HCRA HOSPITAL CONFERENCE November 15, 2011 – updated April 24, 2013
42 Slides3.13 MB

HCRA HOSPITAL CONFERENCE November 15, 2011 – updated April 24, 2013 Your Logo
INTRODUCTIONS Phyllis Stanton, Principal Health Care Fiscal Analyst, DOH John Kazukenus, Manager, KPMG Patrick Bryant, Manager, KPMG
HCRA Refresher SEMINAR OVERVIEW 1 2 Public Health Law on Patient Services Revenue Third Party Payors Requiring an Election Decision 3 Revenue Hospitals are Responsible For 4 HCRA Topics 5 Delinquency Process 6 Compliance Audits 7 Contact Information
HEALTH CARE REFORM ACT PUBLIC HEALTH LAW §2807-j The HCRA law requires Article 28 general hospitals, D&TCs providing ambulatory surgical services, and comprehensive D&TCs to pay a surcharge to the Public Goods Pool on certain net patient services revenue.
Patient Services Revenue : Defined as all moneys received for, or on account of, all patient services related to a preadmission, inpatient, outpatient, or postdischarge visit, including all items or services as are necessary for such care, except where excluded in §2807-j .
Examples of Types of Third Party Payors* That Would Be Considered Non-Electing if No Election Submitted Any not-for-profit insurer, licensed in NYS or elsewhere, (if licensed in NYS they would be termed Article 43 Corporations); Commercial insurers, licensed in NYS, or elsewhere; This can include HMOs HMOs organized under Article 44 of the NYS Public Health Law Self funded plans domiciled in NYS or elsewhere; This includes welfare plans, certain trusts Other Insurer types, including HMOs, licensed out of state; This includes foreign insurers State and local Government payors other than NYS; Example: Other state’s govermental programs except Medicaid *This is a list of the most common types of payors that providers receive patient revenue from and is not meant to be an all inclusive list.
PATIENT SERVICES REVENUE FOR WHICH THE HOSPITAL IS RESPONSIBLE TO PAY A SURCHARGE ON Revenue received from the patient for: 1. 2. 3. Coinsurance Self pay or uninsured Copays and deductibles for which the provider has not received written release from the payor stating they are paying the associated surcharge Revenue received from non-electing payors –third party payors who have an election decision to make and have not made an election. A list of all electing payors (current or past) can be found on www.nyhealth.gov/nysdoh/hcra/hcrahome.htm or www.hcrapools.org entitled “Elector List.” Revenue received from “unspecified” payors – payors who are not obligated to make an election decision because they are not a third party “every day payor” or have been deemed by the Department to be unspecified. Example 1: Foreign countries that have nationalized healthcare making payment directly for claims. Example 2: employer paying a workers compensation claim, rather than submitting the claim to their workers compensation carrier. Revenue received from NYS agencies/programs authorized to pay NYS Medicaid inpatient rates, NYS counties for county inmates, or NYC Corrections, that are not on the Elector List (at the current NYS Medicaid rate of 7.04%). Details discussed on the next screen.
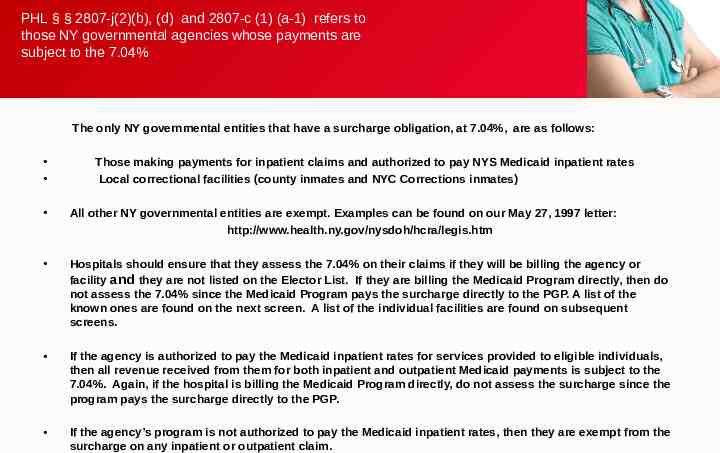
PHL § § 2807-j(2)(b), (d) and 2807-c (1) (a-1) refers to those NY governmental agencies whose payments are subject to the 7.04% The only NY governmental entities that have a surcharge obligation, at 7.04%, are as follows: Those making payments for inpatient claims and authorized to pay NYS Medicaid inpatient rates Local correctional facilities (county inmates and NYC Corrections inmates) All other NY governmental entities are exempt. Examples can be found on our May 27, 1997 letter: http://www.health.ny.gov/nysdoh/hcra/legis.htm Hospitals should ensure that they assess the 7.04% on their claims if they will be billing the agency or facility and they are not listed on the Elector List. If they are billing the Medicaid Program directly, then do not assess the 7.04% since the Medicaid Program pays the surcharge directly to the PGP. A list of the known ones are found on the next screen. A list of the individual facilities are found on subsequent screens. If the agency is authorized to pay the Medicaid inpatient rates for services provided to eligible individuals, then all revenue received from them for both inpatient and outpatient Medicaid payments is subject to the 7.04%. Again, if the hospital is billing the Medicaid Program directly, do not assess the surcharge since the program pays the surcharge directly to the PGP. If the agency’s program is not authorized to pay the Medicaid inpatient rates, then they are exempt from the surcharge on any inpatient or outpatient claim.
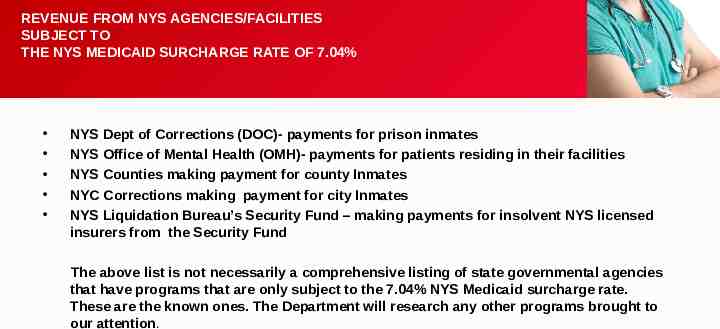
REVENUE FROM NYS AGENCIES/FACILITIES SUBJECT TO THE NYS MEDICAID SURCHARGE RATE OF 7.04% NYS Dept of Corrections (DOC)- payments for prison inmates NYS Office of Mental Health (OMH)- payments for patients residing in their facilities NYS Counties making payment for county Inmates NYC Corrections making payment for city Inmates NYS Liquidation Bureau’s Security Fund – making payments for insolvent NYS licensed insurers from the Security Fund The above list is not necessarily a comprehensive listing of state governmental agencies that have programs that are only subject to the 7.04% NYS Medicaid surcharge rate. These are the known ones. The Department will research any other programs brought to our attention.
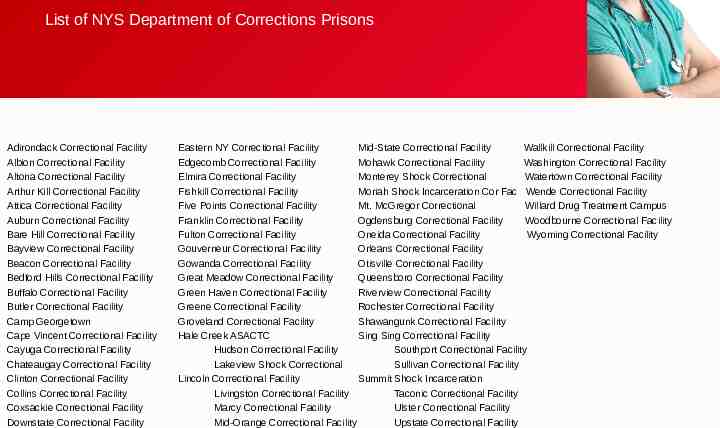
List of NYS Department of Corrections Prisons Adirondack Correctional Facility Albion Correctional Facility Altona Correctional Facility Arthur Kill Correctional Facility Attica Correctional Facility Auburn Correctional Facility Bare Hill Correctional Facility Bayview Correctional Facility Beacon Correctional Facility Bedford Hills Correctional Facility Buffalo Correctional Facility Butler Correctional Facility Camp Georgetown Cape Vincent Correctional Facility Cayuga Correctional Facility Chateaugay Correctional Facility Clinton Correctional Facility Collins Correctional Facility Coxsackie Correctional Facility Downstate Correctional Facility Eastern NY Correctional Facility Mid-State Correctional Facility Wallkill Correctional Facility Edgecomb Correctional Facility Mohawk Correctional Facility Washington Correctional Facility Elmira Correctional Facility Monterey Shock Correctional Watertown Correctional Facility Fishkill Correctional Facility Moriah Shock Incarceration Cor Fac Wende Correctional Facility Five Points Correctional Facility Mt. McGregor Correctional Willard Drug Treatment Campus Franklin Correctional Facility Ogdensburg Correctional Facility Woodbourne Correctional Facility Fulton Correctional Facility Oneida Correctional Facility Wyoming Correctional Facility Gouverneur Correctional Facility Orleans Correctional Facility Gowanda Correctional Facility Otisville Correctional Facility Great Meadow Correctional Facility Queensboro Correctional Facility Green Haven Correctional Facility Riverview Correctional Facility Greene Correctional Facility Rochester Correctional Facility Groveland Correctional Facility Shawangunk Correctional Facility Hale Creek ASACTC Sing Sing Correctional Facility Hudson Correctional Facility Southport Correctional Facility Lakeview Shock Correctional Sullivan Correctional Facility Lincoln Correctional Facility Summit Shock Incarceration Livingston Correctional Facility Taconic Correctional Facility Marcy Correctional Facility Ulster Correctional Facility Mid-Orange Correctional Facility Upstate Correctional Facility
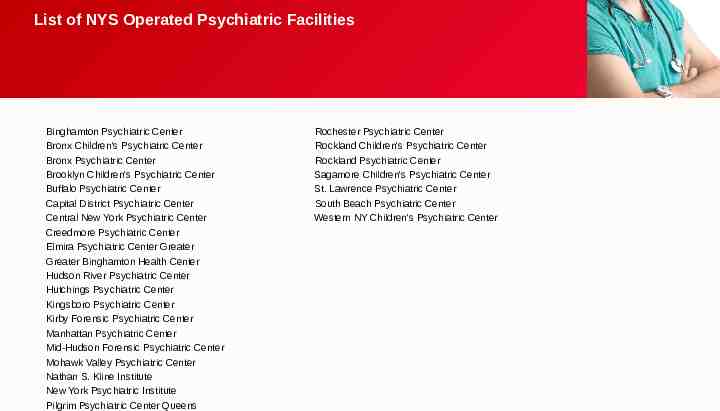
List of NYS Operated Psychiatric Facilities Binghamton Psychiatric Center Bronx Children's Psychiatric Center Bronx Psychiatric Center Brooklyn Children's Psychiatric Center Buffalo Psychiatric Center Capital District Psychiatric Center Central New York Psychiatric Center Creedmore Psychiatric Center Elmira Psychiatric Center Greater Greater Binghamton Health Center Hudson River Psychiatric Center Hutchings Psychiatric Center Kingsboro Psychiatric Center Kirby Forensic Psychiatric Center Manhattan Psychiatric Center Mid-Hudson Forensic Psychiatric Center Mohawk Valley Psychiatric Center Nathan S. Kline Institute New York Psychiatric Institute Pilgrim Psychiatric Center Queens Rochester Psychiatric Center Rockland Children's Psychiatric Center Rockland Psychiatric Center Sagamore Children's Psychiatric Center St. Lawrence Psychiatric Center South Beach Psychiatric Center Western NY Children's Psychiatric Center
Non-electors Subject to the GME: 1 Corporations Organized and Operating in Accordance with Article 43 of the NYS Insurance Law Not for Profit Insurers and HMOs 2 Corporations Operating in Accordance with Article 44 of the NYS PHL HMOs in NYS 3 Self Funded Plans Providing Inpatient Coverage – regardless of insurance type except when providing coverage described in the next screen Regardless of Domicile 4 Insurers and HMOS Authorized to Write Accident and Health Policies (regardless of which state/country they are licensed)
Non-electors NOT Subject to the GME: NYS governmental agencies Workers Compensation carriers providing coverage under NYS Law Auto no-fault carriers providing coverage under NYS Law Volunteer Firefighters providers of coverage under NYS Law Volunteer Ambulance Workers providers of coverage under NYS Law Indemnity Policies that do not provide inpatient coverage on an expense incurred basis, but rather pay a fixed dollar per day for each as an inpatient. (Most of these policies pay the member rather than the hospital, and if patient has no other insurance, patient is to be treated as a self-pay with no GME.
Fixed Dollar Patient Portions 1 Hospital’s Responsibility to Determine if Obligated to Surcharge on Fixed Dollar Patient Portion In fixed dollar patient portions such as fixed dollar co-pays or deductibles, electing payors have a choice between two options on how to pay the associated surcharge Hospitals are obligated to determine which option they’ve chosen, otherwise are obligated themselves 2 3 The Electing Payor’s Choices of Surcharge Payment Options: 1. Payor pays claim by utilizing the second billing example found on the DOH website. Hospital pays the surcharge out of fixed dollar amount and gets reimbursed by payor 2. Payor pays the associated surcharge on the fixed dollar amount directly to the Public Goods Pool via payor report
Fixed Dollar Patient Portions (continued) 3 Proper Reporting of Copays: 1. If payor chooses #1 above, hospitals will report the fixed dollar payment received from the insured patient on Line #10 of their PGP report, entitled: “Self-Pay Uninsured ” Hospital pays the surcharge out of the fixed dollar amount and gets reimbursed by payor 2. If payor chooses #2 above, and notifies hospital of such choice, the hospital will report the fixed dollar payment received from the patient on the following lines: On Hospital Inpatient portion of the PGP report: Line 17 On Hospital Outpatient portion of the PGP report: Line 19 3. In the absence of the electing payor notifying the hospital that they have chosen option #2 above, the hospital’s “default” is to report the fixed dollar payment on line 10 of the PGP 4. A non-electing payor, paying for covered services, must utilize Choice #1 (under Box 2) above, and the hospital must report revenue on line 12, 12a or 12b
Revenue Received for Physician Billings Effective with dates of service 4/1/11, Public Health Law §2807-j (3)(a)(v) now exempts surcharges on revenue received for all discrete physician billings (M.D.s or D.Os) Physician services MUST be billed on a separate claim form, separate from services provided (HCFA 1500 or 837P) This change in law includes discretely billed employed physician services
Foreign Payors and Patients 1 Foreign Insurance Companies and Medical Assistance Companies Foreign insurance companies are insurers licensed in other countries Medical assistance companies act as the conduit for claim payments between the foreign insurance company and providers in U.S.; administer travel policies for expatriates Must make an election like any payor in order to pay current elector rate to the PGP If no election is made, hospital must pay the nonelector rate to the PGP currently at 37.90% and if an inpatient claim and an accident and health policy, or a self funded plan (as known in U.S.), the regional GME percentage 2 Foreign Countries with Nationalized Health Plans or Paid Directly by Foreign Governments Deemed Unspecified payor; pay directly to hospital when billed, at self pay rate currently at 9.63% A List of those countries with known nationalized health plans can be found on our DOH Web site under “Elector List”

Foreign Payors and Patients (continued) 3 Foreign Diplomatic Agents Exempt from all surcharges if protected under their diplomatic mission Those protected by the diplomatic mission carry exemption paperwork
Surchargeability of Personal Items Exemption of Personal Items Revenue from billed patient personal items, not related to the medical service such as TVs, telephones, and private rooms are not subject to the HCRA surcharge since such items are not related to the medical service provided
Medicare 1 Traditional Medicare Exemptions: Revenue received for Medicare covered services is exempt from surcharge; includes revenue received from: 2 the Medicare program an insurer contracted to administer on behalf of the Medicare program a supplemental plan such as a Medigap policy, or, the beneficiary themselves Medigap/Supplemental Policies Pay for certain out-of-pocket expenses that Medicare covers but does not pay in full Also can cover certain services that are not payable by Medicare due to: Non-covered services Exhaustion of benefits Surcharges apply to services not covered, at rates based on election status of payor, but no GME Per Unit of Payment Surcharge (if a non-elector)
Medicare (continued) 3 Medicare Advantage Part C Medicare Advantage Part C plans supply a person with all of their Part A and Part B benefits, plus, depending on the plan chosen, may cover services that traditional Medicare will not, like dental, vision, and unlimited inpatient days ANY service for which Medicare Advantage pays for, is exempt from the surcharge
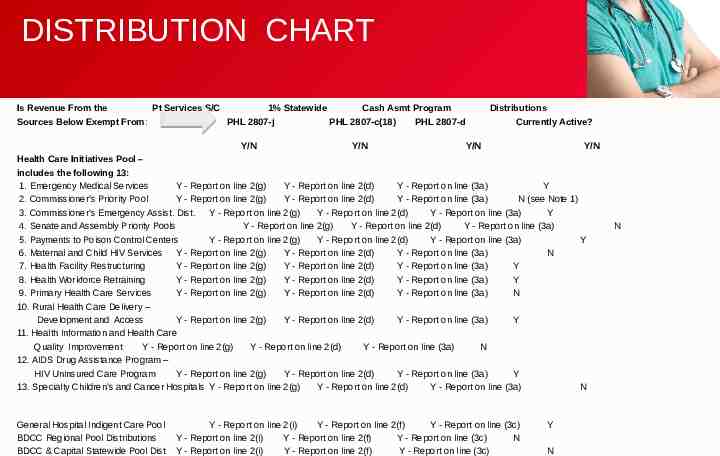
DISTRIBUTION CHART Is Revenue From the Pt Services S/C 1% Statewide Cash Asmt Program Sources Below Exempt From: PHL 2807-j PHL 2807-c(18) PHL 2807-d Distributions Currently Active? Y/N Y/N Y/N Y/N Health Care Initiatives Pool – includes the following 13: 1. Emergency Medical Services Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) Y 2. Commissioner’s Priority Pool Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) N (see Note 1) 3. Commissioner’s Emergency Assist. Dist. Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) Y 4. Senate and Assembly Priority Pools Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) 5. Payments to Poison Control Centers Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) Y 6. Maternal and Child HIV Services Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) N 7. Health Facility Restructuring Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) Y 8. Health Workforce Retraining Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) Y 9. Primary Health Care Services Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) N 10. Rural Health Care Delivery – Development and Access Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) Y 11. Health Information and Health Care Quality Improvement Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) N 12. AIDS Drug Assistance Program – HIV Uninsured Care Program Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) Y 13. Specialty Children’s and Cancer Hospitals Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3a) N General Hospital Indigent Care Pool BDCC Regional Pool Distributions BDCC & Capital Statewide Pool Dist Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) N Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) Y N N
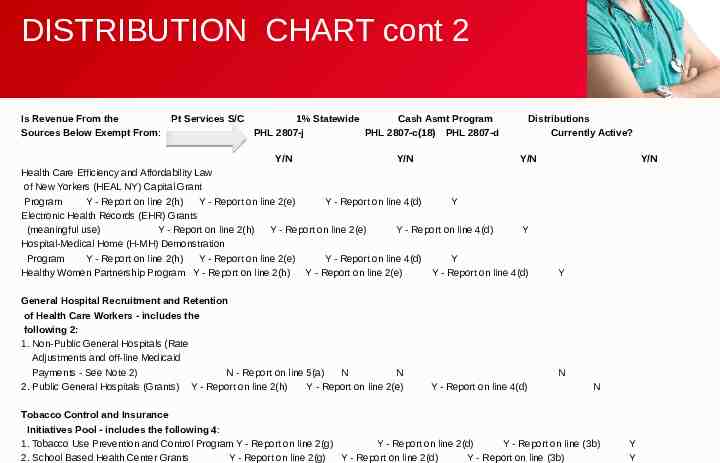
DISTRIBUTION CHART cont 2 Is Revenue From the Sources Below Exempt From: Pt Services S/C 1% Statewide Cash Asmt Program PHL 2807-j PHL 2807-c(18) PHL 2807-d Y/N Y/N Distributions Currently Active? Y/N Health Care Efficiency and Affordability Law of New Yorkers (HEAL NY) Capital Grant Program Y - Report on line 2(h) Y - Report on line 2(e) Y - Report on line 4(d) Y Electronic Health Records (EHR) Grants (meaningful use) Y - Report on line 2(h) Y - Report on line 2(e) Y - Report on line 4(d) Y Hospital-Medical Home (H-MH) Demonstration Program Y - Report on line 2(h) Y - Report on line 2(e) Y - Report on line 4(d) Y Healthy Women Partnership Program Y - Report on line 2(h) Y - Report on line 2(e) Y - Report on line 4(d) General Hospital Recruitment and Retention of Health Care Workers - includes the following 2: 1. Non-Public General Hospitals (Rate Adjustments and off-line Medicaid Payments - See Note 2) N - Report on line 5(a) N N 2. Public General Hospitals (Grants) Y - Report on line 2(h) Y - Report on line 2(e) Y/N Y N Y - Report on line 4(d) N Tobacco Control and Insurance Initiatives Pool - includes the following 4: 1. Tobacco Use Prevention and Control Program Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3b) 2. School Based Health Center Grants Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3b) Y Y
DISTRIBUTION CHART cont 3 Is Revenue From the Sources Below Exempt From Pt Services S/C PHL 2807-j 1% Statewide PHL 2807-c(18) Y/N Cash Asmt Program PHL 2807-d Y/N Distributions Currently Active? Y/N Y/N 3. Workforce Retention – Public General Hospital Grants 4. Infertility Services Program Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3b) Y - Report on line 2(g) Y - Report on line 2(d) Y - Report on line (3b) N NYS Community Health Care Conversion Demonstration Project Grant Funds Y - Report on line 2(g) N Y - Report on line 2(d) Y - Report on line (3b) High Need Indigent Care Adjustment Pool includes the following 4: 1. High Need Indigent Care Adjustment Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) 2. DSH Share Rural Hospital Adjustment Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) 3. Non-DSH Indigent Care Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) 4. Non-DSH Share Rural Hospital Adjustment Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) Professional Education Pool – includes the following 4: 1.Graduate Medical Education Distributions 2. Incentive Pool Distributions - Minority 3. Incentive Pool Distributions - Non-Minority 4. Empire Clinical Research Investigator Program – (ECRIP) Distributions Y - Report on line 2(i) N Y - Report on line 2(i) Y - Report on line 2(i) N Y - Report on line 2(i) N N N Y Y Y Y Y N N N N N N Y
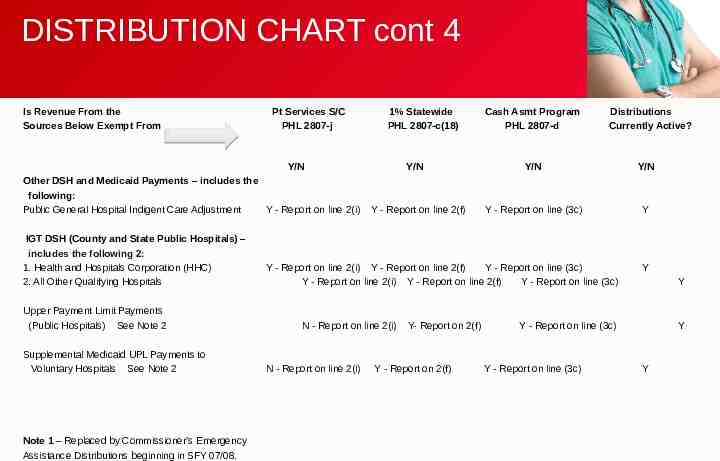
DISTRIBUTION CHART cont 4 Is Revenue From the Sources Below Exempt From Pt Services S/C PHL 2807-j 1% Statewide PHL 2807-c(18) Y/N Other DSH and Medicaid Payments – includes the following: Public General Hospital Indigent Care Adjustment Y - Report on line 2(i) IGT DSH (County and State Public Hospitals) – includes the following 2: 1. Health and Hospitals Corporation (HHC) 2. All Other Qualifying Hospitals Upper Payment Limit Payments (Public Hospitals) See Note 2 Supplemental Medicaid UPL Payments to Voluntary Hospitals See Note 2 Note 1 – Replaced by Commissioner’s Emergency Assistance Distributions beginning in SFY 07/08. Y/N Y - Report on line 2(f) Cash Asmt Program PHL 2807-d Distributions Currently Active? Y/N Y/N Y - Report on line (3c) Y Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) Y - Report on line 2(i) Y - Report on line 2(f) Y - Report on line (3c) N - Report on line 2(i) N - Report on line 2(i) Y- Report on 2(f) Y - Report on 2(f) Y Y Y - Report on line (3c) Y - Report on line (3c) Y Y
DISTRIBUTION CHART cont 5 Note 2 – Upper Payment Limit Payments to Public and Voluntary Hospitals, Supplemental Medicaid UPL Payments to Voluntary Hospitals, NonPublic General Hospitals rate adjustments and off-line Medicaid payments for Hospital Recruitment and Retention of Health Care Workers are paid directly to hospitals by DOH’s MMIS. MMIS pays the related surcharge on these hospital adjustments directly to the HCRA pool. Consequently, these revenues are not exempt from the surcharge. However, since this revenue is exempt from the 1% Statewide (SW) Assessment, in order for hospitals to take this deduction on line 2(f) of the 1% SW report, hospitals should report this revenue on line 2(i) of the Public Goods Pool (PGP) report (not line 5(a) where other NYS Medicaid Program dollars are reported. This avoids double payment of the surcharge and also assumes the revenue is included on line 1 of the PGP report. Special Note: Each of the payments listed in this chart must be reported on line 1 of the Public Goods Pool report.
Amnesty Provision An amendment to the Health Care Reform Act was enacted April 15, 2011, that waives statutorily required interest and penalty if delinquent obligations due, (based on estimated or actual amounts), under Public Health Law (PHL) 2807-j, 2807-s and 2807-t, for reporting periods prior to January 1, 2011, are filed and paid in full between the dates of April 1, 2011, and December 31, 2011. Who Should Take Advantage of this Opportunity: Providers who have not filed a monthly report to the Public Goods Pool for report periods prior to January 1, 2011. (Prior to collection action initiated by DOH). Providers who have not fully paid owed surcharge obligations on patient services revenue received prior to January 1, 2011. Providers who discover an additional amount due to the PGP on patient services revenue received prior to January 1, 2011. Obligations not covered by the Amnesty Provision: Any interest or penalty amount that has been paid to, or collected previously by, DOH. Any surcharge or assessment payments made in response to a final audit finding issued by DOH or its designee. Any delinquent amount (whether estimated or actual) that has been referred to NYS Medicaid for recoupment. Any delinquent amount (whether estimated or actual) that has been referred to the NYS Attorney General’s Office for collection.
DELINQUENCY PROCESS Delinquency Notice Estimated Billing Process Action Taken for Non-Compliance
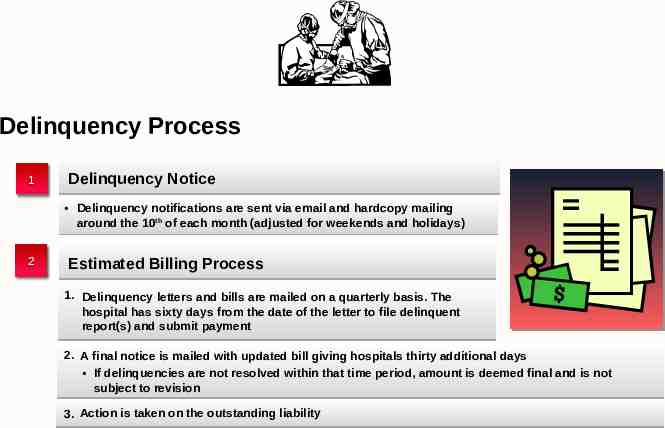
Delinquency Process 1 Delinquency Notice Delinquency notifications are sent via email and hardcopy mailing around the 10th of each month (adjusted for weekends and holidays) 2 Estimated Billing Process 1. Delinquency letters and bills are mailed on a quarterly basis. The hospital has sixty days from the date of the letter to file delinquent report(s) and submit payment 2. A final notice is mailed with updated bill giving hospitals thirty additional days If delinquencies are not resolved within that time period, amount is deemed final and is not subject to revision 3. Action is taken on the outstanding liability
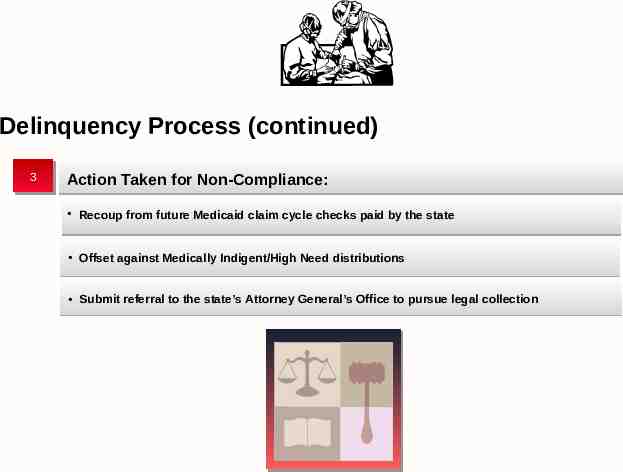
Delinquency Process (continued) 3 Action Taken for Non-Compliance: Recoup from future Medicaid claim cycle checks paid by the state Offset against Medically Indigent/High Need distributions Submit referral to the state’s Attorney General’s Office to pursue legal collection

COMPLIANCE AUDITS Key Phases/Milestones Common Challenges and Better Practices
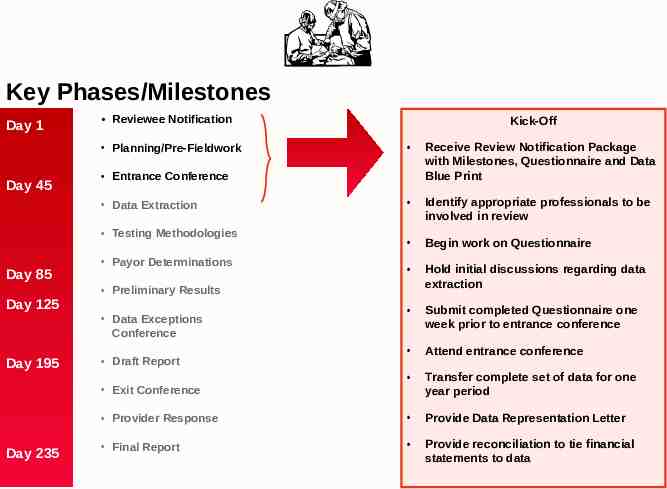
Key Phases/Milestones Day 1 Reviewee Notification Receive Review Notification Package with Milestones, Questionnaire and Data Blue Print Identify appropriate professionals to be involved in review Begin work on Questionnaire Hold initial discussions regarding data extraction Submit completed Questionnaire one week prior to entrance conference Attend entrance conference Transfer complete set of data for one year period Provider Response Provide Data Representation Letter Final Report Provide reconciliation to tie financial statements to data Planning/Pre-Fieldwork Day 45 Entrance Conference Data Extraction Testing Methodologies Day 85 Day 125 Day 195 Payor Determinations Preliminary Results Data Exceptions Conference Draft Report Exit Conference Day 235 Kick-Off
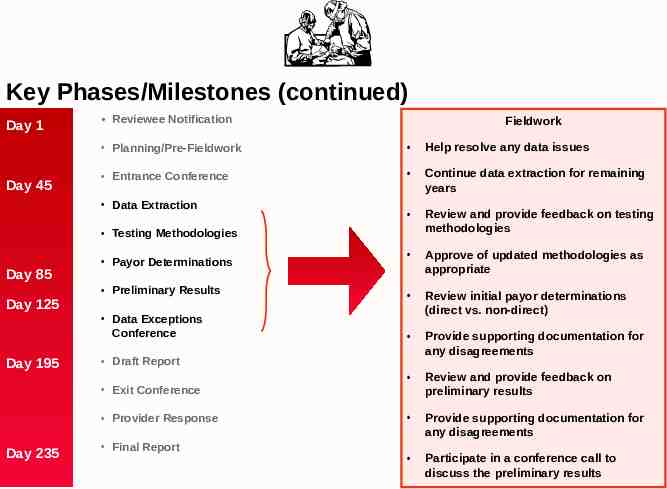
Key Phases/Milestones (continued) Day 1 Day 45 Reviewee Notification Fieldwork Planning/Pre-Fieldwork Help resolve any data issues Entrance Conference Continue data extraction for remaining years Review and provide feedback on testing methodologies Approve of updated methodologies as appropriate Preliminary Results Data Exceptions Conference Review initial payor determinations (direct vs. non-direct) Provide supporting documentation for any disagreements Review and provide feedback on preliminary results Provide supporting documentation for any disagreements Participate in a conference call to discuss the preliminary results Data Extraction Testing Methodologies Day 85 Day 125 Day 195 Payor Determinations Draft Report Exit Conference Provider Response Day 235 Final Report
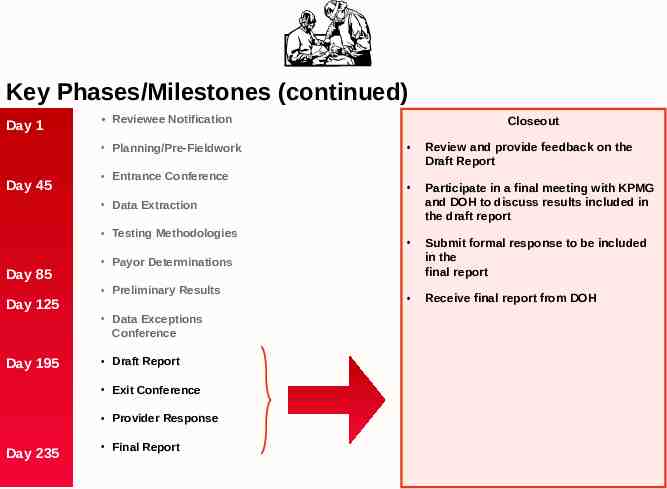
Key Phases/Milestones (continued) Day 1 Reviewee Notification Planning/Pre-Fieldwork Day 45 Entrance Conference Closeout Review and provide feedback on the Draft Report Participate in a final meeting with KPMG and DOH to discuss results included in the draft report Submit formal response to be included in the final report Receive final report from DOH Data Extraction Testing Methodologies Day 85 Day 125 Day 195 Payor Determinations Preliminary Results Data Exceptions Conference Draft Report Exit Conference Provider Response Day 235 Final Report
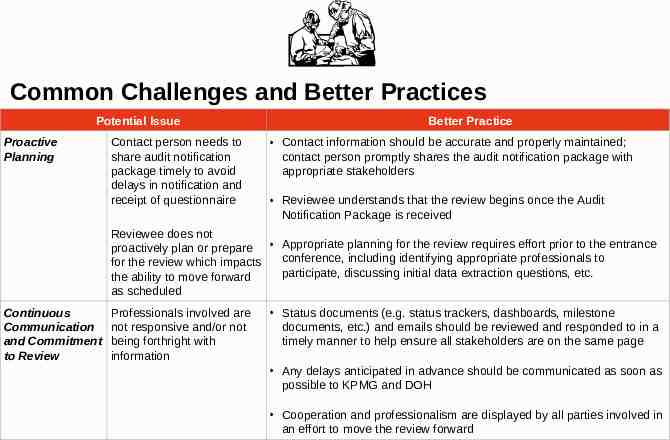
Common Challenges and Better Practices Potential Issue Proactive Planning Contact person needs to share audit notification package timely to avoid delays in notification and receipt of questionnaire Better Practice Contact information should be accurate and properly maintained; contact person promptly shares the audit notification package with appropriate stakeholders Reviewee understands that the review begins once the Audit Notification Package is received Reviewee does not proactively plan or prepare Appropriate planning for the review requires effort prior to the entrance conference, including identifying appropriate professionals to for the review which impacts participate, discussing initial data extraction questions, etc. the ability to move forward as scheduled Continuous Communication and Commitment to Review Professionals involved are not responsive and/or not being forthright with information Status documents (e.g. status trackers, dashboards, milestone documents, etc.) and emails should be reviewed and responded to in a timely manner to help ensure all stakeholders are on the same page Any delays anticipated in advance should be communicated as soon as possible to KPMG and DOH Cooperation and professionalism are displayed by all parties involved in an effort to move the review forward
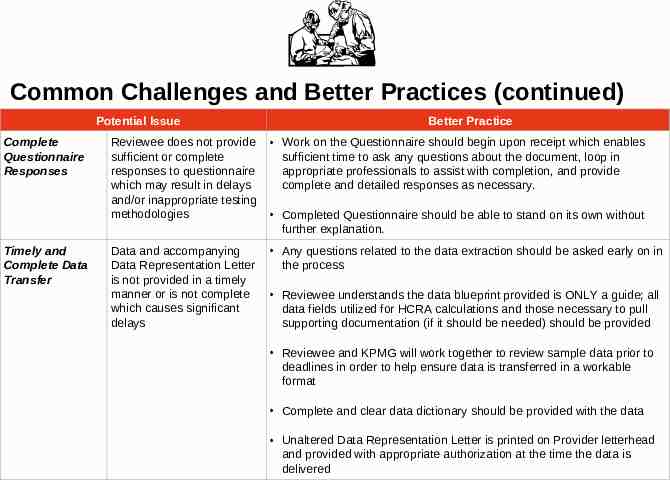
Common Challenges and Better Practices (continued) Potential Issue Complete Questionnaire Responses Timely and Complete Data Transfer Better Practice Reviewee does not provide sufficient or complete responses to questionnaire which may result in delays and/or inappropriate testing methodologies Work on the Questionnaire should begin upon receipt which enables sufficient time to ask any questions about the document, loop in appropriate professionals to assist with completion, and provide complete and detailed responses as necessary. Data and accompanying Data Representation Letter is not provided in a timely manner or is not complete which causes significant delays Any questions related to the data extraction should be asked early on in the process Completed Questionnaire should be able to stand on its own without further explanation. Reviewee understands the data blueprint provided is ONLY a guide; all data fields utilized for HCRA calculations and those necessary to pull supporting documentation (if it should be needed) should be provided Reviewee and KPMG will work together to review sample data prior to deadlines in order to help ensure data is transferred in a workable format Complete and clear data dictionary should be provided with the data Unaltered Data Representation Letter is printed on Provider letterhead and provided with appropriate authorization at the time the data is delivered
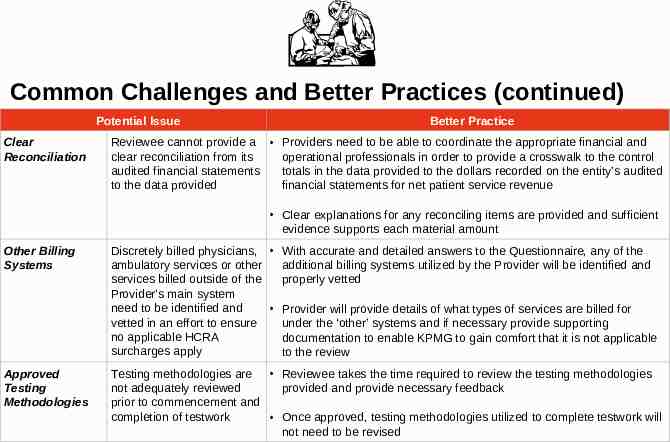
Common Challenges and Better Practices (continued) Potential Issue Clear Reconciliation Better Practice Reviewee cannot provide a Providers need to be able to coordinate the appropriate financial and clear reconciliation from its operational professionals in order to provide a crosswalk to the control audited financial statements totals in the data provided to the dollars recorded on the entity’s audited to the data provided financial statements for net patient service revenue Clear explanations for any reconciling items are provided and sufficient evidence supports each material amount Other Billing Systems Discretely billed physicians, With accurate and detailed answers to the Questionnaire, any of the ambulatory services or other additional billing systems utilized by the Provider will be identified and services billed outside of the properly vetted Provider’s main system need to be identified and Provider will provide details of what types of services are billed for vetted in an effort to ensure under the ‘other’ systems and if necessary provide supporting no applicable HCRA documentation to enable KPMG to gain comfort that it is not applicable surcharges apply to the review Approved Testing Methodologies Reviewee takes the time required to review the testing methodologies Testing methodologies are not adequately reviewed provided and provide necessary feedback prior to commencement and completion of testwork Once approved, testing methodologies utilized to complete testwork will not need to be revised
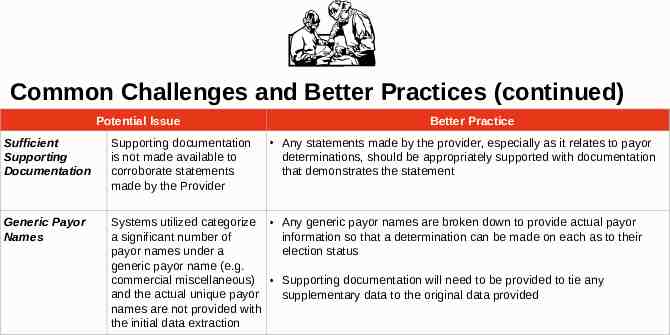
Common Challenges and Better Practices (continued) Potential Issue Better Practice Any statements made by the provider, especially as it relates to payor determinations, should be appropriately supported with documentation that demonstrates the statement Sufficient Supporting Documentation Supporting documentation is not made available to corroborate statements made by the Provider Generic Payor Names Systems utilized categorize Any generic payor names are broken down to provide actual payor a significant number of information so that a determination can be made on each as to their payor names under a election status generic payor name (e.g. commercial miscellaneous) Supporting documentation will need to be provided to tie any and the actual unique payor supplementary data to the original data provided names are not provided with the initial data extraction
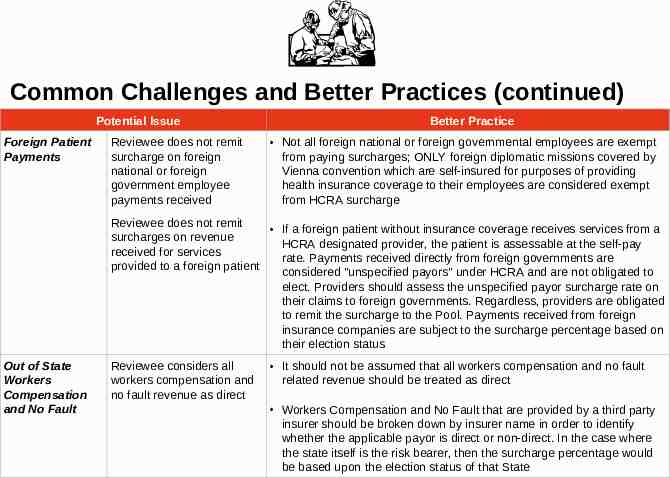
Common Challenges and Better Practices (continued) Potential Issue Foreign Patient Payments Reviewee does not remit surcharge on foreign national or foreign government employee payments received Better Practice Not all foreign national or foreign governmental employees are exempt from paying surcharges; ONLY foreign diplomatic missions covered by Vienna convention which are self-insured for purposes of providing health insurance coverage to their employees are considered exempt from HCRA surcharge Reviewee does not remit If a foreign patient without insurance coverage receives services from a surcharges on revenue HCRA designated provider, the patient is assessable at the self-pay received for services rate. Payments received directly from foreign governments are provided to a foreign patient considered "unspecified payors" under HCRA and are not obligated to elect. Providers should assess the unspecified payor surcharge rate on their claims to foreign governments. Regardless, providers are obligated to remit the surcharge to the Pool. Payments received from foreign insurance companies are subject to the surcharge percentage based on their election status Out of State Workers Compensation and No Fault Reviewee considers all workers compensation and no fault revenue as direct It should not be assumed that all workers compensation and no fault related revenue should be treated as direct Workers Compensation and No Fault that are provided by a third party insurer should be broken down by insurer name in order to identify whether the applicable payor is direct or non-direct. In the case where the state itself is the risk bearer, then the surcharge percentage would be based upon the election status of that State
CONTACT INFORMATION 1 Contact the Office of Pool Administration: Telephone: (315) 671-3800 Email: [email protected] For Questions Relating To: For Questions Relating To: Electronic website for report submission questions Obtaining a user ID and password, or trouble with logging on Setting up file transfer Pool payments Questions relating to receipt of Pool payments
Contact Information (continued) 2 Contact the Department of Health: Telephone: (518) 474-1673 [email protected] For Questions Relating To: The surchargeability of revenue and distributions Interpretation of the Public Health Law on HCRA Specific report line questions about reportable revenue and deductions Any questions regarding the 1% Statewide Report Any delinquencies, Medicaid recoupments or referrals to the state’s Attorney General’s Office based on HCRA delinquencies Electing Payors or Third Party Administrators

QUESTIONS