Catheter-associated Urinary Tract Infection (CAUTI) Toolkit
32 Slides799.40 KB
Catheter-associated Urinary Tract Infection (CAUTI) Toolkit Activity C: ELC Prevention Collaboratives Carolyn Gould, MD MSCR Division of Healthcare Quality Promotion Centers for Disease Control and Prevention Disclaimer: The findings and conclusions in this presentation are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Outline Background – Impact – HHS Prevention Targets – Pathogenesis – Epidemiology Prevention Strategies – Core – Supplemental Measurement – Process – Outcome Tools for Implementation/Resources/References
Background: Impact of CAUTI Most common type of healthcare-associated infection – 30% of HAIs reported to NHSN – Estimated 560,000 nosocomial UTIs annually Increased morbidity & mortality – Estimated 13,000 attributable deaths annually – Leading cause of secondary BSI with 10% mortality Excess length of stay –2-4 days Increased cost – 0.4-0.5 billion per year nationally Unnecessary antimicrobial use Hidron AI et al. ICHE 2008;29:996-1011 Givens CD, Wenzel RP. J Urol 1980;124:646-8 Klevens RM et al. Pub Health Rep 2007;122:160-6 Green MS et al. J Infect Dis 1982;145:667-72 Weinstein MP et al. Clin Infect Dis 1997;24:584-602 Foxman B. Am J Med 2002;113:5S-13S Cope M et al. Clin Infect Dis 2009;48:1182-8 Saint S. Am J Infect Control 2000;28:68-75
Background: Urinary Catheter Use 15-25% of hospitalized patients 5-10% (75,000-150,000) NH residents Often placed for inappropriate indications Physicians frequently unaware In a recent survey of U.S. hospitals: – 50% did not monitor which patients catheterized – 75% did not monitor duration and/or discontinuation Weinstein JW et al. ICHE 1999;20:543-8 Munasinghe RL et al. ICHE 2001;22:647-9 Warren JW et al. Arch Intern Med 1989;149:1535-7 Saint S et al. Am J Med 2000;109:476-80 Benoit SR et al. J Am Geriatr Soc 2008;56:2039-44 Jain P et al. Arch Intern Med 1995;155:1425-9 Rogers MA et al J Am Geriatr Soc 2008;56:854-61 Saint S. et al. Clin Infect Dis 2008;46:243-50
Background: HHS Metrics and Prevention Targets # of symptomatic UTI / 1,000 urinary catheter days as measured in NHSN – National 5-Year Prevention Target: 25% decrease from baseline Appendix G in HHS plan discusses a new type of metric, the standardized infection ratio (SIR) http://www.hhs.gov/ophs/initiatives/hai/prevtargets.html http://www.hhs.gov/ophs/initiatives/hai/appendices.html
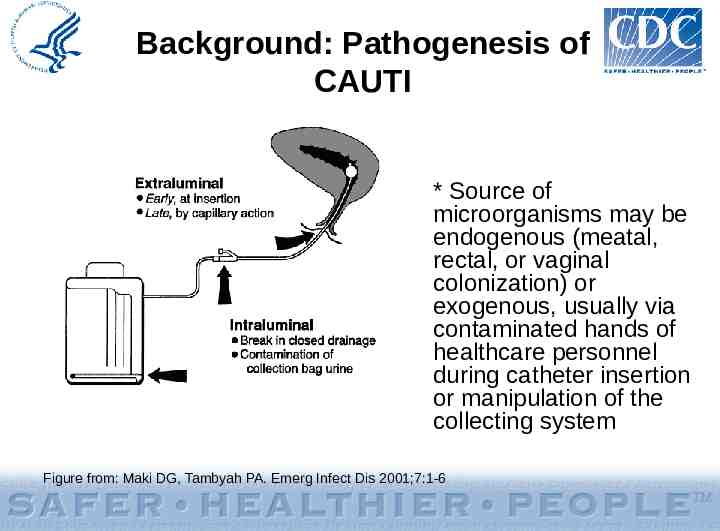
Background: Pathogenesis of CAUTI * Source of microorganisms may be endogenous (meatal, rectal, or vaginal colonization) or exogenous, usually via contaminated hands of healthcare personnel during catheter insertion or manipulation of the collecting system Figure from: Maki DG, Tambyah PA. Emerg Infect Dis 2001;7:1-6
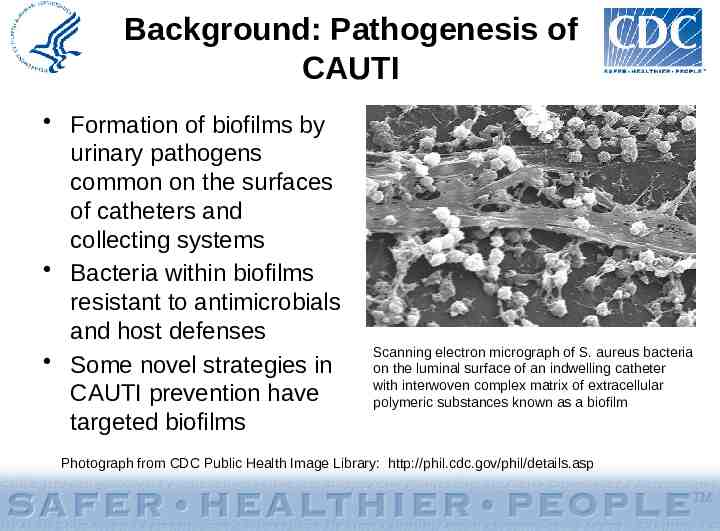
Background: Pathogenesis of CAUTI Formation of biofilms by urinary pathogens common on the surfaces of catheters and collecting systems Bacteria within biofilms resistant to antimicrobials and host defenses Some novel strategies in CAUTI prevention have targeted biofilms Scanning electron micrograph of S. aureus bacteria on the luminal surface of an indwelling catheter with interwoven complex matrix of extracellular polymeric substances known as a biofilm Photograph from CDC Public Health Image Library: http://phil.cdc.gov/phil/details.asp
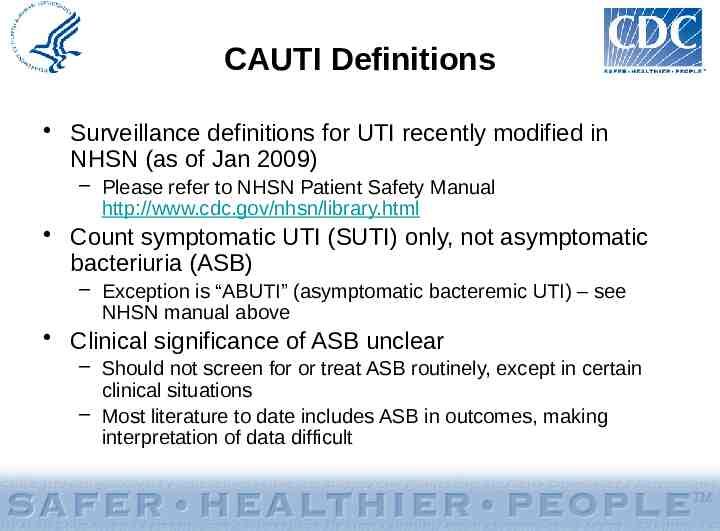
CAUTI Definitions Surveillance definitions for UTI recently modified in NHSN (as of Jan 2009) – Please refer to NHSN Patient Safety Manual http://www.cdc.gov/nhsn/library.html Count symptomatic UTI (SUTI) only, not asymptomatic bacteriuria (ASB) – Exception is “ABUTI” (asymptomatic bacteremic UTI) – see NHSN manual above Clinical significance of ASB unclear – Should not screen for or treat ASB routinely, except in certain clinical situations – Most literature to date includes ASB in outcomes, making interpretation of data difficult
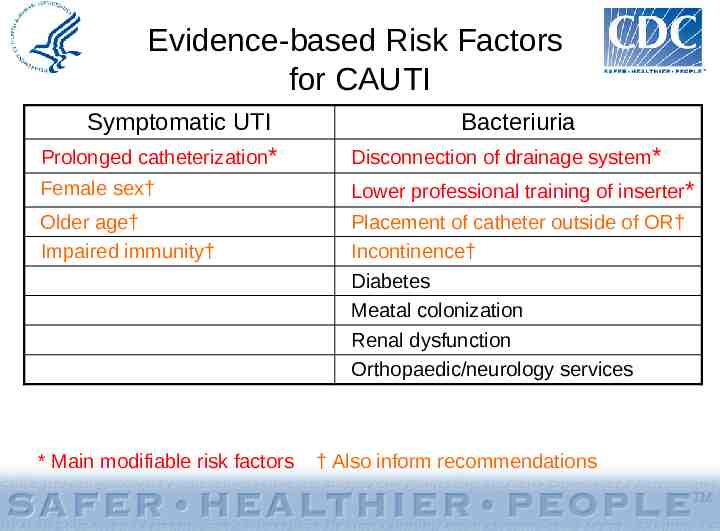
Evidence-based Risk Factors for CAUTI Symptomatic UTI Prolonged catheterization* Disconnection of drainage system* Female sex† Lower professional training of inserter* Older age† Impaired immunity† Placement of catheter outside of OR† Incontinence† Diabetes Meatal colonization Renal dysfunction Orthopaedic/neurology services * Main modifiable risk factors Bacteriuria † Also inform recommendations
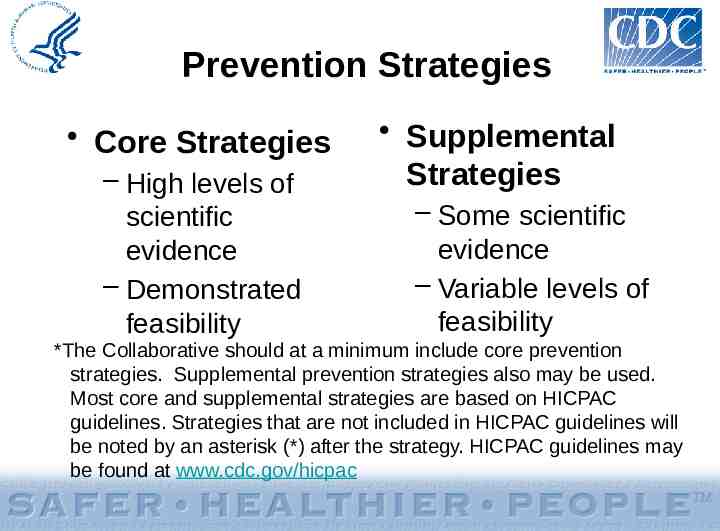
Prevention Strategies Core Strategies – High levels of scientific evidence – Demonstrated feasibility Supplemental Strategies – Some scientific evidence – Variable levels of feasibility *The Collaborative should at a minimum include core prevention strategies. Supplemental prevention strategies also may be used. Most core and supplemental strategies are based on HICPAC guidelines. Strategies that are not included in HICPAC guidelines will be noted by an asterisk (*) after the strategy. HICPAC guidelines may be found at www.cdc.gov/hicpac
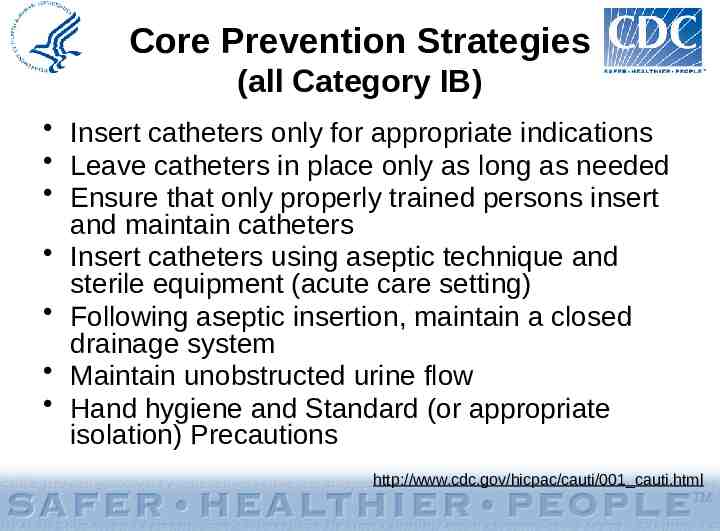
Core Prevention Strategies (all Category IB) Insert catheters only for appropriate indications Leave catheters in place only as long as needed Ensure that only properly trained persons insert and maintain catheters Insert catheters using aseptic technique and sterile equipment (acute care setting) Following aseptic insertion, maintain a closed drainage system Maintain unobstructed urine flow Hand hygiene and Standard (or appropriate isolation) Precautions http://www.cdc.gov/hicpac/cauti/001 cauti.html
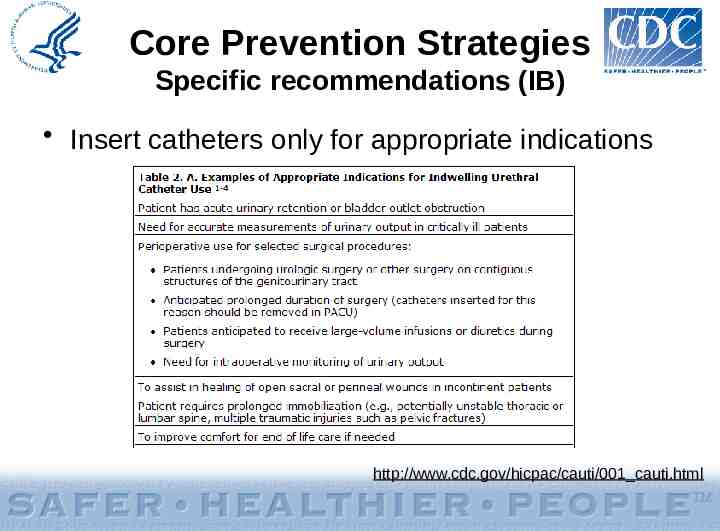
Core Prevention Strategies Specific recommendations (IB) Insert catheters only for appropriate indications http://www.cdc.gov/hicpac/cauti/001 cauti.html
Core Prevention Strategies Specific recommendations (IB) Insert catheters only for appropriate indications – Minimize use in all patients, particularly those at higher risk of CAUTI and mortality (women, elderly, impaired immunity) – Avoid use for management of incontinence – Use catheters in operative patients only as necessary http://www.cdc.gov/hicpac/cauti/001 cauti.html
Core Prevention Strategies Specific recommendations (IB) Leave catheters in place only as long as needed – Remove catheters ASAP postoperatively, preferably within 24 hours, unless there are appropriate indications for continued use http://www.cdc.gov/hicpac/cauti/001 cauti.html
Core Prevention Strategies Specific recommendations (IB) Insert catheters using aseptic technique and sterile equipment (acute care setting) – Perform hand hygiene before and after insertion – Use sterile gloves, drape, sponges, antiseptic or sterile solution for periurethral cleaning, single-use packet of lubricant jelly – Properly secure catheters http://www.cdc.gov/hicpac/cauti/001 cauti.html
Core Prevention Strategies Specific recommendations (IB) Following aseptic insertion, maintain a closed drainage system – If breaks in aseptic technique, disconnection, or leakage occur, replace catheter and collecting system using aseptic technique and sterile equipment – Consider systems with preconnected, sealed catheter-tubing junctions (II) – Obtain urine samples aseptically http://www.cdc.gov/hicpac/cauti/001 cauti.html
Core Prevention Strategies Specific recommendations (IB) Maintain unobstructed urine flow – Keep catheter and collecting tube free from kinking – Keep collecting bag below level of bladder at all times (do not rest bag on floor) – Empty collecting bag regularly using a separate, clean container for each patient. Ensure drainage spigot does not contact nonsterile container. http://www.cdc.gov/hicpac/cauti/001 cauti.html
Core Prevention Strategies: Specific recommendations (IB) Implement quality improvement programs to enhance appropriate use of indwelling catheters and reduce risk of CAUTI Examples: ―Alerts or reminders ―Stop orders ―Protocols for nurse-directed removal of unnecessary catheters ―Guidelines/algorithms for appropriate perioperative catheter management http://www.cdc.gov/hicpac/cauti/001 cauti.html
Supplemental Prevention Strategies: Examples Consideration of alternatives to indwelling urinary catheterization (II) Use of portable ultrasound devices for assessing urine volume to reduce unnecessary catheterizations (II) Use of antimicrobial/antiseptic-impregnated catheters (IB, after first implementing core recommendations for use, insertion, and maintenance ) http://www.cdc.gov/hicpac/cauti/001 cauti.html The following slides will provide further details on supplemental strategies
Supplemental Prevention Strategies: Alternatives to Indwelling Catheterization Intermittent catheterization – consider for: – Patients requiring chronic urinary drainage for neurogenic bladder Spinal cord injury Children with myelomeningocele – Postoperative patients with urinary retention – May be used in combination with bladder ultrasound scanners External (i.e., condom) catheters – consider for: – Cooperative male patients without obstruction or urinary retention http://www.cdc.gov/hicpac/cauti/001 cauti.html
Supplemental Prevention Strategies: Bladder Ultrasound Scanners Rationale: fewer catheterizations lower risk of UTI 2 studies of adults with neurogenic bladder undergoing intermittent catheterization Inpatient rehabilitation centers Fewer catheterizations per day but no reported differences in UTI – Significant study limitations: likely underpowered; UTIs undefined Polliak T et al. Spinal Cord 2005;43:615-19 Anton HA et al. Arch Phys Med Rehab 1998;79:172-5
Supplemental Prevention Strategies: Antimicrobial/Antiseptic-Impregnated Urinary Catheters Considered using if CAUTI rates not decreasing after implementing a comprehensive strategy – First implement core recommendations for use, insertion, and maintenance – Ensure compliance with core recommendations http://www.cdc.gov/hicpac/cauti/001 cauti.html
Supplemental Prevention Strategies: Silver-Coated Catheters Decreased risk of bacteriuria compared to standard latex catheters in a meta-analysis of RCTs Significant differences for silver alloy but not silver oxide-coated catheters Effect greater for patients catheterized 1 week Mixed results in observational studies in hospitalized patients – Most used laboratory-based outcomes (bacteriuria) – 1 positive, 2 negative, 5 inconclusive http://www.cdc.gov/hicpac/cauti/001 cauti.html
Supplemental Prevention Strategies: Silver-Coated Catheters One study in a burn referral center found a decrease in SUTI Pre-intervention catheters standard latex Intervention group had silver-impregnated catheters and had new catheters inserted on admission under nonemergent sterile conditions – “The improved results in time period 2 are probably due to the combination of these two changes in therapy.” Newton et al. Infect Control Hosp Epidemiol 2002;23:217-8
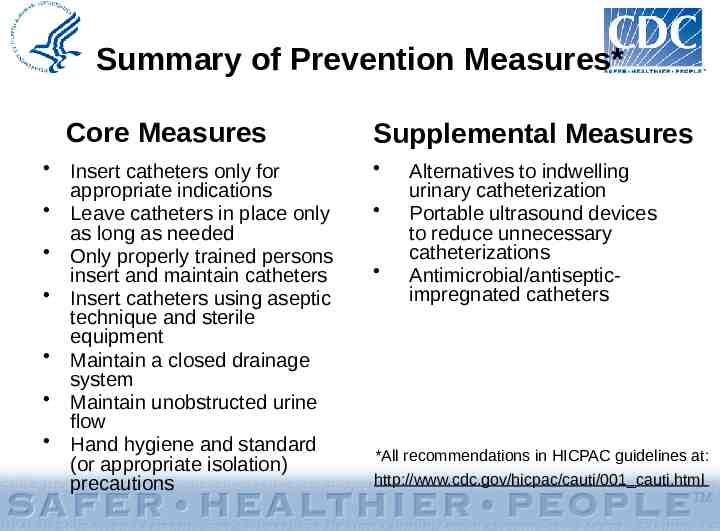
Summary of Prevention Measures* Core Measures Insert catheters only for appropriate indications Leave catheters in place only as long as needed Only properly trained persons insert and maintain catheters Insert catheters using aseptic technique and sterile equipment Maintain a closed drainage system Maintain unobstructed urine flow Hand hygiene and standard (or appropriate isolation) precautions Supplemental Measures Alternatives to indwelling urinary catheterization Portable ultrasound devices to reduce unnecessary catheterizations Antimicrobial/antisepticimpregnated catheters *All recommendations in HICPAC guidelines at: http://www.cdc.gov/hicpac/cauti/001 cauti.html
Strategies NOT recommended for CAUTI prevention Complex urinary drainage systems (e.g., antisepticreleasing cartridges in drain port) Changing catheters or drainage bags at routine, fixed intervals (clinical indications include infection, obstruction, or compromise of closed system) Routine antimicrobial prophylaxis Cleaning of periurethral area with antiseptics while catheter is in place (use routine hygiene) Irrigation of bladder with antimicrobials Instillation of antiseptic or antimicrobial solutions into drainage bags Routine screening for asymptomatic bacteriuria (ASB) http://www.cdc.gov/hicpac/cauti/001 cauti.html
Measurement: Examples of Process Measures Compliance with hand hygiene Compliance with educational program Compliance with documentation of catheter insertion and removal Compliance with documentation of indications for catheter placement http://www.cdc.gov/hicpac/cauti/001 cauti.html
Measurement: Recommended Outcome Measures Examples of metrics: – Number of CAUTI per 1000 catheter-days – Number of BSI secondary to CAUTI per 1000 catheter-days – Catheter utilization ratio (urinary catheter-days/patient-days) x 100 Use CDC/NHSN definitions for numerator data (SUTI only): http://www.cdc.gov/nhsn/library.html http://www.cdc.gov/hicpac/cauti/001 cauti.html
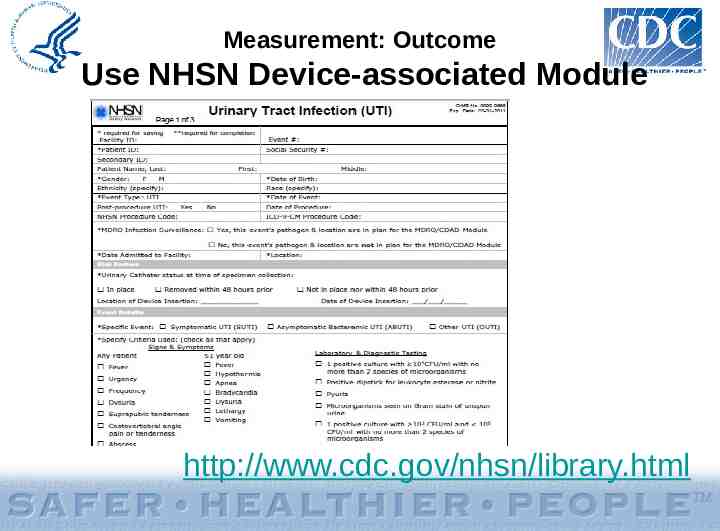
Measurement: Outcome Use NHSN Device-associated Module http://www.cdc.gov/nhsn/library.html
Measurement Considerations May need to consider alternative metrics (in addition to standard rates by device days) to demonstrate a reduction in CAUTIs if catheter days (denominators) greatly reduced with interventions Alternative denominator examples: – Patient days on unit – Numbers of catheters inserted
Evaluation Considerations Assess baseline policies and procedures Areas to consider – Surveillance – Prevention strategies – Measurement Coordinator should track new policies/practices implemented during collaboration
References/resources Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA, and HICPAC. Guideline for Prevention of Catheter-associated Urinary Tract Infections 2009.http://www.cdc.gov/hicpac/cauti/001 cauti.html IHI Program to Prevent CAUTI http://www.ihi.org/ APIC CAUTI Elimination Guide http://www.apic.org/ IDSA Guidelines (Clin Infect Dis 2010;50:625-63) SHEA/IDSA Compendium (ICHE 2008;29:S41-S50) National Quality Forum (NQF) Safe Practices for Better Healthcare – Update April 2010 CDC/Medscape collaboration http://www.cdc.gov/hicpac/