Management of Pediatric Behavioral Health Disorders In An Integrated
46 Slides4.98 MB
Management of Pediatric Behavioral Health Disorders In An Integrated Pediatric Medical Home Stephanie Chapman, PhD, Assistant Professor Baylor College of Medicine, The Center for Children and Women Sydnee Lucas, DNP, RN, APRN, FNP-BC Stephanie Marton, MD, Assistant Professor, Baylor College of Medicine, Associate Medical Director, The Center for Children and Women
Faculty Disclosure The presenters of this session have NOT had any relevant financial relationships during the past 12 months.
Learning Objectives Learners will be able to describe Clinic process that support successful interdisciplinary and integrated treatment of pediatric behavioral health disorders The role of psychiatric providers as curbside consultants to behavioral health and pediatric providers Outcome data related to the care of pediatric behavioral health diagnoses, including clinic prevalence rates, rates of engagement of patients in behavioral health services, and rates of patients receiving medication management from the PCP versus a psychiatric provider.
Management of Pediatric Behavioral Health Disorders In An Integrated Pediatric Medical Home
TCHP The Center for Children and Women

Integrated Behavioral Health Care Cost Effective Service Gap in Tertiary Care Mental and Physical Health Interwoven Reduces Stigma Increases Accessibility Funk & Ibvijaro , 2008
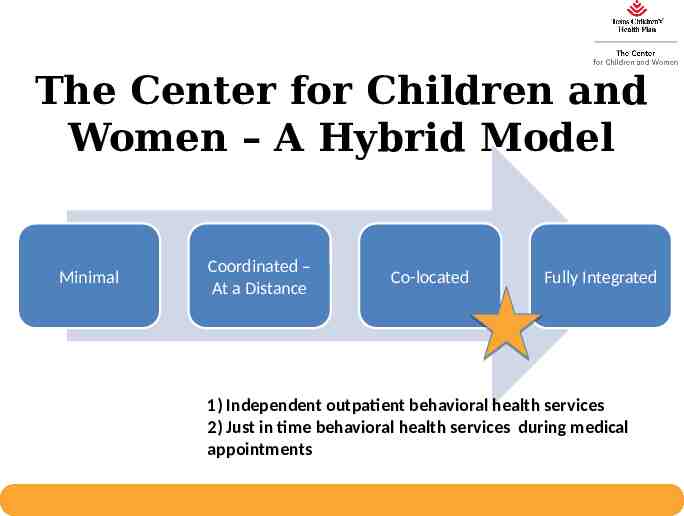
The Center for Children and Women – A Hybrid Model Minimal Coordinated – At a Distance Co-located Fully Integrated 1) Independent outpatient behavioral health services 2) Just in time behavioral health services during medical appointments
Location of the Facility
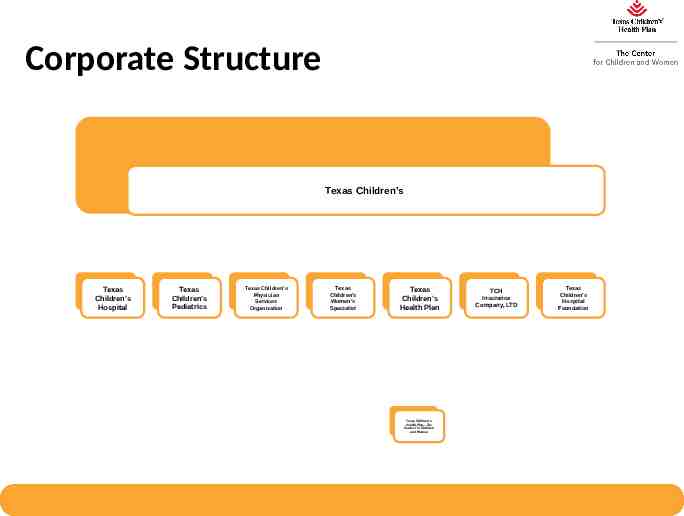
Corporate Structure Texas Children’s Texas Children’s Hospital Texas Children’s Pediatrics Texas Children’s Physician Services Organization Texas Children’s Women’s Specialist Texas Children’s Health Plan Texas Children’s Health Plan—The Center For Children and Women TCH Insurance Company, LTD Texas Children’s Hospital Foundation
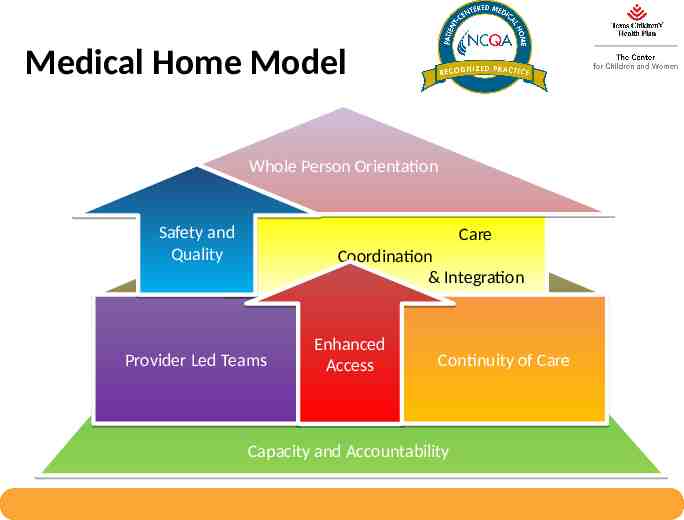
Medical Home Model Whole Person Orientation Safety and Quality Care Coordination & Integration Provider Led Teams Enhanced Access Continuity of Care Capacity and Accountability
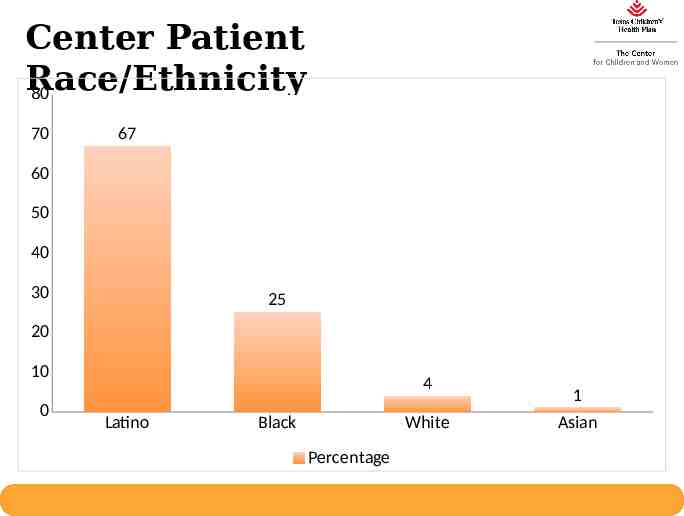
Center Patient Race/Ethnicity 80 70 67 60 50 40 30 25 20 10 0 4 Latino Black White Percentage 1 Asian
Funding – Capitated Payment Flat fee per patient member 100% Risk model Value: No fee for service ability to innovate Value on prevention and maintenance Incentives for reducing costs
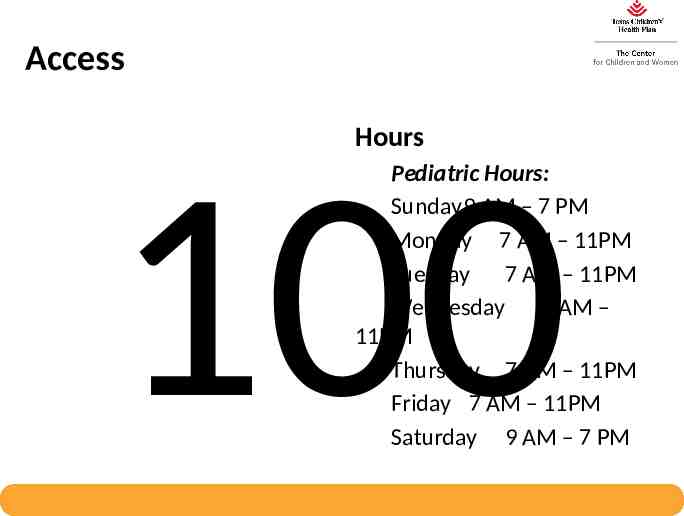
Access Hours Pediatric Hours: Sunday9 AM – 7 PM Monday 7 AM – 11PM Tuesday 7 AM – 11PM Wednesday 7 AM – 11PM Thursday 7 AM – 11PM Friday 7 AM – 11PM Saturday 9 AM – 7 PM 100
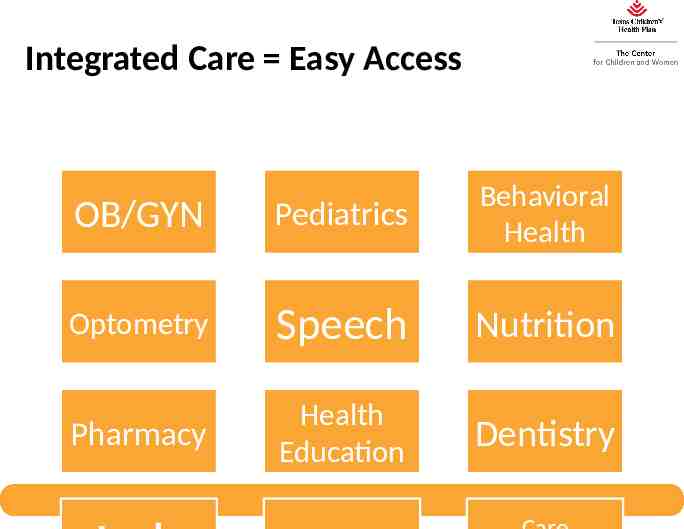
Integrated Care Easy Access OB/GYN Pediatrics Behavioral Health Optometry Speech Nutrition Pharmacy Health Education Dentistry

OVERVIEW OF BEHAVIORAL HEALTH
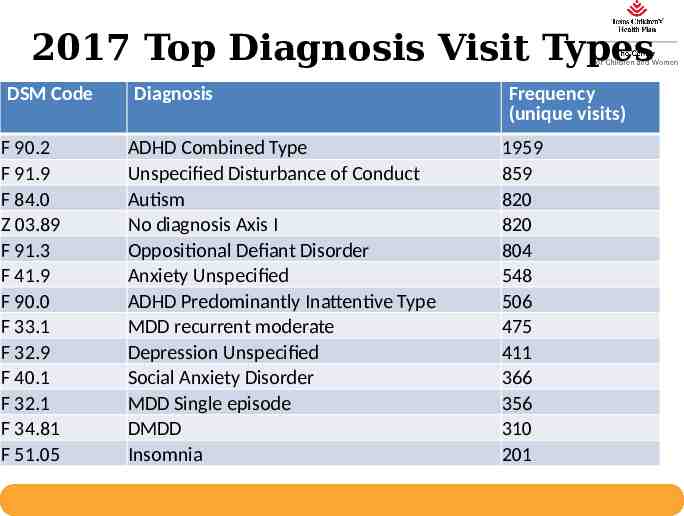
2017 Top Diagnosis Visit Types DSM Code F 90.2 F 91.9 F 84.0 Z 03.89 F 91.3 F 41.9 F 90.0 F 33.1 F 32.9 F 40.1 F 32.1 F 34.81 F 51.05 Diagnosis ADHD Combined Type Unspecified Disturbance of Conduct Autism No diagnosis Axis I Oppositional Defiant Disorder Anxiety Unspecified ADHD Predominantly Inattentive Type MDD recurrent moderate Depression Unspecified Social Anxiety Disorder MDD Single episode DMDD Insomnia Frequency (unique visits) 1959 859 820 820 804 548 506 475 411 366 356 310 201
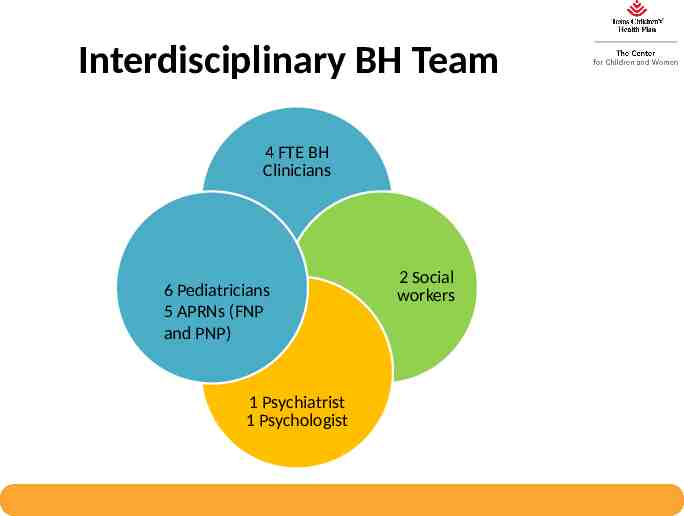
Interdisciplinary BH Team 4 FTE BH Clinicians 6 Pediatricians 5 APRNs (FNP and PNP) 1 Psychiatrist 1 Psychologist 2 Social workers
Integrated Practice Definition – percentage of patients seeing BH providers on same day as medical appointments Target goal: 15%

Engagement in BH Care Definition – percentage of BH members as proportion of total membership Target goal: 15% of total center active population
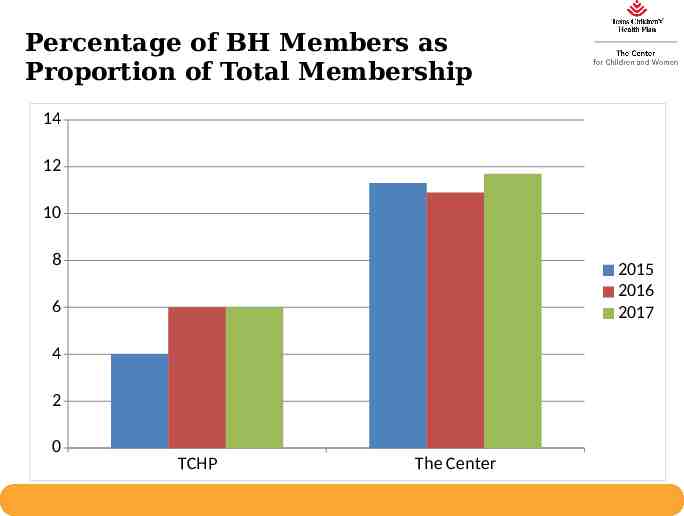
Percentage of BH Members as Proportion of Total Membership 14 12 10 8 2015 2016 2017 6 4 2 0 TCHP The Center
BEHAVIORAL HEALTH CARE – ADHD AND DEPRESSION / ANXIETY

Behavioral Health Care Interventions Screening Evidence-based Therapy Care Coordination School Accommodations Diagnostic Assessment Medication Management
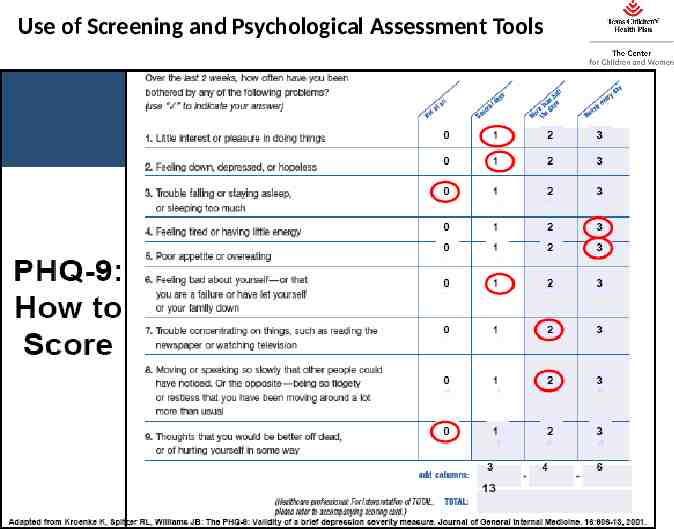
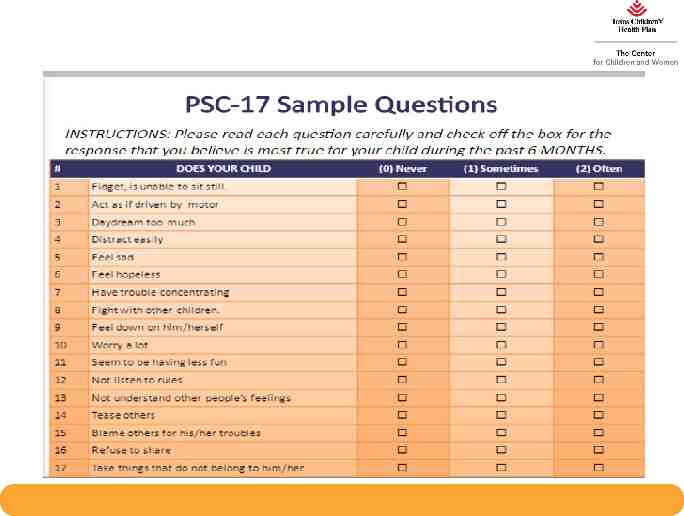
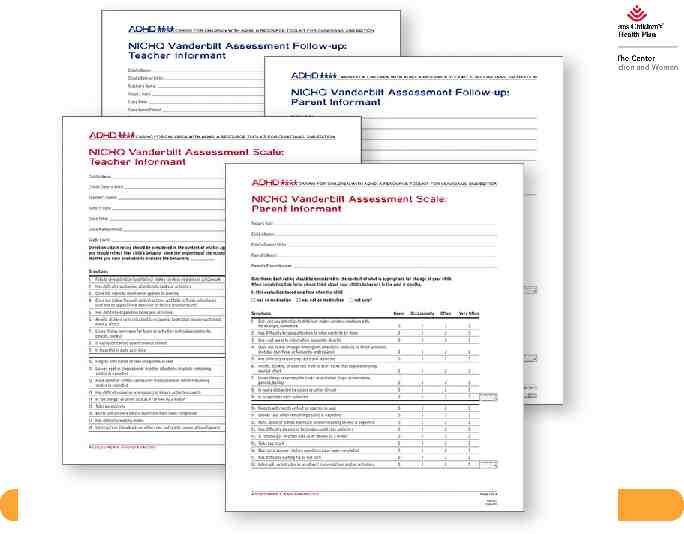
Use of Screening and Psychological Assessment Tools
Evidence-Based Treatments Parent Management Training – A brief (4-10 session) therapy designed to teach parents skills to change child behavior – Effective for a variety of presenting problems: Enuresis/Encopresis Sleep disturbances Feeding difficulties ODD, ADHD, and DBD
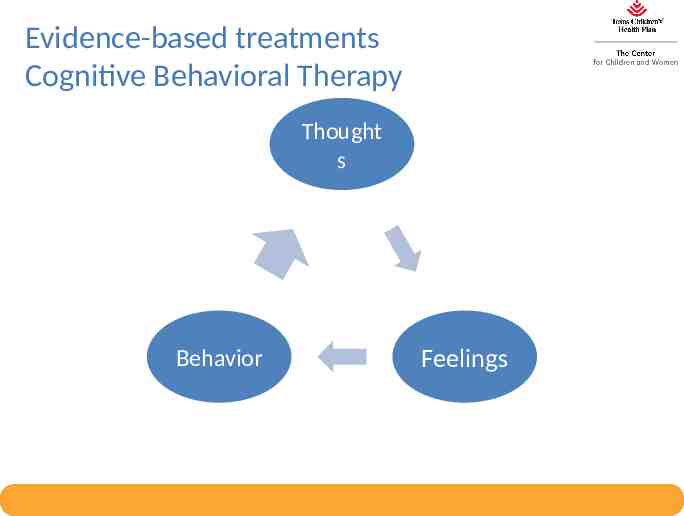
Evidence-based treatments Cognitive Behavioral Therapy Thought s Behavior Feelings

Evidence Based Treatments – Exposure Therapy
Evidence-Based Treatments Motivational Interviewing Medication and Treatment Adherence Substance Reduction Health Goal maintenance
Coordination of Care Patient Registries Staffed regularly by social work and care coordinators ADHD Follow-Up 7 and 30 Day Psych Hospital Followup Maternal Depression Screen Followup
Telehealth Increases Access Telehealth 7% of Psychiatry encounters Contributes to 100% psychiatry template utilization
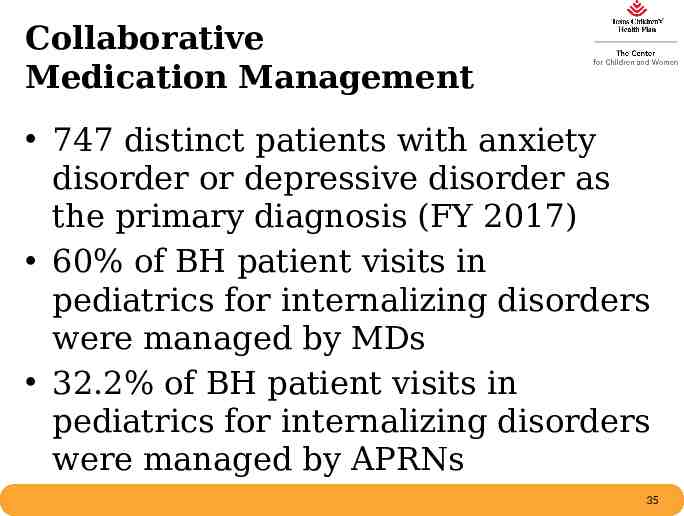
Collaborative Medication Management PCP – Medication Management Protocols standardize care Increase timely access to care for medication titration
Medication Management BH Clinicians and PEDI/OBGYN providers partner to manage the majority of BH medications ADHD Anxiety Depression Sleep Psychiatry - 30 % of time allocated to curbside consult Psychiatrist only sees patients with complex psychiatric disorders
Medication Management BH Clinicians and PEDI/OBGYN providers partner to manage the majority of BH medications ADHD – APRNs do not prescribed for ADHD, however can provide the screening tools and consult with BH to ensure timely follow up and management Depression / Anxiety – APRNs and MDs both screen for and manage depression and/or anxiety in our pediatric patients with the partnership of our BH team
Collaborative Medication Management 747 distinct patients with anxiety disorder or depressive disorder as the primary diagnosis (FY 2017) 60% of BH patient visits in pediatrics for internalizing disorders were managed by MDs 32.2% of BH patient visits in pediatrics for internalizing disorders were managed by APRNs 35
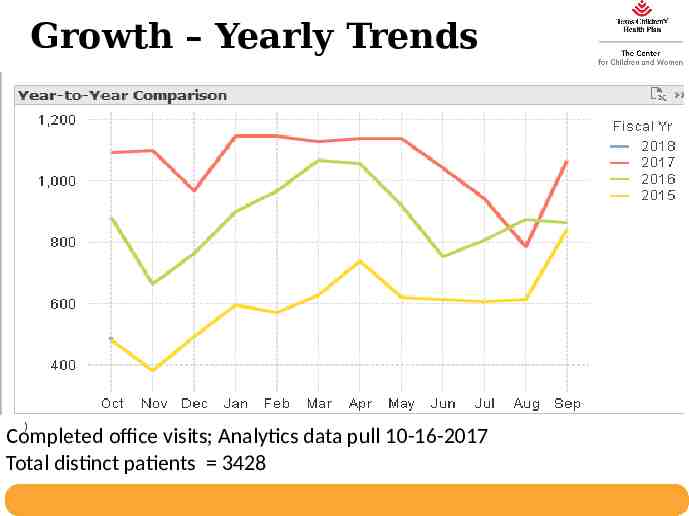
Growth – Yearly Trends ) Completed office visits; Analytics data pull 10-16-2017 Total distinct patients 3428
Center PEDI Medication Management Good Psychiatry Referrals Patients with complex psychotropic medications Patients with psychiatric histories other than ADHD / depression/anxiety Lack of progress with first line treatments Children under 6 years Psychiatry can always be consulted In basket Curbside consult Patient office visit
Case Example – John 16 yo male who presents for his well child check PSC-17 is elevated; pediatric provider asks further questions of child – Concerned that child may be depressed – Real time behavioral health consult Depression diagnosed at visit by psychologist – SSRI started same day
John returns Behavioral health team calls John in one week to check on his symptoms, he is doing well with no side effects noted At follow-up in clinic in 2 weeks John has had some stomach aches and no real change in mood – Pediatric team increases SSRI dose – Behavioral health team provides therapy same day
John continues to return Over next month behavioral health team sees John twice He returns to pediatric clinic and reports he has more energy but still does not see a change in his mood – Pediatric team briefly curbsides psychiatry to enquire as to how long should John stay on same medication with no change in his mood
John returns John is maintained same dose of SSRI for an additional month with continued therapy After 2 months John reports he is having more energy and improved mood Therapy continues. Behavioral health team messages pediatric team that he is doing well and pediatrician team refills medication for an additional month. John stops coming to therapy; pediatrician continues SSRI and checks in with therapist when he comes for medication management visits.
John John’s symptoms were caught early through annual screening exam and he was never hospitalized. A team of multidisciplinary healthcare providers were able to manage John’s symptoms; he was never seen by psychiatry. John’s treatment was successful due to frequent communications and a modifiable treatment plan. John received cost-effective, quality care.
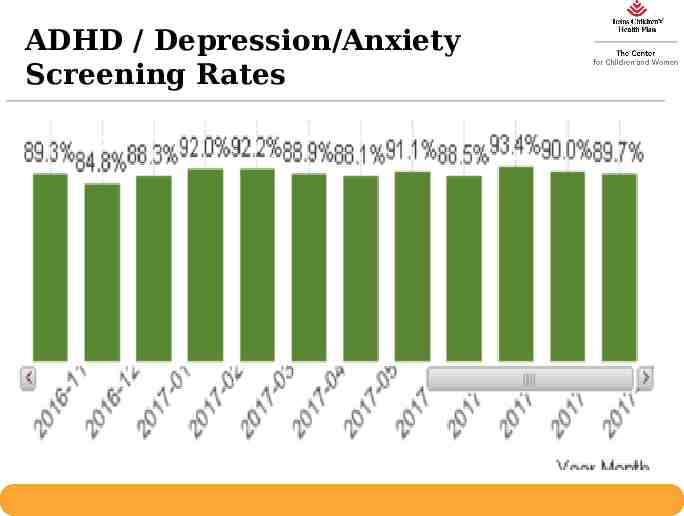
ADHD / Depression/Anxiety Screening Rates
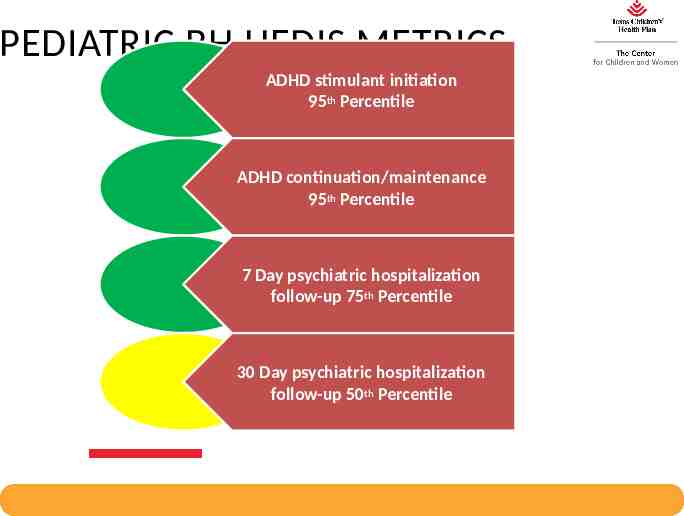
PEDIATRIC BH HEDIS METRICS ADHD stimulant initiation 95th Percentile ADHD continuation/maintenance 95th Percentile 7 Day psychiatric hospitalization follow-up 75th Percentile 30 Day psychiatric hospitalization follow-up 50th Percentile
RIGHT CARE / RIGHT PLACE - BEHAVIORAL HEALTH Behavioral Health Integration Increases Engagement in Underserved Communities
Thank you!