Integrated care pathways Dr Jeremy Rogers MD MRCGP Senior
18 Slides306.50 KB

Integrated care pathways Dr Jeremy Rogers MD MRCGP Senior Clinical Fellow in Health Informatics Northwest Institute of Bio-Health Informatics
Talk Outline ICPs eICPs Challenges
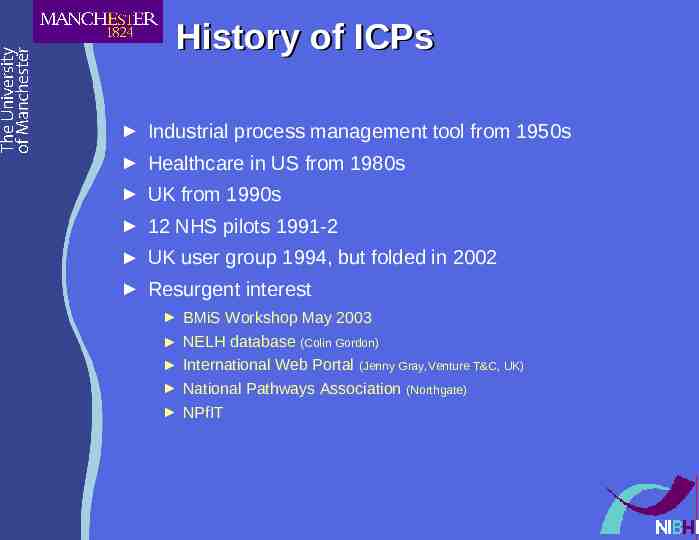
History of ICPs Industrial process management tool from 1950s Healthcare in US from 1980s UK from 1990s 12 NHS pilots 1991-2 UK user group 1994, but folded in 2002 Resurgent interest BMiS Workshop May 2003 NELH database (Colin Gordon) International Web Portal (Jenny Gray,Venture T&C, UK) National Pathways Association (Northgate) NPfIT
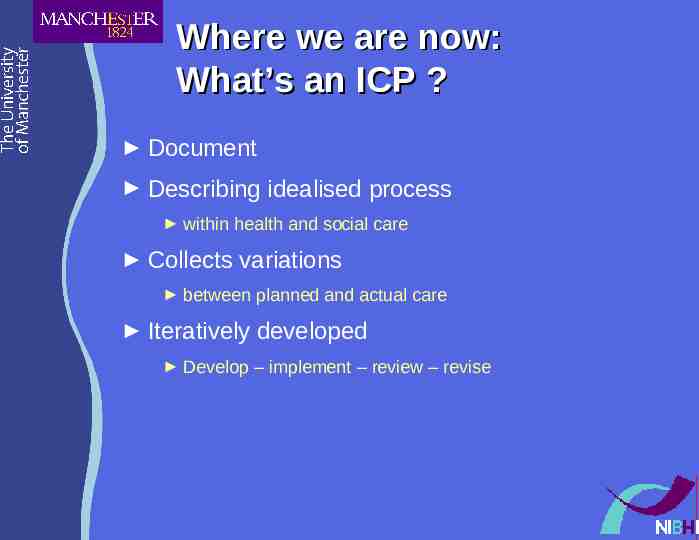
Where we are now: What’s an ICP ? Document Describing idealised process within health and social care Collects variations between planned and actual care Iteratively developed Develop – implement – review – revise
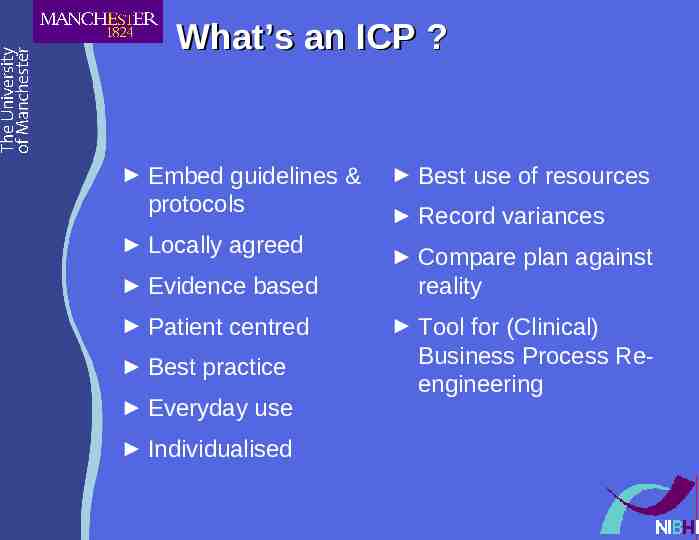
What’s an ICP ? Embed guidelines & protocols Locally agreed Evidence based Patient centred Best practice Everyday use Individualised Best use of resources Record variances Compare plan against reality Tool for (Clinical) Business Process Reengineering
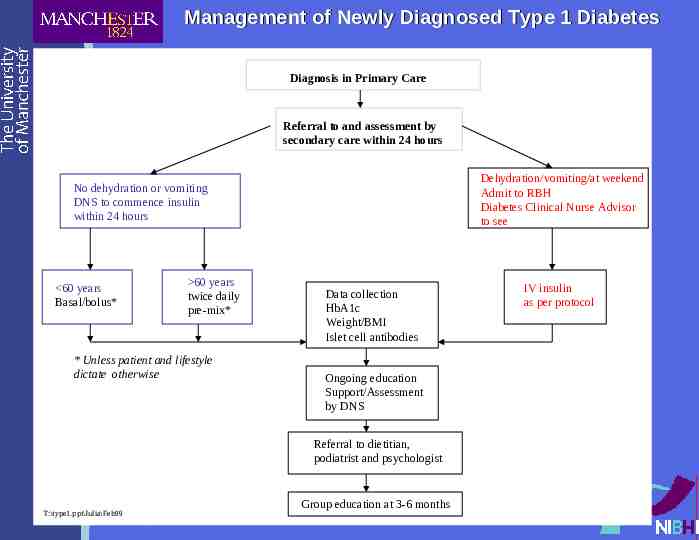
Management of Newly Diagnosed Type 1 Diabetes Diagnosis in Primary Care Referral to and assessment by secondary care within 24 hours Dehydration/vomiting/at weekend Admit to RBH Diabetes Clinical Nurse Advisor to see No dehydration or vomiting DNS to commence insulin within 24 hours 60 years Basal/bolus* 60 years twice daily pre-mix* * Unless patient and lifestyle dictate otherwise Data collection HbA1c Weight/BMI Islet cell antibodies Ongoing education Support/Assessment by DNS Referral to dietitian, podiatrist and psychologist T:\type1.ppt\Julia\Feb99 Group education at 3-6 months IV insulin as per protocol
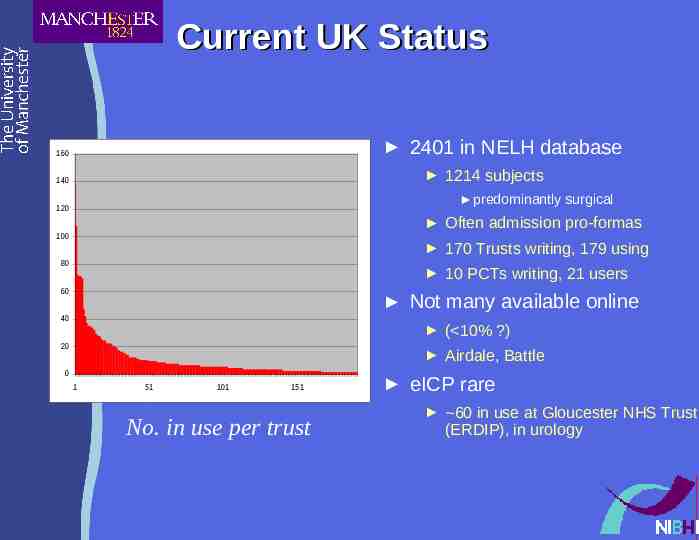
Current UK Status 2401 in NELH database 160 1214 subjects 140 predominantly surgical 120 Often admission pro-formas 100 170 Trusts writing, 179 using 80 10 PCTs writing, 21 users 60 Not many available online 40 ( 10% ?) 20 Airdale, Battle 0 1 51 101 151 No. in use per trust eICP rare 60 in use at Gloucester NHS Trust (ERDIP), in urology
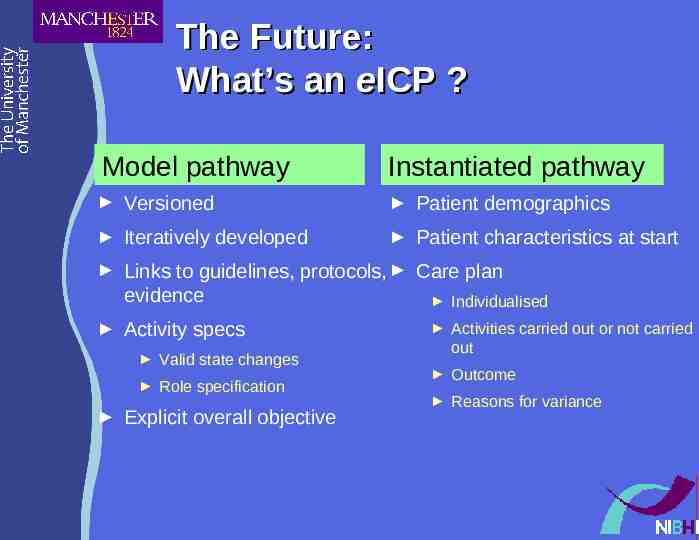
The Future: What’s an eICP ? Model pathway Instantiated pathway Versioned Patient demographics Iteratively developed Patient characteristics at start Links to guidelines, protocols, Care plan evidence Individualised Activity specs Valid state changes Role specification Explicit overall objective Activities carried out or not carried out Outcome Reasons for variance
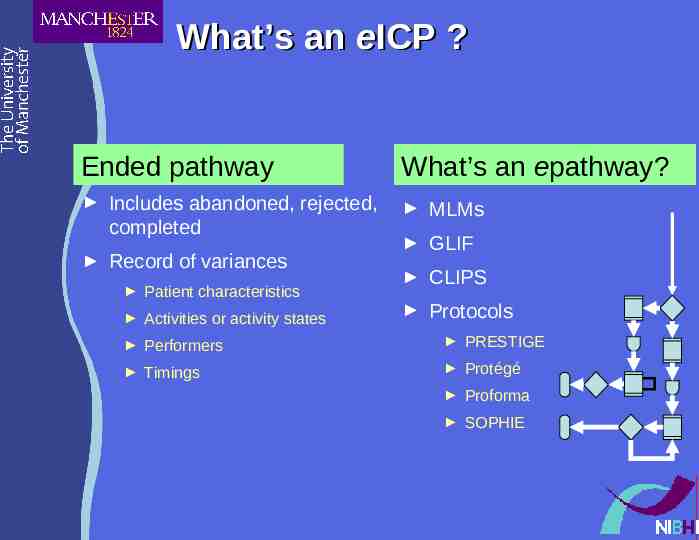
What’s an eICP ? Ended pathway What’s an epathway? Includes abandoned, rejected, completed MLMs Record of variances Patient characteristics Activities or activity states GLIF CLIPS Protocols Performers PRESTIGE Timings Protégé Proforma SOPHIE
eICP in NPfIT Phase I (2004/5) Ability to construct and use ICPs Migrate paper ICPs to eICPs Record total journey times Phase II (2006) Model care pathway Instantiated care pathway Ended care pathway By 2010 All singing all dancing
Automated eICPs ? ‘Evidence-based action at the point of care instantaneously triggers follow on actions elsewhere in the system’ Tackaberry, iSoft (2000) ‘Automatic identification and invoking of workflow, alerts, review and guideline activation’ NPfIT OBS 2003
Implementation: Barriers to the Future Human Factors Technical Factors Cultural Time & Scale Organisational Too many critical dependencies Cognitive Time Not yet invented Lack of EBM Patients Commercial Political Cost Expectations
Human Factors: Likely Hazard Warning The usual No buy-in, time, skills, training, leader, benefit Sabotage, fizzling out ICP from on high (ie written by consultant) Attempt perfection at first draft rather than iterate Or, alternatively, less enthusiasm for necessary iteration Biting off more than can chew Medicine is complex: eat it a bit at a time Interdisciplinary friction Terminology, working practices, culture etc.
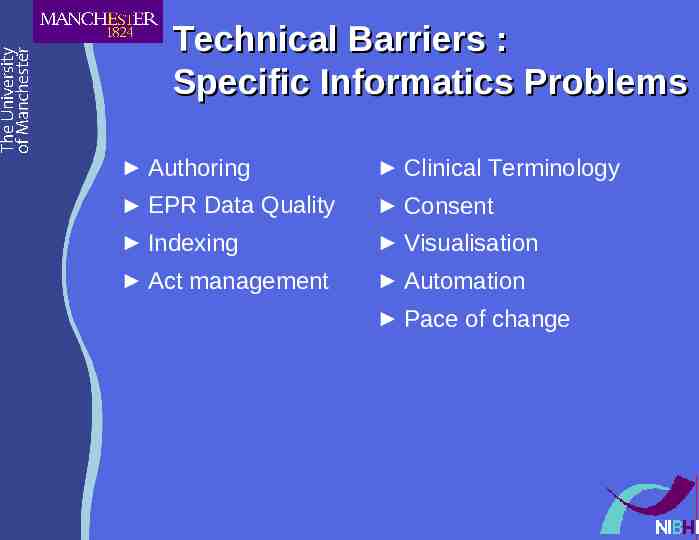
Technical Barriers : Specific Informatics Problems Authoring Clinical Terminology EPR Data Quality Consent Indexing Visualisation Act management Automation Pace of change
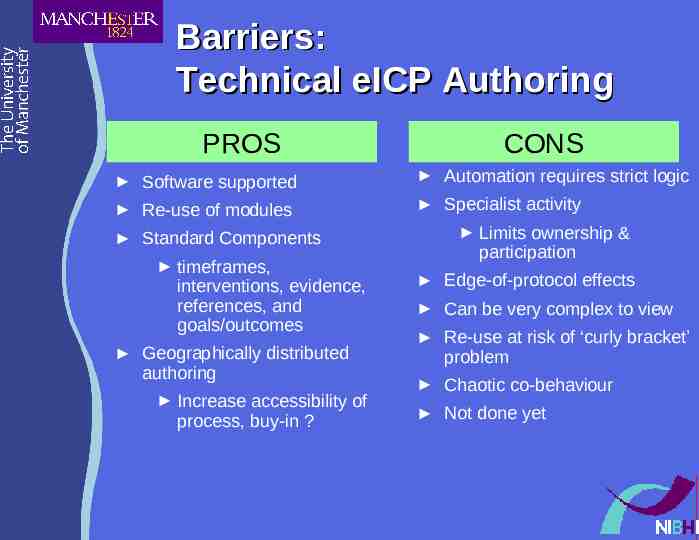
Barriers: Technical eICP Authoring PROS CONS Software supported Automation requires strict logic Re-use of modules Specialist activity Standard Components timeframes, interventions, evidence, references, and goals/outcomes Geographically distributed authoring Increase accessibility of process, buy-in ? Limits ownership & participation Edge-of-protocol effects Can be very complex to view Re-use at risk of ‘curly bracket’ problem Chaotic co-behaviour Not done yet
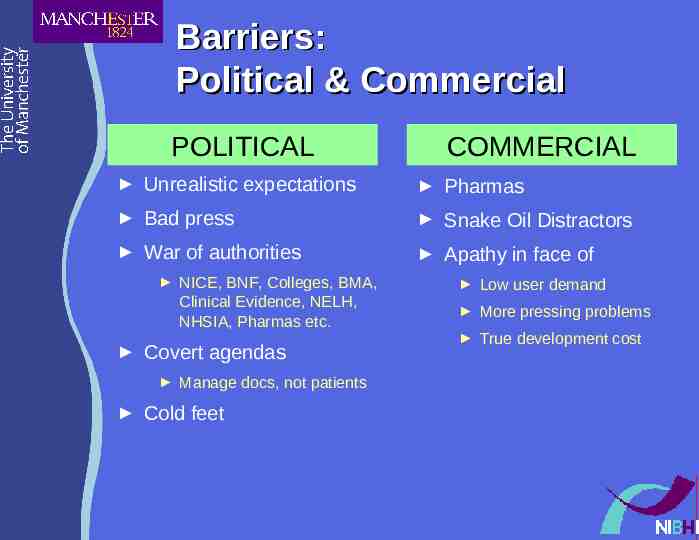
Barriers: Political & Commercial POLITICAL COMMERCIAL Unrealistic expectations Pharmas Bad press Snake Oil Distractors War of authorities Apathy in face of NICE, BNF, Colleges, BMA, Clinical Evidence, NELH, NHSIA, Pharmas etc. Covert agendas Manage docs, not patients Cold feet Low user demand More pressing problems True development cost