HMO 2 interview questions practice Dr Carol Chong Supervisor of
36 Slides299.00 KB

HMO 2 interview questions practice Dr Carol Chong Supervisor of Intern Training June 2019
Practice interview questions Why do you want to work here? Why have you applied for this position?
Why do you want to work here? What skills will you bring to the hospital, does it fit with your career goals? Demonstrate that you know about the hospital eg. training program, research Also, good to know about the community that you will be helping Enthusiasm and positivity helps!
Q What skills can you offer?
What skills can you offer Talk about your strengths - general skills eg. teamwork, leadership, communication - medical – your strengths eg. what you’ve learnt from past rotations eg. responsibility - other skills specific to you
Q What career path have you chosen and why?
What career path have you chosen and why? Doesn’t matter what path you have chosen as long as you have a reason (eg. previous positive experience) Enthusiasm helps yet again If you haven’t chosen a path yet, that’s fine but be careful saying this if you are going for a particular stream (eg. okay to say this for the general stream as 1st preference). Med stream – prefer BPTs. Surg – people keen on SET program.
Q What are your strengths and weaknesses?
Strengths and weaknesses Strengths – General and medical skills. Eg. communication, responsible, enjoy working in a team, excellent clinical skills, feedback from my consultants is that . (something along the lines of I’m just excellent!) Weaknesses – talk about how you aim to improve. Eg. time management – learnt to be more efficient this year as an intern. Breaking bad news – started to practice, now reg is supervising you. Staying back late – re: time management
Often 1 or 2 clinical or behavioural questions or could be mixed together
Example Interview questions What makes a good team and give us an example where teamwork enhanced patient care.
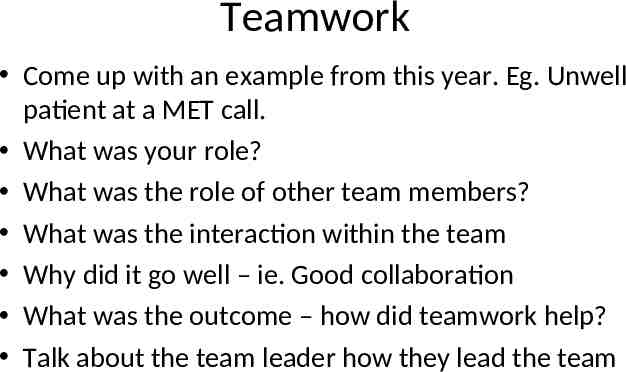
Teamwork Come up with an example from this year. Eg. Unwell patient at a MET call. What was your role? What was the role of other team members? What was the interaction within the team Why did it go well – ie. Good collaboration What was the outcome – how did teamwork help? Talk about the team leader how they lead the team
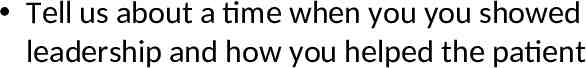
Tell us about a time when you you showed leadership and how you helped the patient
Leadership Come up with an example from this year where you had to be leader Eg. On the wards nurses ask you to do something. Was there any conflict – talk about how things were smoothed over with good leadership. Talk about walking in a team and leading others. Who did you lead? Talk about the other members
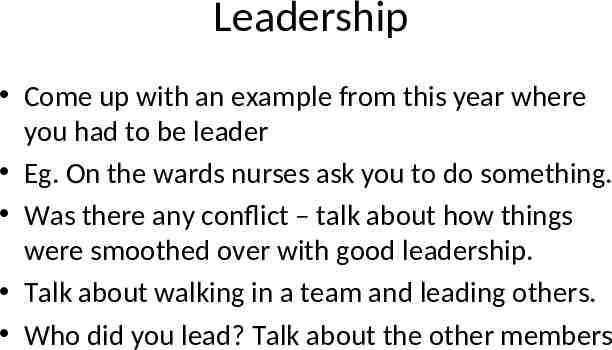
Potential interview questions 3. Tell us when you made a mistake that affected patient care ((4. Clinical scenario -post hartmanns - low urine output – management)) Patient difficult to rouse/ unconsicous patient ((Family doesn’t want patient to know about cancer))
Tell us when you made a mistake that affected patient care
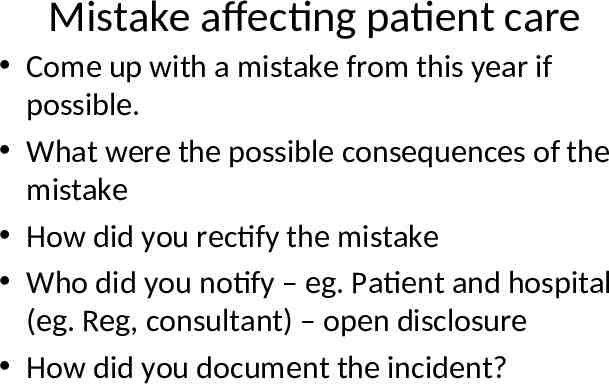
Mistake affecting patient care Come up with a mistake from this year if possible. What were the possible consequences of the mistake How did you rectify the mistake Who did you notify – eg. Patient and hospital (eg. Reg, consultant) – open disclosure How did you document the incident?
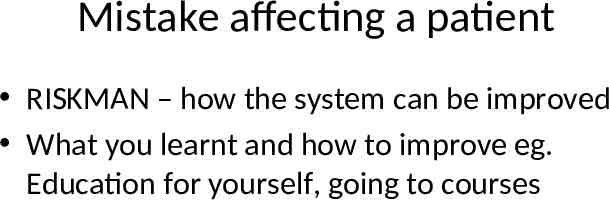
Mistake affecting a patient RISKMAN – how the system can be improved What you learnt and how to improve eg. Education for yourself, going to courses
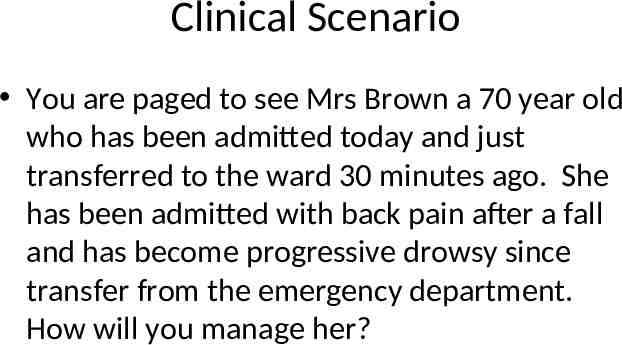
Clinical Scenario You are paged to see Mrs Brown a 70 year old who has been admitted today and just transferred to the ward 30 minutes ago. She has been admitted with back pain after a fall and has become progressive drowsy since transfer from the emergency department. How will you manage her?
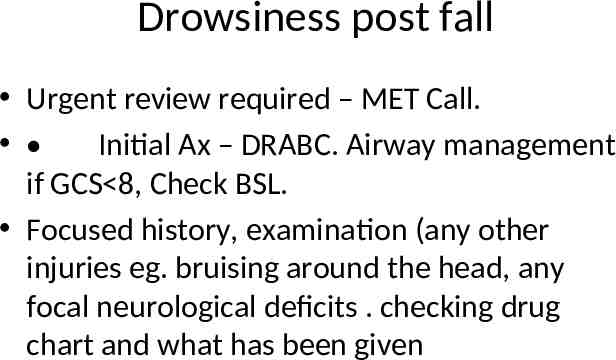
Drowsiness post fall Urgent review required – MET Call. Initial Ax – DRABC. Airway management if GCS 8, Check BSL. Focused history, examination (any other injuries eg. bruising around the head, any focal neurological deficits . checking drug chart and what has been given
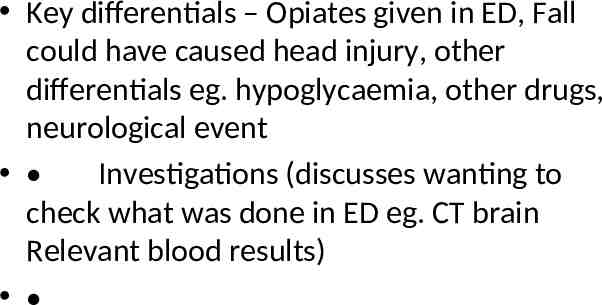
Key differentials – Opiates given in ED, Fall could have caused head injury, other differentials eg. hypoglycaemia, other drugs, neurological event Investigations (discusses wanting to check what was done in ED eg. CT brain Relevant blood results)
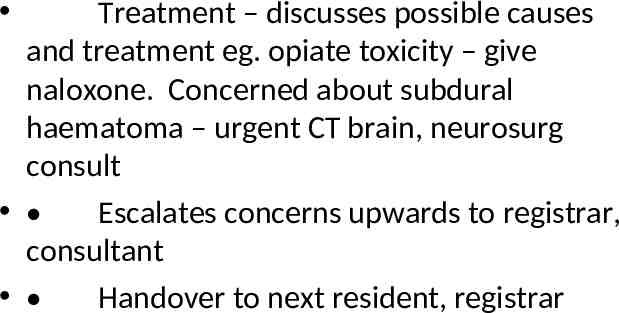
Treatment – discusses possible causes and treatment eg. opiate toxicity – give naloxone. Concerned about subdural haematoma – urgent CT brain, neurosurg consult Escalates concerns upwards to registrar, consultant Handover to next resident, registrar
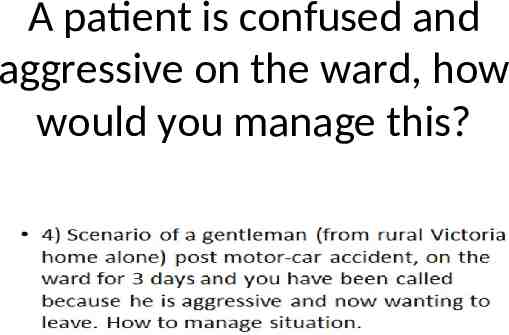
A patient is confused and aggressive on the ward, how would you manage this?
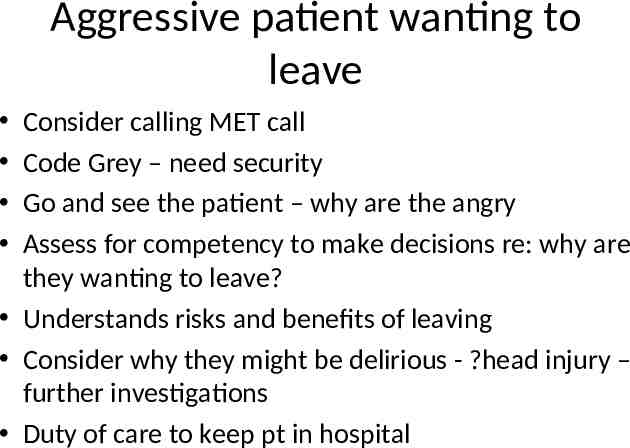
Aggressive patient wanting to leave Consider calling MET call Code Grey – need security Go and see the patient – why are the angry Assess for competency to make decisions re: why are they wanting to leave? Understands risks and benefits of leaving Consider why they might be delirious - ?head injury – further investigations Duty of care to keep pt in hospital
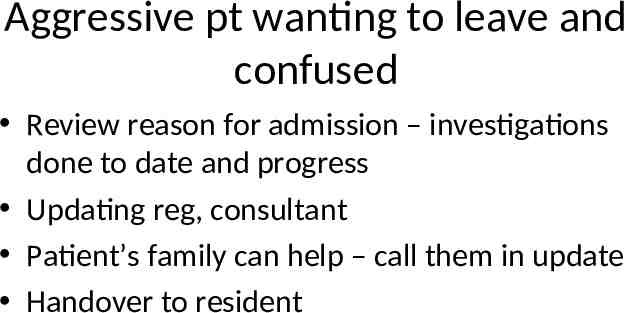
Aggressive pt wanting to leave and confused Review reason for admission – investigations done to date and progress Updating reg, consultant Patient’s family can help – call them in update Handover to resident
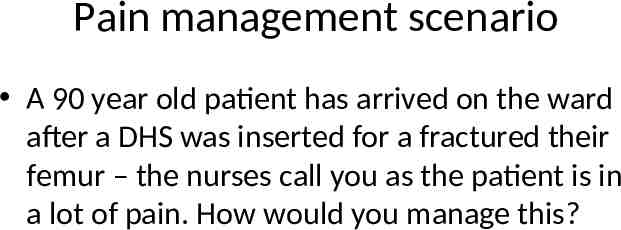
Pain management scenario A 90 year old patient has arrived on the ward after a DHS was inserted for a fractured their femur – the nurses call you as the patient is in a lot of pain. How would you manage this?
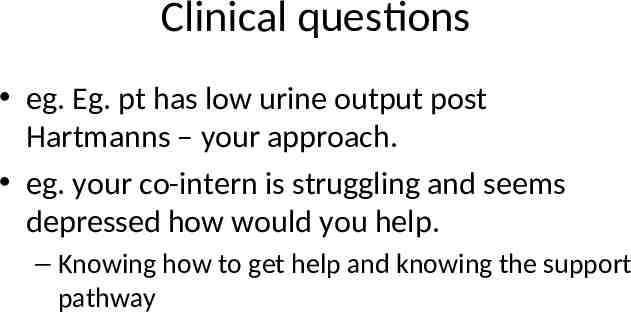
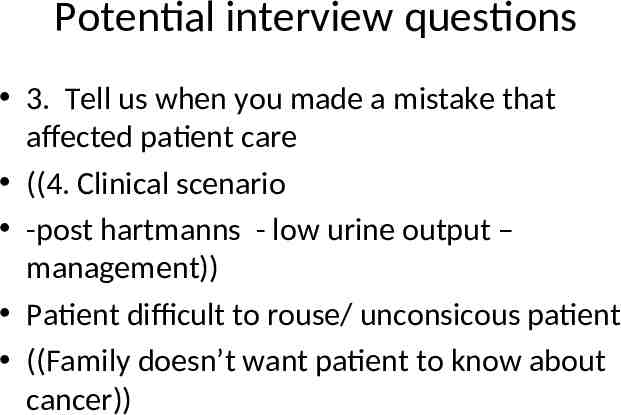
Clinical questions eg. Eg. pt has low urine output post Hartmanns – your approach. eg. your co-intern is struggling and seems depressed how would you help. – Knowing how to get help and knowing the support pathway
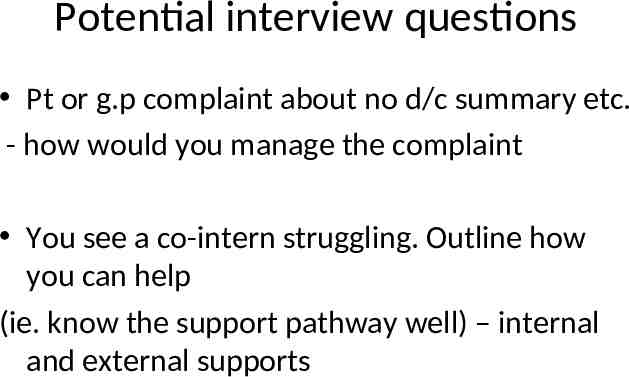
Potential interview questions Pt or g.p complaint about no d/c summary etc. - how would you manage the complaint You see a co-intern struggling. Outline how you can help (ie. know the support pathway well) – internal and external supports
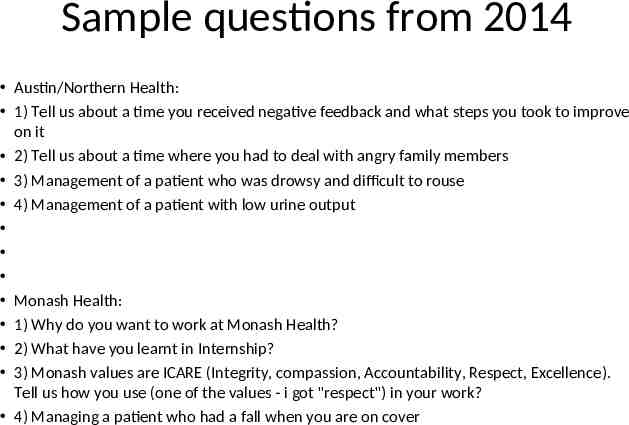
Sample questions from 2014 Austin/Northern Health: 1) Tell us about a time you received negative feedback and what steps you took to improve on it 2) Tell us about a time where you had to deal with angry family members 3) Management of a patient who was drowsy and difficult to rouse 4) Management of a patient with low urine output Monash Health: 1) Why do you want to work at Monash Health? 2) What have you learnt in Internship? 3) Monash values are ICARE (Integrity, compassion, Accountability, Respect, Excellence). Tell us how you use (one of the values - i got "respect") in your work? 4) Managing a patient who had a fall when you are on cover
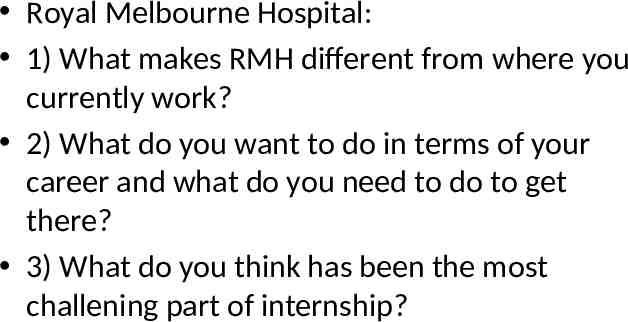
Royal Melbourne Hospital: 1) What makes RMH different from where you currently work? 2) What do you want to do in terms of your career and what do you need to do to get there? 3) What do you think has been the most challening part of internship?
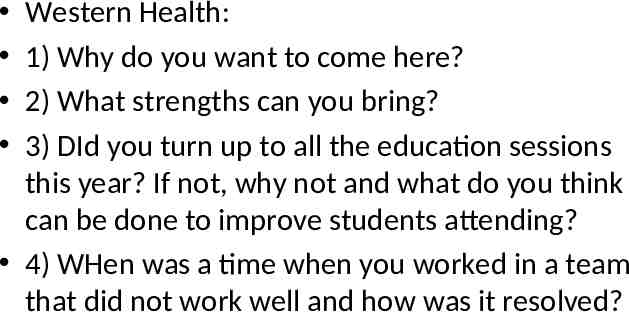
Western Health: 1) Why do you want to come here? 2) What strengths can you bring? 3) DId you turn up to all the education sessions this year? If not, why not and what do you think can be done to improve students attending? 4) WHen was a time when you worked in a team that did not work well and how was it resolved?
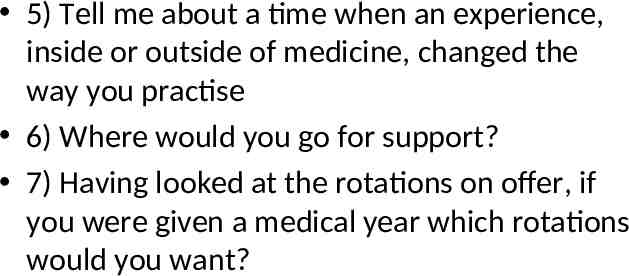
5) Tell me about a time when an experience, inside or outside of medicine, changed the way you practise 6) Where would you go for support? 7) Having looked at the rotations on offer, if you were given a medical year which rotations would you want?
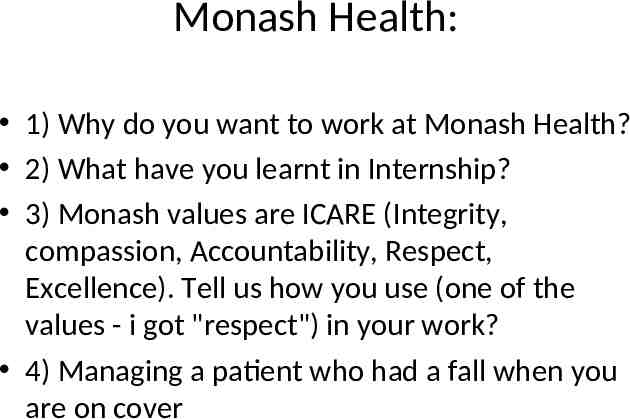
Monash Health: 1) Why do you want to work at Monash Health? 2) What have you learnt in Internship? 3) Monash values are ICARE (Integrity, compassion, Accountability, Respect, Excellence). Tell us how you use (one of the values - i got "respect") in your work? 4) Managing a patient who had a fall when you are on cover
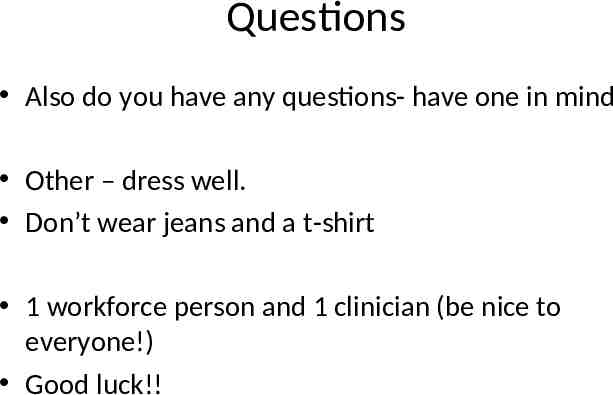
Questions Also do you have any questions- have one in mind Other – dress well. Don’t wear jeans and a t-shirt 1 workforce person and 1 clinician (be nice to everyone!) Good luck!!
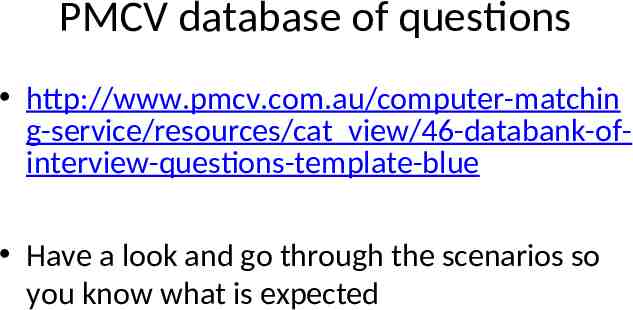
PMCV database of questions http://www.pmcv.com.au/computer-matchin g-service/resources/cat view/46-databank-ofinterview-questions-template-blue Have a look and go through the scenarios so you know what is expected
Good luck! Be prepared. Work on your CV and cover letters. Know the values of each hospital and how you can help them and the community. Ask your mentor to check over your CV. Ask 2 consultants to be your referees. Some jobs want 3 referees (eg. Alfred medical) Aim to get an interview. Practice interview questions – (June/July/August during education)