Diabetes Technologies Insulin Pump Therapy Beverly Thomassian,
57 Slides6.07 MB
Diabetes Technologies Insulin Pump Therapy Beverly Thomassian, RN, MPH, BC-ADM, CDE President, Diabetes Education Services
Diabetes Technologies – Insulin Pumps 1. Describe critical teaching content before starting insulin pump therapy 2. Discuss strategies to determine and fine-tune insulin pump basal rates. 3. Discuss how to determine and fine tune bolus rates including coverage for carbs and hyperglycemia. 4. State important safety measures to prevent hyperglycemic crises. 5. List inpatient considerations for insulin pump therapy and CGMs
Conflict of Interest and Resources Coach Bev has no conflict of interest Technology field is rapidly changing Photos in slide set are from Pixabay – not actual clients Resources AADE Practice Paper 2018- Continuous Subcutaneous Insulin Infusion (CSII) Without and With Sensor Integration AADE Practice Paper 2018- Diabetes Educator Role in Continuous Glucose Monitoring Company web sites – virtual demo AADE – DANA Diabetes Advanced Network Access www.diabeteseducator.org Need to be AADE Member to access Diabetes Forecast Consumer Guide 2019 Pumping Insulin by John Walsh, PA, CDE – Diabetes Mall Gary Scheiner, MS, CDE – Integrated Diabetes Services
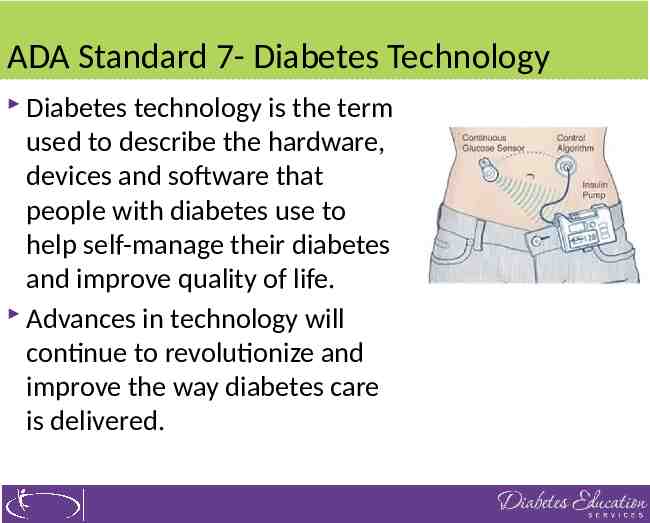
ADA Standard 7- Diabetes Technology Diabetes technology is the term used to describe the hardware, devices and software that people with diabetes use to help self-manage their diabetes and improve quality of life. Advances in technology will continue to revolutionize and improve the way diabetes care is delivered.
Diabetes Technology – Topics This rapid change in the technology landscape can make it difficult and confusing for diabetes educators and providers to keep up to date. Insulin delivery methods Insulin syringes, pens, disposable patch, pumps Setting and evaluating basal and bolus settings Inpatient management Traveling with technology Continuous glucose monitoring
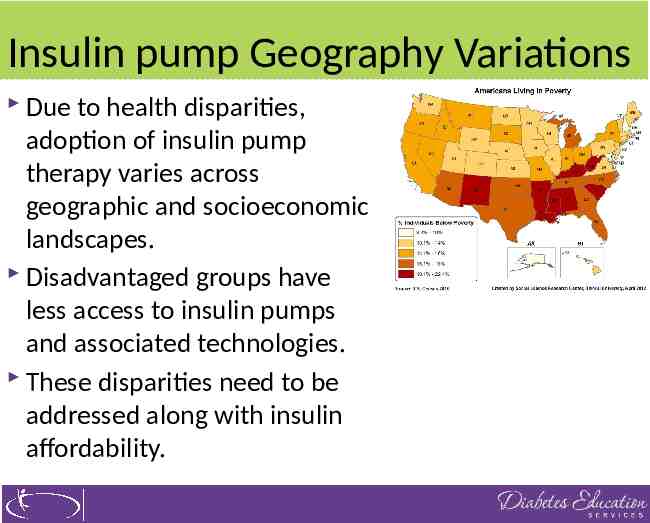
Insulin pump Geography Variations Due to health disparities, adoption of insulin pump therapy varies across geographic and socioeconomic landscapes. Disadvantaged groups have less access to insulin pumps and associated technologies. These disparities need to be addressed along with insulin affordability.
Pre Pump Knowledge / Education Establishment of Goals Competence in Carb counting Insulin Carb Ratios (ICR) & Correction or sensitivity factor (CF) Ability to manage hyper and hypoglycemia Self-adjust insulin Carbs Correction Physical activity
Pre Pump Knowledge / Education Ability to fill and insert cartridge/reservoir and insert and change infusion sets Ability to detect infusion set and site issues Manage sick days, exercise and travel Trouble shoot and ability to solve pump issues Understand BG Data Hypo prevention and treatment Basic of basal bolus therapy and how to switch back to injections if needed
Lifestyle Indications and Attributes Erratic schedule Varied work shifts Frequent travel Desire for flexibility Tired of MDI Athletes Temporary basal adjust Disconnect options Waterproof options
LifeStyle Indications for Candidate or Parents of Pump Wearer Parents and caretakers must have a thorough understanding and willingness and time to understand the pump and work with team to problem solve Willingness to work with healthcare provider during prepump training Adequate insurance benefits or personal resources
LifeStyle Indications for Candidate or Parents of Pump Wearer Physical ability View pump Fill and replace insulin cartridge Insert an infusion set Wear the pump Perform technical functions Emotional stability and adequate emotional support from family or others
Caregiver education about pumps Key Topics Hypo detection /treatment Hyperglycemia trouble shooting Basic bolus procedure Cartridge set change process Understand what alarms mean History recall
Poll Question 3 Teenagers benefit from insulin pump therapy for the following reason. A. Can increase insulin rate to cover for alcohol intake. B. Decreased risk of glucose emergencies C. Greater dependence on parents D. Match insulin to hormone swings
Toddlers benefit Delayed blousing for fussy eaters Dosing precision 10ths or 20ths of a unit Reduced hypo risk Lockout features Teens Basal patterns for hormonal swings Historical data records/ downloading / app sharing Easy snack coverage Greater independence Technical coolness
Written Plan for Pump Use Blood glucose checks or CGM Checks Record keeping of BG, Carbs, insulin, activity and other issues Site-change guidelines Restart injections if needed When to check ketones and action to take Hypoglycemia and Hyperglycemia treatment guidelines
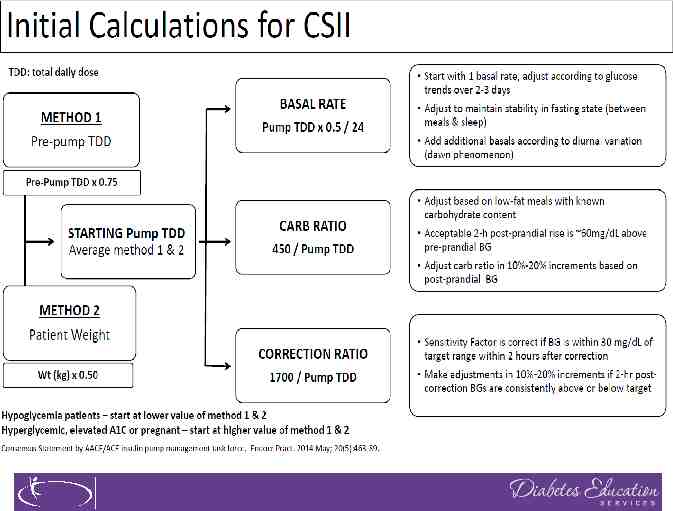
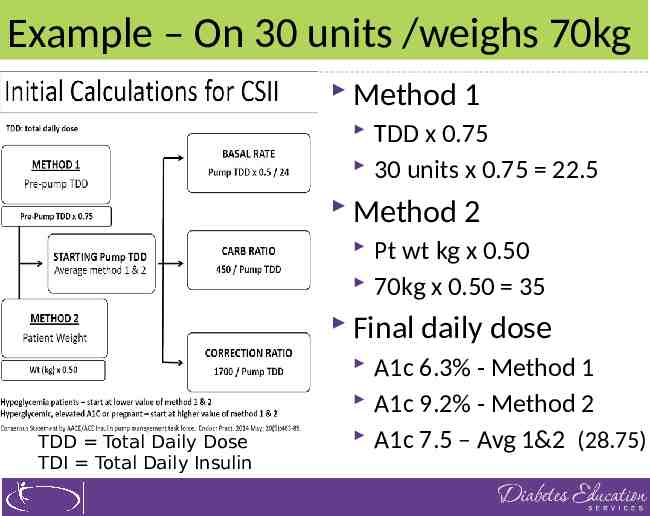
Example – On 30 units /weighs 70kg Method 1 TDD x 0.75 30 units x 0.75 22.5 Method 2 Pt wt kg x 0.50 70kg x 0.50 35 Final daily dose TDD Total Daily Dose TDI Total Daily Insulin A1c 6.3% - Method 1 A1c 9.2% - Method 2 A1c 7.5 – Avg 1&2 (28.75)
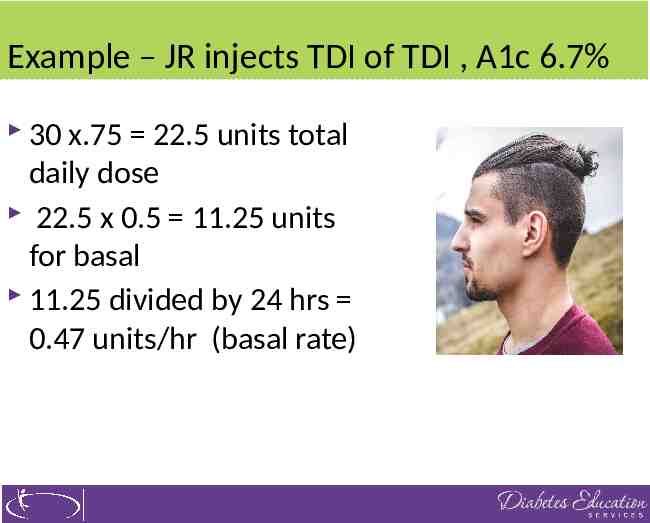
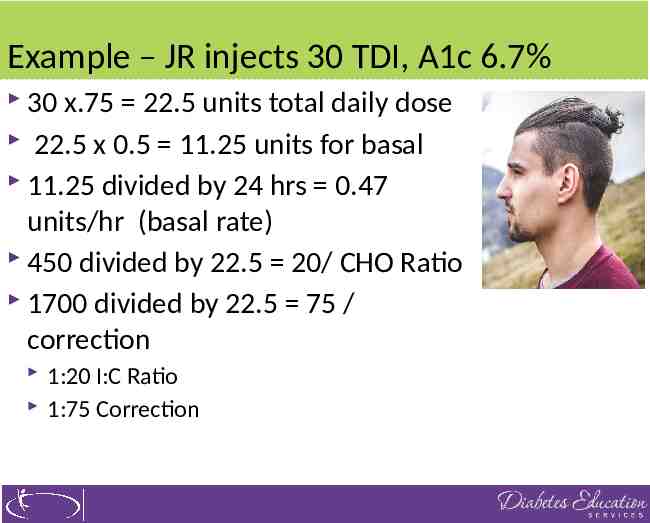
Example – JR injects TDI of TDI , A1c 6.7% 30 x.75 22.5 units total daily dose 22.5 x 0.5 11.25 units for basal 11.25 divided by 24 hrs 0.47 units/hr (basal rate)
Basal insulin Drip of rapid insulin very few minutes If basal rate is set correctly, stable BG between meals and hs Can skip delay meals Delivered auto on 24 hour cycle Temporary adjustments may include: lower basal insulin during exercise increase during sick days
Role of basal insulin in pumps Keep glucose steady On average, 5 different basal segments needed Basal insulin rate not correct Glucose rises or falls even when not eating Fasting glucose is elevated or low Correction bolus does not get glucose to target To prevent hypoglycemia, no coverage for snacks If person is eating to cover for in-between meal hypoglycemia
Basal Insulin Needs Dawn phenomena Higher needs from 3-7am for adults Kids from Midnight to 7am Basal rate can be adjusted to match sleep and work schedule Traveling – change clock in pump to match new time
Typical Basal Needs Gary Scheiner, MS, CDE
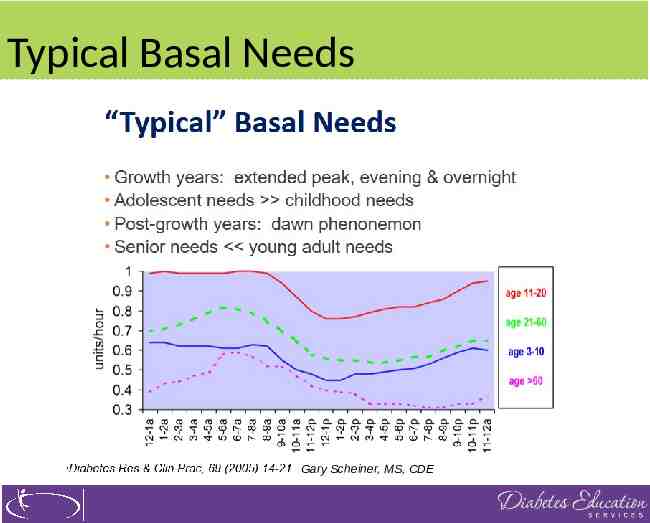
Basal Insulin Dosing – Beyond Basics Active, healthy 35-45% of total daily insulin Less active, lower carb intake 45-55% of total daily insulin Percentage may increase during puberty Tends to decrease with advanced age Sleep and growth patterns have major influence
Basal Rate Testing No food or bolus insulin for 4 hours prior No eating during test No calories, water and decaf diet drinks ok Avoid high-fat food immediately prior No alcohol for 12 hours prior In case of glucose 70, eat and stop test If glucose 250, stop test and bolus Maintain normal activity Avoid during illness, if taking steroids
Monitoring Basal Test Only use fingertip Check every 1-2 hours (daytime) Check every 2-3 hours (overnight) CGM to collect data very helpful Reliable data trends Can download or photograph 6-12 hour screen Adjust basal if rise or falls more than 30 points Double check no outside events
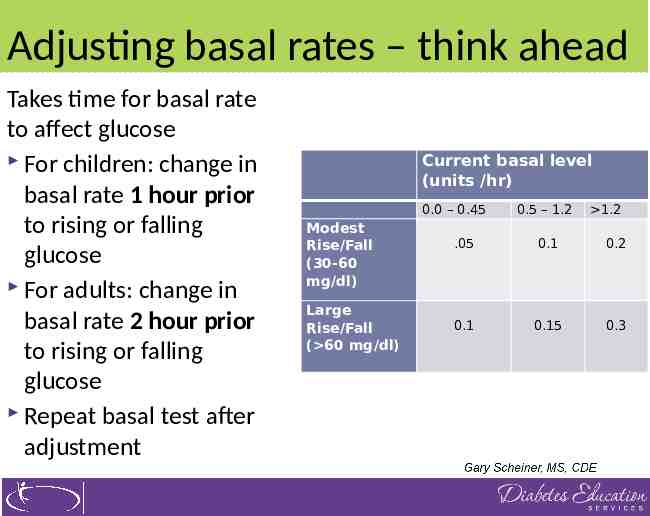
Adjusting basal rates – think ahead Takes time for basal rate to affect glucose For children: change in basal rate 1 hour prior to rising or falling glucose For adults: change in basal rate 2 hour prior to rising or falling glucose Repeat basal test after adjustment Current basal level (units /hr) 0.0 – 0.45 Modest Rise/Fall (30-60 mg/dl) Large Rise/Fall ( 60 mg/dl) 0.5 – 1.2 1.2 .05 0.1 0.2 0.1 0.15 0.3
Problem solving If basal or bolus is more than 65%, usually indicates need to recalculate Prevent missed boluses 1 missed meal bolus over a month raises A1c 0.5% Get in habit of pre-blousing Use reminder alerts on pumps
Bolus Rates - Same for each meal to start Bolus rates CHO Ratio Start with 1:15 or 450 divided by TDD I:C Ratio Correction/sensitivity 1700 divided by TDD Target Range: 95-140 mg/dl Active insulin/insulin On Board 3-6 hours
Example – JR injects 30 TDI, A1c 6.7% 30 x.75 22.5 units total daily dose 22.5 x 0.5 11.25 units for basal 11.25 divided by 24 hrs 0.47 units/hr (basal rate) 450 divided by 22.5 20/ CHO Ratio
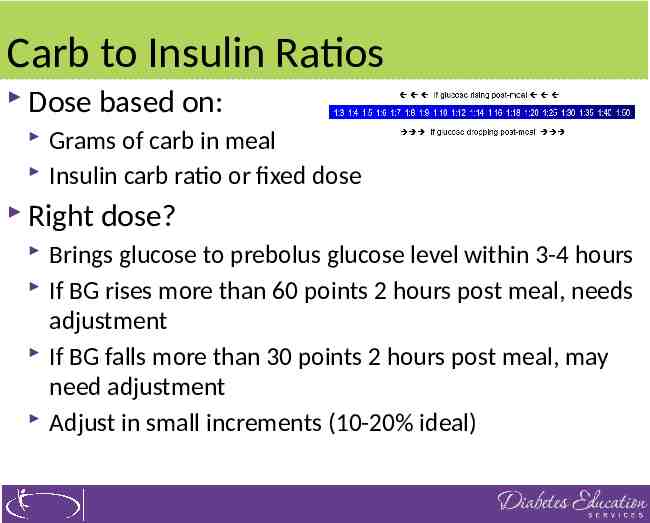
Carb to Insulin Ratios Dose based on: Grams of carb in meal Insulin carb ratio or fixed dose Right dose? Brings glucose to prebolus glucose level within 3-4 hours If BG rises more than 60 points 2 hours post meal, needs adjustment If BG falls more than 30 points 2 hours post meal, may need adjustment Adjust in small increments (10-20% ideal)
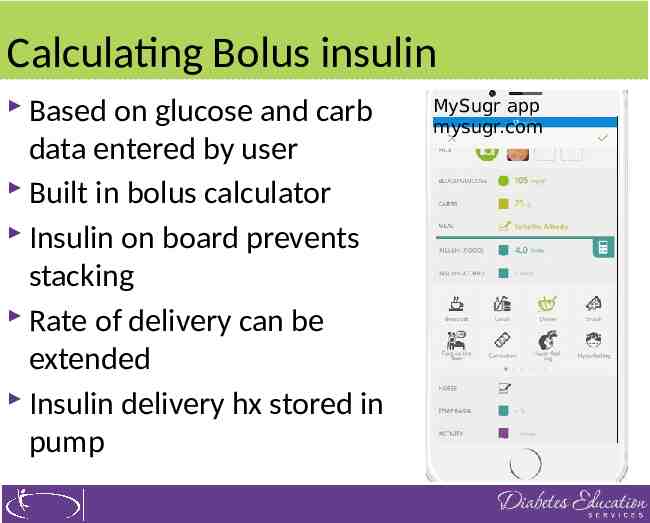
Calculating Bolus insulin Based on glucose and carb data entered by user Built in bolus calculator Insulin on board prevents stacking Rate of delivery can be extended Insulin delivery hx stored in pump MySugr app mysugr.com
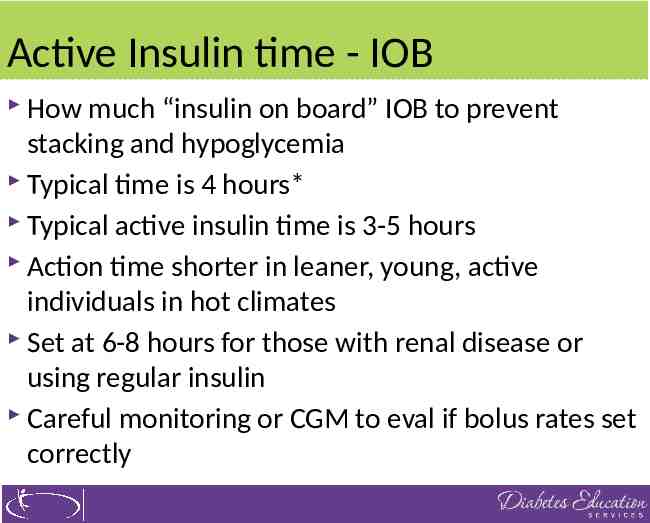
Active Insulin time - IOB How much “insulin on board” IOB to prevent stacking and hypoglycemia Typical time is 4 hours* Typical active insulin time is 3-5 hours Action time shorter in leaner, young, active individuals in hot climates Set at 6-8 hours for those with renal disease or using regular insulin Careful monitoring or CGM to eval if bolus rates set correctly
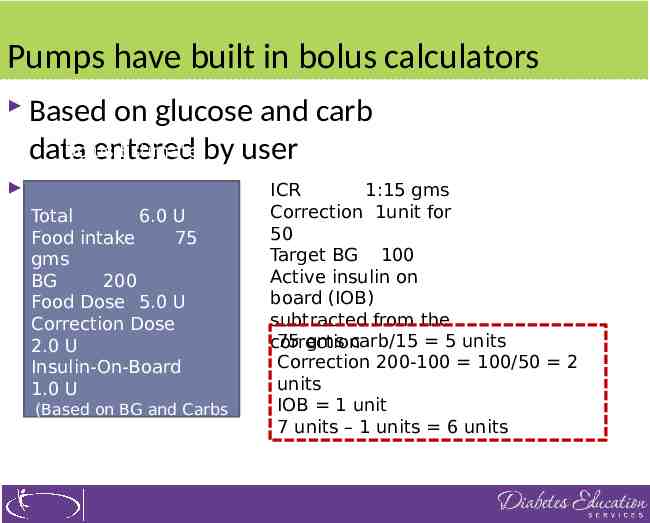
Pumps have built in bolus calculators Based on glucose and carb Bolus Estimate by user data entered Details Total 6.0 U Food intake 75 gms BG 200 Food Dose 5.0 U Correction Dose 2.0 U Insulin-On-Board 1.0 U (Based on BG and Carbs entered by user.) ICR 1:15 gms Correction 1unit for 50 Target BG 100 Active insulin on board (IOB) subtracted from the 75 gms carb/15 5 units correction Correction 200-100 100/50 2 units IOB 1 unit 7 units – 1 units 6 units
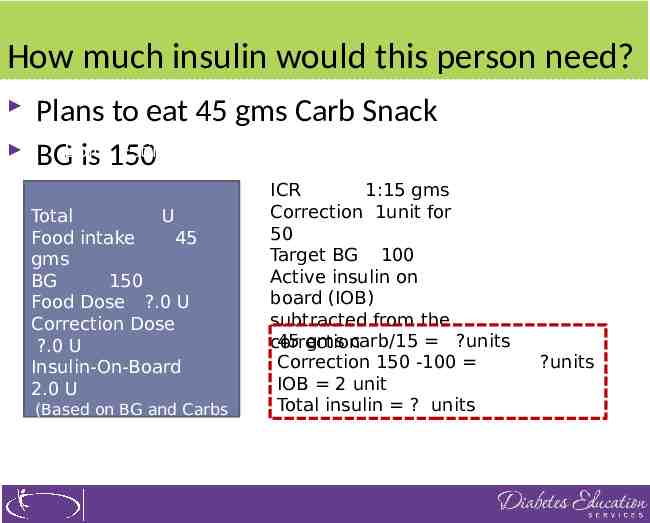
How much insulin would this person need? Plans to eat 45 gms Carb Snack Estimate BGBolus isDetails 150 Total U Food intake 45 gms BG 150 Food Dose ?.0 U Correction Dose ?.0 U Insulin-On-Board 2.0 U (Based on BG and Carbs entered by user.) ICR 1:15 gms Correction 1unit for 50 Target BG 100 Active insulin on board (IOB) subtracted from the 45 gms carb/15 ?units correction Correction 150 -100 IOB 2 unit Total insulin ? units ?units
Poll Question 4 For case study, how much insulin? A. 3 units B. 2 units C. 4 units D. Determine activity first
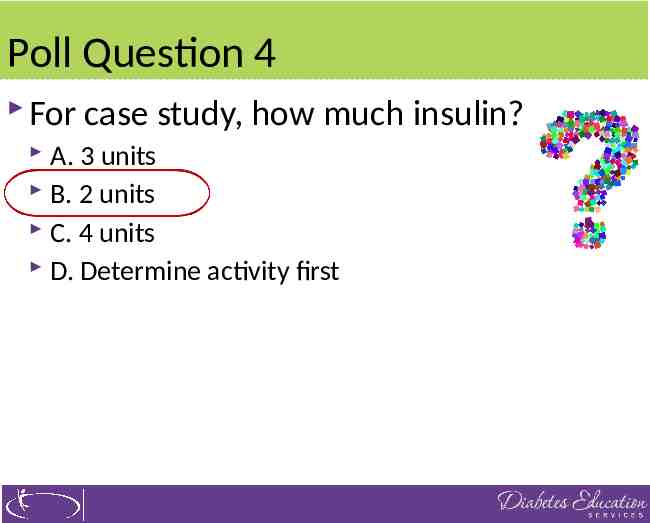
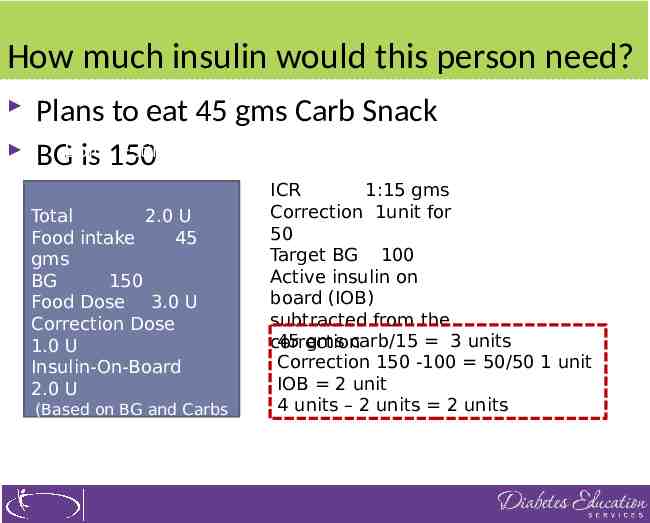
How much insulin would this person need? Plans to eat 45 gms Carb Snack Estimate BGBolus isDetails 150 Total 2.0 U Food intake 45 gms BG 150 Food Dose 3.0 U Correction Dose 1.0 U Insulin-On-Board 2.0 U (Based on BG and Carbs entered by user.) ICR 1:15 gms Correction 1unit for 50 Target BG 100 Active insulin on board (IOB) subtracted from the 45 gms carb/15 3 units correction Correction 150 -100 50/50 1 unit IOB 2 unit 4 units – 2 units 2 units
Not using insulin bolus ratios? Fixed dosing Take half of total daily dose, reduce by 25% and divide by number of meals to get fixed dose per meal Calculate insulin sensitivity correction factor 1700 by total daily insulin No target – choose acceptable target
Advanced Pump Features Prolonged bolus for Gastroparesis, amylin, GLP-1 Receptor Agonists Advanced Basal Features Temporary basal rates Secondary, tertiary programs Custom alerts Data downloads
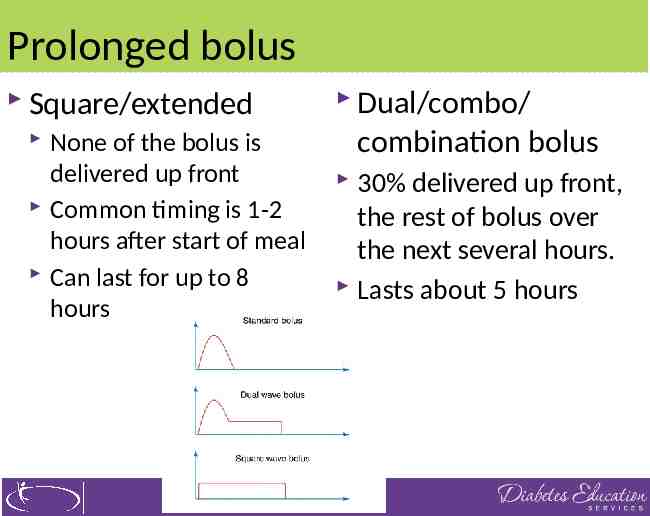
Prolonged bolus Standard bolus Delivered within a few minutes Peaks in one hour Lasts for four hours Prolonged bolus Delivered over a couple of hours Peak delay Duration extended Purpose Match insulin to absorption of food Works well with slowly digested food Applications Large portions Slow consumption Gastroparesis Use of incretin mimetics
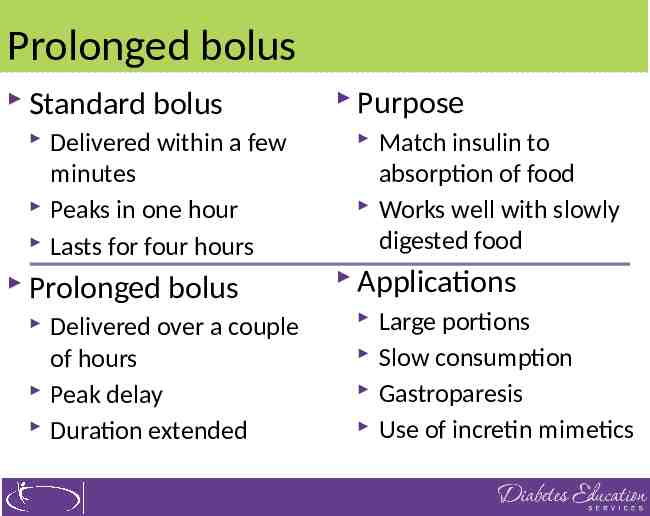
Prolonged bolus Square/extended None of the bolus is delivered up front Common timing is 1-2 hours after start of meal Can last for up to 8 hours Dual/combo/ combination bolus 30% delivered up front, the rest of bolus over the next several hours. Lasts about 5 hours
Insulin coverage for protein? Most of time, protein won’t affect glucose If person on low carb diet, protein may start impacting blood glucose levels Bolus for 50% of protein grams If large protein portion (more than 50g) extended bolus for additional 20-30gs of carb
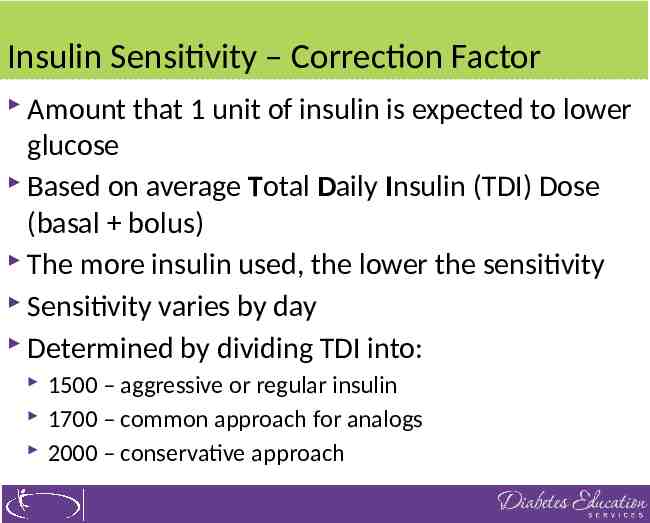
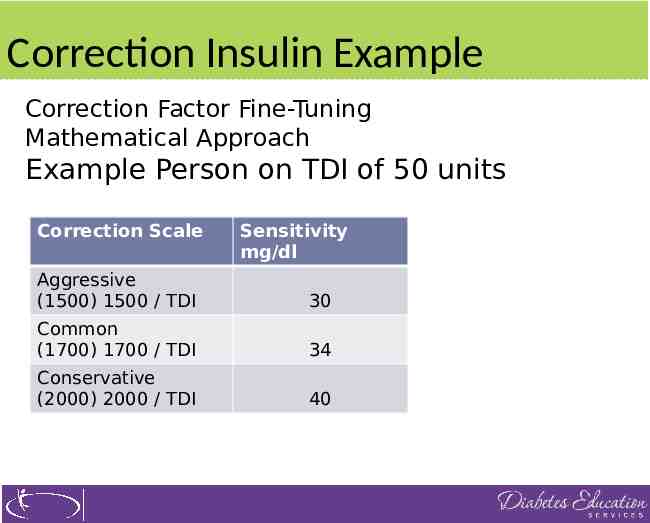
Insulin Sensitivity – Correction Factor Amount that 1 unit of insulin is expected to lower glucose Based on average Total Daily Insulin (TDI) Dose (basal bolus) The more insulin used, the lower the sensitivity Sensitivity varies by day Determined by dividing TDI into: 1500 – aggressive or regular insulin 1700 – common approach for analogs 2000 – conservative approach
Correction Insulin Example Correction Factor Fine-Tuning Mathematical Approach Example Person on TDI of 50 units Correction Scale Sensitivity mg/dl Aggressive (1500) 1500 / TDI 30 Common (1700) 1700 / TDI 34 Conservative (2000) 2000 / TDI 40
Example – JR injects 30 TDI, A1c 6.7% 30 x.75 22.5 units total daily dose 22.5 x 0.5 11.25 units for basal 11.25 divided by 24 hrs 0.47 units/hr (basal rate) 450 divided by 22.5 20/ CHO Ratio 1700 divided by 22.5 75 / correction 1:20 I:C Ratio 1:75 Correction
Transition from MDI to pump Best in am, not travel, outpatient setting okay Wean person off injections NPH, hold am dose Glargine, detemir- take day before, if evening hold is best. Degludec – take ½ usual dose day before if am, if evening, omit.
Safety guidelines Review signs and treatment of hypo Do not suspend pump when low, unless no treatment available Diabetes Ketoacidosis Those with negative c-peptide at higher risk Insulin pump interruption for 2-3 hours can lead to DKA Provide education to prevent, detect and reverse
Poll Question 4A AL is on an insulin pump. Her BG at 10am is 108, at 11am, 219 and noon 298. She has not eaten anything since breakfast. What is best action? A. Program insulin pump to deliver 3 units bolus stat B. Increase basal rate starting at 8am C. Go to emergency room D. Check for ketones
Disconnecting from Pump BG rises about 1 mg/dl a minute when disconnected Avoid extended disconnection since can lead to ketones and hyperglycemia Strategies Short term disconnection 1 hour Bolus to replace missed basal insulin Long term 1 hour and bolus missed basal insulin hourly Protective caps usually not necessary
Prevent DKA and Hyperglycemia Eval sites for malabsorption, make sure to change site and infusion sets every 2-3 days Protect insulin from overheating Tubing or infusion set clogs – change site Check for leaks, smell for insulin, use angled sets Make sure to purge air bubbles before priming tube Inspect daily for dislodgement Priming insulin tubing when changing infusion set Extended pump suspension or disconnect (limit to one hour, carry syringes at all times)
Hospital Stay for Pumpers Staff need to assess: How long using pump? Who adjusts pump settings? What type of insulin is used? How much insulin is in pump now? When is next site change? Who does it? Basal rates? I:C ratios? Correction? Have your supplies? When usually check BG or CGM?
Hospital Stay - Need orders Backup plan in case pump can’t be used Don’t stop pump without administering rapid insulin first (or IV insulin). Designate surrogate programmer(s) Specify frequency and carb count for meals/snacks Keep pump and programmer outside room during MRI, CT Scan, Xray. Remove infusion set and sensor for MRI Don’t aim Echo/US transducer at pump
Pumpers Responsibility in Hospital Provide own pump (and sensor) supplies Change pump reservoirs and infusion sets Provide staff with SMBG and insulin doses Notify staff of adjustments to standard doses Respond to alarms
Backup Plan if pump isn’t working Immediate basal insulin injection Mealtime rapid insulin injection Keep written log of I:C ratios, correction and meal boluses Keep log of off-pump activity Resume pump when basal insulin wears off
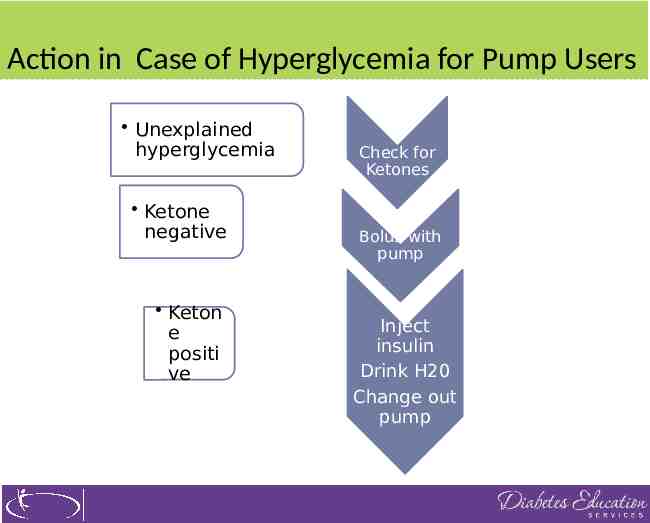
Action in Case of Hyperglycemia for Pump Users Unexplained hyperglycemia Ketone negative Keton e positi ve Check for Ketones Bolus with pump Inject insulin Drink H20 Change out pump
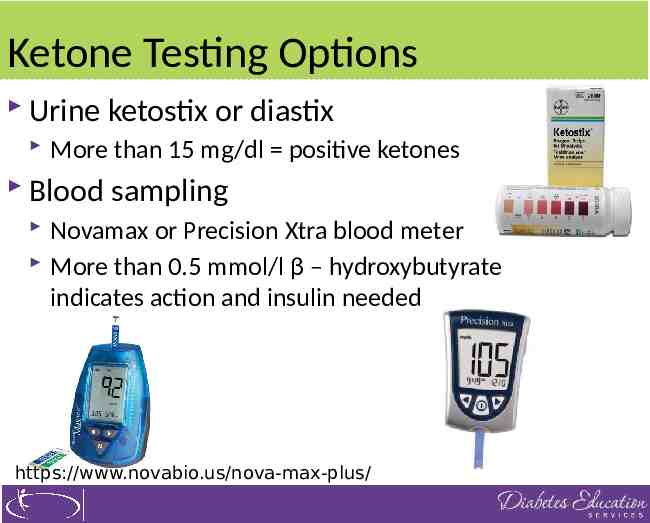
Ketone Testing Options Urine ketostix or diastix More than 15 mg/dl positive ketones Blood sampling Novamax or Precision Xtra blood meter More than 0.5 mmol/l β – hydroxybutyrate indicates action and insulin needed https://www.novabio.us/nova-max-plus/
When to contact clinical staff Severe or repeated hypo Ketosis Signs of infection Call pump company if technical difficulties See pt in 1-2 weeks, download device, troubleshooting At 3-4 weeks review more advanced features
Thank You Please email us with any questions. [email protected] www.diabetesed.net