May 2013 Update Medication Administration Approved by the Alaska Board
70 Slides435.88 KB
May 2013 Update Medication Administration Approved by the Alaska Board of Nursing for training Unlicensed Assistive Personnel/ UAPs

Why Medications Are Given Prescription vs. Over-the-Counter Medications Controlled Substances Why Give Medications as Prescribed? Factors Affecting Medication Levels and Responses in the Body Allergic Reactions to Medications Administration: Routes of Entry The Six Rights of Medication Administration Documentation Medication Errors The DON’Ts of Medication Administration How are Medications Named? Medication Packaging and Delivery Storage of Medications Medication Interactions Side Effects of Medications Medication Measurements Medication Classification Overdose, Toxic Dose, or Allergic Reactions Confidentiality What You Will Learn 2

» The human body does not always function perfectly. Most of us, at one time or another, will use some type of medication. » Medications are given in hopes of obtaining a desired effect that is beneficial. Why Meds are Given 3

» Preventing Illness Polio and Tetanus vaccines PREVENT illness » Eliminate a Disease Antibiotics such as penicillin ELIMINATE illness » Reduce Symptoms Related to Illness or Injuries Cold Remedies/suppressants and aspirin REDUCE symptoms » Replace Something the Body is Lacking Insulin Thyroid Medication Prevent, Eliminate, Reduce, Replace 4

» To ensure quality in the medical administration aspect of care, all caregivers should be competent in the following areas: Medication Administration Maintaining agency specific medication records and documentation for each individual The safe storage of all medications Knowing who to call if there are questions; having a list of contacts for questions and concerns Competency Required 5

» Prescribed medications: Require an order from a healthcare provider Physician Physicians Assistant Advanced Nurse Practitioner Osteopath Optometrist Podiatrist Dentist Must be obtained from a Pharmacy Prescribed vs Over-the-Counter 6

» Controlled Substances Prescription Controlled by the DEA (Drug Enforcement Agency, federal) Narcotics Pain Medications ADHD Medications like Ritalin Must have specific policies for handling (counting, disposing, etc.) By order of Controlled Substances 7

» Available without a prescription » Unlicensed caregivers-must have an order from parent or caregiver on file BEFORE giving the medication. » Be aware of the dangers of OTC medications, in excess or combined with other medications. Iron, aspirin, and Tylenol (acetaminophen) can be toxic in large doses Cold medicines can interact with Blood Pressure medications OTC’s: Over the Counter 8

» Additional Over-the-Counter Products: Nutritional Supplements (FDA approved) Herbal remedies » Must be pre-approved by the healthcare provider (MD, DO, PA, ANP) and documented each time administered Nutritional & Herbal 9

» All prescription and non-prescription (over-thecounter) medications, including vitamins or herbs, once approved by the healthcare provider, must be written on the medication record along with complete instructions for giving. » Must be complete documentation including what time they are given. Documenting Vitamins & Herbs 10

» Most medications work when they reach a certain blood level » Must reach a certain level for desired effect » If the level rises too high with some medications, they may be harmful » If the level is too low, the medication may not work Therapeutic Medication Levels 11

» Studies have been done to determine how often a medication should be given to obtain/maintain a therapeutic level in the body. » If medication is not given on time, the level may be too low or too high and be dangerous. » People with seizures may have breakthrough seizures if their medications are not given on time. » Diabetics risk high or low blood sugar if insulin is not given at the correct time & dose. Medications as Prescribed 12

» Many factors can determine whether a medication is appropriate for a particular person: Age Body Weight & Size Sex Pregnancy & Breastfeeding Genetic Factors Psychological Factors Illnesses Allergies » Always be aware of the person’s response to a medication and always report ANY changes in their condition. Factors to be Considered 13

» Age: as a person ages, their body is affected by several changes: Absorption: » Decreased absorption from intestines » Decreased blood flow » Increased gastric pH Distribution in the Body: » Decreased circulation » Decreased water in cells » Decreased protein in the blood » Increased body fat Factors, cont 14

Additional Factors for older adults Metabolism: » Decreased ability of liver to process drugs » Decreased blood flow & fewer liver cells Excretion by Kidneys: » Drugs excreted at a slower rate » Decreased blood flow » Kidney cells that do not function as well Factors, cont 15

» Children differ from adults in how they take in and process drugs in several ways: In infants, many systems are not fully developed to handle medications Blood-brain barrier isn’t fully developed The liver isn’t fully developed, so they cannot process meds properly Kidneys are immature so medications are excreted slowly Infants and children have higher concentrations of body water and lower concentrations of body fat Children 16

» Because of genetics, diseases, or injuries a person who is one age may have a body that responds like someone older or younger » Premature infants may have bodies that respond like a child much younger than their birth age » A person with heart, kidney, or liver disease may respond like someone older. IE: a 35 year old with kidney disease may process medications as if they were 50 years old. Chronological & Physical Age 17

» Is the patient able to swallow the medication as prescribed? » Is the patient vomiting so they cannot keep meds in their system long enough for absorption? » The larger the person, the more body tissue there is to absorb medications, affecting absorption & distribution. » Sex differences between men & women (hormones, body fat, muscle mass, fluids) affect how meds are absorbed and utilized in the body. Factors that Affect 18

» Pregnancy & Breastfeeding Medications taken by a pregnant woman can cross the placenta and affect the developing fetus. Some medications are toxic to the baby. Medications taken by a breastfeeding mother can be in the breast milk and taken in by the baby. » Always make sure the patient’s healthcare provider knows the patient is pregnant or breastfeeding. Pregnancy & Breastfeeding 19

» Genetic Factors Person’s with Down Syndrome age prematurely. A 40 year old has a body that acts like a 60 year old. Some genetic factors cannot be seen on the outside because they determine how cells on the inside process medications. » Psychological Factors Emotional factors, such as stress, affect how the body responds to medications. » Illness Diseases of the stomach, intestines, kidneys, liver & circulatory system will affect medication levels in the body Stomach/intestinal problems change absorption Other Factors 20

» Individuals can develop allergies to medications at any time » These allergies can be life-threatening » Always be aware of any current medication allergies of people you are caring for Allergies 21

Severe allergic reactions are known as Anaphylaxis » Signs may be: Skin Redness Rash Hives Runny Nose Difficulty Breathing Swelling (face,body) » Non-Life-Threatening: Mild Rash » LIFE-THREATENING: Difficulty Breathing Swelling of any body part Anaphylaxis 22

» What do you do? If you observe difficulty breathing and/or swelling of face or lips: Call 9 1 1 If you see an unexpected reaction Observe the person Hold the medication (do not give more) Contact healthcare provider for instructions Responding to Anaphylaxis 23

» Medications are absorbed or used by many different parts of the body: Skin, topical Lungs, inhaled Digestive System, swallowed » Factors affecting absorption: Body weight Age Gender Physiological status of a persons cells and tissues Diagnosis Dosage and route Genetics Immune status Psychological and emotional factors Medication Absorption 24

» Some medicines must be given with food » Some medicines must NOT be given with food » Always read ALL labels and handouts on each medication » A printout from the pharmacy or other source on each medication is needed. If one is lost or unreadable, get a new one » Call the pharmacy and request it if needed Medication Absorption, cont. 25

» 4 Ways Germs are Spread: 1. Airborne or Respiratory Route: When infected droplets from nose, mouth, sinuses, throat, lungs, from contaminated tissues or fabric when inhaled Tuberculosis, Colds, Chicken Pox, Influenza 2. Direct Contact Route: Occurs by directly touching the infected area or body fluid such as saliva, mucus, eye discharge, pus or spit Conjunctivitis (pink eye), impetigo, lice, poison ivy, chicken pox 3. Fecal-Oral Route: Enter the body from hands, food, mouthed toys, toilet, diaper that have been unintentionally infected with germs from stool Hepatitis A, Rotavirus 4. Blood Contact Route: Direct contact with infected blood or body fluids HIV/AIDS, Hepatitis B, Hepatitis C Routes of Transmission 26

» All communicable diseases are spread via one of those 4 ways » Some diseases cause only mild illness » Some diseases are life-threatening » Understanding the Route of Transmission directs our efforts in preventing the spread of disease Route of Transmission, cont. 27

Medications are administered in one of 8 ways: 1. Mouth, or Oral (po): swallowing tablets, capsules, liquids Sublingual means “under the tongue” and is absorbed or dissolved there. When a med is placed between the cheek and teeth, this is the “buccal” area. 2. 3. 4. 5. Topical: creams, lotions, ointments, drops, powders, oils and patches Eyes, or Ophthalmic: used for eye drops and ointments Ears: drops or ointments Intramuscular (IM), Intravenous (IV), Subcutaneous (SQ/SC): injected into the body. Only a doctor or nurse can do this, not a UAP 6. Rectal: always use gloves when using this route 7. Vaginal: douches, vaginal suppositories & creams. Wear Gloves 8. Gastrostomy or Jejunal Tubes: G-Tubes or J-Tubes are used when patient has difficulty swallowing so it goes directly into the stomach Routes of Entry 28

Important: 6 Rights of Medication Administration 1. The Right Person 2. The Right Medication 3. The Right Dose 4. The Right Route 5. The Right Time 6. The Right Documentation 6 Rights of Administration 29

The Right Person: Always look on the medication label & Medication Administration Record (MAR) to make sure the name matches the person Medications are to be used ONLY for the person whose name is on the label The Right Medication: The medication must be the one prescribed by the person’s healthcare provider Many medication names sound alike but are VERY different There can be several names for the same medication; generic, trade The Right Dose: The correct dose will be documented on the prescription label Multiple tablets or measuring liquids may need to happen to give the correct dose Abbreviations & measurements may be used & will be discussed later The Rights 30

The Right Route: This is the method with which it is given: oral, eye drops, ear drops, inhaler, rectal, vaginal, or topical The Right Time: Medications & Treatments must be given within 1 hour before, or 1 hour after the scheduled time Some medications are given at multiple times during the day Some medications are ordered for once a day or on different days of the week Most medications are ordered on a specific time schedule Some medications are ordered to be given “as needed” or “prn” Before giving a “prn” medication you must: 1. Have written instructions of WHEN to administer 2. Written instructions that you follow for administering which includes the dosage amount, how often, and how long 3. And when to contact the Nurse The Rights 31

The Right Documentation: The Medication Administration Record (MAR) is used to document the administration of all medications After the medication is given, your initials are written in the correct box to note the time it was given If the medication is NOT given, circle your initials and document in the narrative why it was not given Whatever system is used, the purpose of documentation, from a legal perspective, is to always accurately & completely record the care given to individuals, as well as their response to that care Documentation is CRUCIAL. It is a permanent record and a legal one. A familiar phrase in healthcare is “If it wasn’t documented, it wasn’t done.” Documentation must be complete & legible Draw a single line through an erroneous entry to identify it as an error Always follow your agency’s policies for documentation The Rights 32

» A medication error is any time that: 1. 2. 3. 4. 5. 6. The right medication is not administered To the right person At the right time In the right amount Or by the right route Or if it is not documented correctly Medication Errors 33

» Steps to take if a Medication Error occurs: 1. Always check the level of consciousness & breathing of the person first 2. If there are breathing problems, seizures, or difficulty arousing the person, Call 9-1-1 3. Call the healthcare provider who prescribed the medication 4. If the provider does not respond within 1 hour, call the emergency room for guidance 5. Provide care if needed 6. Call the nurse or your supervisor 7. Document per your agency policy Medication Errors 34

» The “Don’ts” of Medication Administration Don’t administer medications that aren’t filled by a pharmacy or a healthcare provider with an original label Don’t administer one person’s medication to another person Don’t double up on a missed dose unless instructed to by the primary healthcare provider Don’t cut or crush an un-scored pill without the “OK” of the pharmacist or healthcare provider Don’t document until you give the medication Don’t try to hide your mistakes Don’t ask another person to perform the task you are responsible for Medication administration is a serious responsibility & may not be transferred Medication Don’ts 35

» How are medications named? All medications have two names Trade or Brand Name: chosen by the drug manufacturer & picked to be simple or memorable. Brand names are capitalized Generic Name: generally derived from the chemical structure of the drug. The generic name is always lower case; used in scientific literature and reports Two VERY different medications can have very similar generic names. (fluoxetine & fluvoxamine is one example) Medication Naming 36

» Pharmacy’s package in two methods: Medisets May be in the form of blister packs, bubble packs or reusable hard cases Contain medications for an entire week Delivered on the same day of every week Clear plastic cover on the front of the package to ensure easy inspection of the medications by the caregiver Mediset Label state: Name Start/end date Prescription Number Name of Med Name & number of prescriber Medication directions Dosage Time and amount Pill descriptions # Pills in bottle # Refills Notes identifying medications needing provider renewal Packaging & Delivery 37

Pharmacy Bottles Contains one type of medication Enough for 1-3 months May be liquid, tablet, capsule Pharmacy Bottle Label Individuals’ name Prescription number Name of med Name/number of prescriber Directions Number of capsules/tablets Number of refills How to take med (ex. with food) Packaging, cont 38

Medications should be secured so they cannot be tampered with or accidentally eaten Refrigerated medications should have safeguards, such as locked cabinet or drawers Medications should be kept in the original container or meidset, with original labeling Topical medications should be stored separately from internal medications Each person should have his/her own compartment, bin, or area for his/her own medications Are to be used ONLY by the person for whom they are prescribed Should not be used after the expiration date Dispose of medications according to your agency’s policy Medication Storage 39

Medication Interactions are when a combination of medications cause an effect that can be a desired effect or an unwanted effect The chances of a drug interaction increases when a person is taking several medications A HCP should always be aware of all medications one takes including OTC’s such as vitamins, cold meds, laxatives, or pain relievers Always obtain a specific order from the HCP for each medication If a HCP discontinues a medication, make sure they write it down If a HCP adds a new medication, this may affect the levels of other medications Med interactions may increase or decrease the effects of one or more meds. Ex: antacids given with an antibiotic may prevent the antibiotic from being absorbed in stomach, therefore, there would be no effect on the bacteria it is supposed to treat Medication Interactions 40

Foods may have a certain effect on medications. If it says to take on an empty stomach, do so. All prescription, non-prescription, vitamins, herbs, once approved by the HCP, must be written on the Medication Record with complete instructions for giving Must be documentation completed indicating when the medications were given Medication Interactions, cont. 41

Watch for any side effects when a new medication has been started, especially during the first few days Observe & report any changes in physical or behavioral well being to your contact person Document any changes and who you reported the changes to Some meds need time to reach optimal blood levels before seeing their side effects: Anti-depressants or psychotropics Side Effects 42

Why is this medication being used? What is the intended effect? Therapeutic action or therapeutic effect What are the likely unintended effects? Side effects Is the medication compatible with other medications being taken? Medication interactions What to Know? 43

The healthcare provider prescribing the med The agency nurse or nurse practitioner The pharmacist Medication manufacturers (ask for the medication insert when filling the Rx) Attention Warning: this is a general medication administration training module. Each caregiver must be trained and checked off by the agency nurse on each individual’s specific medication needs before administering medications. Where Can I Get More Information? 44

Now What? As a person caring for or providing support for an individual, YOU are responsible for that person If you have ANY concern about the person you are supporting or their medication, contact: Their HCP, Pharmacist, or Agency Staff IMMEDIATELY. Call 911 for Serious Emergency What to Do? 45

PDR: Physicians Desk Reference Nursing Drug Books Drugs in Pregnancy and Lactation www.drugs.com Pharmacy where the prescriptions were filled Patient’s healthcare provider, call if you have questions! Sources for Medication Information 46

Anyone can post information on the Internet. This information is NOT always correct! Some people dislike medications and so will post false information about them Check to make sure the information came from a drug company or healthcare institution www.webmd.com www.mayoclinic.com www.drugs.com The Internet 47

» Doctors, Nurse Practitioners and other HCPs may give patients sample of medications » All medication samples should be labeled with: The HCP’s name and address Date medication was given to patient Medication name Medication dose When medication should be taken » DO NOT give sample medications to a patient if this information isn’t on the sample! Meds from HCP’s 48

» Hand Washing » Universal Precautions » Gloves » Common Metric Measurements you should know: Most capsules and tablets are in milligrams (mg) or grams (gm) 1000 mg 1 gram 500 mg 0.5 gram 250 mg 0.25gram Administration 49

» Scenarios 1. You have Dilantin 100 mg capsules. John needs 400mg to be taken at bedtime. 4 100 mg capsules 400 mg 2. You need a dose of 1 gram of Tylenol. You only have 500 mg (0.5gram) tablets 2 500 mg tables 1000 mg 1 gram Warning: when a new medication comes into the home, make sure it is the SAME strength or dose as the old medication! Administration, cont 50

» Commonly used abbreviations for prescriptions: am morning cc cubic centimeter h or hr hour hs at bedtime ml milliliter pm afternoon; evening po by mouth prn when required sup or supp suppository tab tablet Tbsp tablespoonful tsp teaspoonful mg milligram Abbreviations 51

» When preparing a liquid dose of medication, caregiver holds the measure at eye level, with thumbnail resting on calibration that marks the level to which liquid should be poured. » Liquid Measurement (volume) 1 ml 1 cc 2 ½ ml ½ teaspoon (tsp) 5 ml 1 teaspoon (tsp) 15 ml 3 teaspoons (tsp) 15 ml 1 Tablespoon (Tbsp)/0.5 fluid ounce 30 ml 1fluid ounces (oz) Liquid Medication 52

» Most liquids are measured in milliliters (ml) or liters (L) » 5ml 5cc 1 teaspoonful (tsp) » 15ml 15cc 1 tablespoon (Tbsp) » 30ml 30cc 1 ounce (oz) » 240ml 240cc 8 ounces (oz) 1 cup (c) » A ml is 1/1000th of a liter, and a cc is one cubic centimeter Liquid Measures 53

» The strength of liquid medicine is measured in mg/ml » The number of mg of medicine in each ml, for example, of Amoxicillin suspension may have 250 mg/5 ml or diphenhydramine elixir (Benadryl) has 12.5 mg/5 ml Warning: when a new medication comes into the home, make sure it is the same strength or dose as the old medication. Strength of Liquid Meds 54

» Example: » Your directions say to give 1 tablespoonful of cough syrup every 4 hours as needed » You know the soup spoon is not accurate » You choose to measure using a metric cup » You know that you would give 15 ml because this equals 1 tablespoonful Strength of Liquid Meds, cont. 55
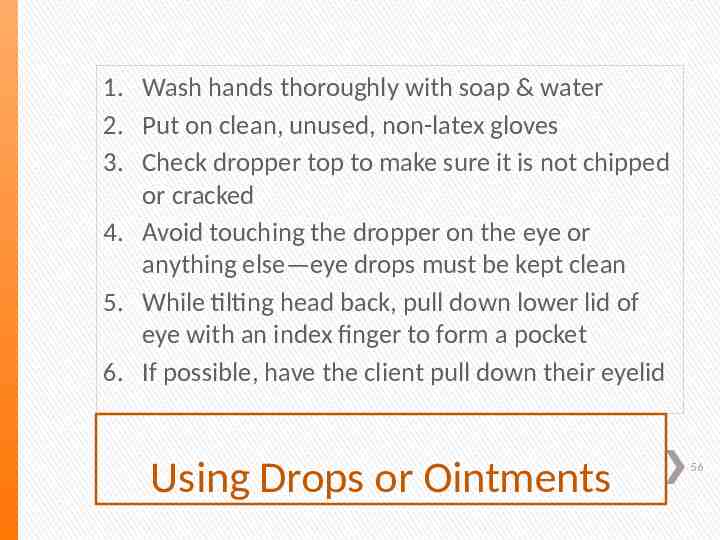
1. Wash hands thoroughly with soap & water 2. Put on clean, unused, non-latex gloves 3. Check dropper top to make sure it is not chipped or cracked 4. Avoid touching the dropper on the eye or anything else—eye drops must be kept clean 5. While tilting head back, pull down lower lid of eye with an index finger to form a pocket 6. If possible, have the client pull down their eyelid Using Drops or Ointments 56

7. With the other hand, hold dropper tip as close to the eye as possible without touching it 8. Brace the remaining fingers of the hand against the face 9. Gently squeeze the dropper so that the correct number of drops fall into the pocket made by the lower eyelid 10. Close the eye for 2-3 minutes. Wipe away any excess with tissue 11. Replace and tighten the cap right away. Do not wipe or rinse the dropper tip 12. Remove gloves and wash hands Using Drops or Ointments, cont 57

» Medications are placed into categories or classifications based on the type of medication, its desired outcome or effect on the body, and type of illness or problem that it tackles. Antibiotics, Bacteria Killers Anti-Virals, Virus Inhibitors or Killers Anti-Fungal, Yeast or Fungi Inhibitors or Killers Cardiovascular Drugs, Heart, High Blood Pressure meds » Central Nervous System Medications: Anti-Convulsants, prevents seizures Sedatives Anti-Psychotics Anti-Depressants Anti-Anxiety Stimulants Medication Classifications 58

» Other Medications classified by their action on the brain: Therapeutic Action Stimulants Beta Blockers Opiate Blockers Effect Examples Treat Attention Deficit methylphenidate Hyperactivity Disorder (Ritalin) (ADHD) dextroamphetamine (Dexedrine) pemoline (Cylert) Treat some forms of propranolol (Inderal) severe aggression Treat some forms of naltrexone (RiVea) self injurious behaviors Central Nervous System Meds 59

» Overview & General Psychotropic medications are medications prescribed to stabilize or improve mood, mental status, or behavior. They are used to modify emotions or behavior. Sometimes called “psychiatric” or “psychoactive” medications. Some medications may have more than one purpose. Tegretol (carbamazepine) may be used to control seizures in an individual with epilepsy. Tegretol can be used to reduce mood swings in a person with Bipolar disorder. When used in this way, it is called a psychotropic medication. Psychotropic Medications 60

» Many service providers & families find the therapeutic action grouping the most useful: Therapeutic Actions Antidepressants Effect Examples Elevate mood in people who are depressed fluoxetine (Prozac) paroxetine (Paxil) sertraline (Zoloft) imipramine (Tofranil) Antianxiety Used to treat anxiety disorders and reduce anxiety symptoms clonazepam (Klonapin) lorazepam (Ativan) buspirone (BuSpar) Mood Stabilizers Reduce mood swings in individuals with manicdepressive illness carbamazepine (Tegretol) lithium (Lithonate) valproic acid (Depakene, Depakote) Antipsychotics or Neuroleptics Treat psychotic disorders such as schizophrenia. Reduce psychotic symptoms haloperidol (Haldol) risperidone (Risperdal) olanzapine (Zyprexa) Psychotropic Medications, cont 61

» A high dose of medication can be poisonous or harmful to the patient » Symptoms Include: Blurred or double vision Convulsions/seizures Muscle weakness that is severe Confusion Shortness of breath Unusually sleepy or groggy Vomiting » If you notice any symptoms of overdose, toxic dose or adverse reactions, you must ACT! » If the reaction seems to be life-threatening, call 9-1-1 Adverse Reactions 62

» Watch for the following signs/symptoms of lifethreatening Anaphylaxis: Hives Wheezing Generalized Itching Sore or Itchy Throat Difficulty Breathing Abdominal Cramps Low Blood Pressure/Shock Swelling in the Throat Itching of the Eyes or Nose Cough Flushing of the Skin Increased Heart Rate Anaphylaxis Symptoms 63

Points to Remember: 1. These generalized reactions can usually be easily reversed if treated early, BUT they can be lifethreatening without immediate medical attention. 2. Severe allergic reactions can occur from medications, insect stings, injections, or food. 3. Some people with allergies, such as bee stings or peanuts, have a device called an Epipen prescribed by their health care provider. If the person you support uses one of these devices, you will need to receive additional training! Anaphylaxis Symptoms, cont 64

o Tardive Dyskinesia is a neurological syndrome caused by the longterm use of neuroleptic medications. o Neuroleptics are generally prescribed for psychiatric disorders as well as for some gastrointestinal and neurological disorders. o It is characterized by repetitive, involuntary, purposeless movements. o Features of the disorder may include: Grimacing Tongue Protrusion Lip Smacking Lip Puckering Lip Pursing Rapid Eye Blinking Rapid Movements Impaired Finger Movements (playing invisible (arms, legs, trunk) guitar or piano) If this occurs, let the health care provider and your supervisor know. Tardive Dyskinesia 65

Prognosis for Tardive Dyskinesia? The symptoms of Tardive Dyskinesia may remain long after the neuroleptic medication has been discontinued. With careful management, some symptoms may improve and disappear over time. Tardive Dyskinesia, cont 66

A possible life-threatening emergency is associated with the use of neuroleptic medications such as Haldol. Symptoms include: Sudden Fever Rapid Pulse Rigidity Shaking Red Sweaty Skin Street drugs, such as Ecstasy, can also cause these symptoms. Call 9-1-1 Immediately Neuroleptic Malignant Syndrome 67

A person’s illnesses & medications are considered a private matter to be discussed only with a health care provider, other health providers, and family or care givers. A care giver should always be aware of this responsibility and never discuss any matter pertaining to health or medications with any other person not involved in the care of the patient unless you have the specific written consent of the person and his/her guardian. There are laws that protect a persons right to privacy of their health information. A person/patient has the right to refuse medication. You must always be respectful of the patient and familiar with your agency’s Patient Bill of Rights. Confidentiality 68

To ensure quality care and the safety and wellbeing of every individual, each caregiver must be competent and knowledgeable. The caregiver must know specific information about the individual and their ordered medication. The caregiver should be knowledgeable about the process of medication administrations and specific policies of their agency. The caregiver is expected to know when to ask for help and when to report problems. In Summary 69

This PowerPoint was edited and recreated from the Alaska Board of Nursing website document by Nancy Edtl, MBA, RN, BSN, NCSN; director of Nursing & Health Services, Anchorage School District. November 2012. Updated again in May 2013 by Nancy Sanders. 70