Rapid Sequence Intubation Putting It All Together For the Assistant
90 Slides3.64 MB
Rapid Sequence Intubation Putting It All Together For the Assistant New Hampshire Division of Fire Standards & Training and Emergency Medical Services
What is “RSI” ? Ref: Manual of Emergency Airway Management “Rapid Sequence Intubation (RSI) is the administration of a potent sedative followed immediately by a rapidly acting neuromuscular blocking agent that produces rapid unconsciousness and motor paralysis to facilitate endotracheal intubation.” This procedure is only to be used by paramedics that are trained and credentialed to perform RSI by NH Bureau of EMS.
RSI Assistant Why RSI Assistants? Required as part of 2009 NHEMS Patient Care Protocol 5.4 RSI RSI Assistant retraining required every two years 2009 NHEMS Rapid Sequence Intubation (RSI) Protocol 5.4 This procedure is only to be used by paramedics that are trained and credentialed to perform RSI by NH Bureau of EMS. Either 2 RSI paramedics or 1 RSI paramedic and 1 RSI assistant must be present.
Role of the RSI Assistant 1. 2. 3. 4. Assist an RSI certified provider during RSI emergency airway procedures. Be familiar and practiced with all basic and advanced airway equipment/adjuncts maintained on EMS unit. Be competent in basic airway management. Be familiar and practiced with rescue airways maintained on EMS unit. 5. Combitube, EasyTube, LMA, and King-LT-D Capable team member, directed by RSI Provider
RSI Indication As determined by RSI Provider As per NH EMS protocol RSI 5.4 Immediate, severe airway compromise in the context of trauma, drug overdose, status epilepticus, etc., where respiratory arrest is imminent. Basically, RSI is considered for patients requiring advanced airway management who would not tolerate awake intubations.
Potential RSI Candidates Patients requiring oxygenation/ventilation management and or positive pressure ventilation: Such as, Traumatic brain injury with ALOC Severe thoracic trauma (flail chest, pulmonary contusions with hypoxemia) Clinical condition expected to deteriorate Unconscious or ALOC with potential for or actual airway compromise or vomiting And patient has A clenched jaw An active gag reflex
Contraindications As determined by RSI Provider As per NHEMS Protocol 5.4 Extensive recent burns or crush injuries greater than 24 hours old. History of Malignant Hyperthermia Too risky, based on a Risk/Benefit Analysis performed by RSI provider.
Complications There are many for the RSI provider to consider Increased intracranial pressure Increased intraocular pressure Increased intragastric pressure Aspiration due to decreased gag reflex Malignant hyperthermia Dysrhythmias Hypoxemia Airway trauma Failure to intubate / failure to ventilate DEATH
Preparation is the KEY for an organized, smooth intubation Remember the 7 P’s!!
RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation Preoxygenation Premedication Paralyze Pass the tube Proof of placement Post intubation care
IF Endotracheal Intubation fails, there must be a back-up plan.
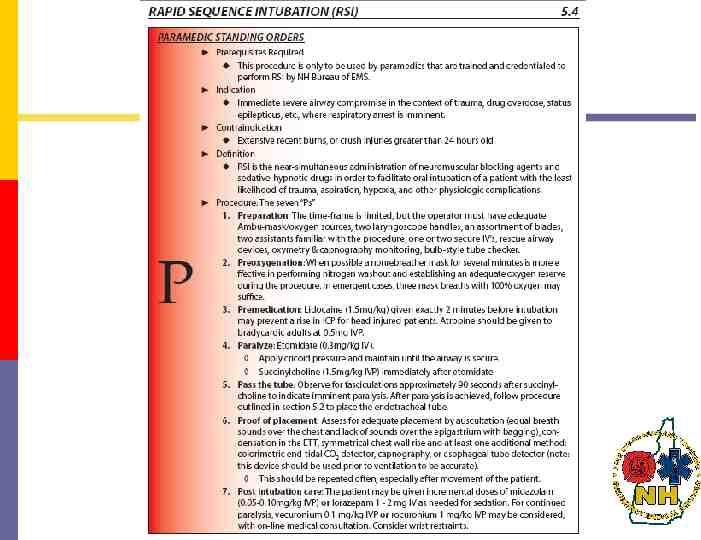
1. Preparation – Assess the risks 1. Preparation A two-part process: Assess the risks Prepare the equipment, RSI assistants Must be familiar with the RSI procedure and all necessary airway equipment
1. Preparation – Assess the risks 1. Preparation RSI Assistants should as directed prepare the following equipment: Basic adjuncts Suction Adult BVM with O2 Source ETT equipment as requested by RSI Provider Alternative airways accessible and ready Combitube, EasyTube, LMA, King, and Commercial Trach Device ETT placement confirmation devices Capnography
How does the RSI Provider know if the patient is going to be difficult to intubate and does it really matter?

Some Predictors of a Difficult Airway 1. Preparation – Assess the risks C-spine immobilized trauma patient Protruding tongue Short, thick neck Prominent upper incisors (“buckteeth”) Receding mandible High, arched palate Beard or facial hair Dentures Limited jaw opening Limited cervical mobility Upper airway conditions Face, neck, or oral trauma Laryngeal trauma Airway edema or obstruction Morbidly obese
1. Preparation – Assess the risks Objectives RSI Providers use the following mnemonics to help predict a difficult airway: MOANS LEMONS DOA
1. Preparation – Assess the risks Difficult to Bag (MOANS) Performed by RSI Provider Mask Seal Obesity or Obstruction Age 55 No Teeth Stiff
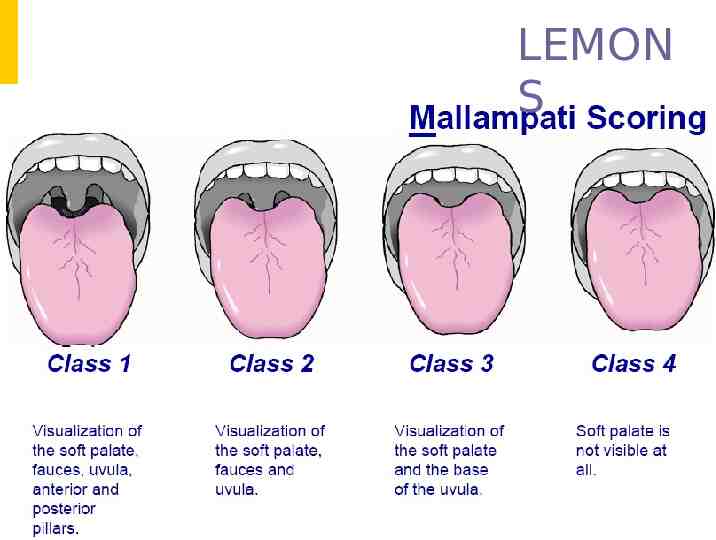
1. Preparation Difficult Laryngoscopy & – Assess the risks Intubation Performed by RSI Provider LEMONS Look Externally Evaluate 3-3-2 Mallampati Score Obstruction Neck Mobility Scene and Situation Not these lemons
LEMON S
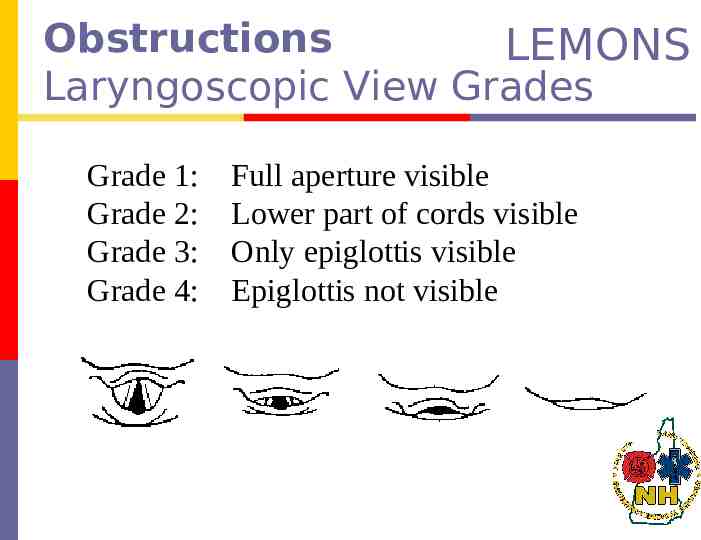
Obstructions LEMONS Laryngoscopic View Grades Grade Grade1:1: Grade Grade2:2: Grade Grade3:3: Grade Grade4:4: Full Fullaperture aperturevisible visible Lower Lowerpart partofofcords cordsvisible visible Only Onlyepiglottis epiglottisvisible visible Epiglottis Epiglottisnot notvisible visible
1. Preparation – Assess the risks Difficult Cricothyrotomy Performed by RSI Provider DOA Disruption or Distortion Obstruction Access Problems If you can’t bag and can’t cric, they’re DOA
Scene and Situation Scene safety, every crew members responsibility Environment Do you have a reasonable chance to get the tube? Space, positioning, access Egress Will you be able to ventilate during egress? A respiratory rate of 4 is better than a rate of 0!
RSI Assistant If endotracheal intubation proves difficult or fails for the RSI Provider. BE PERPARED Have Basic Adjuncts and BVM ready Consider two NPA’s and an OPA, Cricoid pressure w/ gentle ventilation) Have Combitube, EasyTube, King LT-D or LMA setup and ready
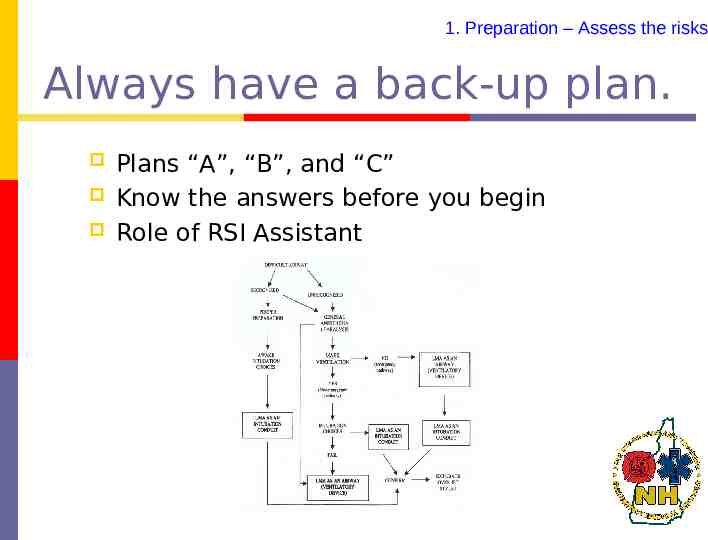
1. Preparation – Assess the risks Always have a back-up plan. Plans “A”, “B”, and “C” Know the answers before you begin Role of RSI Assistant
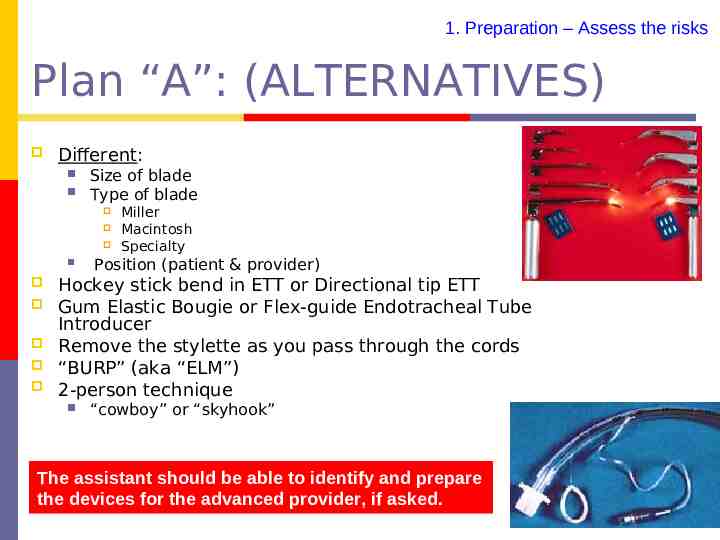
1. Preparation – Assess the risks Plan “A”: (ALTERNATIVES) Different: Size of blade Type of blade Miller Macintosh Specialty Position (patient & provider) Hockey stick bend in ETT or Directional tip ETT Gum Elastic Bougie or Flex-guide Endotracheal Tube Introducer Remove the stylette as you pass through the cords “BURP” (aka “ELM”) 2-person technique “cowboy” or “skyhook” The assistant should be able to identify and prepare the devices for the advanced provider, if asked.
“BURP” – a.k.a. 1. Preparation – Assess the risks “External Laryngeal Manipulation” Differs from the Sellick Maneuver
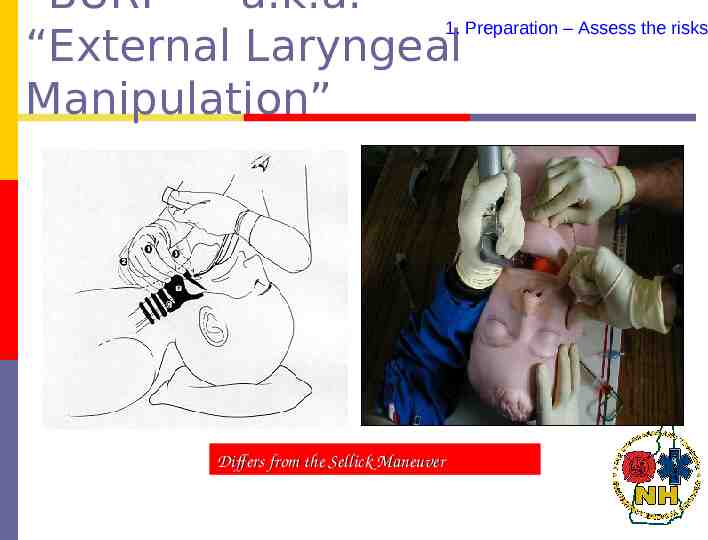
BURP Maneuver While the RSI assistant is applying the Sellick maneuver, the RSI Provider may ask for: Backward, Upward, Rightward Pressure: manipulation of the trachea Manipulate the trachea by pushing directly posterior and up to the patients right. The RSI Provider will be sweeping the oral anatomy to the patients left with a laryngoscope. This simple procedure will increase the RSI Provider chance of successfully placing the tube.
1. Preparation – Assess the risks Plan “B”: (BVM and BLIND INTUBATION & BACKUP AIRWAY Techniques )

What do we do when faced with a 1. Preparation – Assess the risks “Can’t Intubate Can’t Ventilate” situation? Plan “C”: (CRIC) Commercial, Needle, or Surgical Last resort The assistant should be able to identify and help prepare the cricothyrotomy devices for the advanced provider, if asked.
Always expect the unexpected! 1. Preparation – Assess the risks

RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation - CONTINUED Preoxygenate Premedication Paralyze Pass the tube Proof of placement Post intubation care
1. Preparation A two-part process: Assess the risks Prepare the equipment
1. Preparation – Prepare the Equipment Prepare the Equipment Equipment is present, opened and ready for use Adequate Ambu-mask/oxygen sources/suction 2 laryngoscope handles Assortment of blades Assortment of ET tubes, stylette, syringe RSI Assistant
Prepare the Equipment continued 1. Preparation – Prepare the Equipment 1-2 secure IV lines All pharmaceutical agents needed for the procedure Back-up plan and rescue airway devices Oximetry and capnography monitoring Bulb-style tube checker If appropriate, explain procedure to patient
1. Preparation – Prepare the Equipment Monitor the Patient Cardiac monitor Monitor for dysrhythmia's Blood Pressure monitoring (manual or NIBP) Monitor for hypo- or hypertension Pulse oximeter bradycardia, tachycardia, ectopy Monitor for hypoxia Waveform Capnography Monitor for hypo- or hypercarbia
RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation - CONTINUED Preoxygenate Premedication Paralyze Pass the tube Proof of placement Post intubation care
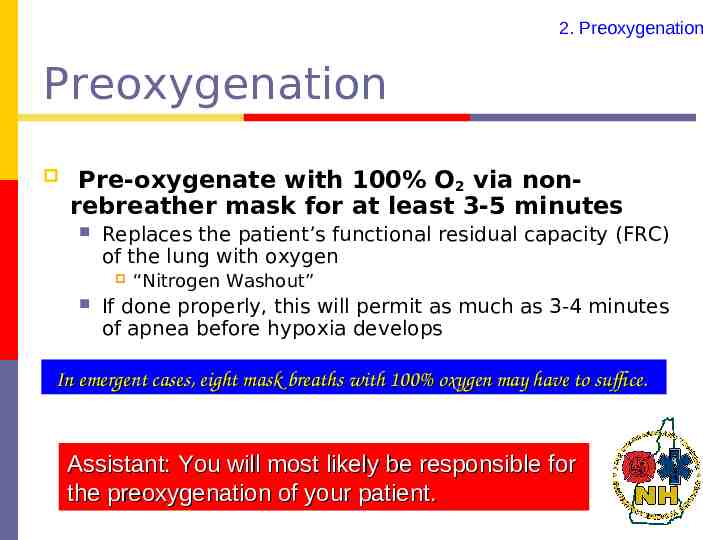
2. Preoxygenation Preoxygenation Pre-oxygenate with 100% O2 via nonrebreather mask for at least 3-5 minutes Replaces the patient’s functional residual capacity (FRC) of the lung with oxygen “Nitrogen Washout” If done properly, this will permit as much as 3-4 minutes of apnea before hypoxia develops In emergent cases, eight mask breaths with 100% oxygen may have to suffice. Assistant: You will most likely be responsible for the preoxygenation of your patient.
2. Preoxygenation Preoxygenation Resist the use of positive pressure ventilation (PPV). Use only if the patient is not ventilating adequately. PPV leads to gastric distention regurgitation aspiration If PPV is necessary, utilize cricoid pressure Place NG/OG if prolonged use of BVM Little known fact: Aspirating a few CC’s gastric contents increases the patients risk of death. Did we say cricoid pressure?
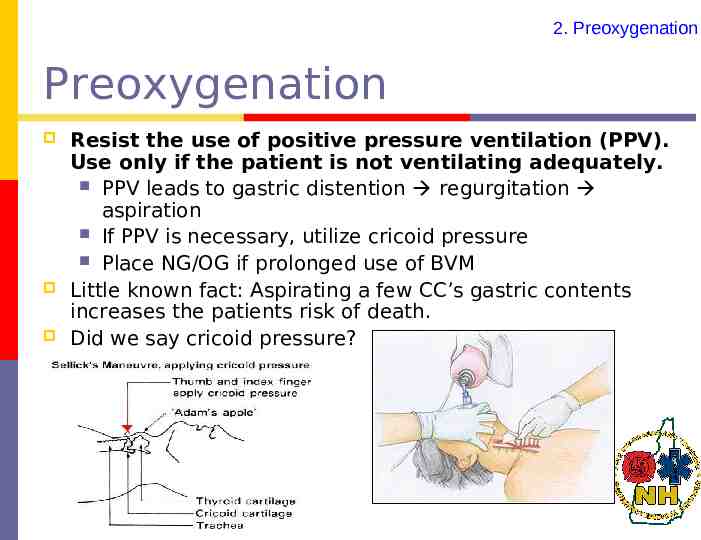
4. Paralyze Cricoid Pressure Also known as “Sellick’s Maneuver” Should be automatic Begin just as Etomidate is administered Maintained until ETT placement is confirmed and tube is secure (cuff inflated) Used to occlude the esophagus and prevent passive regurgitation common with Succs If patient starts to actively vomit – RELEASE! and suction oropharynx. Otherwise, can lead to esophageal rupture Assistant: This an important role for you!
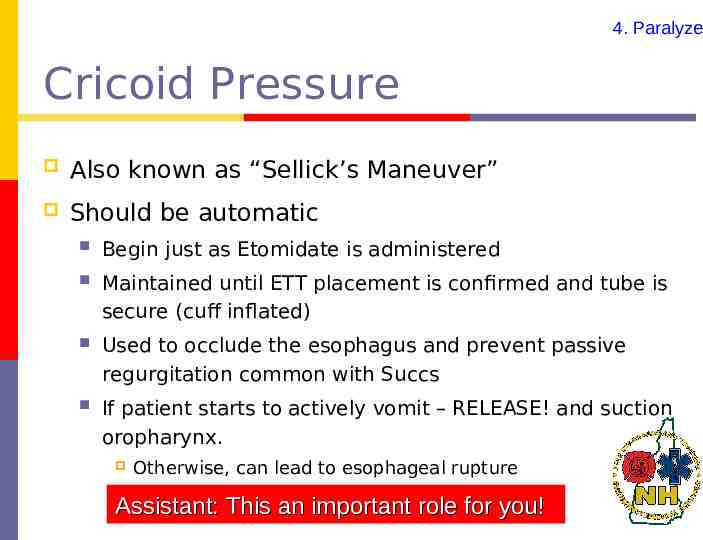
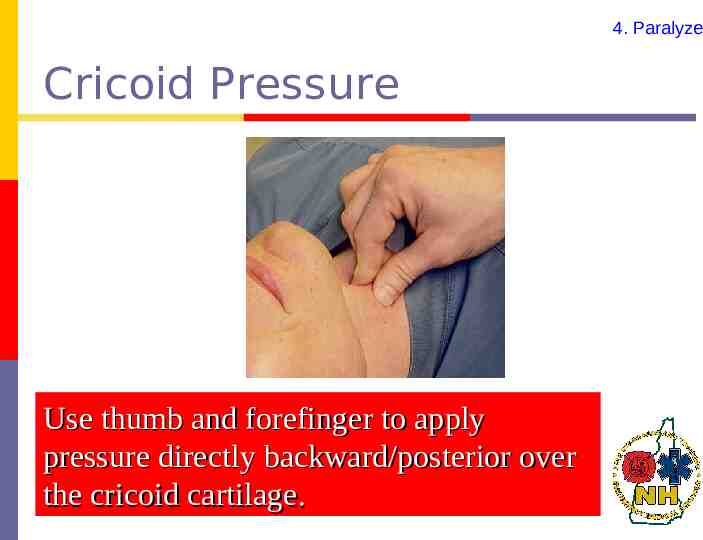
4. Paralyze Cricoid Pressure Use thumb and forefinger to apply pressure directly backward/posterior over the cricoid cartilage.
RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation - CONTINUED Preoxygenation Premedication Paralyze Pass the tube Proof of placement Post intubation care
Rapid Sequence Intubation Medications
Note about Medications Medications are ONLY to be drawn, prepared, and administered by the Paramedic RSI Provider. The Basic or Intermediate Assistance cannot prepare RSI Medications, as they are not licensed or credentialed for their use.
3. Premedication Lidocaine Why: May prevent a rise in intracranial pressure in traumatic brain injured patients. When: At least minutes prior to intubation Assistant: Will not see any major change in patient.
3. Premedication Atropine Why: Given to prevent worsening bradycardia From Succs, vagal stimulation during direct visualization, and hypoxia When: Prior to intubation for bradycardic adults Assistant: Will not see any major change in patient.
4. Paralyze Etomidate Hypnotic induction agent No analgesic properties Should always be given prior to paralytic Assistant: Will see the patient become less responsive.
4. Paralyze Succinylcholine Why: Relaxes the patient’s muscles enabling the paramedic to intubate the patient. When: Immediately after Etomidate. Will cause “fasciculations” Assistant: You will likely see the patient go through a brief period of fasciculation followed by complete flaccidity, as the patient becomes paralyzed.
4. Paralyze Fasciculations Muscular twitching involving the simultaneous contraction of contiguous groups of muscle fibers Merriam-Webster Dictionary
RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation - CONTINUED Preoxygenation Premedication Paralyze Pass the tube Proof of placement Post intubation care
4. Paralyze Paralyze A three step process: Induction medications administered by RSI provider Cricoid Pressure, provided by RSI Assistant Constant vigilance for necessary intervention (i.e suctioning, hypoxia) Paralytic medications administered by RSI provider

RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation - CONTINUED Preoxygenation Premedication Paralyze Pass the tube Proof of placement Post intubation care
5. Pass the Tube Pass the Tube Intubation is performed when there is full relaxation of the airway muscles About 90 seconds after Succinylcholine If intubation fails, maintain cricoid pressure and ventilate with BVM After patient is reoxygenated, reattempt or move to a different airway adjunct Assistant: You are still performing the cricoid pressure at this point.
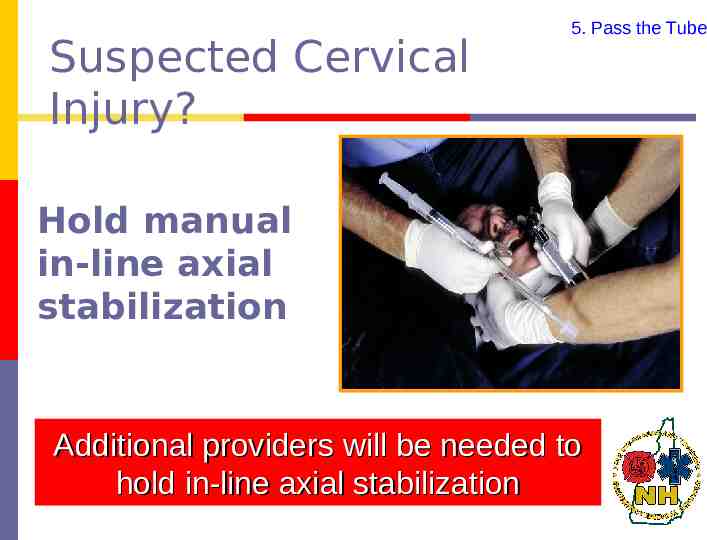
Suspected Cervical Injury? 5. Pass the Tube Hold manual in-line axial stabilization Additional providers will be needed to hold in-line axial stabilization
5. Pass the Tube Pass the Tube COMPLICATIONS: If the paramedic misses or is unable to intubate after 30 seconds be prepared to Ventilate with BVM / high flow O2 with cricoid pressure maintained They may make ONE more attempt to intubate If still unsuccessful – continue BVM / Cricoid pressure Secure Airway with backup device (CombiTube, LMA or King-LT-D) Assistant: The advanced provider may ask you to perform the BURP maneuver to better visualize the cords.
5. Pass the Tube If ETT Unsuccessful If unable to intubate, unable to secure the airway with backup device, and unable to maintain an SpO2 of 90% with a BVM RSI Provider should contact Med Control The medications administered by the RSI Provider to facilitate intubation will wear off in several minutes.
RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation - CONTINUED Preoxygenation Premedication Paralyze Pass the tube Proof of placement Post intubation care
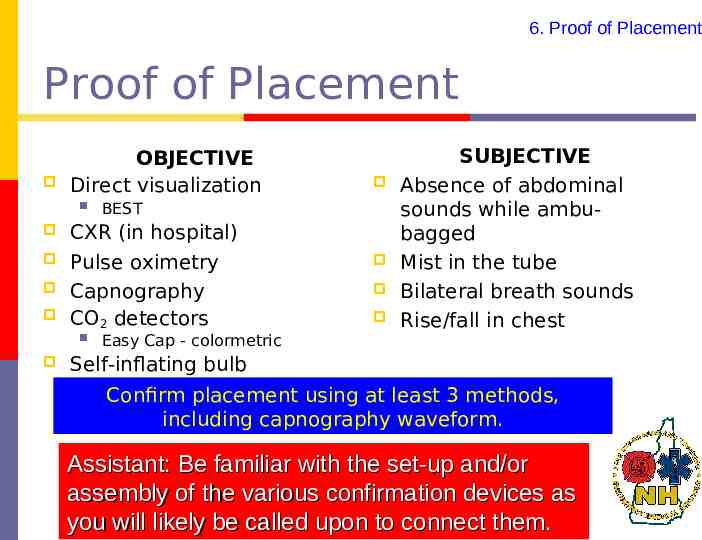
6. Proof of Placement Proof of Placement OBJECTIVE Direct visualization BEST CXR (in hospital) Pulse oximetry Capnography CO2 detectors Easy Cap - colormetric SUBJECTIVE Absence of abdominal sounds while ambubagged Mist in the tube Bilateral breath sounds Rise/fall in chest Self-inflating bulb Confirm placement using at least 3 methods, including capnography waveform. Assistant: Be familiar with the set-up and/or assembly of the various confirmation devices as you will likely be called upon to connect them.
6. Proof of Placement SpO2 (Pulse Oximetry) Provides quick estimate of PaO2 Often referred to as an additional vital sign Non-invasive
6. Proof of Placement Waveform Capnometry Number of important applications Monitor & Confirm ETT placement Useful to document adequacy of ventilation during mechanical ventilation Limitations: For patients with impaired pulmonary function or hemodynamic instability Assistant: Become familiar with the appropriate waveform for a properly ventilated patient.
6. Proof of Placement Waveform Capnometry Prerequisite Requirement Becoming a standard of care Easy to Use Good measure of Pulmonary Perfusion Relates well to PaCO2 Does have limitations

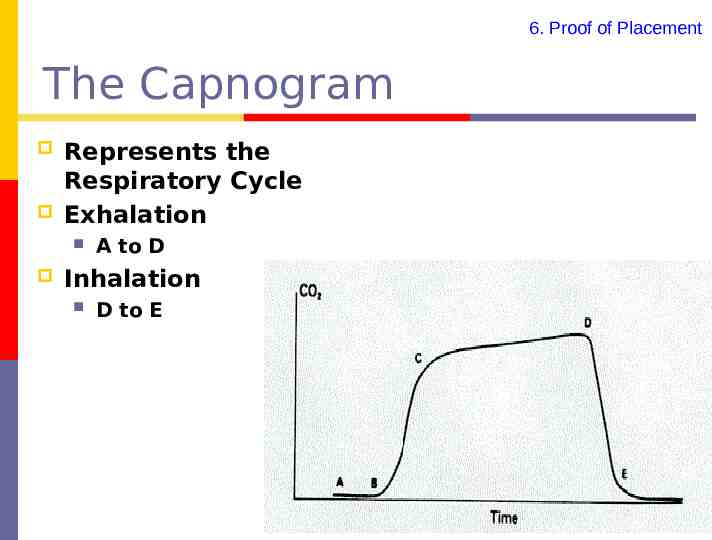
6. Proof of Placement The Capnogram Represents the Respiratory Cycle Exhalation A to D Inhalation D to E
6. Proof of Placement After confirming placement: RSI assistant should secure airway device with commercial device Immobilize the head with a cervical collar RSI provider must verify correct placement each time the patient is moved Continue to monitor Waveform capnography SpO2 Vital Signs Patients LOC Assistant: Be familiar with these steps and be able to perform.
RSI Procedure: The Seven P’s 1. 2. 3. 4. 5. 6. 7. Preparation - CONTINUED Preoxygenation Premedication Paralyze Pass the tube Proof of placement Post intubation care
7. Post Intubation Care Sedation Assessment Sign/symptoms Movement Increase in heart rate Increase in blood pressure Decrease in SpO2 Changes in muscle tone Facial muscle tension Assistant: Pay close attention to the patient’s level of consciousness. Should the patient at anytime show any of these signs/symptoms of discomfort inform the advanced provider immediately!
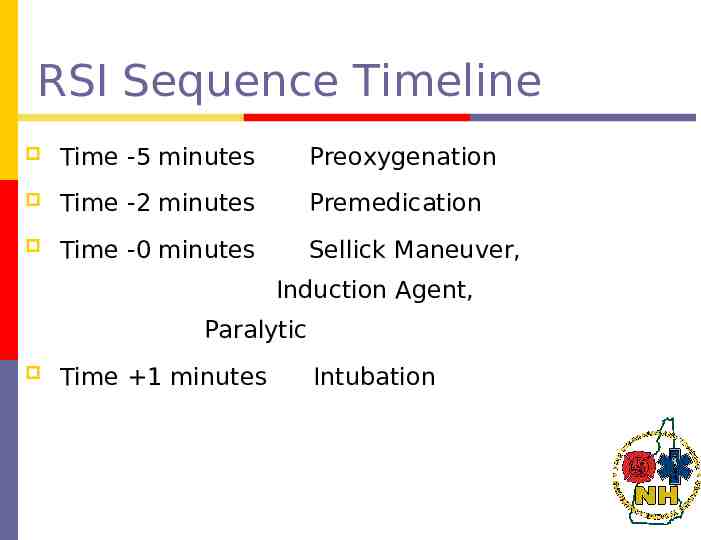
RSI Sequence Timeline Time -5 minutes Preoxygenation Time -2 minutes Premedication Time -0 minutes Sellick Maneuver, Induction Agent, Paralytic Time 1 minutes Intubation
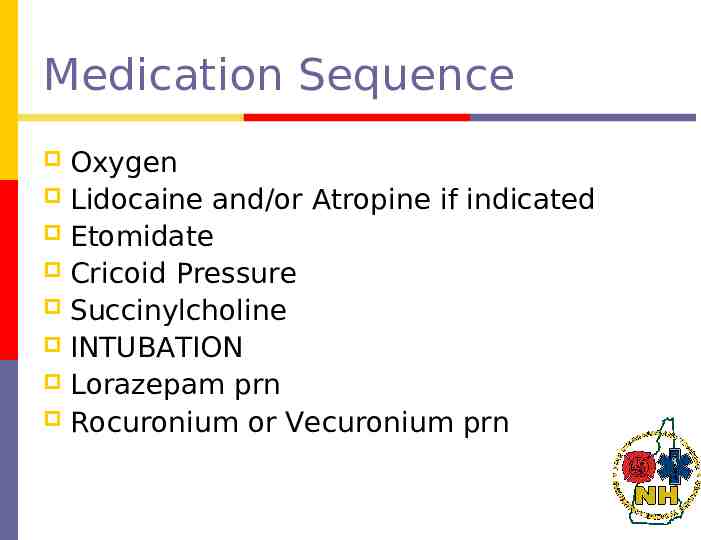
Medication Sequence Oxygen Lidocaine and/or Atropine if indicated Etomidate Cricoid Pressure Succinylcholine INTUBATION Lorazepam prn Rocuronium or Vecuronium prn
& Don’t hesitate to use them!
Rescue Airway Management Have a back-up plan Algorithmic approach BVM Gum Elastic Bougie Laryngeal Mask Airway (LMA) Esophageal Tracheal Combitube King-LT-D Become familiar with the rescue airway carried on your EMS unit. Assistant: Be familiar with the set-up and/or assembly of the various backup devices as you will likely be called upon to assist with them.
BVM Can you obtain a good mask seal? Adequate chest rise & fall? Adequate oxygenation & ventilation? Assistant: You will most likely be performing this skill.
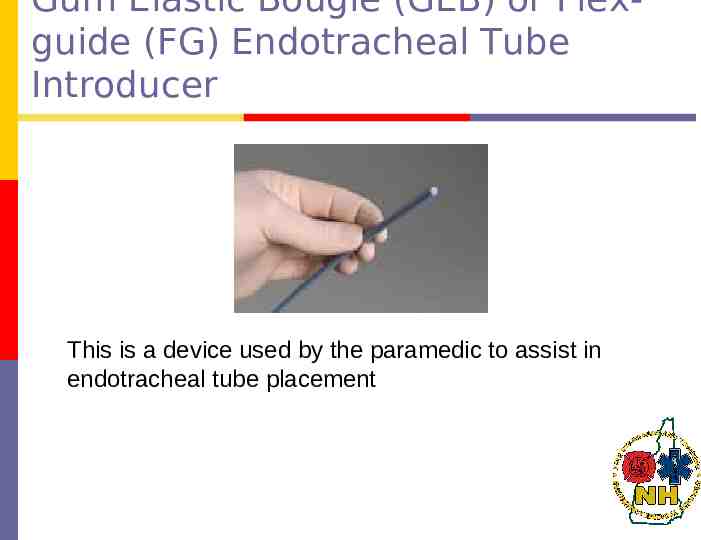
Gum Elastic Bougie (GEB) or Flexguide (FG) Endotracheal Tube Introducer This is a device used by the paramedic to assist in endotracheal tube placement
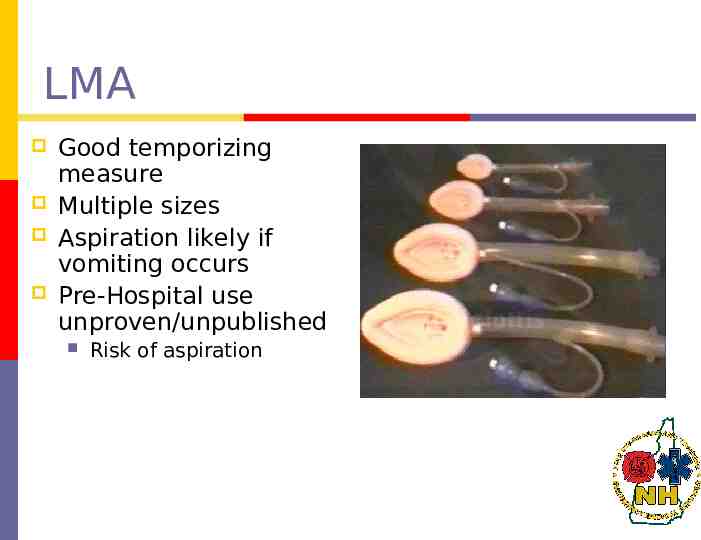
LMA Good temporizing measure Multiple sizes Aspiration likely if vomiting occurs Pre-Hospital use unproven/unpublished Risk of aspiration
Combitube Especially suited for Patients with difficult anatomy Reduced access spaces Reduced illumination (bright light)
King-LT-D

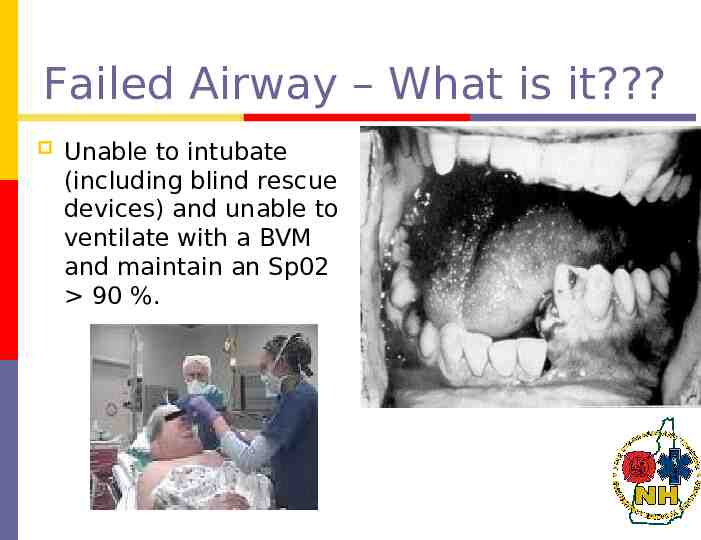
Failed Airway – What is it? Unable to intubate (including blind rescue devices) and unable to ventilate with a BVM and maintain an Sp02 90 %.

Cricothyrotomy RSI Providers last resort for airway control Low frequency/high risk skill Can be complex and confound decisions
Final Thoughts on the “Failed Airway” In all cases of a failed airway, the operator must continually assess the adequacy of oxygenation and ventilation 7% of all trauma patients will require intubation
Golden Rule-Do No Harm “Always weigh the risks and benefits of intubation in the prehospital setting against transport to the ED. In many circumstances, rapid transport might be the best way of managing the airway.” Manual of Emergency Airway Management
Do No Harm “Master bag-and-mask ventilation. There are very few airway emergencies in the prehospital setting that will not be temporized or managed adequately with proper bag-and-mask ventilation until the patient can be transported to the hospital.” Manual of Emergency Airway Management
Documentation Required Responsibility of the RSI Provider EMS Agency and Resource Hospital Medical Director are required to CQI/QA 100% of prehospital RSIs
Case Studies
Case 1 67 y/o female “code blue” – in asystole. RSI or not? PLAN?
Case 2 72 y/o female with Hx fever, productive cough and progressive dyspnea. Lethargic, perioral cyanosis. RR 34 and labored, HR 114, BP 117/76. Lung sounds equal with scattered rhonchi. RSI or not? PLAN?

Case 3 41 y/o female with c/o “asthma attacks” x20 minutes. Severe respiratory distress. RR 32, HR 127, BP 160/92. Bilateral I/E wheezes. Within 10 minutes, she becomes lethargic and her RR slows. RSI or not? PLAN?
Case 4 46 y/o male with a Hx of EtOH and drug abuse. Presents with “had a seizure” per bystanders. Pt is responsive to pain, but does not follow commands or answer questions. RR 18, HR 109, BP 120/80. Within minutes, he has 2 episodes of vomiting and “gurgling respirations”. PLAN?
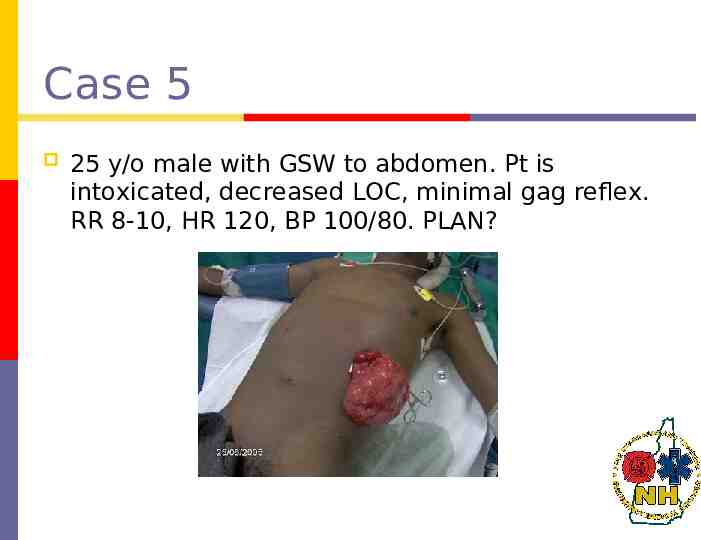
Case 5 25 y/o male with GSW to abdomen. Pt is intoxicated, decreased LOC, minimal gag reflex. RR 8-10, HR 120, BP 100/80. PLAN?
Case 6 87 y/o male MVC, high-speed, unrestrained. Patient gasping for air, able to talk, c/o right side CP. RR 32, HR 120, BP 186/92. Multiple deformities to face and chin. Ecchymosis and swelling to neck and anterior chest. Large flail segment to ant/lat chest. Decreased BS on the right. No stridor, but some gurgling in throat. PLAN?
References Marx: Rosen's Emergency Medicine: Concepts and Clinical Practice, 5th ed., Copyright 2002 Mosby, Inc. Miller: Miller's Anesthesia, 6th ed., Copyright 2005 Elsevier Roberts: Clinical Procedures in Emergency Medicine, 4th ed., Copyright 2004 Elsevier