Social Security Number Removal Initiative (SSNRI) Safety Net Provider
15 Slides217.40 KB
Social Security Number Removal Initiative (SSNRI) Safety Net Provider Open Door Forum 04/19/17
Background The Health Insurance Claim Number (HICN) is a Medicare beneficiary’s identification number, used for paying claims and for determining eligibility for services across multiple entities (e.g. Social Security Administration (SSA), Railroad Retirement Board (RRB), States, Medicare providers and health plans, etc.) The Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 mandates the removal of the Social Security Number (SSN)-based HICN from Medicare cards to address current risk of beneficiary medical identity theft The legislation requires that CMS mail out new Medicare cards with a new Medicare Beneficiary Identifier (MBI) by April 2019 2
SSNRI Program Goals Primary goal: To decrease Medicare Beneficiary vulnerability to identity theft by removing the SSN-based HICN from their Medicare identification cards and replacing the HICN with a new Medicare Beneficiary Identifier (MBI) In achieving this goal CMS seeks to: Minimize burdens for beneficiaries Minimize burdens for providers Minimize disruption to Medicare operations Provide a solution to our business partners that allows usage of HICN and/or MBI for business critical data exchanges Manage the cost, scope, and schedule for the project 3
Complex IT Systems affecting Providers, Partners, and Beneficiaries Along with our partners, CMS will address complex systems changes for over 75 systems, conduct extensive outreach & education activities and analyze the many changes that will be needed to systems and business processes Affected stakeholders include: Federal partners, States, Beneficiaries, Providers, and Plans Other key stakeholders, such as billing agencies, advocacy groups, data warehouses, etc. CMS has been working closely with partners and stakeholders to implement the SSN Removal Initiative 4
Implementation of SSNRI 5
Solution Concept: Medicare Beneficiary Identifier (MBI) The solution for SSNRI must provide the following capabilities: 1. Generate MBIs for all beneficiaries: Includes existing (currently active, deceased or archived) and new beneficiaries 2. Issue new, redesigned Medicare cards: New cards containing the MBI to existing and new beneficiaries 3. Modify systems and business processes: Required updates to accommodate receipt, transmission, display, and processing of the MBI CMS will use a MBI generator to: Assign 150 million MBIs in the initial enumeration (60 million active and 90 million deceased/archived) and generate a unique MBI for each new Medicare beneficiary Generate a new unique MBI for a Medicare beneficiary whose identity has been compromised 6
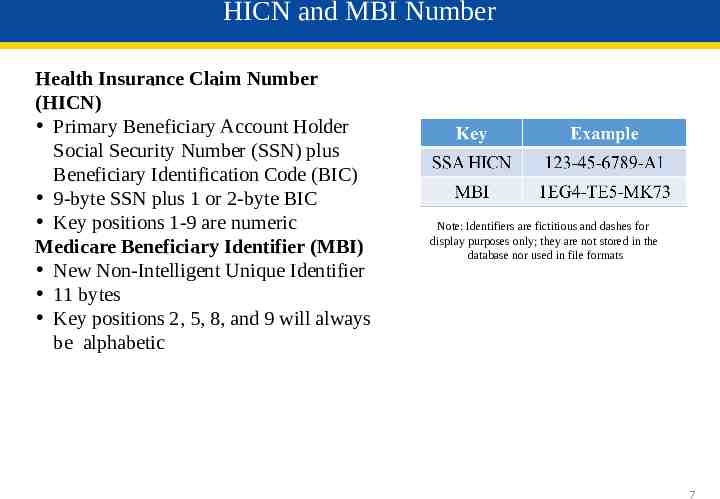
HICN and MBI Number Health Insurance Claim Number (HICN) Primary Beneficiary Account Holder Social Security Number (SSN) plus Beneficiary Identification Code (BIC) 9-byte SSN plus 1 or 2-byte BIC Key positions 1-9 are numeric Medicare Beneficiary Identifier (MBI) New Non-Intelligent Unique Identifier 11 bytes Key positions 2, 5, 8, and 9 will always be alphabetic Note: Identifiers are fictitious and dashes for display purposes only; they are not stored in the database nor used in file formats 7
MBI Characteristics The Medicare Beneficiary Identifier will have the following characteristics: The same number of characters as the current HICN (11), but will be visibly distinguishable from the HICN Contain uppercase alphabetic and numeric characters throughout the 11 digit identifier Occupy the same field as the HICN on transactions Be unique to each beneficiary (e.g. husband and wife will have their own MBI) Be easy to read and limit the possibility of letters being interpreted as numbers (e.g. Alphabetic characters are upper case only and will exclude S, L, O, I, B, Z) Not contain any embedded intelligence or special characters Not contain inappropriate combinations of numbers or strings that may be offensive CMS anticipates that the MBI will not be changed for an individual unless the MBI is compromised or other limited circumstances still undergoing review 8
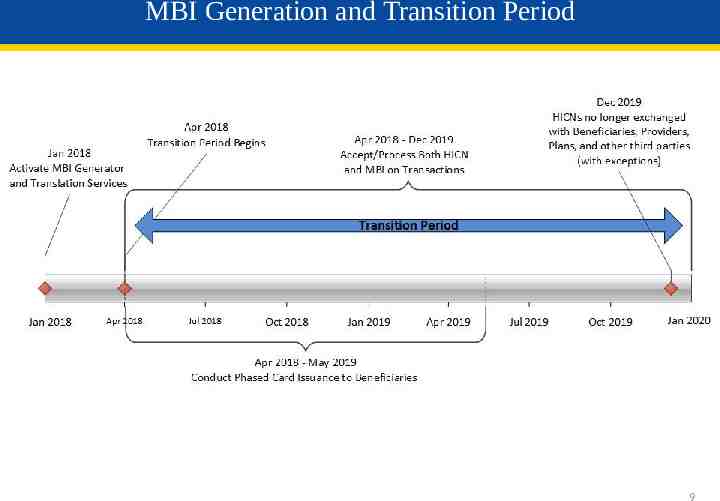
MBI Generation and Transition Period 9
SSNRI Transition Periods CMS will complete its system and process updates to be ready to accept and return the MBI on April 1, 2018 All stakeholders who submit or receive transactions containing the HICN must modify their processes and systems to be ready to submit or exchange the MBI by April 1, 2018. Stakeholders may submit either the MBI or HICN during the transition period CMS will accept, use for processing and return to stakeholders either the MBI or HICN, whichever is submitted, during the transition period In addition, beginning October 2018 through the end of the transition period, when a valid and active HICN is submitted on Medicare fee-forservice claims both the HICN and the MBI will be returned on the remittance advice The transition period will run from April 2018 through December 31, 2019 10
SSNRI Exceptions After the Transition Period Once the transition period is over, you’ll still be able to use the HICN in these situations: 1. Appeals Appeal requests and related forms will be accepted with either a HICN or MBI 2. Reports Incoming Reports to CMS* (i.e., Quality reporting, Disproportionate Hospital data requests) Outgoing Reports from CMS (i.e., Provider Statistical & Reimbursement Report, Accountable Care Organization Reports) 3. Retroactive enrollments 4. Span-date claims 11X-Inpatient Hospital, 32X-Home Health and 41X-Religious Non-Medical Health Care Institution claims with a “From Date” prior to the end of the transition period (12/31/19) 5. Adjustments Use the HICN for adjustments where you originally submitted a HICN on the claim (i.e. PDE, Risk Adjustment and Encounter data) 6. Incoming information requests (i.e. inquiries, Medicare Secondary Payer information requests, Requests for Medical Documentation, etc.) 7. Incoming premium payments (i.e. (Part A premiums, Part B premiums, Part D income related monthly adjustment amounts, etc.) *note: we will use the HICN on these reports until further notice 11
SSNRI Card Issuance CMS will begin issuing new Medicare cards for existing beneficiaries after the initial enumeration of MBIs; roughly 60 million beneficiaries The gender and signature line will be removed from the new Medicare cards The Railroad Retirement Board who will issue their new cards to RRB beneficiaries We will work with states that currently include the HICN on Medicaid cards to remove the Medicare ID or replace it with a MBI CMS will conduct intensive education and outreach to all Medicare beneficiaries and their agents to help prepare for this change 12
Outreach and Education CMS will provide outreach and education to: Approximately 60 million beneficiaries, their agents, advocacy groups and caregivers Health Plans The provider community (1.5M providers) States and Territories Key stakeholders, vendors & other partners CMS will ensure that we involve all stakeholders in our outreach and education efforts through their existing vehicles for communication (e.g. Open Door Forums, HPMS notices, etc.) 13
Health Plan Specific Information What do I need to do? Continue to review the HPMS memos for SSNRI related information: SSNRI Related Memo – November 18th Participate in our Open Door Forums Check our SSNRI website for other information: http://go.cms.gov/ssnri 14
Final Thoughts Thank you for participating in this discussion today Please submit any additional information to the SSNRI team mailbox at: [email protected] 15