Designing & Delivering Whole-Person Transitional Care The Hospital
32 Slides845.86 KB
Designing & Delivering Whole-Person Transitional Care The Hospital Guide to Reducing Medicaid Readmissions Webinar 6: Enhance Services for High-Risk Patients
Agenda Describe strategies to enhance services for high-risk patients Give examples of how transitional care services and high utilizer programs effectively meet “whole-person needs” Describe the usefulness of an emerging tool: the ED Care Plan Identify ways to reduce readmissions from the ED
Objectives Enhanced services go beyond standard care to provide services and support in the post-hospital time period Adapt transitional care models to address “whole-person needs” Develop new services to improve care for frequently hospitalized patients Use care plans to improve care over time and across settings Engage the ED in efforts to reduce readmissions
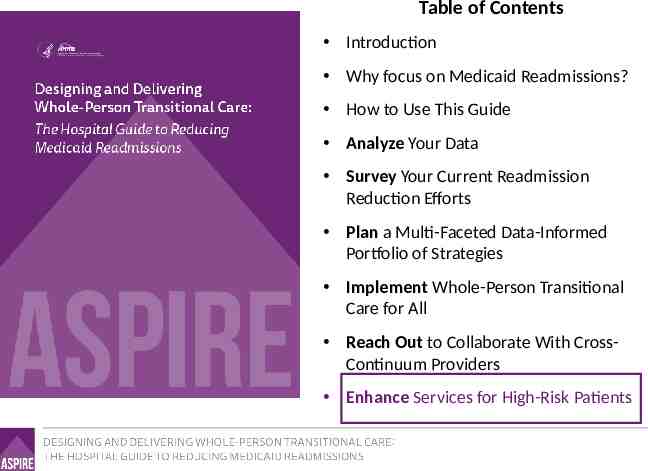
Table of Contents Introduction Why focus on Medicaid Readmissions? How to Use This Guide Analyze Your Data Survey Your Current Readmission Reduction Efforts Plan a Multi-Faceted Data-Informed Portfolio of Strategies Implement Whole-Person Transitional Care for All Reach Out to Collaborate With CrossContinuum Providers Enhance Services for High-Risk Patients
List of Tools The guide comes with 13 customizable tools to be used in hospital teams’ day-to-day operations. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Data Analysis Readmission Review Hospital Inventory Community Inventory Portfolio Design Operational Dashboard Portfolio Presentation Conditions of Participation Handout Whole-Person Transitional Care Planning Discharge Process Checklist Community Resource Guide Cross Continuum Collaboration ED Care Plan Examples
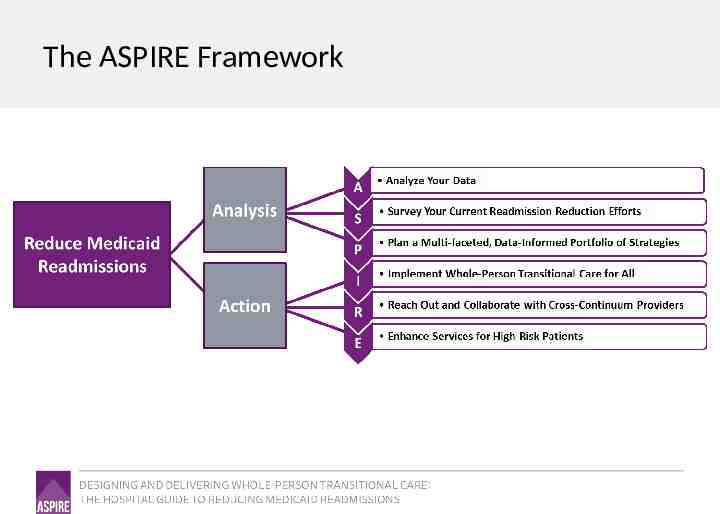
The ASPIRE Framework
“I think that there’s always going to be a group of folks that’s always going to need somebody to help them. That’s never going to change.”
Enhanced Services Additional services and supports in the time following hospitalization; Services not provided to all patients as part of routine care; Offered to subgroups identified as “high risk” of readmission; Delivered prior to and after discharge, often for 30 days; Deployed at provider expense so as to reduce readmissions; Delivered by hospital staff or by contracted staff from other entities
High Risk Target Populations There may be several target populations at high risk of readmission identified by your data analyses Consider the following high risk target populations: – – – – Adults with sickle cell disease; Adults residing in group homes or other residential settings; Patients discharged to short term skilled nursing facilities; Adults with a personal history of repeated hospitalizations in the past year One “standard” transitional care model would not likely meet the needs and address the root causes of readmissions for all these populations Design “enhanced services” to meet the needs of each target population
Transitional Care for High-Risk Patients
Transitional Care Services “Our [navigators] are flexible, proactive, and persistent; they address all needs. Each of them has incredible interpersonal skills.”
“Whole-Person” Adaptations to Transitional Care Navigating Hand-holding Arranging for . Providing with . Harm reduction Meet “where they are” Patient priorities first Relationship-based
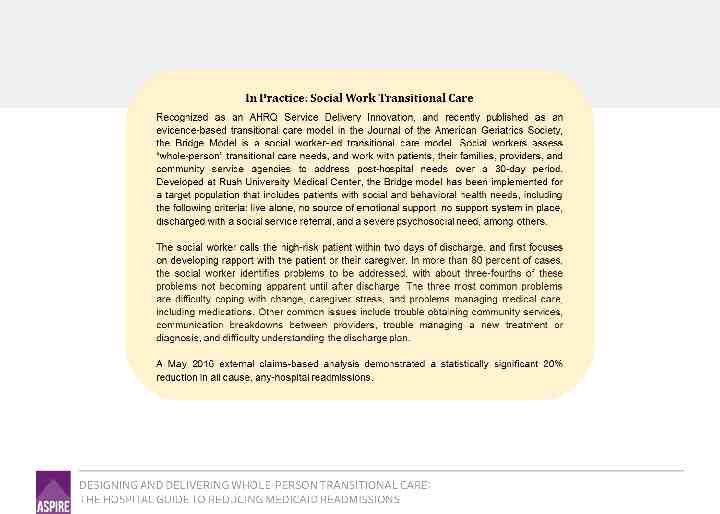
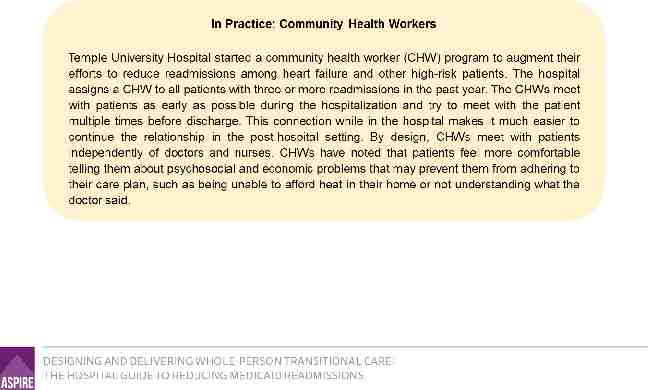
Social Work-based Transitional Care “Bridge model” Engage with patients with clinical, behavioral health and social needs Assess for transitional care needs Expect needs will change over time Use motivational interviewing Identify services in place Assess eligibility for services Discuss finances in context of needs and priorities Link directly to services Brief short term therapeutic support Coordinate with clinical and social service providers
Improving Care for High Utilizers
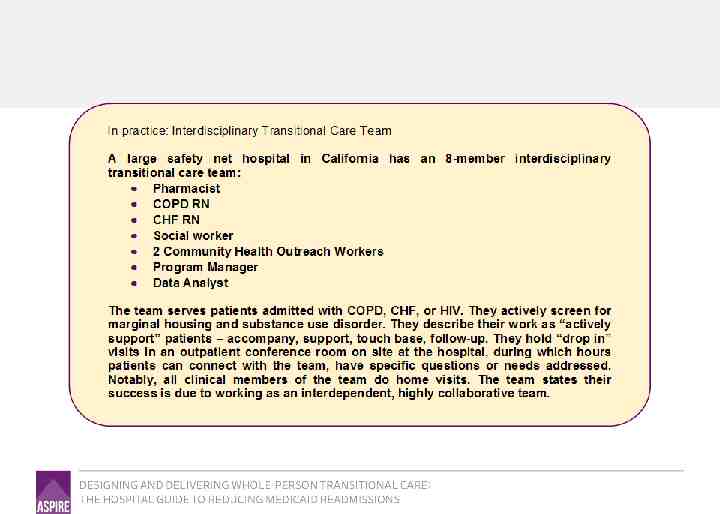
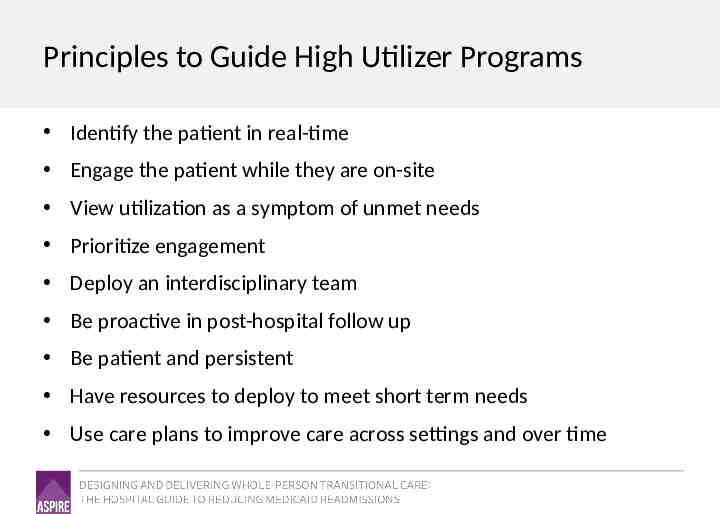
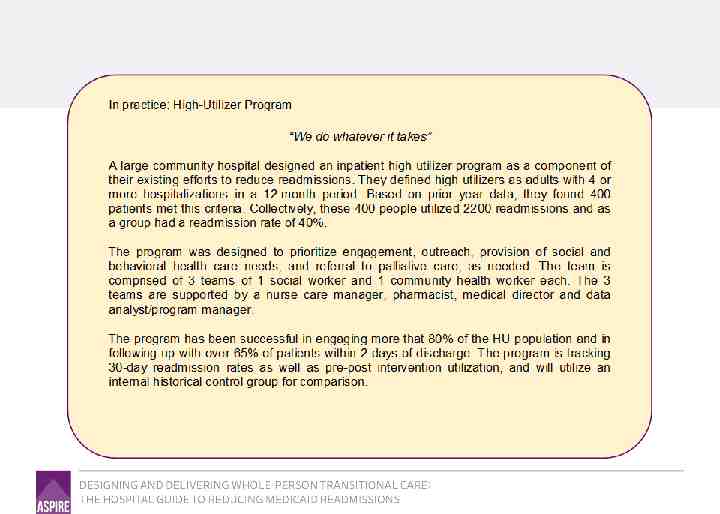
Principles to Guide High Utilizer Programs Identify the patient in real-time Engage the patient while they are on-site View utilization as a symptom of unmet needs Prioritize engagement Deploy an interdisciplinary team Be proactive in post-hospital follow up Be patient and persistent Have resources to deploy to meet short term needs Use care plans to improve care across settings and over time
Using Care Plans to Improve Care Over Time and Across Settings
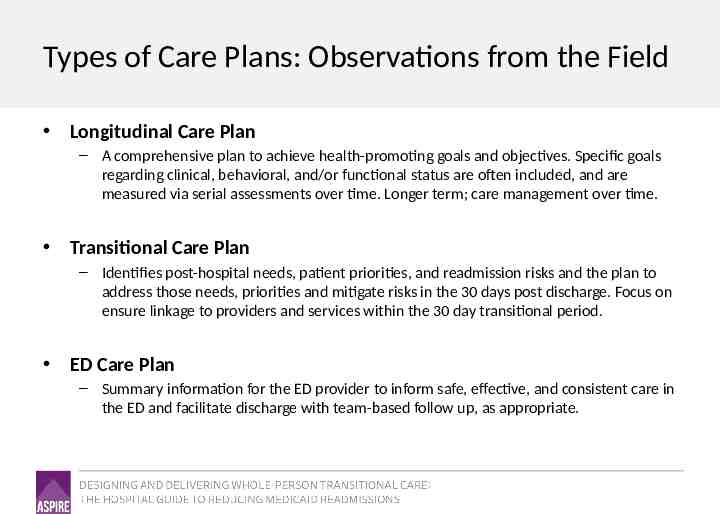
Types of Care Plans: Observations from the Field Longitudinal Care Plan – A comprehensive plan to achieve health-promoting goals and objectives. Specific goals regarding clinical, behavioral, and/or functional status are often included, and are measured via serial assessments over time. Longer term; care management over time. Transitional Care Plan – Identifies post-hospital needs, patient priorities, and readmission risks and the plan to address those needs, priorities and mitigate risks in the 30 days post discharge. Focus on ensure linkage to providers and services within the 30 day transitional period. ED Care Plan – Summary information for the ED provider to inform safe, effective, and consistent care in the ED and facilitate discharge with team-based follow up, as appropriate.
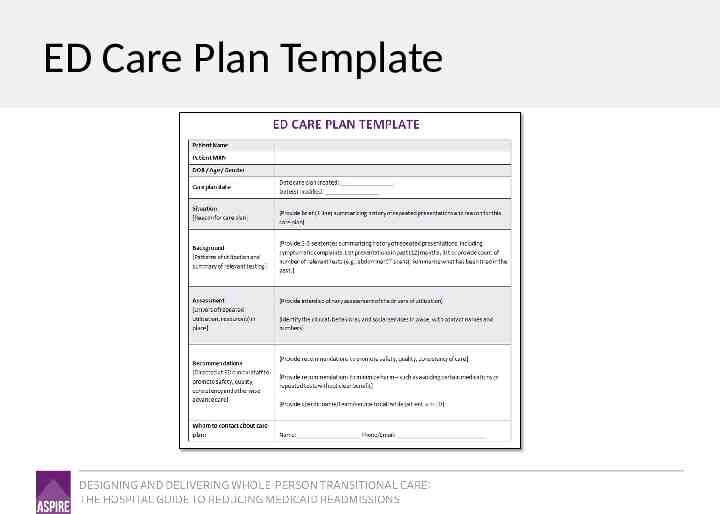
ED Care Plan: Emerging Tool in the Field Purpose: Improve the management of the high-risk patient the next time they come to the ED Audience: ED clinical staff Content: Executive summary of prior utilization and testing; Identification of the driver of hospital utilization; Recommendations for consideration Identification of a point of contact
ED Care Plan Template
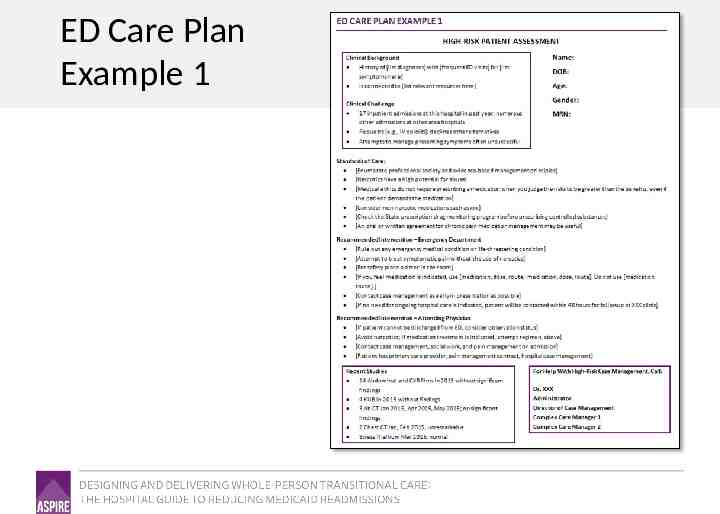
ED Care Plan Example 1
ED Care Plans: Lessons from the Field Brevity: No more than 1 page; the essential summary information in a way that saves time and promotes quality, informed decision making. Audience: Who is your intended audience? ED doc? Develop the “clinical snapshot” and recommended interventions with the end-user in mind. Summarize the “utilization” part of “high utilizer:” This summary is not just a clinical summary, but a utilization profile. Quantify prior visits, admissions, tests, consults to convey what has been done in the past. Delegate the synthesis, collaborate on the plan: Delegate the drafting of the care plan summary to a member of the high-risk care team. Meet as a team to develop recommendations and next steps.
Engage the ED in Reducing Readmissions
“In previous times, the path would’ve been to simply admit the patient, and we’ll sort it out 5 days later. We’re becoming more accustomed to having resources in the ER to help us discharge patients from the ED. That’s a culture change.”
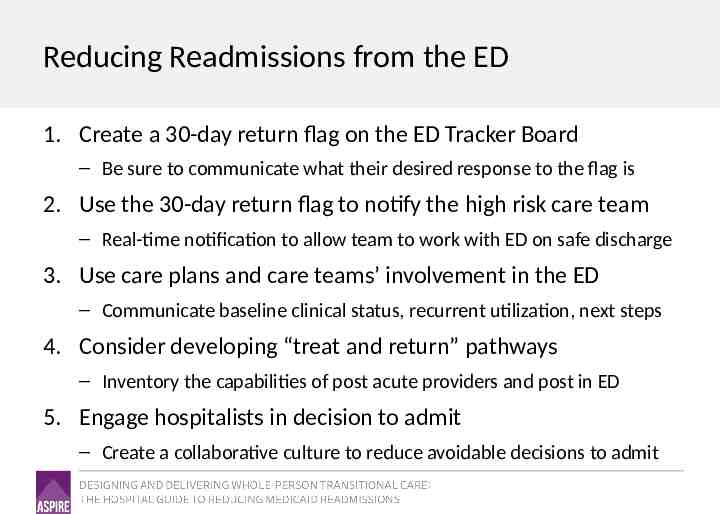
Reducing Readmissions from the ED 1. Create a 30-day return flag on the ED Tracker Board – Be sure to communicate what their desired response to the flag is 2. Use the 30-day return flag to notify the high risk care team – Real-time notification to allow team to work with ED on safe discharge 3. Use care plans and care teams’ involvement in the ED – Communicate baseline clinical status, recurrent utilization, next steps 4. Consider developing “treat and return” pathways – Inventory the capabilities of post acute providers and post in ED 5. Engage hospitalists in decision to admit – Create a collaborative culture to reduce avoidable decisions to admit
Summary Deploy enhanced services for patients at high risk of readmission Match the enhanced services to the needs of the high risk patient population; consider different services for different populations Do not over-medicalize services Develop care plans for patients who are frequently hospitalized Engage the ED in your efforts to reduce readmissions
Thank you for your commitment to reducing readmissions Amy E. Boutwell, MD, MPP Collaborative Healthcare Strategies Angel Bourgoin, PhD & Jim Maxwell, PhD John Snow, Inc. [email protected] Angel [email protected]; Jim [email protected]