Name that Rash— Common Pediatric Skin Problems PATT Y P E S KA , A P R
72 Slides2.85 MB
Name that Rash— Common Pediatric Skin Problems PATT Y P E S KA , A P R N - C P N P- P C M I S S I S C H E M B A R I , A P R N - C P N P- P C
Objectives Participants will be able to identify distinguishing features of common childhood rashes Participants will be able to discuss the management & treatment of common childhood rashes Participants will be able to triage concerns for a rash Participants will be able to identify if a child can remain in the classroom or will need to be sent home

Rashes There are more than 12 million office visits annually for rashes and other skin concerns in children and adolescents 68% of those 12 million visits are made to a child’s PCP Important considerations to aid in diagnosis and treatment of rashes: Appearance of rash Location of rash Clinical course Associated symptoms (i.e. pruritus, fevers, diarrhea, sore throat)
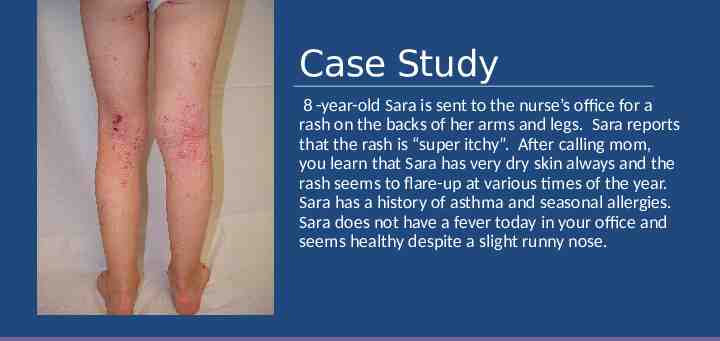
Case Study 8 -year-old Sara is sent to the nurse’s office for a rash on the backs of her arms and legs. Sara reports that the rash is “super itchy”. After calling mom, you learn that Sara has very dry skin always and the rash seems to flare-up at various times of the year. Sara has a history of asthma and seasonal allergies. Sara does not have a fever today in your office and seems healthy despite a slight runny nose.

What is this rash? A) Eczema B) Viral Exanthem C) Bed Bugs D) Henoch-Schonlein Purpura (HSP)
GOALS of treatment are to reduce symptoms, prevent exacerbations, & prevent secondary skin infections. Management Plan: Atopic Dermatitis (Eczema) 1) Identify triggers: Avoid harsh soaps and detergents, contact with wool/synthetic clothing, perfumes, trigger foods, very dry hot air, or becoming too hot and sweaty 2) Humidify the home, keep nails short. 3) Maintain adequate hydration: Bathe in lukewarm water using mild soap. Avoid excessive bathing 4) Soak and Seal: Moisturize with an emollient such as Aquaphor or Eucerin within minutes of bath. Ointments are better than creams. 5) Topical steroid cream: Are used in conjunction with emollients and are often the mainstay of therapy. Avoid application of steroids to face and genitalia. Use the lowest potency during exacerbations and for a limited time (usually no more than 7 days)
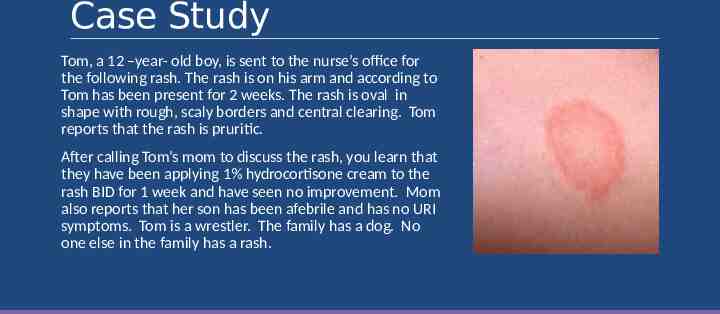
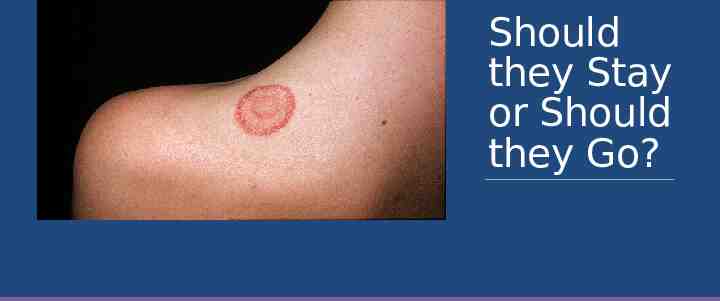
Case Study Tom, a 12 –year- old boy, is sent to the nurse’s office for the following rash. The rash is on his arm and according to Tom has been present for 2 weeks. The rash is oval in shape with rough, scaly borders and central clearing. Tom reports that the rash is pruritic. After calling Tom’s mom to discuss the rash, you learn that they have been applying 1% hydrocortisone cream to the rash BID for 1 week and have seen no improvement. Mom also reports that her son has been afebrile and has no URI symptoms. Tom is a wrestler. The family has a dog. No one else in the family has a rash.
What is this rash? A) Nummular Eczema B) Pityriasis Rosea C) Tinea Corporis D) Urticaria

Tinea Corporis (Ringworm) Lesions are erythematous, ring-shaped and are sharply marginated with a scaly border. Develops when dermatophytic fungi invade the outer skin layers at the affected body region. Tinea Capitis: ringworm of scalp Tinea Corporis: ringworm of body Tinea Cruris: jock itch Tinea Pedis: ringworm of the feet Acquired by direct skin contact with an infected individual or animal, contact with fomites, or from secondary spread from other sites of dermatophyte infection.
Question What would you recommend mom do to treat Tinea Corporis? A) Reassure Tom & his mom that it is a self-limiting rash and will go away on its own. B) Recommend OTC antifungal cream be applied BID for 1-3 weeks C) Recommend mom schedule an appointment for Tom to see his PCP because he will need to be placed on a short course of oral griseofulvin. D) Tell parents that Tom cannot return to school or wrestling until the lesion is completely resolved.
Answer: B-OTC antifungal Tinea Corporis – Managemen t OTC antifungal-clotrimazole (lotrimin) or miconazole are usually effective. Apply cream to the lesion and surrounding area of normal skin BID until resolved, which may take 1 to 3 weeks. Systemic medication-Griseofulvin for patients with extensive infection or patients who fail topical therapy. Tinea capitis (ringworm of the scalp) MUST be treated with oral medications because the fungal infection is found at the root of the hair follicles, where topical agents do not reach. Identify and treat contacts, educate about communicability, exclude from daycare or school for 24 hours after start of treatment. Athletes with tinea corporis can participate in matches 72 hours after commencement of topical therapy and when the infected area can be covered.
Tinea CorporisPrevention Do not share clothing, sports equipment, or towels with other people. Always wear slippers or sandals when at the gym, local pool, or other public areas. Wash thoroughly with soap & shampoo after any sport involving skinto-skin contact. Wash all workout clothing after each practice in hot water and drying on high heat setting Avoid tight fitting clothing. Change socks and underwear daily. Keep skin dry and clean. Dry thoroughly after bathing. Put your socks on before your underwear if you have athlete’s foot to prevent the spread of infection to other parts of your body. Have your pet seen by their vet if they have patches of missing hair or a rash. If someone in your family has symptoms of ringworm, have them treated right away to decrease chances of spreading infection to other family members
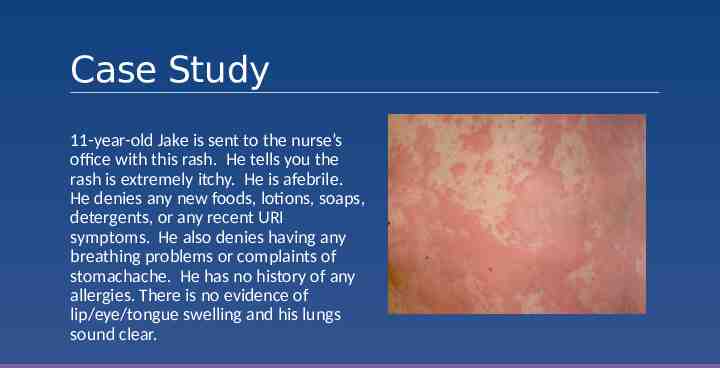
Case Study 11-year-old Jake is sent to the nurse’s office with this rash. He tells you the rash is extremely itchy. He is afebrile. He denies any new foods, lotions, soaps, detergents, or any recent URI symptoms. He also denies having any breathing problems or complaints of stomachache. He has no history of any allergies. There is no evidence of lip/eye/tongue swelling and his lungs sound clear.
What is this rash? A) Contact Dermatitis B) Urticaria or Hives C) Henoch-Schonlein Purpura (HSP) D) Insect Bites
Urticaria (Hives) Circumscribed, raised erythematous plaques, often with central pallor Usually round, oval or serpiginous in shape, ranging from 1cm to several cm in diameter Intensely itchy----often worse at night Transient NOT painful & resolve without leaving ecchymotic marks Any area of the body may be affected Causes Infections—viral, bacterial, and parasitic Allergic reactions to meds, foods, insect bites/stings Ingestion of NSAIDs Often underlying cause is unknown
Treatment of Hives Initial treatment should focus on short-term relief of pruritus and angioedema, if present 2/3 of cases will be self-limited and resolve spontaneously H1 antihistamines First generation—Benadryl, hydroxyzine Second generation—Claritin, Zyrtec, Allegra **preferred over 1st generation because they are less sedating, have fewer side effects, fewer drug-drug-interactions, and require less frequent dosing

Case Study Suzie, a 5-year-old girl, is sent to the nurse’s office for this facial rash. Suzie is afebrile in the office and has no complaints. After speaking with mom, you learn that Suzie had low -grade fevers and complained of a sore throat and body aches a few days ago. No one else in the family is ill, no known exposures, no family pets, child is UTD on her immunizations.
What is this rash? A) Systemic Lupus Erythematosus B) Measles C) Roseola D) Erythema Infectiosum
Caused by human parvovirus B19 Usually affects children between 4 and 10 years of age, more common in spring Fifth Disease (Erythema Infectiosum) Transmission is via respiratory droplets. Incubation period is 4 to 14 days Low grade fevers, malaise, myalgia, headache, and sore throat often precede the rash Rash appears first on the face—often present with a “slapped cheek” appearance 1 to 4 days after the facial rash appears, the rash spreads to the trunk & extremities. The rash develops a characteristic lacy, reticular pattern as it moves down the body Sunlight, physical activity, and hot baths can often exacerbate the rash
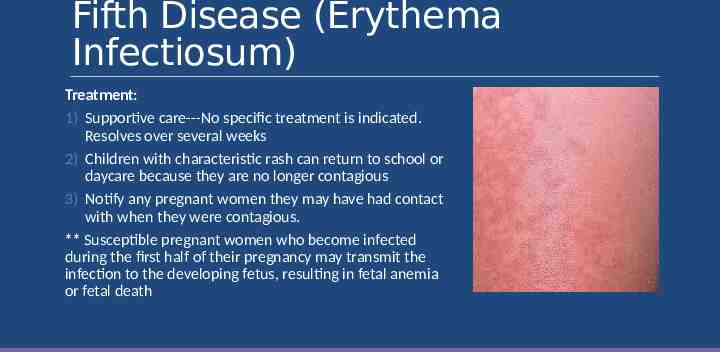
Fifth Disease (Erythema Infectiosum) Treatment: 1) Supportive care---No specific treatment is indicated. Resolves over several weeks 2) Children with characteristic rash can return to school or daycare because they are no longer contagious 3) Notify any pregnant women they may have had contact with when they were contagious. ** Susceptible pregnant women who become infected during the first half of their pregnancy may transmit the infection to the developing fetus, resulting in fetal anemia or fetal death
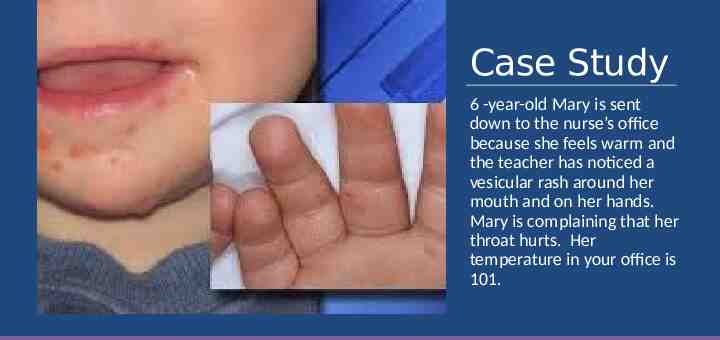
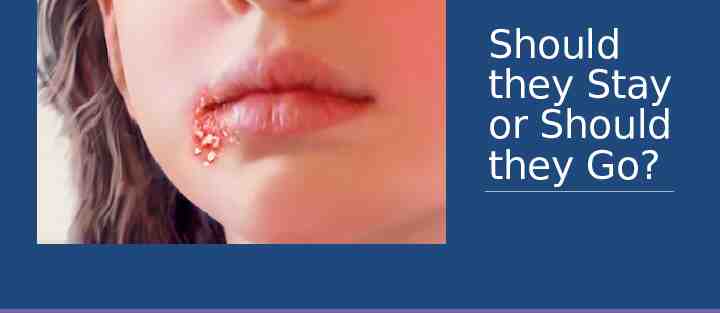
Case Study 6 -year-old Mary is sent down to the nurse’s office because she feels warm and the teacher has noticed a vesicular rash around her mouth and on her hands. Mary is complaining that her throat hurts. Her temperature in your office is 101.
What is this rash? A) Hand, Foot, & Mouth B) Herpangina C) Herpes Zoster D) Herpes Simplex

Hand, Foot, & Mouth Disease (HFM) Caused by enteroviral or coxsackie viruses Occurs most often in late summer or early fall Incubation period is 4 to 6 days Signs & Symptoms: Fevers Vesicular eruptions in oropharynx (ulcerations most commonly found on buccal mucosa, tongue, soft palate, uvula, and tonsillar pillars) Painful vesicular lesions on hands, feet, buttocks, elbows, knees and perineum
Question What teaching should you provide parents regarding HFM? A) Tell parents that HFM is an illness that only young children can catch and that they will not come down with the disease. B) Instruct parents to make an appointment for their daughter because she will need to be placed on oral antibiotics. C) Tell parents that nail shedding may occur for several months following HFM. D) Tell parents that HFM is not contagious and their child may stay at school.
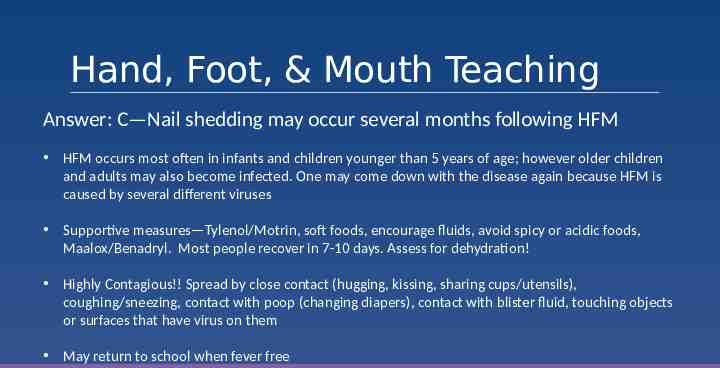
Hand, Foot, & Mouth Teaching Answer: C—Nail shedding may occur several months following HFM HFM occurs most often in infants and children younger than 5 years of age; however older children and adults may also become infected. One may come down with the disease again because HFM is caused by several different viruses Supportive measures—Tylenol/Motrin, soft foods, encourage fluids, avoid spicy or acidic foods, Maalox/Benadryl. Most people recover in 7-10 days. Assess for dehydration! Highly Contagious!! Spread by close contact (hugging, kissing, sharing cups/utensils), coughing/sneezing, contact with poop (changing diapers), contact with blister fluid, touching objects or surfaces that have virus on them May return to school when fever free
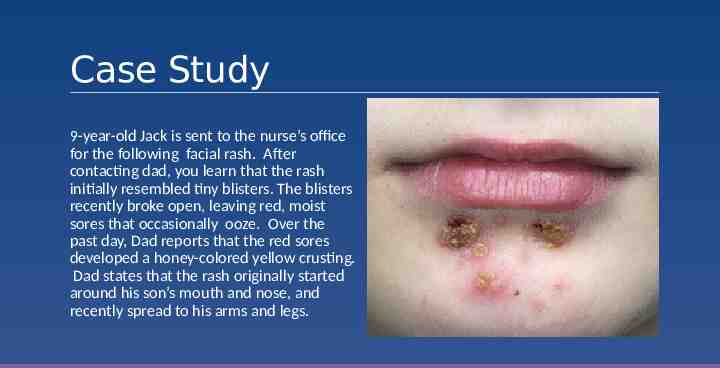
Case Study 9-year-old Jack is sent to the nurse’s office for the following facial rash. After contacting dad, you learn that the rash initially resembled tiny blisters. The blisters recently broke open, leaving red, moist sores that occasionally ooze. Over the past day, Dad reports that the red sores developed a honey-colored yellow crusting. Dad states that the rash originally started around his son’s mouth and nose, and recently spread to his arms and legs.

What is this rash? A) Scabies B) Hand, Foot, & Mouth C) Herpes Simplex D) Impetigo
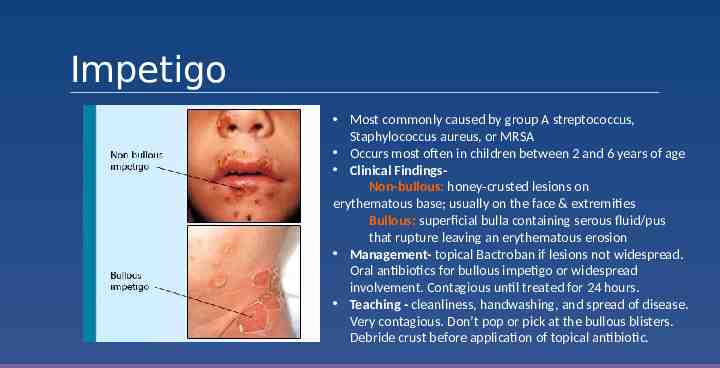
Impetigo Most commonly caused by group A streptococcus, Staphylococcus aureus, or MRSA Occurs most often in children between 2 and 6 years of age Clinical FindingsNon-bullous: honey-crusted lesions on erythematous base; usually on the face & extremities Bullous: superficial bulla containing serous fluid/pus that rupture leaving an erythematous erosion Management- topical Bactroban if lesions not widespread. Oral antibiotics for bullous impetigo or widespread involvement. Contagious until treated for 24 hours. Teaching - cleanliness, handwashing, and spread of disease. Very contagious. Don’t pop or pick at the bullous blisters. Debride crust before application of topical antibiotic.
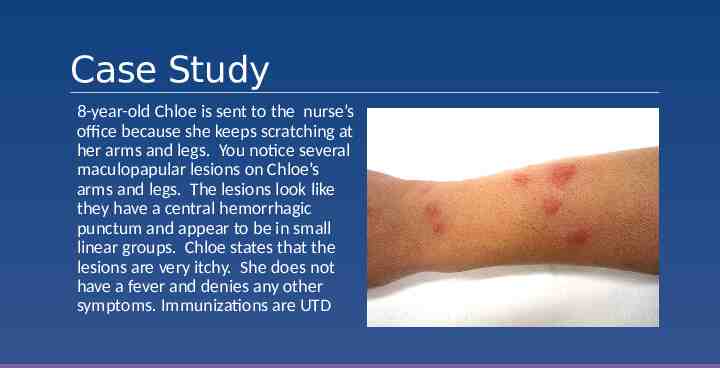
Case Study 8-year-old Chloe is sent to the nurse’s office because she keeps scratching at her arms and legs. You notice several maculopapular lesions on Chloe’s arms and legs. The lesions look like they have a central hemorrhagic punctum and appear to be in small linear groups. Chloe states that the lesions are very itchy. She does not have a fever and denies any other symptoms. Immunizations are UTD

What is this rash? A) Scabies B) Chicken Pox C) Bed Bugs D) Hives
Often in a breakfast-lunch-dinner alignment Most common clinical presentation is a 2-5 mm pruritic maculopapular lesion with a central hemorrhagic punctum located in areas typically uncovered when sleeping Bed Bugs Most common sites are arms and legs; however, can occur anywhere Caused by bite of C.lectularius Blister-capped papules and intense itching occur within 48 hours after a bite. Other symptoms include pruritis, papules, nodules, and bullous eruptions
Most reactions spontaneously resolve within 3-10 days May treat irritations due to the bite with topical steroid and oral antihistamines Encourage good handwashing and hygiene to prevent secondary infections Treatment for Bed Bugs Eradication of infestation Vacuum all rugs, floors, furniture, bed frames, and any cracks or crevices in home Place mattress and box springs in encasements designed to protect against bed bugs for 1 year Wash anything that touches the floor, clothes, bed sheets, blankets, and bedspreads in water with temperature 120 degrees Fahrenheit If items can not be laundered, place in plastic bad and put outdoors in a hot sunny location or inside a closed vehicle for at least 1 day Professional eradication is most efficient and safest option to verify and treat infestations
Prevention of Bed Bugs SLEEP Acronym Survey surfaces for signs of infestation Lift & look for all bed bug hiding spots, including underneath mattress, bed frame, headboard, and furniture. Elevate luggage on luggage rack away from the bed and wall Examine luggage carefully while repacking and when returning home Place all clothing packed in luggage in the dryer for at least 15 minutes at the highest setting immediately after returning home
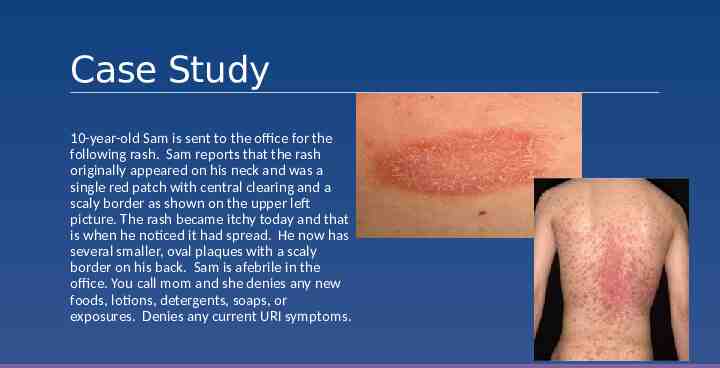
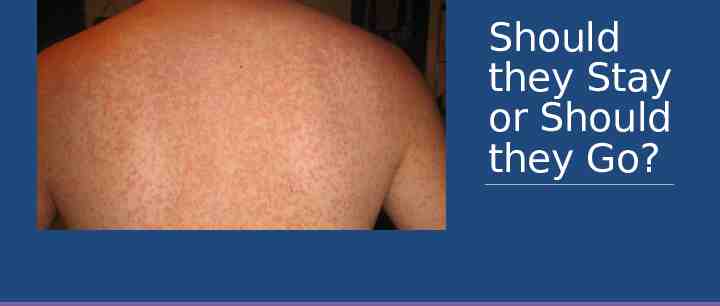
Case Study 10-year-old Sam is sent to the office for the following rash. Sam reports that the rash originally appeared on his neck and was a single red patch with central clearing and a scaly border as shown on the upper left picture. The rash became itchy today and that is when he noticed it had spread. He now has several smaller, oval plaques with a scaly border on his back. Sam is afebrile in the office. You call mom and she denies any new foods, lotions, detergents, soaps, or exposures. Denies any current URI symptoms.
What is this rash? A) Pityriasis Rosea B) Poison Ivy C) Tinea Corporis D) Tinea Versicolor
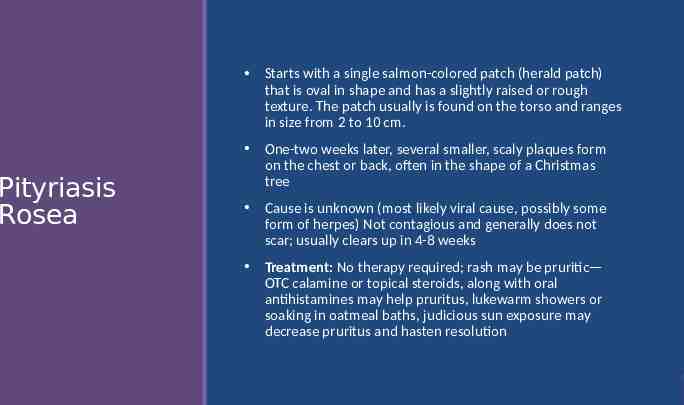
Pityriasis Rosea Starts with a single salmon-colored patch (herald patch) that is oval in shape and has a slightly raised or rough texture. The patch usually is found on the torso and ranges in size from 2 to 10 cm. One-two weeks later, several smaller, scaly plaques form on the chest or back, often in the shape of a Christmas tree Cause is unknown (most likely viral cause, possibly some form of herpes) Not contagious and generally does not scar; usually clears up in 4-8 weeks Treatment: No therapy required; rash may be pruritic— OTC calamine or topical steroids, along with oral antihistamines may help pruritus, lukewarm showers or soaking in oatmeal baths, judicious sun exposure may decrease pruritus and hasten resolution
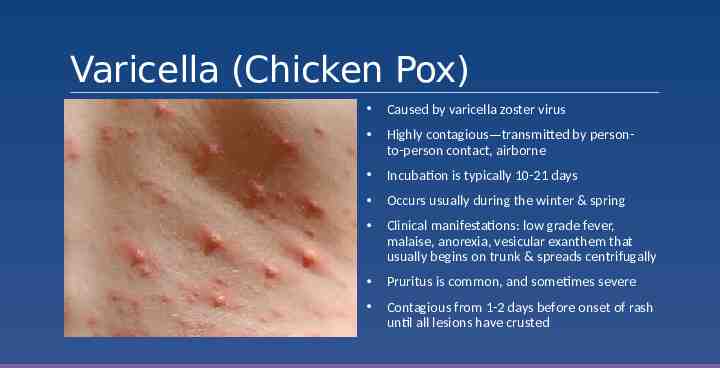
Varicella (Chicken Pox) Caused by varicella zoster virus Highly contagious—transmitted by personto-person contact, airborne Incubation is typically 10-21 days Occurs usually during the winter & spring Clinical manifestations: low grade fever, malaise, anorexia, vesicular exanthem that usually begins on trunk & spreads centrifugally Pruritus is common, and sometimes severe Contagious from 1-2 days before onset of rash until all lesions have crusted

Treatment Treatment: Supportive 1) Tylenol for fever (NO ASPIRIN) 2) Calamine lotion 3) Antihistamines 4) Keep fingernails short, frequent bathing 5) Acyclovir—must be started within 24 hours Prevention: Immunization with Varivax Children with uncomplicated varicella may return to school/daycare when the rash has crusted over, or in immunized people without crusts, when no new lesions have appeared within a 24-hour-period
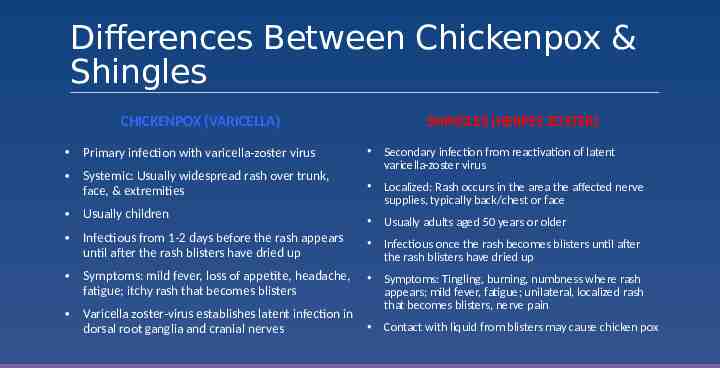
Differences Between Chickenpox & Shingles CHICKENPOX (VARICELLA) SHINGLES (HERPES ZOSTER) Primary infection with varicella-zoster virus Systemic: Usually widespread rash over trunk, face, & extremities Secondary infection from reactivation of latent varicella-zoster virus Localized: Rash occurs in the area the affected nerve supplies, typically back/chest or face Usually children Usually adults aged 50 years or older Infectious from 1-2 days before the rash appears until after the rash blisters have dried up Infectious once the rash becomes blisters until after the rash blisters have dried up Symptoms: mild fever, loss of appetite, headache, fatigue; itchy rash that becomes blisters Varicella zoster-virus establishes latent infection in dorsal root ganglia and cranial nerves Symptoms: Tingling, burning, numbness where rash appears; mild fever, fatigue; unilateral, localized rash that becomes blisters, nerve pain Contact with liquid from blisters may cause chicken pox
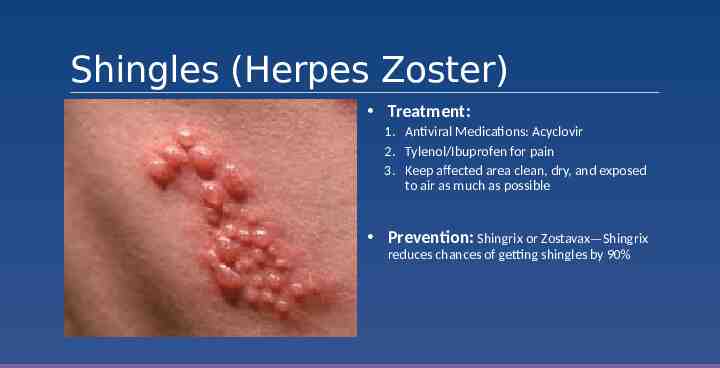
Shingles (Herpes Zoster) Treatment: 1. Antiviral Medications: Acyclovir 2. Tylenol/Ibuprofen for pain 3. Keep affected area clean, dry, and exposed to air as much as possible Prevention: Shingrix or Zostavax—Shingrix reduces chances of getting shingles by 90%
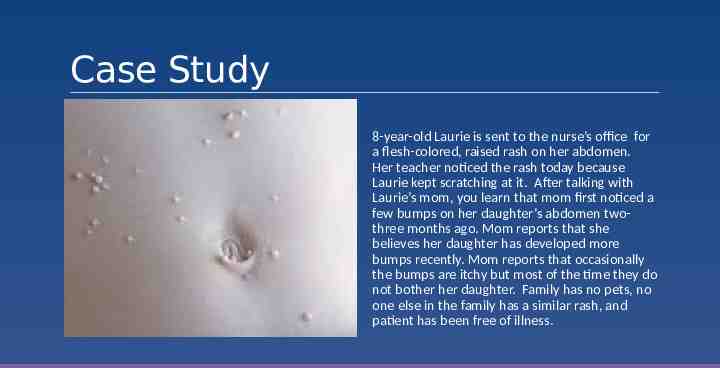
Case Study 8-year-old Laurie is sent to the nurse’s office for a flesh-colored, raised rash on her abdomen. Her teacher noticed the rash today because Laurie kept scratching at it. After talking with Laurie’s mom, you learn that mom first noticed a few bumps on her daughter’s abdomen twothree months ago. Mom reports that she believes her daughter has developed more bumps recently. Mom reports that occasionally the bumps are itchy but most of the time they do not bother her daughter. Family has no pets, no one else in the family has a similar rash, and patient has been free of illness.

What is this rash? A) Folliculitis B) Skin Tags C) Flat Warts D) Molluscum Contagiosum
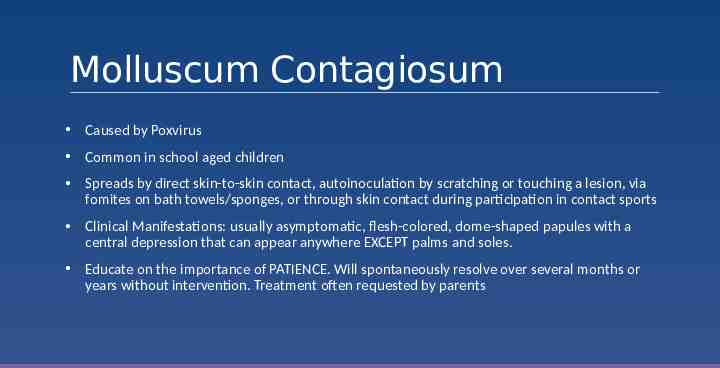
Molluscum Contagiosum Caused by Poxvirus Common in school aged children Spreads by direct skin-to-skin contact, autoinoculation by scratching or touching a lesion, via fomites on bath towels/sponges, or through skin contact during participation in contact sports Clinical Manifestations: usually asymptomatic, flesh-colored, dome-shaped papules with a central depression that can appear anywhere EXCEPT palms and soles. Educate on the importance of PATIENCE. Will spontaneously resolve over several months or years without intervention. Treatment often requested by parents
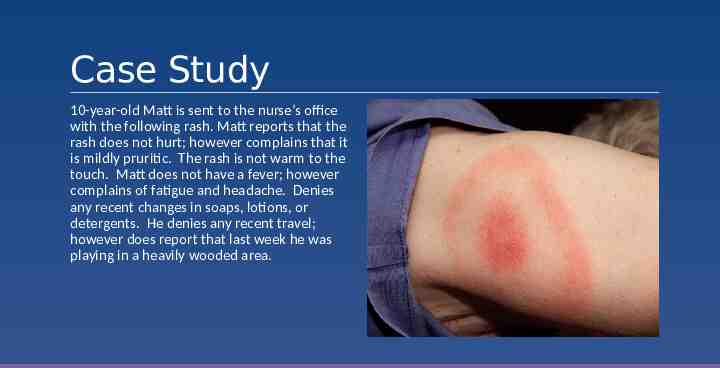
Case Study 10-year-old Matt is sent to the nurse’s office with the following rash. Matt reports that the rash does not hurt; however complains that it is mildly pruritic. The rash is not warm to the touch. Matt does not have a fever; however complains of fatigue and headache. Denies any recent changes in soaps, lotions, or detergents. He denies any recent travel; however does report that last week he was playing in a heavily wooded area.
What is this rash? A) Erythema Multiforme B) Cellulitis C) Lyme Disease D) Nummular Eczema
Transmitted by the tick Ixodes scapularis (black-legged tick or deer tick) In 2019 for the first time in Nebraska, established populations (meeting CDC criteria) of this tick were identified in Douglas, Sarpy, and Saunders counties. Lyme Disease Early localized Lyme disease is manifested by a single erythema migrans lesion at the site of attachment of the tick Erythema migrans lesions usually are flat and without scale; they may be pruritic or burning but are rarely painful. Other symptoms associated with erythema migrans include fever, fatigue, headache, neck pain, arthralgia, and myalgia.

Early Disseminated & Late Disease Early Disseminated Disease: o Occurs weeks to months after the tick bite o The clinical manifestations of early disseminated Lyme disease in children include multiple erythema migrans, cranial nerve palsy, meningitis , & carditis Late Disease o Occurs months to years after the onset of infection o May not be preceded by history of early localized or disseminated Lyme Disease o Arthritis is leading symptom in US followed by neurologic manifestations o Knee most common joint affected
Treatment of Lyme Disease Oral doxycycline, amoxicillin, and cefuroxime are treatment for Early Lyme Disease and recommended if patient has erythema migrans Treatment usually ranges from 10-21 days depending on antibiotic Discuss Prevention Checking for and removing ticks after outdoor activities Bathing after outdoor activities where ticks are abundant Placing dry clothes in dryers for a short time period after outdoor activities Wear protective covering Using tick repellent, such as DEET on skin, and permethrin on clothing
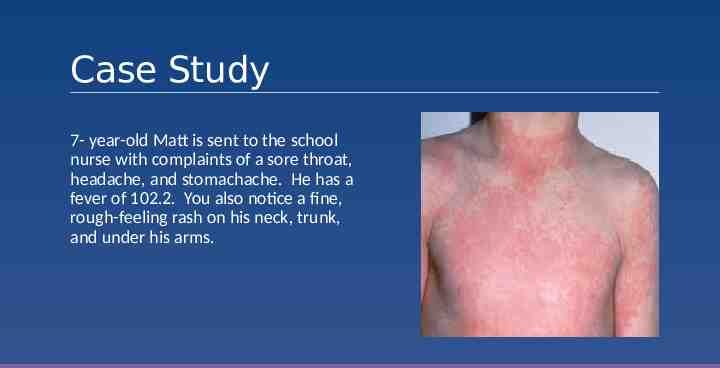
Case Study 7- year-old Matt is sent to the school nurse with complaints of a sore throat, headache, and stomachache. He has a fever of 102.2. You also notice a fine, rough-feeling rash on his neck, trunk, and under his arms.

What is this rash? A) Measles B) Scarlatina C) Viral Exanthem D) Urticaria
Rash starts out looking like a bad sunburn; typically starts on neck and face, and then spreads to chest, back, and the rest of the body Scarlet Fever (Scarlatina) Rash is red, raised, blanchable, feels rough like sandpaper. In body creases (underarms, elbows, groin), the rash forms red streaks Usually accompanied by strawberry looking tongue, sore throat, fever, chills, headache, N/V, stomachache Caused by Group A Strep; occurs most often in children ages 5 to 15 years; spread from person to person via respiratory droplets, incubation is usually 2-4 days Treatment: Antibiotics: PCN, Keflex if PCN allergic, for 10 days; Tylenol/Motrin for fevers/sore throat; offer soft foods and push fluids; may return to daycare/school when afebrile and has been on antibiotic for 24 hours
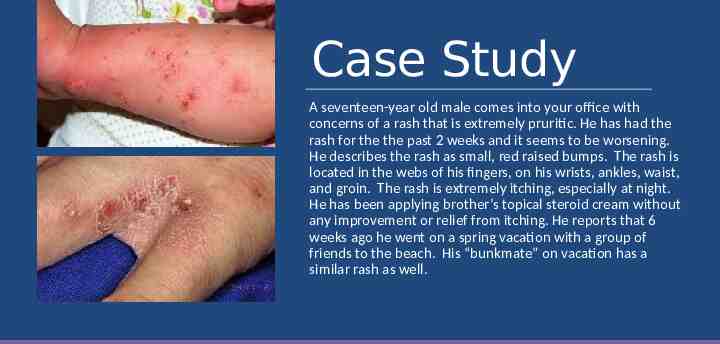
Case Study A seventeen-year old male comes into your office with concerns of a rash that is extremely pruritic. He has had the rash for the the past 2 weeks and it seems to be worsening. He describes the rash as small, red raised bumps. The rash is located in the webs of his fingers, on his wrists, ankles, waist, and groin. The rash is extremely itching, especially at night. He has been applying brother’s topical steroid cream without any improvement or relief from itching. He reports that 6 weeks ago he went on a spring vacation with a group of friends to the beach. His “bunkmate” on vacation has a similar rash as well.

What is this rash? A) Eczema B) Psoriasis C) Herpes Simplex D) Scabies
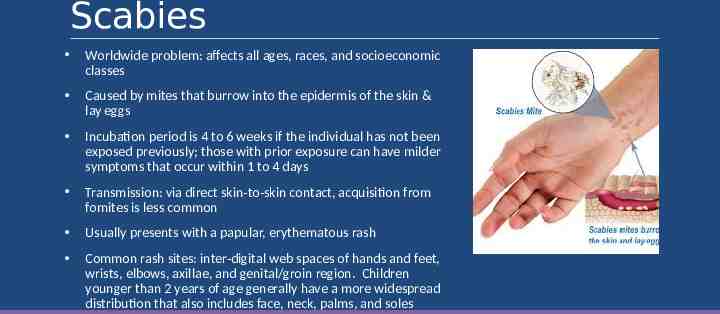
Scabies Worldwide problem: affects all ages, races, and socioeconomic classes Caused by mites that burrow into the epidermis of the skin & lay eggs Incubation period is 4 to 6 weeks if the individual has not been exposed previously; those with prior exposure can have milder symptoms that occur within 1 to 4 days Transmission: via direct skin-to-skin contact, acquisition from fomites is less common Usually presents with a papular, erythematous rash Common rash sites: inter-digital web spaces of hands and feet, wrists, elbows, axillae, and genital/groin region. Children younger than 2 years of age generally have a more widespread distribution that also includes face, neck, palms, and soles
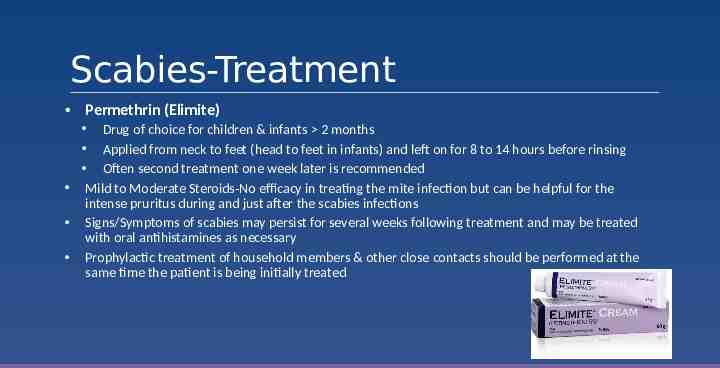
Scabies-Treatment Permethrin (Elimite) Drug of choice for children & infants 2 months Applied from neck to feet (head to feet in infants) and left on for 8 to 14 hours before rinsing Often second treatment one week later is recommended Mild to Moderate Steroids-No efficacy in treating the mite infection but can be helpful for the intense pruritus during and just after the scabies infections Signs/Symptoms of scabies may persist for several weeks following treatment and may be treated with oral antihistamines as necessary Prophylactic treatment of household members & other close contacts should be performed at the same time the patient is being initially treated
Question What information would you provide this patient & his family regarding things they should do to get rid of the infestation and prevent its spread? A) Bedding and clothing worn next to the skin during the 3 days before the initiation of therapy should be laundered in a washer with hot water and dried using a hot cycle for at least 10 minutes. B) Anything that cannot be washed should be removed from the patient & stored for several days, up to a week, to avoid re-infestation. C) Furniture and carpets in the household of an infected person should be vacuumed. D) He may return to school/work after treatment has been completed E) All of the above
Important things to assess Triaging Rashes Appear or act ill? Is there lip, tongue or throat swelling? Is the child breathing comfortably? Does the rash blanch? Other important questions to ask Fever Medications Any change in soap, lotions or detergents Any new clothes or bed linens not washed prior to using New foods Bites or stings Travel or camping

RED FLAGS Blistering, Skin Sloughing or Mucosal Involvement

RED FLAGS Diarrhea and/or Abdominal Pain

RED FLAGS Fever and inconsolability OR fever and petechiae/purpura

RED FLAGS Urticaria with Respiratory Distress
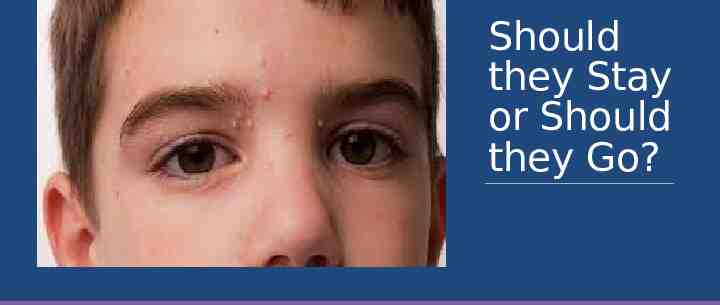
Should they Stay or Should they Go?

Should they Stay or Should they Go?

Should they Stay or Should they Go?
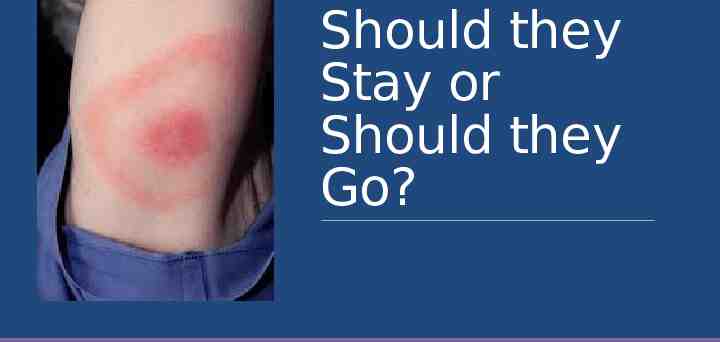
Should they Stay or Should they Go?

Should they Stay or Should they Go?
Should they Stay or Should they Go?
Should they Stay or Should they Go?
Should they Stay or Should they Go?

Should they Stay or Should they Go?

Should they Stay or Should they Go?

Questions?