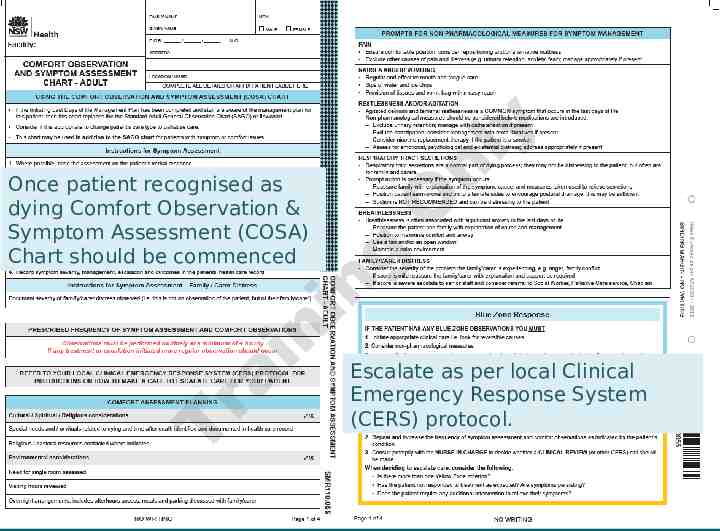
Once patient recognised as dying Comfort Observation & Symptom Assessment (COSA) Chart should be commenced Escalate as per local Clinical Emergency Response System (CERS) protocol. PRESENTATION NAME – MONTH YYYY PRESENTER NAME 10
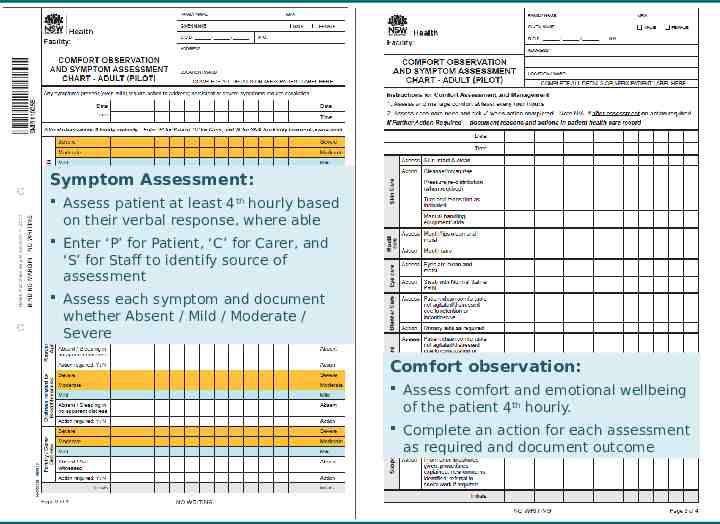
Symptom Assessment: Assess patient at least 4th hourly based on their verbal response, where able Enter ‘P’ for Patient, ‘C’ for Carer, and ‘S’ for Staff to identify source of assessment Assess each symptom and document whether Absent / Mild / Moderate / Severe Comfort observation: Assess comfort and emotional wellbeing of the patient 4th hourly. Complete an action for each assessment as required and document outcome
Care after death Care of a patient and their family doesn’t end when the patient dies. All organisations should have a policy for good practice for the care and viewing of the body after death. Staff should be aware of how to ensure timely verification and certification of death. Staff should also be aware that the coroner may need to be involved in particular cases. Medical and Nursing staff need to be familiar with: Local policies on care of the deceased patient NSW health policy PD2015 040 Death-Verification of Death & Medical Certificate of Cause of Death NSW health policy PD2010 054 Coroners Cases and the Coroners Act 2009
Remember . It is what we are already/should be doing for our patients and their families i.e. best practice Empowers and promotes confidence in nursing staff and junior doctors to be their patients’ advocates Means the patient/family/carer is heard and has control Enhances MDT working Enhances the quality of documentation Should give staff no extra work, if anything it should save staff time

Contact Details Clinical Excellence Commission Bernadette King – Program Lead [email protected] [email protected]