+ “The Basics of Vision Impairments and Functional Applications” Tina
70 Slides340.04 KB
"The Basics of Vision Impairments and Functional Applications” Tina Mastrangelo, MCD, CCC-SLP, Senior SLP Janine E. Pacheco, PT, DPT, C/NDT, Melissa Lorenzo, B.S Brianna Morris, SPT HealthSouth Rehab Hospital of Largo
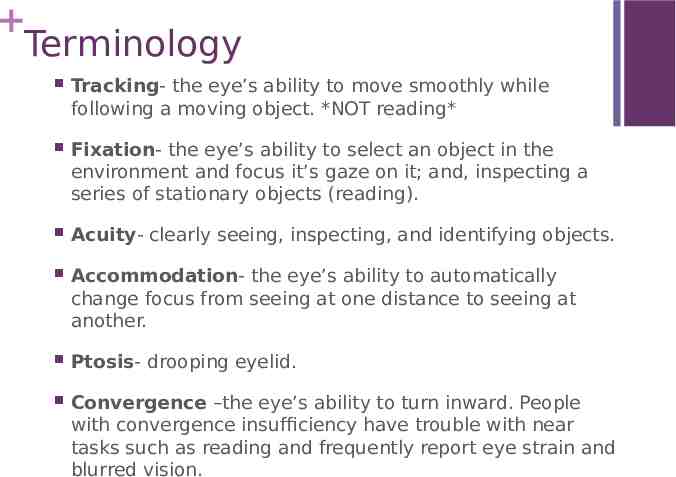
Terminology Tracking- the eye’s ability to move smoothly while following a moving object. *NOT reading* Fixation- the eye’s ability to select an object in the environment and focus it’s gaze on it; and, inspecting a series of stationary objects (reading). Acuity- clearly seeing, inspecting, and identifying objects. Accommodation- the eye’s ability to automatically change focus from seeing at one distance to seeing at another. Ptosis- drooping eyelid. Convergence –the eye’s ability to turn inward. People with convergence insufficiency have trouble with near tasks such as reading and frequently report eye strain and blurred vision.

the ability to use both eyes as a team Divergenceand be able to turn the eyes out toward a far object. Diplopia- when two images of the same object are perceived by one or both eyes.(double vision) Fusion- the union of images from each eye into a single image. Strabismus- a misalignment of the eyes. The eyes don’t point at the same object together. Tropia-always present Esotropia- when one or both eyes point inward. Exotropia- When one or both eyes point outward. Phoria- you have to break fusion Esophoria- when one or both eyes point inward Exophoria- when one or both eyes point outward

Nystagmus- rhythmic oscillations or tremors of the eyes which occur independently of the normal eye movement Occlusion- to block out light. An eye can be completely or partially blocked. Occlusion is often used to promote the use of one eye or both eyes. (ex: patching, squinting) Suppression- Stimulated by dissimilar stimuli or when noncorresponding retinal areas are stimulated by similar stimuli or the other is temporarily inhibited or suppressed to prevent confusion. Binocular Vision- Ability of both eyes to work together to achieve proper focus, depth perception and range of vision. Monocular Vision- Ability of one eye to focus. No depth perception (when changing surfaces). Saccades - Rapid shifts , or little jumps, of the eyes from object to object allowing quick localization of movements in the periphery. The ability of the eye to change fixation from point to point.

Extra Ocular Muscles

Visual Pathway

Visual Pathway

Scope of practice: ST According to ASHA’s Practice Policy on Scope of Practice in Speech-Language Pathology, it is in an SLP’s scope of practice to asses and treat: Cognition attention memory sequencing problem solving executive functioning Language literacy (reading, writing, spelling)

Scope of practice: OT AOTA resource manual: Practice Guidelines for Adults With Low Vision Use remaining vision to participate in desired occupations Support independent lives Modify home environment to facilitate safe participation in ADLs Recommend adaptive devices and assistive technology (optical and non-optical devices) (www.aota.org) The AOTA recognizes that occupational therapists help address visual impairment difficulties Activities of Daily Living Evaluate specific daily task Evaluate environment, and recommend modifications Recommend adaptive devices and assistive technology (optical and non-optical devices)

Scope of practice: PT Examining individuals with impairment, functional limitation, and disability or other health-related conditions. Tests and measures may include the following: environmental, home, and work (job/school/play) barriers gait, locomotion, and balance neuromotor development and sensory integration sensory integrity work (job/school/play), community, leisure integration or reintegration (including instrumental activities of daily living) Design, implement, and modify therapeutic interventions

Fixation The eye’s ability to select an object in the environment and focus it’s gaze on it; and inspecting a series of stationary objects (reading). Assessment Hold stick with a round bead 16-20 inches away from face Ask them to look at the bead for five seconds Observe their ability to focus If they are unable to complete task: Have them hold out their own thumb & stare at it for 5 seconds. Input from their own hand may increase the ability to focus Scoring WFL: Able to stare at bead for 5 seconds with no apparent eye movement. Impaired: Unable to stare at bead for 5 seconds and/or has abnormal eye movement

Fixation Treatment Activities to encourage holding gaze on a single object Start with short duration and increase accordingly Goal: for eyes to fixate and not dart in any other direction Achieving attention to a single object Notes: “Fixation” requires “attention” Make it fun – Staring contest 1.2.3 GO! Use bright colors and familiar objects Reduce stimulation in environment Provide postural stability

Saccades Definition: Rapid shifts, or little jumps, of the eyes from object to object allowing quick localization of movements in the periphery. The ability of the eye to change fixation from point to point. Implications: Reading Losing their place often skipping lines rereading lines words appearing to jump around the page letter order confusion. Poor hand-eye coordination, i.e. ball throwing and catching, self-feeding, writing Impaired safety

Saccades Assessment Hold two sticks, with different colored beads on top (i.e red and green), about shoulder width apart. Ask them to hold their head still and look at one of the colored beads (red). While they fixate on the red bead, move the other bead (green) up or down. Then ask them to look at the other bead. Repeat this process until you have assessed their visual pattern. Look for accuracy, under or over shooting, nystagmus (shaky movements), extended search time, ability or inability to isolate eyes from head movements, and ability or inability to shift into all fields of gaze

Saccades Treatment Have them call out letters from two columns on opposite sides of the page Change the distance between the letters by increasing blank space or adding more columns. Trail making Yardstick Activity Focus on both small and large saccadic training Vestibular based movement activities with demands for saccadic skills Always watch for speed and accuracy of fixations on targets

Column Activity 3 5 7 8 2 9 6 1 4 7 5 1 9 6 3 7 Try anything alternating i.e. words, colors, names, objects

Trail Making Activity 25 circles distributed over a sheet of paper Explain and demonstrate task on a separate sheet of paper Give a worksheet (Part A, then B) Part A : circles are numbered 1-25 Part B : Circles are labeled with both 1-13 and A-L. Direction: Draw a line to connect circles in ascending order Pt. draws lines to connect 1 to A, A to 2, 2 to B, etc. Record time it takes them to finish worksheet. (Baseline – Treatment – Reassessment)

Small Precise Saccadic Movements Puzzles Word puzzles Newspaper cancellation tasks Last letter cancellation For right hemiparesis Wall fixation

Large Saccadic Training Dynavision and similar training devices http://dynavisioninternational.com/ Head and eye shifts Descriptive walking Search Strategies Large Table Cards Wii Tennis

Visual Fields The part of space where objects can be seen in the peripheral even though the person is fixating their gaze on one single object ahead of them. Broken in nasal (medial) and temporal (lateral) hemi fields Temporal (lateral) hemi field is much larger

Central Field Also called peripheral field Highly detailed area of the retina 5 around fixation point Responsible for Detailed vision Reading Recognizing faces Detecting colors Highly sensitive to light Low sensitivity to motion

Peripheral Field The total area around central vision Becomes a secondary visual process to central vision. This process is then used as general spatial orientation system and is integrated into the sensory-motor feedback loop Characterized by: High sensitivity to movement Low sensitivity to light and detail

Visual Field WNL: 50 -60 upward 70 -75 downward 60 nasally/medial 90 -110 temporally/laterally

Field Loss vs. Visual Neglect Visual Neglect Visual Field Loss Physical loss of visual field to one side Decreased Perceptual field Also Called: Homonymous hemianopsia Pt. with both have a worse prognosis for recovery, due to difficulty learning to compensate Attention impairment where pt. is unable to attend to one side of their body Also Called Hemi-spatial neglect Hemiagnosia Hemi-neglect Unilateral neglect Hemi-inattention Unilateral visual inattention Neglect syndrome

How Lesions Effect the Visual Field Level 1 lesion- Can lose sight fully in one eye Level 2-4 lesions – Cortical blindness Treatment: Compensate- NOT regain function

Visual Field Loss Treatment Determine available range Use of target localization tasks to train them to make large eye movements and systematic scanning strategies Incorporate efficient ROM/head turning training with PT and OT treatment Use of visual/auditory anchors Colored electric tape on table edges, doorways (red for left, green for right) Placing objects that provide auditory feedback on the affected side (alarm clock, phone) Appropriate challenge only (Safety first) Compensate first to reduce stress Grade activities up as skill increases

Visual Field Loss or Cut Assessment Have pt. cover one eye and fixate on an object in front of them Stand behind them with a long wand Ask them to tell you when they see something in their field of view and slowly bring the wand into their view from behind them at various angles, including: top, bottom, horizontal, diagonal approach to test each quadrant. Present target multiple times to confirm deficit. Be cautious not to let them see your arm move because they may guestimate when they will see the wand based on your body movement Repeat with other eye and both eyes together Scoring WFL: They see wand within appropriate degree measures Impairment: They don’t see the wand in their peripheral field within the specified degrees.
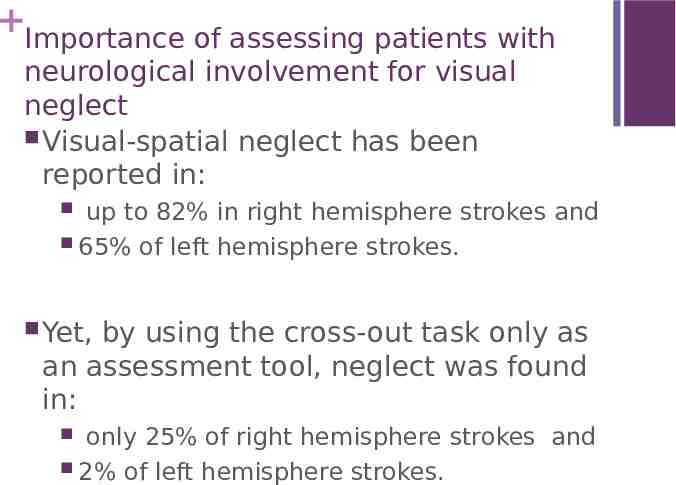
Importance of assessing patients with neurological involvement for visual neglect Visual-spatial neglect has been reported in: up to 82% in right hemisphere strokes and 65% of left hemisphere strokes. Yet, by using the cross-out task only as an assessment tool, neglect was found in: only 25% of right hemisphere strokes and 2% of left hemisphere strokes.

Moderatel y severe Peri-personal – Their world within arms reach Least severe Extra-personal – The world beyond arms reach Personal – their own body awareness Most severe Neglect

Visual Field Loss Treatment SLP’s Targets: Communication targeting – identification of object/picture/word/paragraphs – midline, right, left Impacts swallowing treatment ex: ability to recognize labial loss, pocketing, etc; Neck posturing Cognition - Attention, focus, safety judgement – Fixation and Saccadic Eye Movement Training Social interaction- pragmatics – eye contact, turn-taking More – think in and out of the box

Visual Field Loss Treatment PT Examples: Mobility training Safety awareness Central and Peripheral training Head and eye turns with gait retraining Postural/Trunk midline positioning Balance Car scanning More – think in and out of the box

Visual Field Loss Treatment OT Examples: Activities of daily living – Dressing, selffeeding, toileting Safety awareness Body awareness in transfers, dressing Reach/Extension Independent living skills Store scanning/shopping Money Management Driving More – think in and out of the box

Technologies: Interactive Metronome DynaVision Visual Prism Restoration Treatment glasses – specialized opthomologist neuroophthomologists

Visual Neglect Treatment Increase Self awareness of deficits grading Have client grade how they think they will perform How long will it take? What percentage will you get correct? Do you understand the activity? Will you need to ask more questions? What might effect your performance Have client re-grade themselves after they’ve completed the task

Visual Neglect Treatment Ideas Red Velcro Strip Red guides on side of page Tracking printed words from book on tape Vibrating pager - Set to vibrate on effected side every 12 seconds Place items on effected side and have patient look for them and retrieve them. Marking Money counting Checker Have each box of a grid with a X Board patients manipulate tokens vertically and horizontally across board

Visual Neglect Treatment Use of stimuli known to activate the affected side of the brain Left brain: use letters and numbers Right brain: use shapes and blocks Environmental modifications at home Incorporate motor movements of the affected side PT: clenching and unclenching affected hand during gait retraining OT: Use the affected arm as a perceptual anchor for full visual field scanning during performance of ADLs

Vergence Eye teaming – or using both eyes together efficiently Eye teaming is a reflex related to accommodation Accommodation- eye’s ability to automatically change focus from seeing at one distance to seeing at another. Convergence – with accommodation Divergence – relaxation of accommodation This reflex allows object fuse into single and clear, both at a distance and near. Impairment of vergence leads to: Dioplia, or double vision Confusion Phorias- misalignment of eyes Strabismus – noticeable eye turns in or out Suppression- the brain ignores all or part of an image in order to avoid dioplia Amblyopia – brain disregards most information coming from one or both eyes

Convergence The eye’s ability to turn inward. People with convergence insufficiency have trouble with near tasks such as reading and frequently report eye strain and blurred vision. Assessment Hold a colorful target approximately 16 inches away from the pt’s nose Instruct the pt to keep there eyes on the target as it moves closer to them and to tell you when they see double. Slowly move the target towards the pt’s face. Observe the pt’s eyes to see when one of the deviates from the target, signifying the point where the pt should see double. Scoring WNL: deviation when target is 3-4 inches from pt’s nose WFL: deviation when target is 4-6 inches from pt’s nose Impaired: deviation when target is more than 6 inches from pt’s nose.

Convergence Treatment Brock String A white string approx. 10-15 ft. long with three beads of various colors Tie one end of string to a stationary objects such as a door knob of cabinet Have pt. hold the other end at the tip of their nose Method 2 Bead positions six inches, 18 inches and four feet from the loose end Push gaze to focus on first bead. Strings should cross Hold for 10 seconds Repeat on 2nd and 3rd beads Repeat entire process 5 times Method 2 Place 1st bead at the place of double vision Place 2nd bead at the place of single vision Have patient focus on each Method 3 See treatment hand outs

Convergence Tasks Jump Convergence Give patient two different color pencils and position them approx. 5 feet in front of a blank wall. Have pt. hold one pencil in left hand with their arm fully extended in front of the face. Hold the other pencil right hand and position midway between pt.’s nose and the other pencil. Look at the pencil that is further away. Pt . should see the closer one in double. Look at the closer pencil. Pt. should see the further pencil in double Have patient bring both pencils closer to their face and look at each of them again. Repeat this exercise until patient is unable to avoid double vision when looking directly at one of the pencils. Dotted Card Draw a straight line in the across the middle a sheet of paper Draw 5 or more dots equally spaced along the line with different color inks Position the paper in front of pt’s face so that the line extends outward so they can see the dots on the line. Have pt. look at the furthest dot for 10 seconds. The rest of the dots should form a blurry letter A. Move to the next closest dot, while maintaining a single image of the furthest dot. Focus on the second farthest dot for 10. Continue moving closer, looking at each dot for 10 seconds until the pt can no longer maintain a single image of the dot they are focusing on. The blurry A shape should gradually transform into a blurry V-like shape as the pt. focus on points that are closer to their nose.

Divergence Assessment Position pt in front of your left side, where they can look over your shoulder. Have pt. look at a pencil topper approx. 6 inches in front of them. Next have pt look at an object behind you. Observe how the pts eyes turn in and out between convergence and divergence. Repeat with pt positioned on right side.

Divergence Treatment Divergence “Dynamic divergence” http://www.forbestvision.com/eye-exerc ises-for-myopia-dynamic-divergence / Divergence Use & convergence /fusion ipad http://www.forbestvision.com/dynamicfixation-trainer-fusion-in-divergencecon vergence/

Ocular Alignment Alignment is crucial to coordination/function of both eyes. If unaligned, pt. may experience double vision, vertigo, etc. Assessment Sit directly in front of pt. at midline. Instruct pt. to look into your eyes. Shine pen light between pt.’s eyes from 16-20 inches away Observe if the reflections in pt.’s eyes are in approximately the same positions. Scoring WFL: light reflects in the same position in each eye (typically in the center of each pupil) Impaired: light reflects in different position in each eye (strabismus of one or both eyes)

Ocular Range of Motion Assessment Hold a stick with a bead on top approximately 16-20 inches from pt’s face. Instruct pt’s to keep their eyes on the bead everywhere it goes while keeping their head still Move bead through the horizontal, vertical, and diagonal planes, holding 5 seconds between each movement. *slow and steady* Observe the pt’s eye movements to see if they complete the full range or if their eyes drift instead Repeat with each eye individually and together Scoring WFL: Able to follow target through full range Impaired: if pt. is unable to follow bead

Smooth Pursuits Movements that allow the image to stay in focus on the retina while tracking a moving target. Quality of ROM Assessed in conjunction with ROM During ROM assessment: Observe the pt’s eye movements. Do they jerk, shake, or have erratic/ballistic movements. Scoring WFL: Movements are smooth while tracking bead Impaired: Eyes jerk, have nystagmus (shaky movements) or move erratically.

Treatment for Alignment, ROM and Smooth Pursuits Medication Surgical SLP treatments Acquired alignment impairments are different from congenital deficits. If problem is due to muscle imbalance, begin eye exercises, such as ROM exercises If problem is due to double vision occlude the affected eye ** Begin fusion exercises Place an object where the pt can see it without double vision, then slowly move the object into the pt’s double vision range. Adaptation of lifestyle

Treatment for Alignment, ROM and Smooth Pursuits Therapist’s Role: Visual tracking exercises Move head with eyes stable Move eyes with head stable Complete exercises with eyes closed Turn head right and scan left, and vice versa Grid searches Follow lines on ceilings and walls Track people walking pen light

Visual Spatial Skills Skills used to understand directional concepts in space Signs and Symptoms Difficulty distinguishing left and right Lack of coordination and balance Reverses letters or numbers when writing or copying Does not cross midline when doing tasks Gets lost following directions

Visual Orientation Laterality: Directionality Awareness of the two body sides and knowing they are different. Awareness of up, down, ahead, behind, and any combination there after Consists of two orientations: Internal Self Awareness i.e. left and right hands Projection into the external visual space i.e. Understanding the difference between the left and right side of the room. ** If a pt’s internal self awareness is impaired, their concept of external visual space will also be impaired. **

Visual Orientation Assessment Asses pt’s awareness of left, right, up, down, ahead, behind with both auditory and visual tasks. Reading of minimal pairs with graphemes that have similar orthographic representations. i.e. ben, den, pen, qen If visual orientation is impaired letter decoding will be impaired.

Visual Orientation Tx Incorporate: sequencing, auditory comprehension reading comprehension upper extremity movement with laterality Encourage crossing of midline Examples: Catch and throw a ball with the left and right hands Look left – look right Place all the red items on your left and yellow ones on the right Go down the hall and turn right and tell me what picture is on the left

Bilateral Integration Ability to use both sides of the body separately and/or simultaneously i.e. typing, walking Must have a solid visual orientation foundation Using both hands to put on a shirt

Visual Analysis/ Visual Discrimination Ability to identify, sort, organize, store, and recall information from visual stimuli. Includes: Figure Ground Visual Form Recognition/ Discrimination and Constancy Visual Closure S/S Literacy Impairment Easily distracted Visual Spatial Memory Attention Impairment Visual Sequential Memory Difficulty understanding directions/ sequencing Visualization

Figure Ground Ability to attend and search for specific visual information or ignoring irrelevant information. i.e searching for a specific word or sentence in a paragraph, specific tool in the tool box, or railing in a bathroom. Treatment examples: Hidden picture puzzle Where’s Waldo puzzle Word Search Cancellation exercises App: http://tactustherapy.com/app/vat/

Visual Form Recognition/ Discrimination and Constancy Ability to discriminate differences in form including size, shape, color and orientation i.e CAT Cat cat; (Which one is lower case?) Which is more water? The water in the glass or the water in the bowl? Of these 2, which is larger? Treatment examples: Tetris Recognition of word similarities with variation of orthographic forms i.e. Horse HORSE horse

Visual Closure The ability to recognize visual stimuli which cues the pt to determine what an object or word should look like. i.e. Being able to complete a word or picture that is partially obstructed, such as words on a road sign or pictures on a warning sign. Treatment examples: Trail making with dots, letter, numbers, or words Choose the missing piece given F:3

Visual Spatial Memory Ability to recall the spatial location of an object or stimuli. The ability to be able to recall, identify, or reproduce a design or dominant feature of an object. Example: Being able to picture a lost object; seeing a printed word and developing a mental picture to the corresponding object. Treatment examples: Memory Card Game, Reduplication of bicolored block designs without a visual reference

Visual Sequential Memory Ability to view and recall a sequence of numbers, letters, objects in the order they were presented. i.e recalling a phone number, how to spell a medication name, or dosage instructions. Treatment example: Electronic Simon Says

Visualization Ability to mentally manipulate a previously viewed stimuli. i.e. deciding if a flattened box will fit an object you want to ship, if a walker will fit through a doorway, or if there is enough room to safely stand up between the chair and a supportive surface (table, grab bar, therapist) Treatment examples: Tangram puzzles Pegboard Functional mobility around hospital, office, home with prompts to check visualization accuracy

Visual Midline Shift Syndrome “mismatch between spatial information received through ambient visual process and kinesthetic, proprioceptive, and vestibular system” Ambient visual process From the peripheral portion of the retina to the midbrain (sensory-motor loop) to occipital cortex (feed-forward) Responsible for body awareness in space Results in a tilt in the horizontal space causing balance deficits Visual Midline

VMSS Assessment Patient position: sitting or standing Therapist: Move an object horizontally in front of patient’s facial plane Ask patient to tell you when it is directly in front of their nose Move an object vertically in front of patient’s facial plane Ask patient to tell you when it is directly at eye level Result: Perception to the left means visual midline has shifted to that direction resulting in right neglect Perception of eye level when target is above eye level means there was a posterior shift resulting in backward lean * Shift is typically away from neurologically affected side

VMSS Treatment Neuro-opthamologists Prescription of yoked prisms OT Changes orientation, and concept of midline Performance of ADLs in sitting and standing position with yoked prism PT Gait retraining with yoked prism Static and dynamic balance training in sitting and standing with yoked prism

VMSS Treatment Allow patient success 70%-80% of the time OT: Parquetry blocks Copy a pattern Increase challenge by progressively increasing number of blocks Puzzles Discourage trial and error Hidden picture puzzle Highlight magazines to Where’s Waldo? Complete the picture Tracing

VMSS Treatment PT: Visualizing direction Have pt give the therapist directions from point A to point B Follow the directions (even if wrong) Have the pt perform the task, then report it to therapy Real life hidden picture Teach scanning strategies during performance of task

Visual-Motor Integration Aka. Hand-eye coordination Coordination of visual perceptual skills with gross and fine motor movements i.e. Written word repetition S/S Poor organization Poor awareness of mistakes Sloppy writing Close working distance Treatment examples: Interactive Metronome Utilize visual stimuli / guides Rotations

Visual-Auditory Integration Visual-auditory integration Visual-auditory integration involves correlating visual information with information heard. i.e. such as seeing a word and saying it aloud, or hearing a word and writing it down. Involves auditory and visual skills in: Attention, Discrimination, Memory, Figure ground, and Closure Signs and symptoms: Slow reading speed Requires frequent repetition of directions Poor spelling ability Difficulty learning to read phonetically Difficulty relating phonemes to print symbol.

Missing things on one side Hemi neglect and/or field cut Head turn to one side Hemi neglect and/or field cut Head tilt Restriction of gaze (usually superior oblique), nystagmus or Double Vision Closing one eye intermittently Double Vision Closing one eye all the time Oculomotor nerve (CN III) palsy Squinting in the distance Distance acuity, double vision, divergence insufficiency Headache when watching TV or words getting jumbled up when completing activity close to pt Convergence insufficiently, near acuity, decreased saccadic movement

Eyes asymmetrical Double vision, restriction of gaze, erratic tracking Excessive blinking Convergence insufficiency, distance/near acuity Difficulty identifying faces Distance acuity *** Over/under shoots when reaching for an item Double vision Pushing toward weaker side Visual midline shift Dizziness with tracking Erratic Oculomotor skills Unable to track laterally past midline Abducens nerve (CN VI) palsy, double vision Keeping eyes closed Decreased visual attention, double vision, eye strain, contrast sensitivity issues

Documentation for vision treatments Discipline specific goals OT: Complete ADLs PT: Balance, Stand, Walk ST: Communicate, Read, Think Keep the goals you are doing, but add the modality and facilitation of the vision prior to and throughout the task.

Resources Information on hemianopsia and visual neglect Trail Making App www. Hemianopsia.net https://www.apptweak.com/trail-making-test/ipad/australia/ en/app-marketing-app-store-optimization-aso/report/ 689951658 Visual Perceptual/Ocular Motor activities https://www.pinterest.com/kirstenot/ot-visual-perception-oc ular-motor-activities /