GASTROINTESTINAL GASTROINTESTINAL PHARMACOLOGY PHARMACOLOGY
59 Slides6.93 MB
GASTROINTESTINAL GASTROINTESTINAL PHARMACOLOGY PHARMACOLOGY Charles Nichols, PhD Department of Pharmacology & Experimental Therapeutics LSUHSC, New Orleans, LA 70112
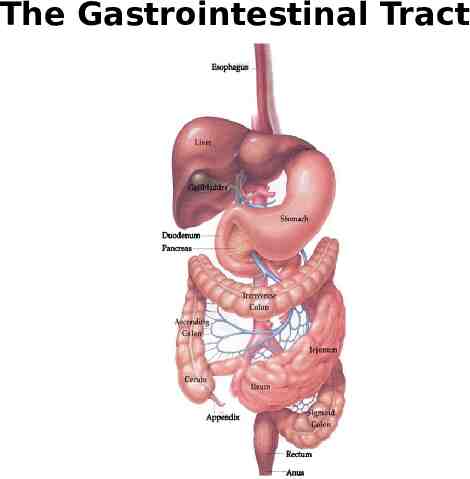
The Gastrointestinal Tract
GASTROINTESTINAL GASTROINTESTINAL DISORDERS DISORDERS Gastroesophageal Peptic Reflux Disease (GERD) Ulcer Disease (PUD) Duodenal Ulcer Nausea Emesis IBS Diarrhea Constipation
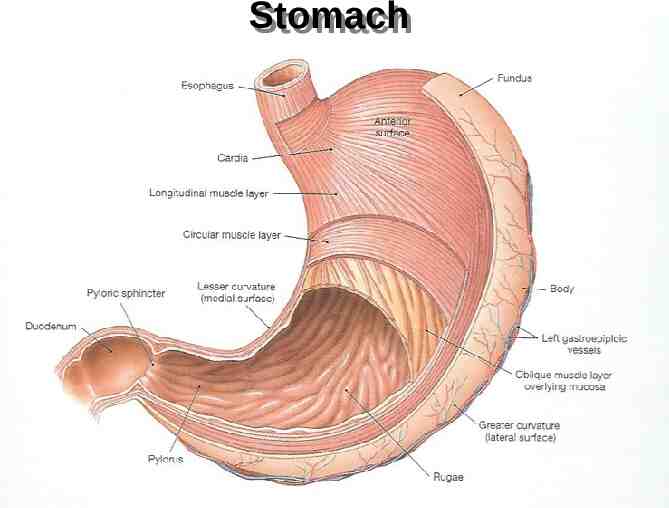
Stomach Stomach
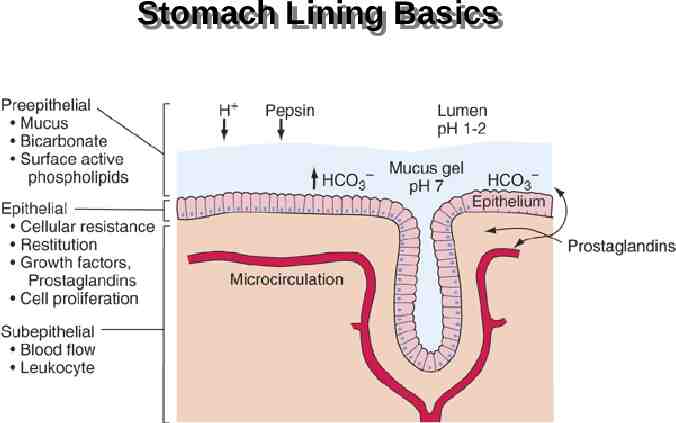
Stomach Stomach Lining Lining Basics Basics
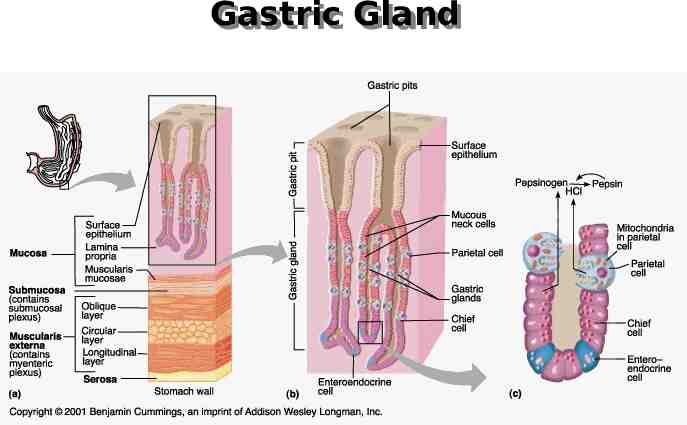
Gastric Gastric Gland Gland
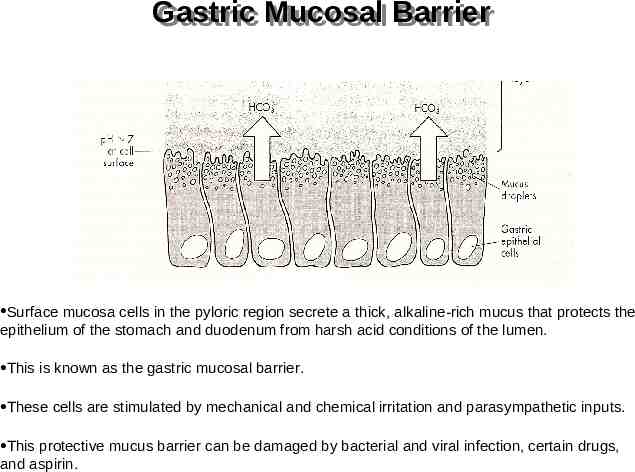
Gastric Gastric Mucosal Mucosal Barrier Barrier Surface mucosa cells in the pyloric region secrete a thick, alkaline-rich mucus that protects the epithelium of the stomach and duodenum from harsh acid conditions of the lumen. This is known as the gastric mucosal barrier. These cells are stimulated by mechanical and chemical irritation and parasympathetic inputs. This protective mucus barrier can be damaged by bacterial and viral infection, certain drugs, and aspirin.
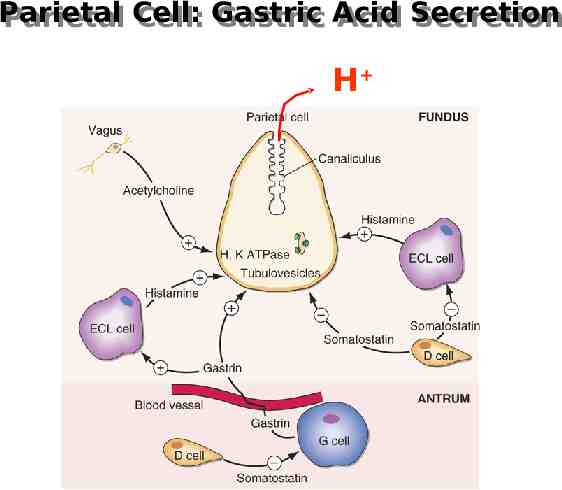
Parietal Parietal Cell: Cell: Gastric Gastric Acid Acid Secretion Secretion H
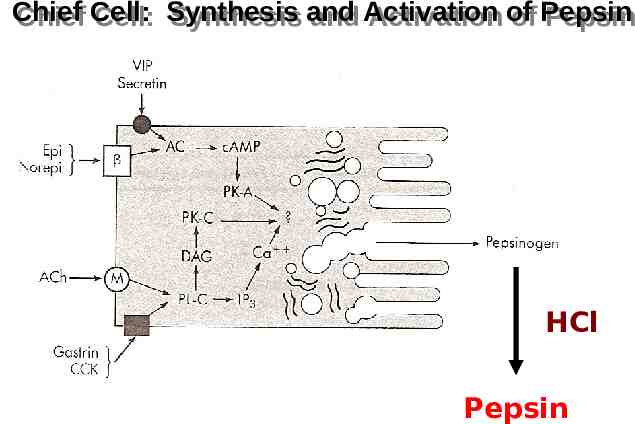
Chief Chief Cell: Cell: Synthesis Synthesis and and Activation Activation of of Pepsin Pepsin HCl HCl Pepsin Pepsin
Serotonin Serotonin (5-Hydroxytryptamine) (5-Hydroxytryptamine) Key neurotransmitter in the intestine Present in abundance within the gut Most is stored in enterochromaffin cell granules Released by many stimuli - most potently by mucosal stroking Serotonin stimulates enteric nerves to initiate secretion and propulsive motility
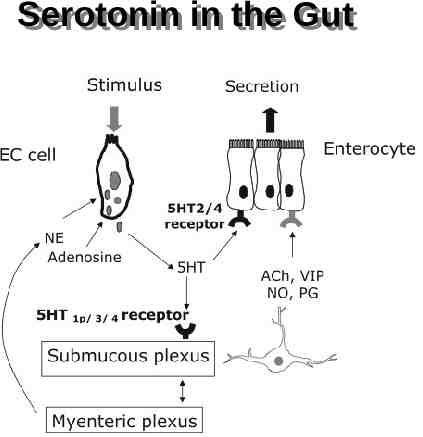
Serotonin Serotonin in in the the Gut Gut
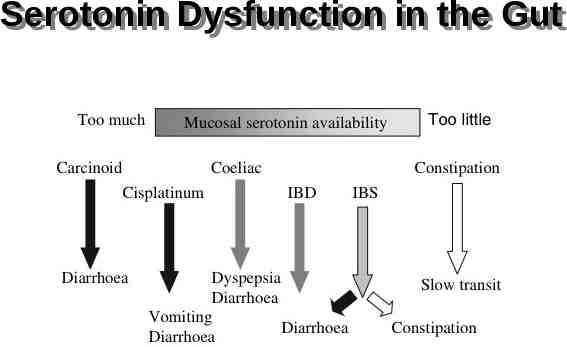
Serotonin Serotonin Dysfunction Dysfunction in in the the Gut Gut
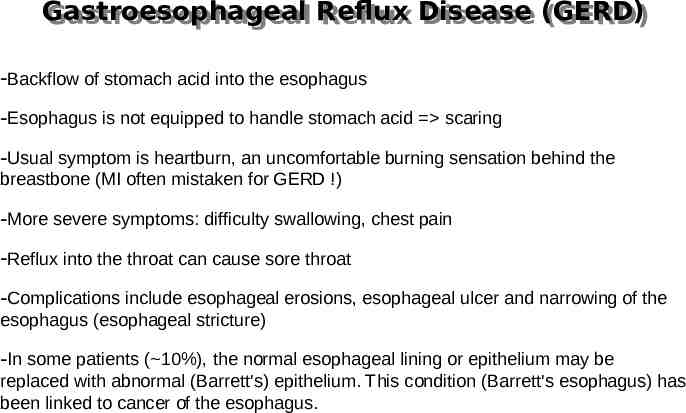
Gastroesophageal Gastroesophageal Reflux Reflux Disease Disease (GERD) (GERD) -Backflow of stomach acid into the esophagus -Esophagus is not equipped to handle stomach acid scaring -Usual symptom is heartburn, an uncomfortable burning sensation behind the breastbone (MI often mistaken for GERD !) -More severe symptoms: difficulty swallowing, chest pain -Reflux into the throat can cause sore throat -Complications include esophageal erosions, esophageal ulcer and narrowing of the esophagus (esophageal stricture) -In some patients ( 10%), the normal esophageal lining or epithelium may be replaced with abnormal (Barrett's) epithelium. This condition (Barrett's esophagus) has been linked to cancer of the esophagus.
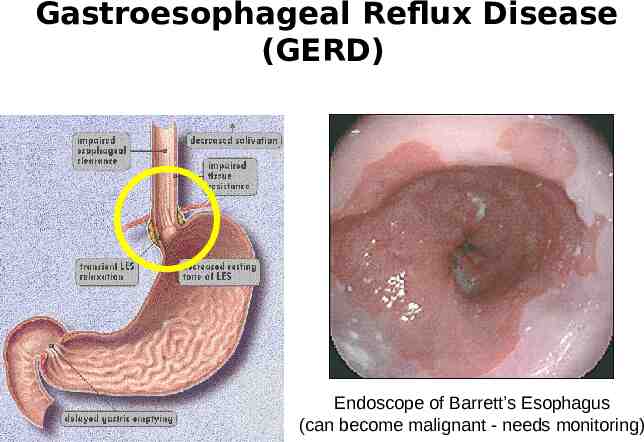
Gastroesophageal Reflux Disease (GERD) Endoscope of Barrett’s Esophagus (can become malignant - needs monitoring)

Gastroesophageal Gastroesophageal Reflux Reflux Disease Disease (GERD) (GERD) Precipitants: Food (fatty food, alcohol, caffeine) Smoking Obesity Pregnancy Usually chronic relapsing course
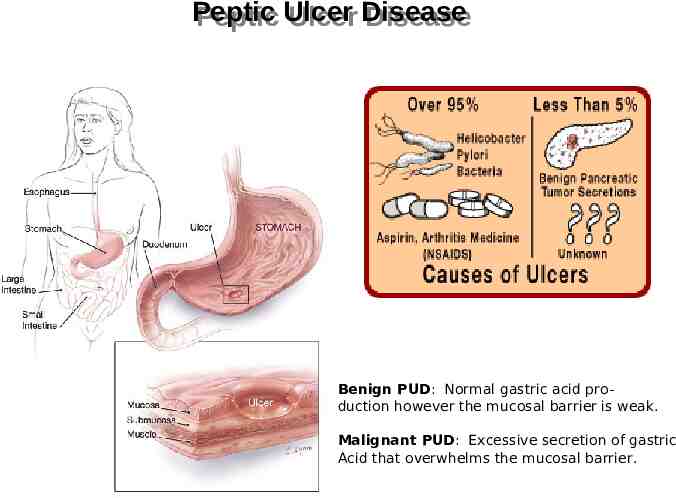
Peptic Peptic Ulcer Ulcer Disease Disease Benign PUD: Normal gastric acid production however the mucosal barrier is weak. Malignant PUD: Excessive secretion of gastric Acid that overwhelms the mucosal barrier.
Treatment Treatment of of Heartburn, Heartburn, GERD GERD and and PUD PUD Antacids H2 Receptor Blockers Mucosal Protective Agents Proton Pump Inhibitors Anti-cholinergics Prostaglandin Analogs Anti-microbial Agents
Antacids Antacids Systemic Antacid: Sodium Bicarbonate Nonsystemic Antacid: Aluminum Hydroxide Magnesium Hydroxide Combinations (Maalox and Mylanta) Contraindicated in patients with impaired renal function Magnesium may cause diarrhea Calcium Carbonate (Tums) Calcium may cause constipation
ANTACID ANTACID NEUTRALIZING NEUTRALIZING CAPACITY CAPACITY (ANC) (ANC) Amount of 1N HCl(meq) brought to pH 3.5 by an antacid solution within 15 min. FDA requires a Min 5 meq/dose As the ANC number increases the neutralizing capacity of an antacid increases. Maalox TC 28 Mylanta DS 23 Tums EX 15

Histamine Histamine H H22 Receptor Receptor Blockers Blockers Inhibit secretion of gastric acid through competitive inhibition of Histamine H2 receptors Prevention & tx of PUD, Esophagitis, GI bleeding, stress ulcers, and ZollingerEllison Syndrome May alter the effects of other drugs through interactions with CYP450 (especially cimetidine) Very few side effects (except for cimetidine - inhibits metabolism of estrogen) Suppresses 24 hour gastric secretion by 70% Cimetidine Famotidine Ranitidine Nizatidine

Proton Proton Pump Pump Inhibitors Inhibitors Strong inhibitors of gastric acid secretion through irreversible inhibition of proton pump, preventing “pumping” or release of gastric acid (24 hr action) Indicated in PUD, Gastritis, GERD, & Zollinger-Ellison syndrome Faster relief and healing than H2 receptor blockers Decreases acid secretion by up to 95% for up to 48 hours 4-8 week course of treatment Omeprazole Lansoprazole Rebeprazole Esomeprazole Pantoprazole
Misoprostol Prostaglandins Prostaglandins PGE1 analog Stimulates Gi pathway, leading to decrease in gastric acid release For treatment of NSAID induced injury Side effects include diarrhea, pain, and cramps (30%) Do not give to women of childbearing years unless a reliable method of birth control can be DOCUMENTED Can cause birth defects, and premature birth Misoprostol
Anticholinergics Anticholinergics Pirenzipine Muscarinic M1 acetylcholine receptor antagonist Blocks gastric acid secretions About as effective as H2 blockers Rarely used, primarily as adjunct therapy Anticholinergic side effects (anorexia, blurry vision, constipation, dry mouth, sedation)
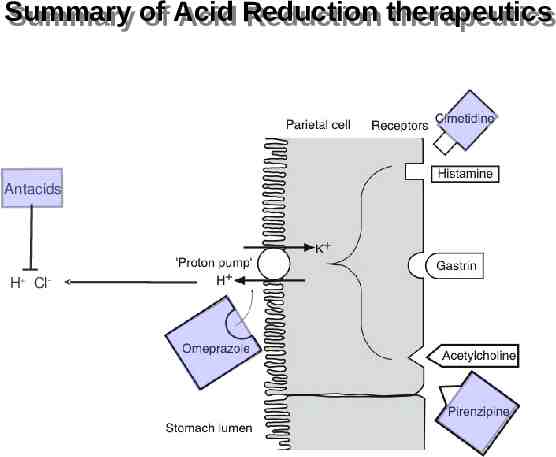
Summary Summary of of Acid Acid Reduction Reduction therapeutics therapeutics Antacids H Cl-
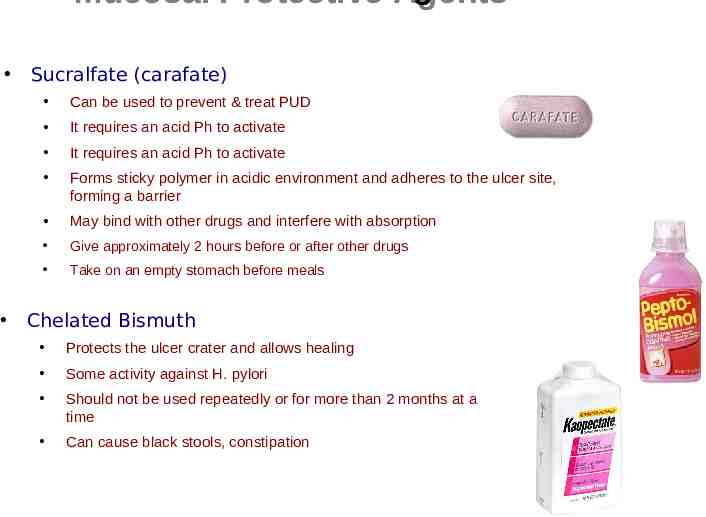
Mucosal Protective Agents Sucralfate (carafate) Can be used to prevent & treat PUD It requires an acid Ph to activate It requires an acid Ph to activate Forms sticky polymer in acidic environment and adheres to the ulcer site, forming a barrier May bind with other drugs and interfere with absorption Give approximately 2 hours before or after other drugs Take on an empty stomach before meals Chelated Bismuth Protects the ulcer crater and allows healing Some activity against H. pylori Should not be used repeatedly or for more than 2 months at a time Can cause black stools, constipation
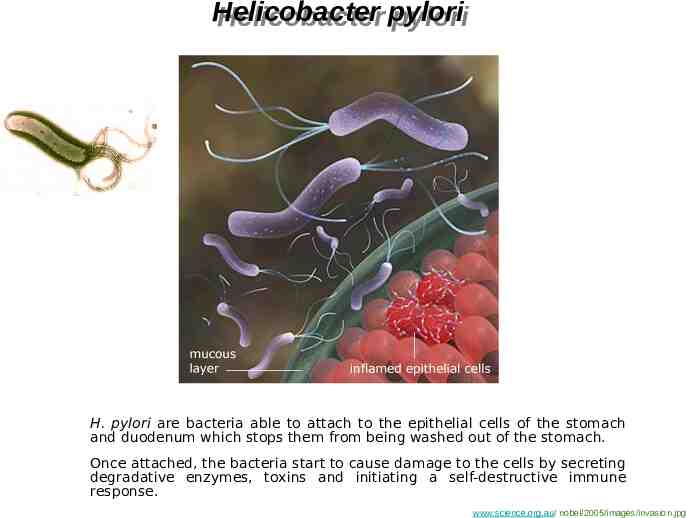
Helicobacter Helicobacter pylori pylori H. pylori are bacteria able to attach to the epithelial cells of the stomach and duodenum which stops them from being washed out of the stomach. Once attached, the bacteria start to cause damage to the cells by secreting degradative enzymes, toxins and initiating a self-destructive immune response. www.science.org.au/ nobel/2005/images/invasion.jpg
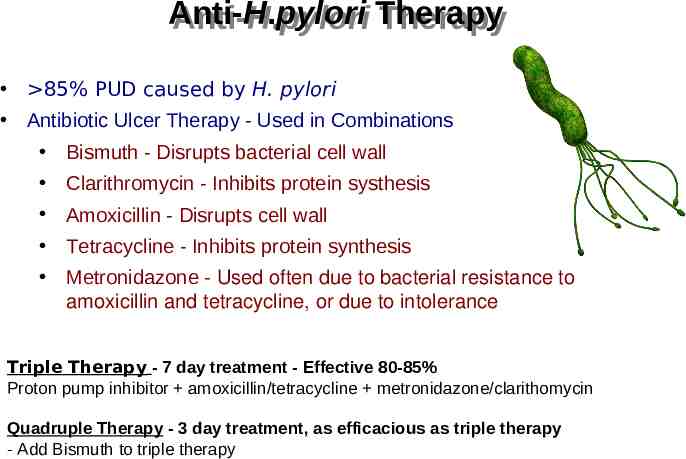
Anti-H.pylori Anti-H.pylori Therapy Therapy 85% PUD caused by H. pylori Antibiotic Ulcer Therapy - Used in Combinations Bismuth - Disrupts bacterial cell wall Clarithromycin - Inhibits protein systhesis Amoxicillin - Disrupts cell wall Tetracycline - Inhibits protein synthesis Metronidazone - Used often due to bacterial resistance to amoxicillin and tetracycline, or due to intolerance Triple Therapy - 7 day treatment - Effective 80-85% Proton pump inhibitor amoxicillin/tetracycline metronidazone/clarithomycin Quadruple Therapy - 3 day treatment, as efficacious as triple therapy - Add Bismuth to triple therapy

Moving Moving down down the the system. system.
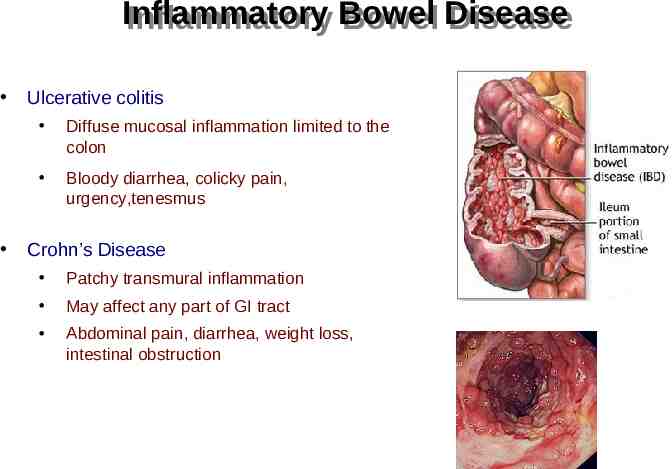
Inflammatory Inflammatory Bowel Bowel Disease Disease Ulcerative colitis Diffuse mucosal inflammation limited to the colon Bloody diarrhea, colicky pain, urgency,tenesmus Crohn’s Disease Patchy transmural inflammation May affect any part of GI tract Abdominal pain, diarrhea, weight loss, intestinal obstruction
Inflammatory Inflammatory Bowel Bowel Disease Disease Treatment Resolve acute episodes and prolong remission Therapeutics: Aminosalicylates - for mild symptoms Corticosteroids - for moderate symptoms Thiopurines - for active and chronic symptoms Methotrexate - for active and chronic symptoms Cyclosporin - for active and chronic symptoms refractory to corticorsteroids- (significant side effects) Infliximab - antibody infusion
Aminosalicylates Aminosalicylates Sulfasalazine (5-aminosalicylic acid and sulfapyridine as carrier substance) Mesalazine (5-ASA), eg Asacol, Pentasa Balsalazide (prodrug of 5-ASA) Olsalazine (5-ASA dimer cleaves in colon) Oral, rectal preparation Use Maintaining remission Active disease May reduce risk of colorectal cancer Adverse effects 10-45% Nausea, headache, epigastric pain, diarrhoea, hypersensitivity, pancreatitis, blood disorders, lung disorders, myo/pericarditis Caution in renal impairment, pregnancy, breast feeding
Corticosteroids Corticosteroids Anti-inflammatory agents for moderate to severe relapses eg 40mg Prednisolone Inhibition of inflammatory pathways ( IL transcription, suppression of arachidonic acid metabolism, lymphocyte apoptosis) Side effects Acne, moon face Sleep, mode disturbance Dyspepsia, glucose intolerance Cataracts, osteoporosis, myopathy
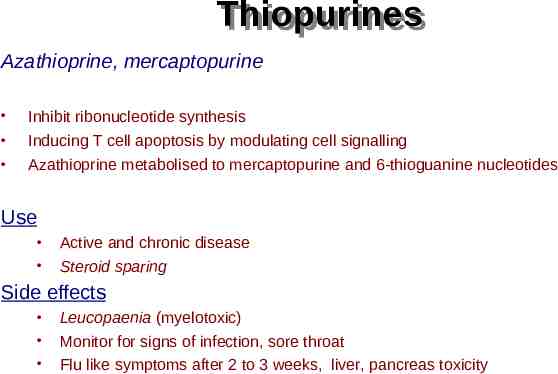
Thiopurines Thiopurines Azathioprine, mercaptopurine Inhibit ribonucleotide synthesis Inducing T cell apoptosis by modulating cell signalling Azathioprine metabolised to mercaptopurine and 6-thioguanine nucleotides Use Active and chronic disease Steroid sparing Side effects Leucopaenia (myelotoxic) Monitor for signs of infection, sore throat Flu like symptoms after 2 to 3 weeks, liver, pancreas toxicity
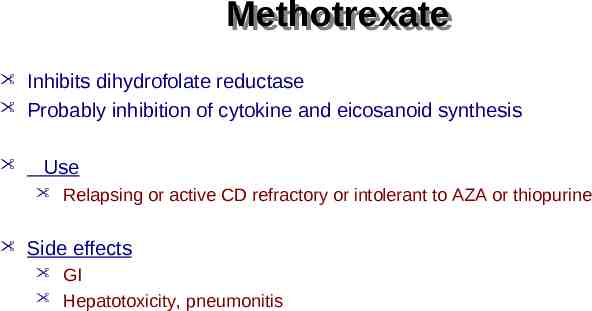
Methotrexate Methotrexate Inhibits dihydrofolate reductase Probably inhibition of cytokine and eicosanoid synthesis Use Relapsing or active CD refractory or intolerant to AZA or thiopurine Side effects GI Hepatotoxicity, pneumonitis
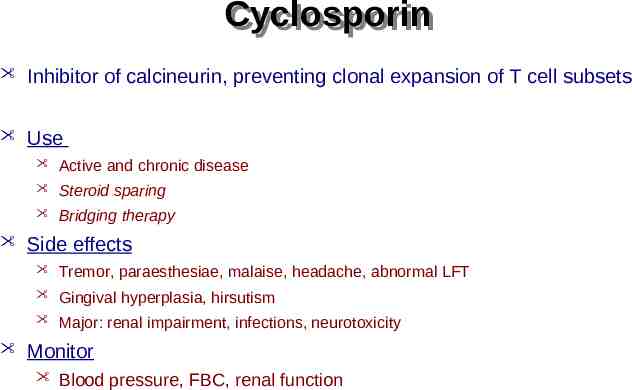
Cyclosporin Cyclosporin Inhibitor of calcineurin, preventing clonal expansion of T cell subsets Use Active and chronic disease Steroid sparing Bridging therapy Side effects Tremor, paraesthesiae, malaise, headache, abnormal LFT Gingival hyperplasia, hirsutism Major: renal impairment, infections, neurotoxicity Monitor Blood pressure, FBC, renal function
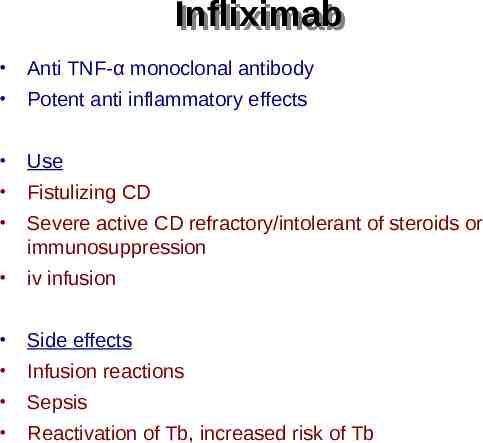
Infliximab Infliximab Anti TNF-α monoclonal antibody Potent anti inflammatory effects Use Fistulizing CD Severe active CD refractory/intolerant of steroids or immunosuppression iv infusion Side effects Infusion reactions Sepsis Reactivation of Tb, increased risk of Tb
Constipation Constipation
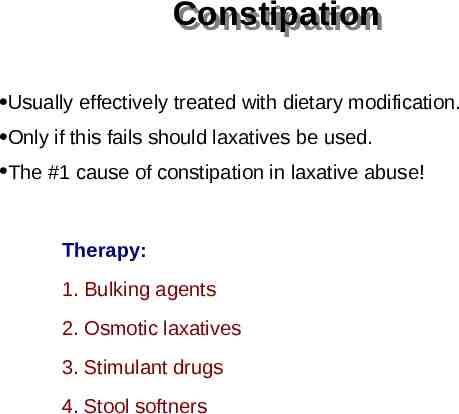
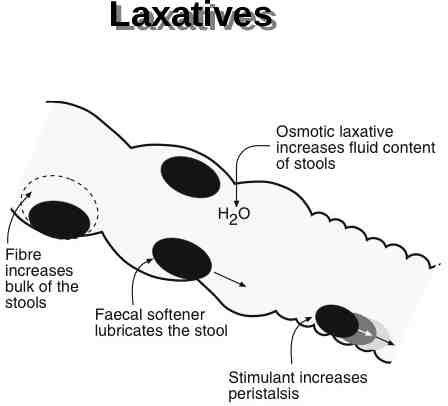
Constipation Constipation Usually effectively treated with dietary modification. Only if this fails should laxatives be used. The #1 cause of constipation in laxative abuse! Therapy: 1. Bulking agents 2. Osmotic laxatives 3. Stimulant drugs 4. Stool softners
Laxatives Laxatives
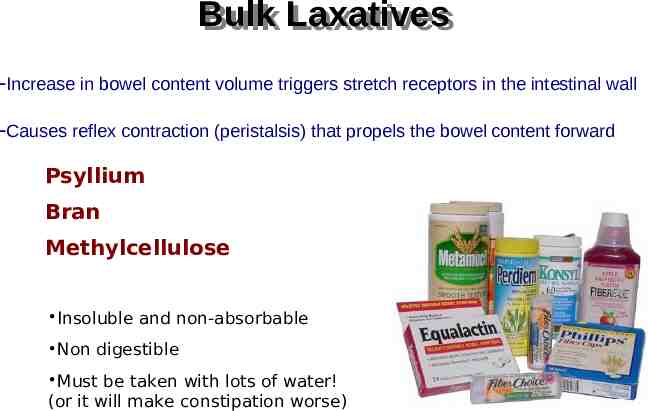
Bulk Bulk Laxatives Laxatives -Increase in bowel content volume triggers stretch receptors in the intestinal wall -Causes reflex contraction (peristalsis) that propels the bowel content forward Psyllium Bran Methylcellulose Insoluble and non-absorbable Non digestible Must be taken with lots of water! (or it will make constipation worse)
Saline Saline and and Osmotic Osmotic Laxatives Laxatives -Effective in 1-3 hours -Used to purge intestine (e.g. surgery, poisoning) -Fluid is drawn into the bowel by osmotic force, increasing volume and triggering peristalsis Nondigestible sugars and alcohols Lactulose (broken down by bacteria to acetic and lactic acid, which causes the osmotic effect) Salts Milk of Magnesia (Mg(OH)2) Epsom Salt (MgSO4) Glauber’s Salt (Na2SO4) Sodium Phosphates (used as enema) Sodium Citrate (used as enema) Polyethylene glycol
Stool Stool Softners Softners -- Emollients Emollients Docusate sodium (surfactant and stimulant) Liquid Paraffin (oral solution) Glycerin suppositories Docusate
Irratant/Stimulant Irratant/Stimulant Laxatives-Cathartics Laxatives-Cathartics -Increases intestinal motility -Irritate the GI mucosa and pull water into the lumen -Indicated for severe constipation where more rapid effect is required (6-8 hours) Castor Oil - From the Castor Bean Senna - Plant derivative Bisacodyl Lubiprostone -PGE1 derivative that stimulates chloride channels, producing chloride rich secretions Bisacodyl Senna Lubiprostone
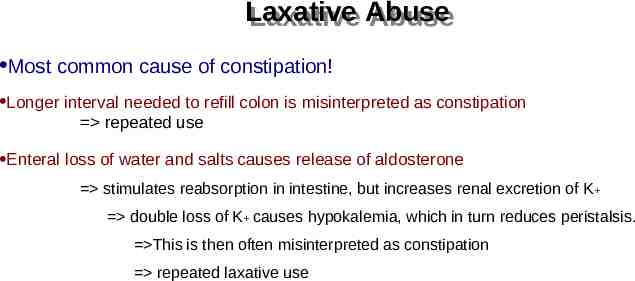
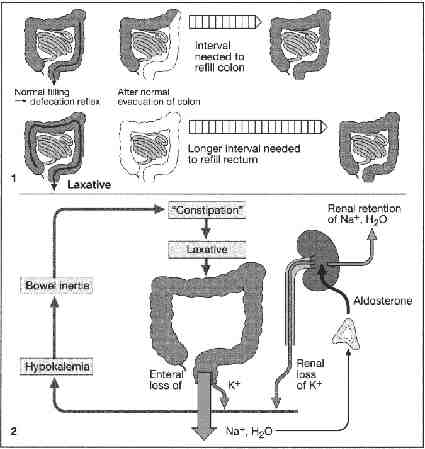
Laxative Laxative Abuse Abuse Most common cause of constipation! Longer interval needed to refill colon is misinterpreted as constipation repeated use Enteral loss of water and salts causes release of aldosterone stimulates reabsorption in intestine, but increases renal excretion of K double loss of K causes hypokalemia, which in turn reduces peristalsis. This is then often misinterpreted as constipation repeated laxative use
Diarrhea Diarrhea
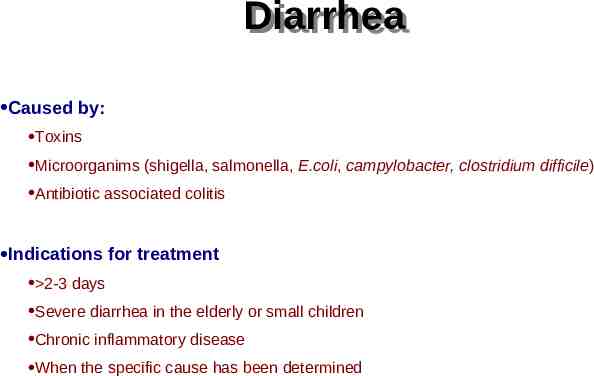
Diarrhea Diarrhea Caused by: Toxins Microorganims (shigella, salmonella, E.coli, campylobacter, clostridium difficile) Antibiotic associated colitis Indications for treatment 2-3 days Severe diarrhea in the elderly or small children Chronic inflammatory disease When the specific cause has been determined
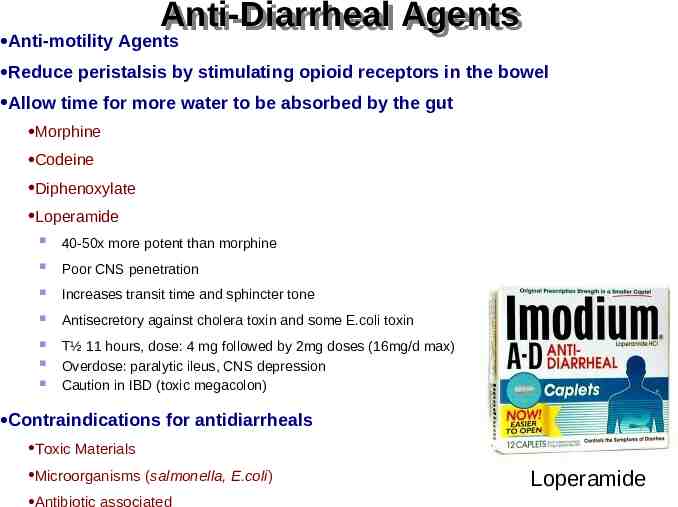
Anti-Diarrheal Agents Anti-Diarrheal Agents Anti-motility Agents Reduce peristalsis by stimulating opioid receptors in the bowel Allow time for more water to be absorbed by the gut Morphine Codeine Diphenoxylate Loperamide 40-50x more potent than morphine Poor CNS penetration Increases transit time and sphincter tone Antisecretory against cholera toxin and some E.coli toxin T½ 11 hours, dose: 4 mg followed by 2mg doses (16mg/d max) Overdose: paralytic ileus, CNS depression Caution in IBD (toxic megacolon) Contraindications for antidiarrheals Toxic Materials Microorganisms (salmonella, E.coli) Antibiotic associated Loperamide
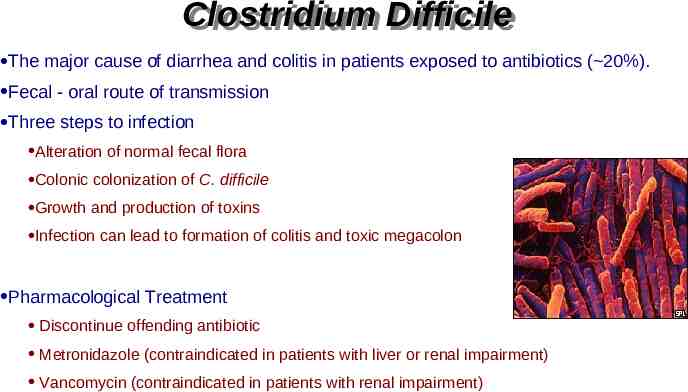
Clostridium Clostridium Difficile Difficile The major cause of diarrhea and colitis in patients exposed to antibiotics ( 20%). Fecal - oral route of transmission Three steps to infection Alteration of normal fecal flora Colonic colonization of C. difficile Growth and production of toxins Infection can lead to formation of colitis and toxic megacolon Pharmacological Treatment Discontinue offending antibiotic Metronidazole (contraindicated in patients with liver or renal impairment) Vancomycin (contraindicated in patients with renal impairment)
Antiflatulants Antiflatulants (Le Pétomane)
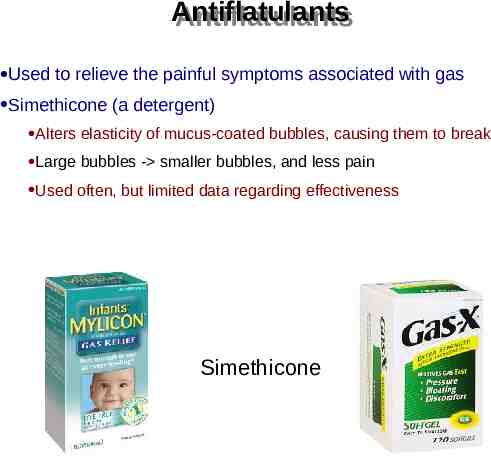
Antiflatulants Antiflatulants Used to relieve the painful symptoms associated with gas Simethicone (a detergent) Alters elasticity of mucus-coated bubbles, causing them to break Large bubbles - smaller bubbles, and less pain Used often, but limited data regarding effectiveness Simethicone
Emesis Emesis (Vomiting)
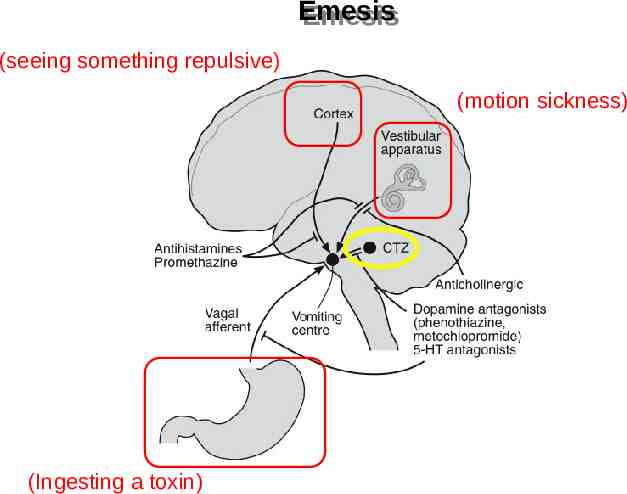
Emesis Emesis (seeing something repulsive) (motion sickness) (Ingesting a toxin)
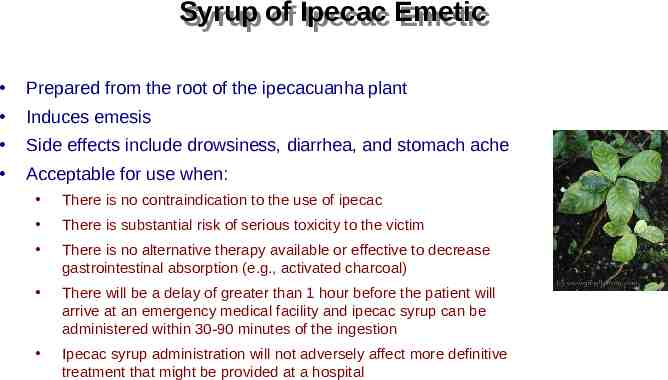
Syrup Syrup of of Ipecac Ipecac Emetic Emetic Prepared from the root of the ipecacuanha plant Induces emesis Side effects include drowsiness, diarrhea, and stomach ache Acceptable for use when: There is no contraindication to the use of ipecac There is substantial risk of serious toxicity to the victim There is no alternative therapy available or effective to decrease gastrointestinal absorption (e.g., activated charcoal) There will be a delay of greater than 1 hour before the patient will arrive at an emergency medical facility and ipecac syrup can be administered within 30-90 minutes of the ingestion Ipecac syrup administration will not adversely affect more definitive treatment that might be provided at a hospital
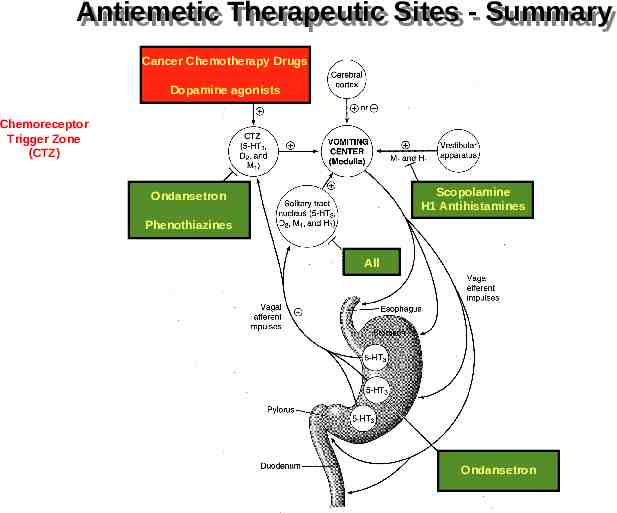
Antiemetic Antiemetic Therapuetics Therapuetics Muscarinic M1 receptor antagonist Scopolamine Side Effects: Dry Mouth Dizziness Restlessness Dilated Pupils Delirium at high doses Allergic Reaction Contraindications Kidney or liver disease Enlarged prostate Difficulty in urination / bladder problems Heart Disease
Antiemetic Therapuetics Antiemetic Therapuetics D2 receptor antagonist Histamine H1/Dopamine Phenothiazines Promethazine (Phenergan) Prochlorperazine (Compazine) Side Effects These drugs are neuroleptics (typical antipsychotics) Blurred vision Dry mouth Dizziness Restlessness Seizures Extrapyramidal effects - Tardive dyskinesia (long term treatment) Contraindications Allergy to phenthiazines Glaucoma Liver disease
Antiemetic Antiemetic Therapuetics Therapuetics Serotonin 5-HT3 receptor antagonist Ondansetron (Zofran) Granisetron Excellent for chemotherapy induced nausea and vomiting Side Effects Very few common side effects - usually well tolerated Headache Constipation Rarely Hiccups Itchiness Transient blindness
Antiemetic Antiemetic Therapeutic Therapeutic Sites Sites -- Summary Summary Cancer Chemotherapy Drugs Dopamine agonists Chemoreceptor Trigger Zone (CTZ) Scopolamine H1 Antihistamines Ondansetron Phenothiazines All Ondansetron