Controlling Healthcare Costs through Accountable Care Organizations
95 Slides7.78 MB
Controlling Healthcare Costs through Accountable Care Organizations By: Robert James Cimasi, MHA, ASA, FRICS, MCBA, AVA, CM&AA President HEALTH CAPITAL CONSULTANTS HEALTH CAPITAL CONSULTANTS 1
INTRODUCTION TO ACOs HEALTH CAPITAL CONSULTANTS 2
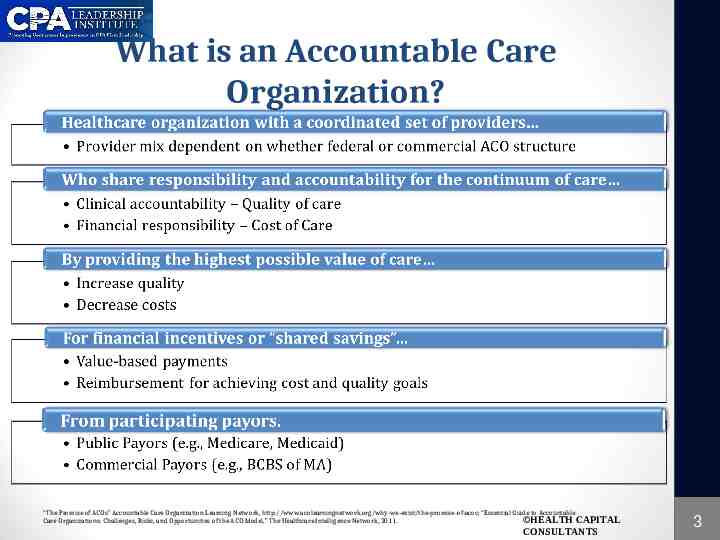
What is an Accountable Care Organization? “The Promise of ACOs” Accountable Care Organization Learning Network, http://www.acolearningnetwork.org/why-we-exist/the-promise-of-acos; “Essential Guide to Accountable Care Organizations: Challenges, Risks, and Opportunities of the ACO Model,” The Healthcare Intelligence Network, 2011. HEALTH CAPITAL CONSULTANTS 3

Key Principles and Elements of ACOs “AC0 Model Principles,” The Accountable Care Organization Learning Network, http://www.acolearningnetwork.org/why-we-exist/aco-model-principles (Accessed 09/16/2011) HEALTH CAPITAL CONSULTANTS 4

Why Accountable Care? National Health Expenditures per Capita, 1960-2009 Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group, at http://www.cms.hhs.gov/NationalHealthExpendData/ (see Historical; NHE summary including share of GDP, CY 1960-2009; file nhegdp09.zip). HEALTH CAPITAL CONSULTANTS 5
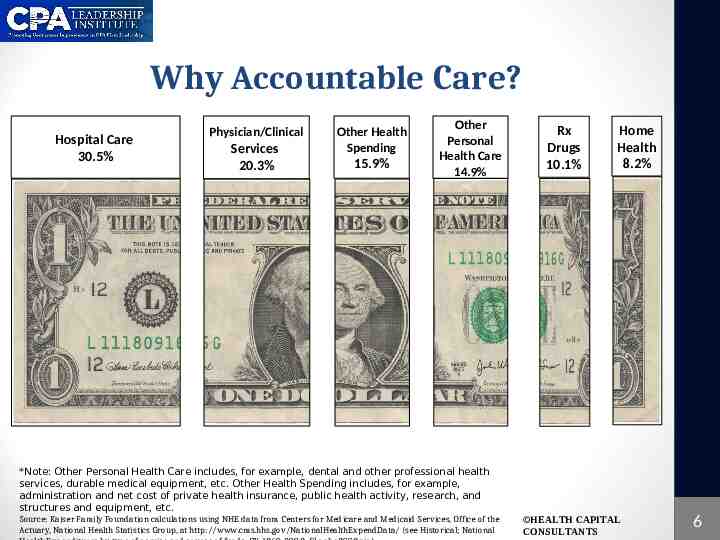
Why Accountable Care? Hospital Care 30.5% Physician/Clinical Services 20.3% Other Health Spending 15.9% Other Personal Health Care 14.9% Rx Drugs 10.1% Home Health 8.2% *Note: Other Personal Health Care includes, for example, dental and other professional health services, durable medical equipment, etc. Other Health Spending includes, for example, administration and net cost of private health insurance, public health activity, research, and structures and equipment, etc. Source: Kaiser Family Foundation calculations using NHE data from Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group, at http://www.cms.hhs.gov/NationalHealthExpendData/ (see Historical; National HEALTH CAPITAL CONSULTANTS 6
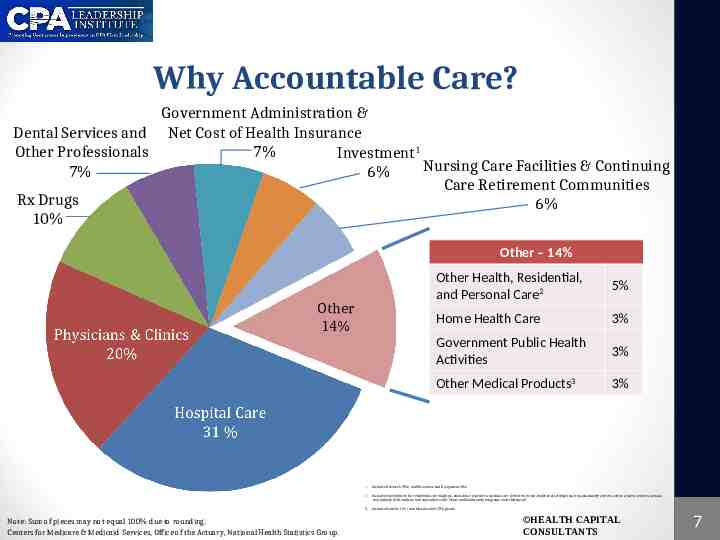
Why Accountable Care? Government Administration & Dental Services and Net Cost of Health Insurance 7% Other Professionals Investment1 Nursing Care Facilities & Continuing 7% 6% Care Retirement Communities Rx Drugs 6% 10% Other – 14% Other 14% Note: Sum of pieces may not equal 100% due to rounding. Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. Other Health, Residential, and Personal Care2 5% Home Health Care 3% Government Public Health Activities 3% Other Medical Products3 3% 1. Includes Research (2%) and Structures and Equipment (4%) 2. Includes expenditures for residential care facilities, ambulance providers, medical care delivered in non-traditional settings (such as community centers, senior citizens centers, schools, and military field stations, and expenditures for Home and Community programs under Medicaid 3. Includes Durable (1%) and Non-durable (2%) goods HEALTH CAPITAL CONSULTANTS 7
THE PATH TO ACCOUNTABLE CARE HEALTH CAPITAL CONSULTANTS 8
The Path to Accountable Care “The only thing new in the world is the history you don’t know.” - Harry S. Truman “A Guide to Consulting Services for Emerging Healthcare Organizations,” By Robert James Cimasi, John Wiley & Sons, Inc., 1999, p. 12. HEALTH CAPITAL CONSULTANTS 9
The Path to Accountable Care Managed Care Managed care plans integrate the financing and provision of health services o Administered by one managed care organization (MCO) in an effort to contain costs Hold providers accountable for providing care to a population through: o Clinical practice standardization o Selective contracting o o o Low-cost settings Reduced discretionary hospital admissions Effective staff use “A Guide to Consulting Services for Emerging Healthcare Organizations,” By Robert James Cimasi, John Wiley & Sons, Inc., 1999, p. 12. HEALTH CAPITAL CONSULTANTS 10
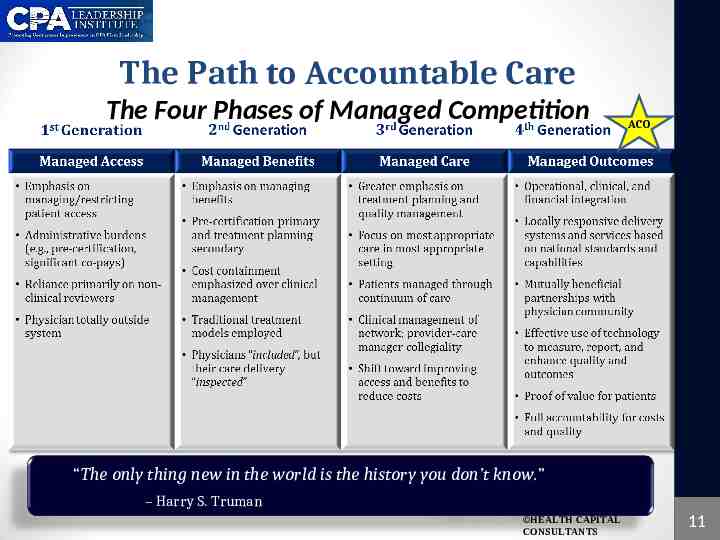
The Path to Accountable Care The Four Phases of Managed Competition ACO “The only thing new in the world is the history you don’t know.” – Harry S. Truman HEALTH CAPITAL CONSULTANTS 11

The Path to Accountable Care Accountable Care is Not a New Concept Accountable care was linked to better healthcare in 1932 when the Committee on the Costs of Medical Care suggested, among other things, that the focus of medical care should be on coordination of care to help lower costs. HEALTH CAPITAL CONSULTANTS 12
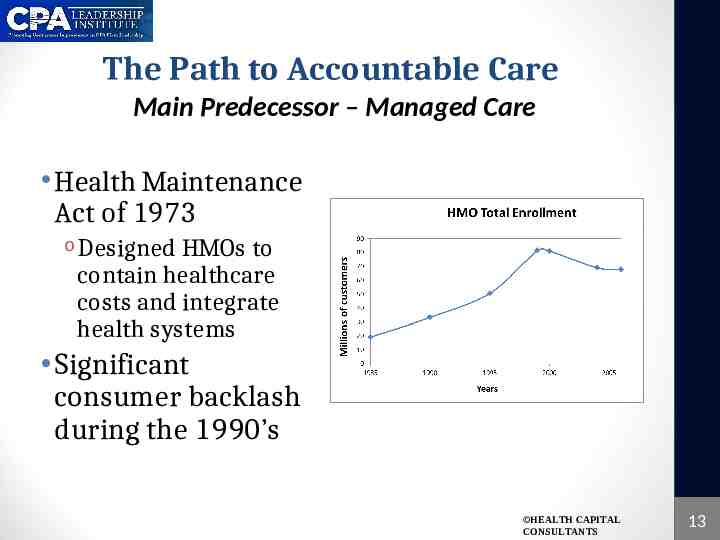
The Path to Accountable Care Main Predecessor – Managed Care Health Maintenance Act of 1973 o Designed HMOs to contain healthcare costs and integrate health systems Significant consumer backlash during the 1990’s HEALTH CAPITAL CONSULTANTS 13

The Path to Accountable Care An Evolved Form of Managed Competition Dominant theory of 1990’s healthcare reform Formalized by Alain Enthoven of Stanford University in 1993 Blends competitive and regulatory strategies Aims to achieve maximum value for both consumers and providers Definition of Managed Competition Competing healthcare entities, mainly payors, are monitored by a supervisory structure that established equitable rules, creates priceelastic demand, and avoids uncompensated risk selection “The History and Principals of Managed Competition” By Alain C. Enthoven, Health Affairs, Vol. 12, No. Supp. 1, 1993, p. 24. HEALTH CAPITAL CONSULTANTS 14
The Path to Accountable Care The Birth of a Term Medicare Physician Group Practice (PGP) Demonstration o Examined incentive-based payment methods o Initiated in 2005 o Took place over a 5 year period o Main Foundation for Medicare Shared Savings Program (MSSP), a/k/a, Federal ACOS Term ACO was coined in 2006 o Elliott Fisher, a physician and professor of medicine at Dartmouth Medical School o Glenn Hackbarth, the chairman of the Medicare Payment Advisory Commission (MedPAC) HEALTH CAPITAL CONSULTANTS 15

The Path to Accountable Care Enter Healthcare Reform March 23, 2010 The Patient Protection and Affordable Care Act (ACA) is Signed into Law A mere four pages introduces the next big movement in healthcare ACOs HEALTH CAPITAL CONSULTANTS 16
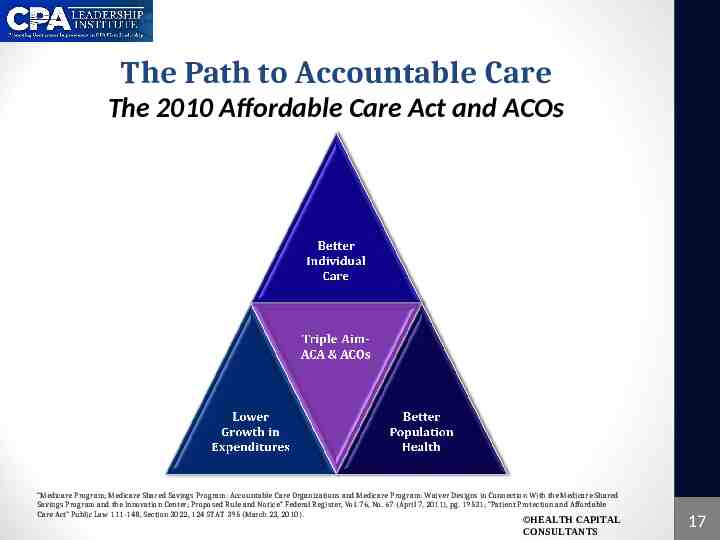
The Path to Accountable Care The 2010 Affordable Care Act and ACOs “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” Federal Register, Vol. 76, No. 67 (April 7, 2011), pg. 19531; “Patient Protection and Affordable Care Act” Public Law 111-148, Section 3022, 124 STAT 395 (March 23, 2010). HEALTH CAPITAL CONSULTANTS 17
Related ACA Provisions Value Based Purchasing (VBP) VBP refers to any concept that links payments to quality of care o Rewards providers for providing high quality, efficient clinical care The ACA establishes several VBP demonstration programs o Hospitals (§3001) o Home health agencies (§ 3006) o Ambulatory surgery centers (§ 10301) The MSSP is one form of value-based purchasing linking provider payments to efficient coordinated care of Medicare beneficiaries that meets standards set within CMS’s proposed rules “Patient Protection and Affordable Care Act” Public Law 111-148, Section 3021, 124 STAT 353, 372, 936 (March 23, 2010). “The Cost of Confusion: Healthcare Reform and Value Based Purchasing” By Trent Haywood, Healthcare Financial Management, Vol. 64, No. 10, October 2010. “CMS Releases Proposed Regulations Regarding Formation of Accountable Care Organizations” By Emily J. Cook and David L. Klatsky, McDermott Will & Emery, April 8, 2011, http://www.mwe.com/index.cfm/fuseaction/publications.nldetail/object id/3bf8ec04-7a4d-4a4e-8ffe-b4281889b282.cfm (Accessed 4/17/2011) HEALTH CAPITAL CONSULTANTS 18

Related ACA Provisions Other Payment Reforms Medical Home Model o Promotes team-based approach to care of a patient through a spectrum of disease states and across the various stages of life Bundling Demonstration Projects o A voluntary national pilot program on bundling payments to healthcare providers o Aim to provide incentives for providers to coordinate patient care across the continuum and to be jointly accountable for an entire episode of care Community Health Teams o ACA Section 3502 directs the Secretary to establish a program to provide grants to enter into contracts with eligible entities o Establish community based interdisciplinary, inter-professional teams (referred to in the statute as ‘‘health teams’’) to support primary care practices (including OBGYN practices, within the hospital service areas served by the eligible entities “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” Federal Register, Vol. 76, No. 67 (April 7, 2011), p. 19602. Affordable Care Act, Pub. L. No. 111-148, Section 3023 (March 23, 2011) HEALTH CAPITAL CONSULTANTS 19

CMS Final Rule For ACOs MEDICARE SHARED SAVINGS PROGRAM HEALTH CAPITAL CONSULTANTS 20

Medicare Shared Savings Program Overview and Intent Encourage ACO development for Medicare populations through a program that: “[P]romotes accountability for a patient population and coordinates items and services under parts A and B, and encourages investment in infrastructure and redesigned care processes for high quality and efficient service delivery.” “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), pg. 67804. “Patient Protection and Affordable Care Act” Public Law 111-148, Section 3022, 124 STAT 395 (March 23, 2010). “Patient Protection and Affordable Care Act” Public Law 111-148, Section 3022, 124 STAT 395 (March 23, 2010). HEALTH CAPITAL CONSULTANTS 21

Medicare Shared Savings Program ACO Requirements “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67807-08, 67814-16, 67821-22, 67825, 67827, 67829, 67891, 67980. HEALTH CAPITAL CONSULTANTS 22
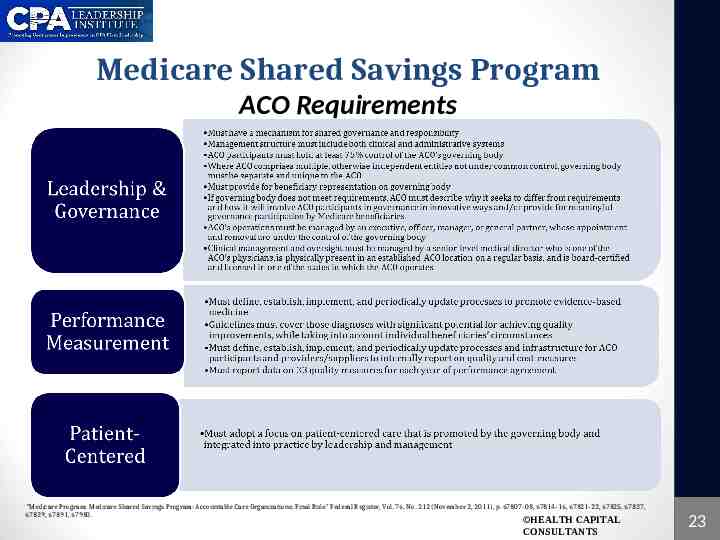
Medicare Shared Savings Program ACO Requirements “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67807-08, 67814-16, 67821-22, 67825, 67827, 67829, 67891, 67980. HEALTH CAPITAL CONSULTANTS 23
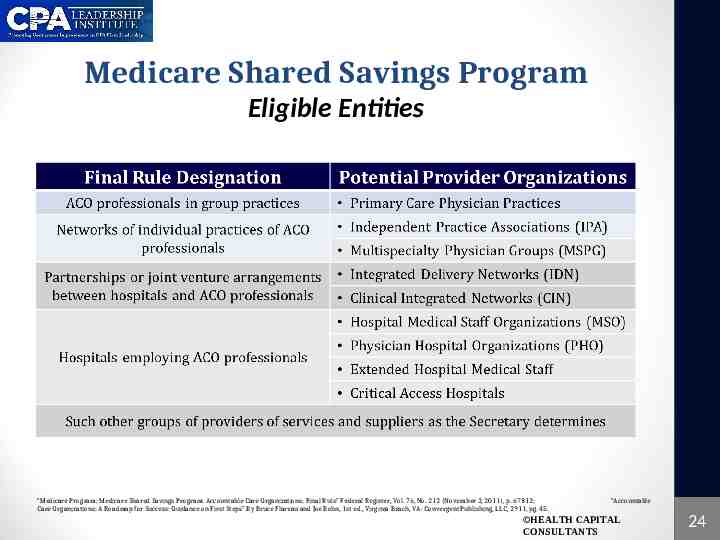
Medicare Shared Savings Program Eligible Entities “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67812; Care Organizations: A Roadmap for Success: Guidance on First Steps” By Bruce Flareau and Joe Bohn, 1st ed., Virginia Beach, VA: Convergent Publishing, LLC, 2911, pg. 45. “Accountable HEALTH CAPITAL CONSULTANTS 24

Medicare Shared Savings Program Becoming an ACO Potential ACOs Must Apply and Provide Documentation of Ability to Manage Population Health Application Must Include Documents Outlining: Agreements describing ACO participants’ rights and obligations in the ACO Organizational and management structure Information regarding all of the ACO participants Methods the ACO will use to achieve “patient centeredness,” including a description of the remedial processes and penalties for failure to comply Ways the ACO’s governing body will adhere to structural requirements, or a description of why the ACO seeks to differ from requirements Any other documents as requested “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67978. HEALTH CAPITAL CONSULTANTS 25
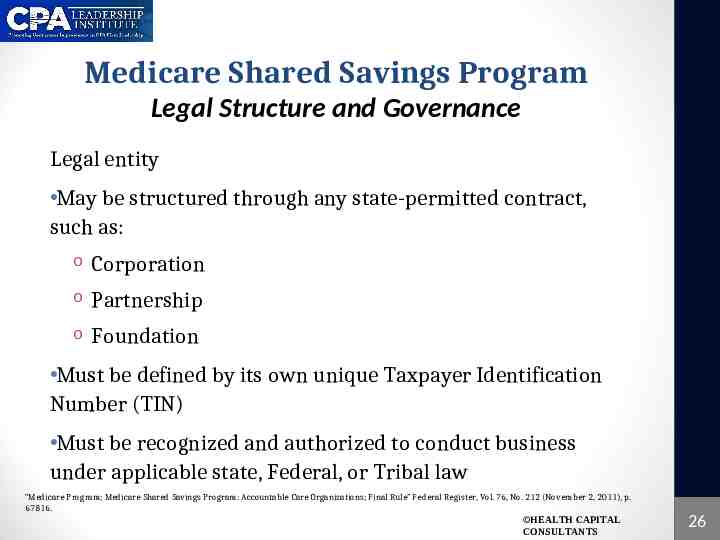
Medicare Shared Savings Program Legal Structure and Governance Legal entity May be structured through any state-permitted contract, such as: o Corporation o Partnership o Foundation Must be defined by its own unique Taxpayer Identification Number (TIN) Must be recognized and authorized to conduct business under applicable state, Federal, or Tribal law “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67816. HEALTH CAPITAL CONSULTANTS 26
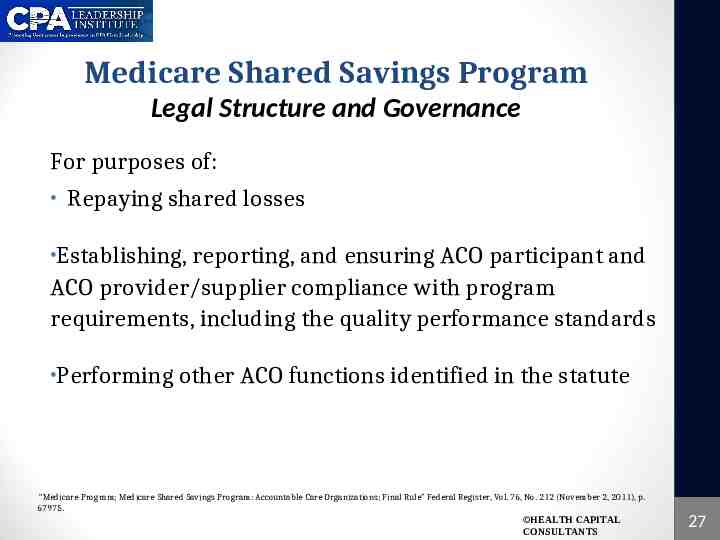
Medicare Shared Savings Program Legal Structure and Governance For purposes of: Repaying shared losses Establishing, reporting, and ensuring ACO participant and ACO provider/supplier compliance with program requirements, including the quality performance standards Performing other ACO functions identified in the statute “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67975. HEALTH CAPITAL CONSULTANTS 27
Medicare Shared Savings Program Leadership and Governance An “ACO shall have in place leadership and management structure that includes both clinical and administrative systems” “Mechanism for shared governance” o Organization must “maintain an identifiable governing body with authority to execute the functions of the ACO” o Governing body must be transparent and act in accordance with fiduciary duty to ACO o Responsible for strategic direction and oversight “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67975. HEALTH CAPITAL CONSULTANTS 28
Medicare Shared Savings Program Leadership and Governance Does not require a specific formation for the governing body ACO Medicare-enrolled TIN participants must control at least 75% of an ACO’s governing body Each individual ACO participant required to have “meaningful participation” in the governing body Must have Medicare beneficiary representation in the ACO governing body, with flexibility for “innovative” inclusion “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67818-67821. HEALTH CAPITAL CONSULTANTS 29

Medicare Shared Savings Program Leadership and Governance ACO’s operations o Managed by an executive, officer, manager, or general partner o Appointment and removal are under control of the organization’s governing body o Leadership team demonstrated ability to influence or direct clinical practice to improve efficiency processes and outcomes Clinical management and oversight Managed by a senior-level medical director who is one of the ACO’s physicians o Board-certified physician o Licensed in one of the states in which the ACO operates o Physically present at “any clinic, office, or other location participating in the ACO.” “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67823-67825. HEALTH CAPITAL CONSULTANTS 30

Medicare Shared Savings Program The ACO Agreement “ACO shall enter into an agreement with the Secretary to participate in the [Shared Savings Program] for not less than a 3-year period ” CMS will review applications and approve application from eligible organizations prior to end of calendar year ACO’s performance periods will begin on Jan. 1 of each respective year Extended agreement periods for ACOs beginning April 1, 2012 and July 1, 2012, of 21 and 18 months “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67835-67837. HEALTH CAPITAL CONSULTANTS 31
Medicare Shared Savings Program Assignment of Medicare Beneficiaries Based on utilization of primary care services provided by an “ACO professional”, which includes both physicians and non-physician practitioners Retroactively assigned to the ACO where a plurality of primary care services are received ACOs are responsible for any care received by the beneficiary, even if not received through the ACO o “Snowbirds” example “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67851, 67861-67870. HEALTH CAPITAL CONSULTANTS 32
Medicare Shared Savings Program Quality Reporting Requirements Must determine appropriate measures to assess the quality of care furnished by the ACO, including: o Measures of clinical processes and outcomes o Patient and caregiver experience of care o Utilization rates (e.g., admission for ambulatory sensitive conditions) Requires ACO participants to collect clinical and quality data and submit this information to CMS “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67870, 67891-67895. HEALTH CAPITAL CONSULTANTS 33

Medicare Shared Savings Program Quality Reporting Requirements 33 quality reporting criteria across 4 domains include: Domain 1. Patient/Caregiver Experience CMS Criteria Measures 1-7 2. Care coordination/Patient Safety Measures 8-13 3. Preventive Health Measures 14-21 4. At-Risk Population Measures 22-33 HEALTH CAPITAL “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67889-67890, 67897. CONSULTANTS 34
Medicare Shared Savings Program Payment Mechanism – Shared Savings ACOs to receive payment for shared Medicare savings provided it o Meets the quality performance requirements o Demonstrates that it has achieved savings against benchmark of expected average per capita Medicare FFS expenditures An ACO shall be eligible for payment of shared savings “[O]nly if the estimated average per capita Medicare expenditures under the ACO for Medicare FFS beneficiaries for Parts A and B services is at least the percent specified by the Secretary below the applicable benchmark.” ACOs receive bonuses for achieving resource use and quality targets over the course of a year ACOs face penalties for failing to meet these requirements The final rule sets out two risk models with various incentives for ACOs to receive shared savings payments “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule” Federal Register, Vol. 76, No. 212 (November 2, 2011), p. 67910, 67927-67930. HEALTH CAPITAL CONSULTANTS 35
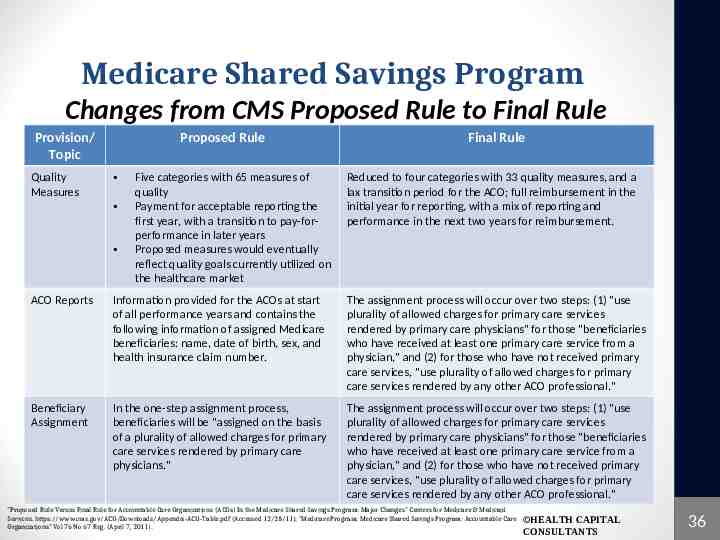
Medicare Shared Savings Program Changes from CMS Proposed Rule to Final Rule Provision/ Topic Quality Measures Proposed Rule Five categories with 65 measures of quality Payment for acceptable reporting the first year, with a transition to pay-forperformance in later years Proposed measures would eventually reflect quality goals currently utilized on the healthcare market Final Rule Reduced to four categories with 33 quality measures, and a lax transition period for the ACO; full reimbursement in the initial year for reporting, with a mix of reporting and performance in the next two years for reimbursement. ACO Reports Information provided for the ACOs at start of all performance years and contains the following information of assigned Medicare beneficiaries: name, date of birth, sex, and health insurance claim number. The assignment process will occur over two steps: (1) "use plurality of allowed charges for primary care services rendered by primary care physicians" for those "beneficiaries who have received at least one primary care service from a physician," and (2) for those who have not received primary care services, "use plurality of allowed charges for primary care services rendered by any other ACO professional." Beneficiary Assignment In the one-step assignment process, beneficiaries will be "assigned on the basis of a plurality of allowed charges for primary care services rendered by primary care physicians." The assignment process will occur over two steps: (1) "use plurality of allowed charges for primary care services rendered by primary care physicians" for those "beneficiaries who have received at least one primary care service from a physician," and (2) for those who have not received primary care services, "use plurality of allowed charges for primary care services rendered by any other ACO professional." "Proposed Rule Versus Final Rule for Accountable Care Organizations (ACOs) In the Medicare Shared Savings Program: Major Changes" Centers for Medicare & Medicaid Services. https://www.cms.gov/ACO/Downloads/Appendix-ACO-Table.pdf (Accessed 12/28/11); "Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations" Vol 76 No 67 Reg. (April 7, 2011). HEALTH CAPITAL CONSULTANTS 36
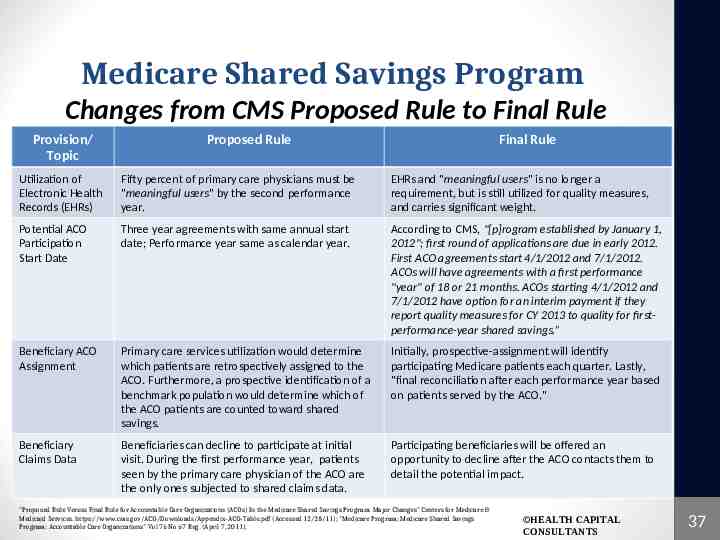
Medicare Shared Savings Program Changes from CMS Proposed Rule to Final Rule Provision/ Topic Proposed Rule Final Rule Utilization of Electronic Health Records (EHRs) Fifty percent of primary care physicians must be "meaningful users" by the second performance year. EHRs and "meaningful users" is no longer a requirement, but is still utilized for quality measures, and carries significant weight. Potential ACO Participation Start Date Three year agreements with same annual start date; Performance year same as calendar year. According to CMS, "[p]rogram established by January 1, 2012"; first round of applications are due in early 2012. First ACO agreements start 4/1/2012 and 7/1/2012. ACOs will have agreements with a first performance "year" of 18 or 21 months. ACOs starting 4/1/2012 and 7/1/2012 have option for an interim payment if they report quality measures for CY 2013 to quality for firstperformance-year shared savings.” Beneficiary ACO Assignment Primary care services utilization would determine which patients are retrospectively assigned to the ACO. Furthermore, a prospective identification of a benchmark population would determine which of the ACO patients are counted toward shared savings. Initially, prospective-assignment will identify participating Medicare patients each quarter. Lastly, "final reconciliation after each performance year based on patients served by the ACO." Beneficiary Claims Data Beneficiaries can decline to participate at initial visit. During the first performance year, patients seen by the primary care physician of the ACO are the only ones subjected to shared claims data. Participating beneficiaries will be offered an opportunity to decline after the ACO contacts them to detail the potential impact. "Proposed Rule Versus Final Rule for Accountable Care Organizations (ACOs) In the Medicare Shared Savings Program: Major Changes" Centers for Medicare & Medicaid Services. https://www.cms.gov/ACO/Downloads/Appendix-ACO-Table.pdf (Accessed 12/28/11); "Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations" Vol 76 No 67 Reg. (April 7, 2011). HEALTH CAPITAL CONSULTANTS 37

Medicare Shared Savings Program Changes from CMS Proposed Rule to Final Rule Provision/ Topic Proposed Rule Final Rule Track 1 and Conversion to Risk ACOs can choose from either Track 1 or Track 2. Track 1 should comprise two years of one-sided shared savings with a required change in the third year. Track 2 would consist of three years performing in regards to the two-sided model. Three year agreement for both tracks. Two-sided risk eliminated from Track 1, but two tracks are still available for ACOs depending on where they fall on the spectrum of preparedness. Track 2 allows for greater reward and greater risk. Marketing Guidelines for ACOs The Centers for Medicare & Medicaid Services must acknowledge and approve all ACO marketing materials. CMS will provide feedback on acceptable and "approved language," and the ACO can utilize marketing materials five days after they file materials with CMS, and "after certifying compliance with marketing guidelines." Eligible ACO Entities or Participants (1) ACO professionals in group practice arrangements, (2) networks of individual practices of ACO professionals, (3) partnerships or joint venture arrangements between hospitals and ACO professionals, and (4) hospitals employing ACO professionals. Lastly, other eligible entities detailed by the Secretary of HHS. Aside from those detailed in the ACA, eligibility is extended to "Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs)." The only stipulation is FQHCs and RHCs need to detail primary care providers in their facilities who provide services to beneficiaries. ACO Shared Savings One-sided risk model: 2% savings triggers sharing amongst ACO, (small, physician-only and rural ACOs will have some exceptions compared to normal ACOs). Two-Sided Risk Model: shared savings from the beginning with no 2% savings required to trigger savings. When the minimum savings rate is achieved, participating ACOs will have shared savings from the "first dollar." "Proposed Rule Versus Final Rule for Accountable Care Organizations (ACOs) In the Medicare Shared Savings Program: Major Changes" Centers for Medicare & Medicaid Services. https://www.cms.gov/ACO/Downloads/Appendix-ACO-Table.pdf (Accessed 12/28/11); "Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations" Vol 76 No 67 Reg. (April 7, 2011). HEALTH CAPITAL CONSULTANTS 38
COST FOR PROVIDERS: DEVELOPMENT AND OPERATION OF ACOs HEALTH CAPITAL CONSULTANTS 39
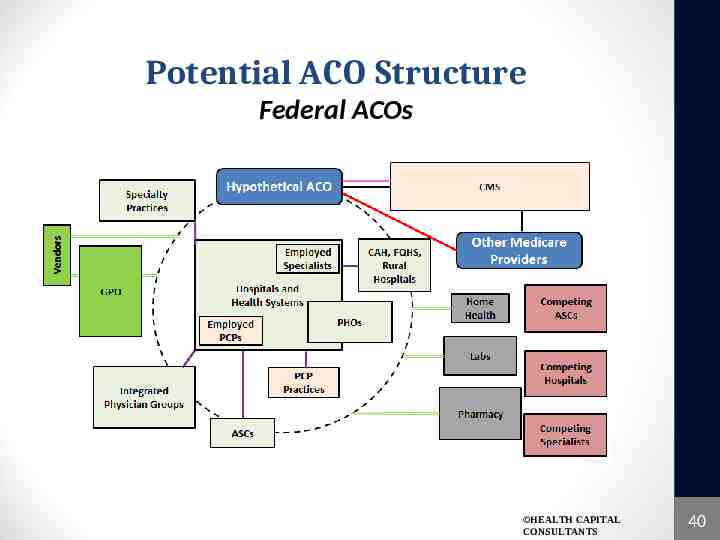
Potential ACO Structure Federal ACOs HEALTH CAPITAL CONSULTANTS 40
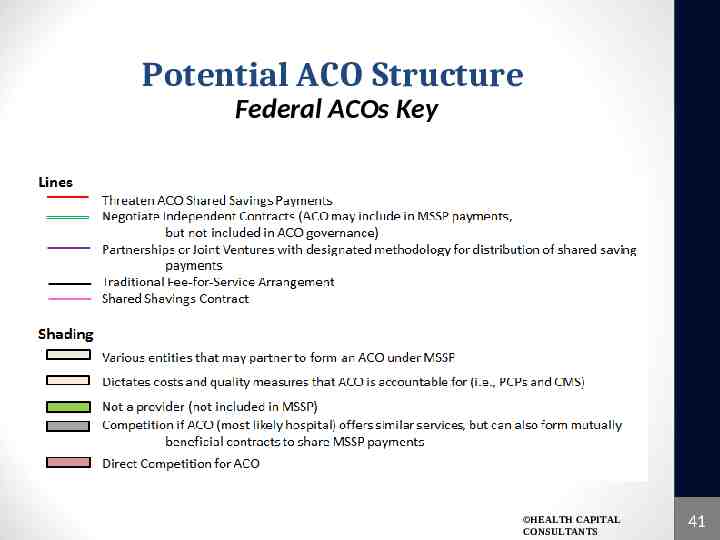
Potential ACO Structure Federal ACOs Key HEALTH CAPITAL CONSULTANTS 41
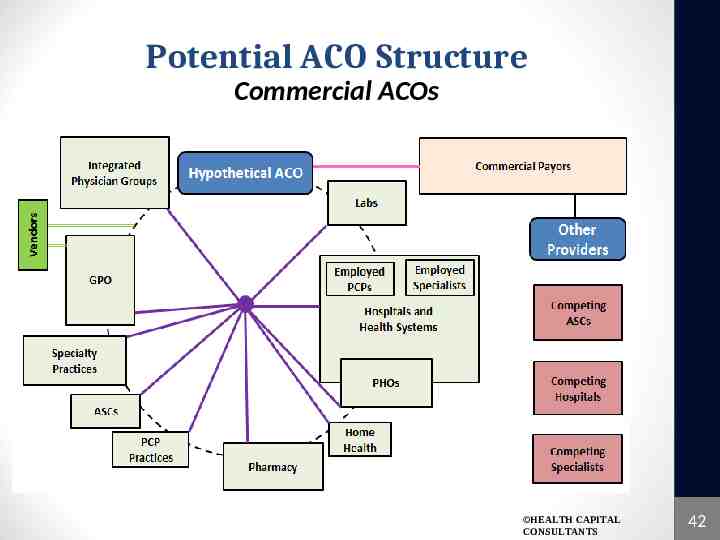
Potential ACO Structure Commercial ACOs HEALTH CAPITAL CONSULTANTS 42

Potential ACO Structure Commercial ACOs Key HEALTH CAPITAL CONSULTANTS 43
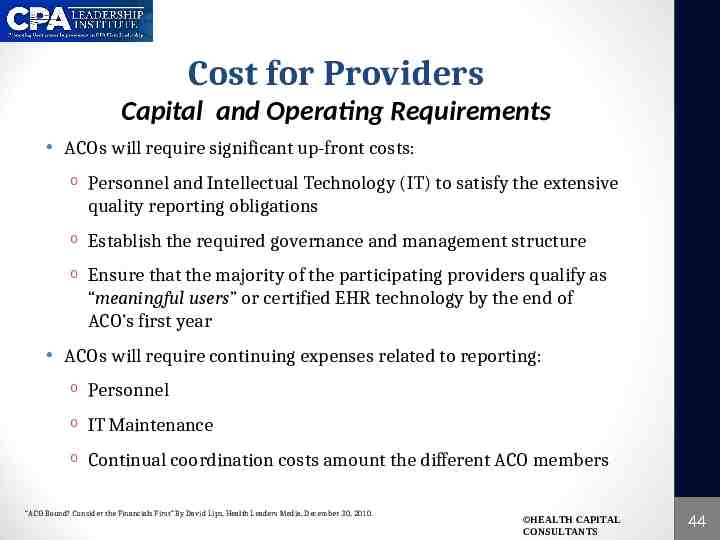
Cost for Providers Capital and Operating Requirements ACOs will require significant up-front costs: o Personnel and Intellectual Technology (IT) to satisfy the extensive quality reporting obligations o Establish the required governance and management structure o Ensure that the majority of the participating providers qualify as “meaningful users” or certified EHR technology by the end of ACO’s first year ACOs will require continuing expenses related to reporting: o Personnel o IT Maintenance o Continual coordination costs amount the different ACO members “ACO Bound? Consider the Financials First” By David Lips, Health Leaders Media, December 30, 2010. HEALTH CAPITAL CONSULTANTS 44

Cost for Providers Capital Requirements for ACO Development ACOs are required to establish a self-executing method for repaying losses to the Medicare program by indicating that: o Funds may be recouped from Medicare payments to the ACO’s participants o ACOs must obtain reinsurance o Place funds in escrow o Obtain surety bonds o Establish a line of credit that Medicare can draw upon, or o Establish another appropriate repayment mechanism in order to ensure repayment to the Medicare Program “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” Federal Register, Vol. 76, No. 67 (April 7, 2011), p. 19643. HEALTH CAPITAL CONSULTANTS 45
Cost for Providers Financial Commitments The financial commitment will be quite large, even for more sophisticated ACO participants First year start-up and operation costs for all ACOs is anticipated as being between 132 million to 263 million The Government Accountability Office (GAO) reported that in 2008 that the participants in the CMS PGP Demonstration invested 1.7 million to meet the requirements of that program through the first year Many believe that these investments will not be recouped under the MSSP “Managing the Risks of Accountable Care,” By Max Reynolds, Healthcare Financial Management Association, http://www.hfma.org/Templates/Print.aspx?id 27518 (Accessed 9/14/11). HEALTH CAPITAL CONSULTANTS 46
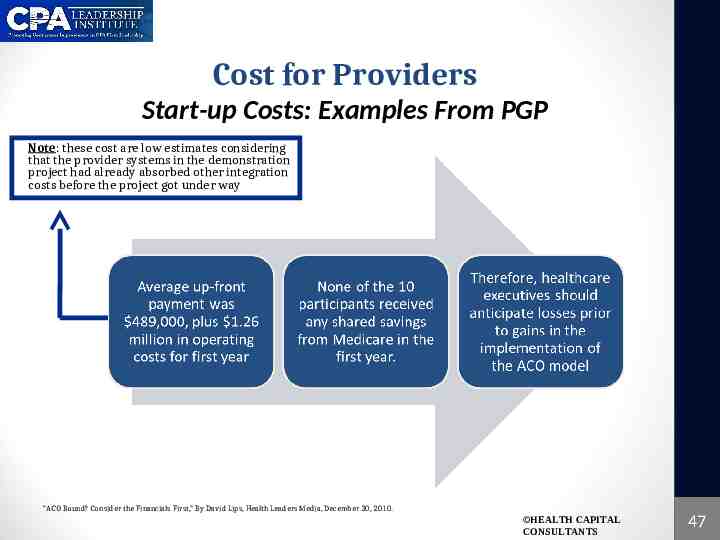
Cost for Providers Start-up Costs: Examples From PGP Note: these cost are low estimates considering that the provider systems in the demonstration project had already absorbed other integration costs before the project got under way “ACO Bound? Consider the Financials First,” By David Lips, Health Leaders Media, December 30, 2010. HEALTH CAPITAL CONSULTANTS 47
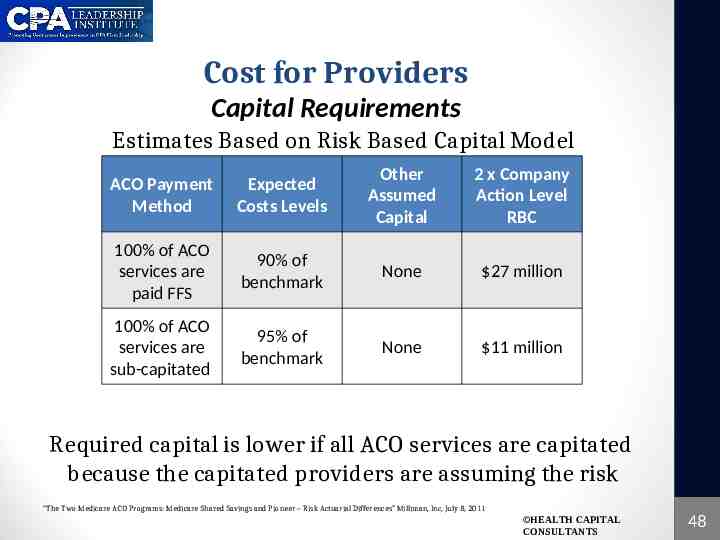
Cost for Providers Capital Requirements Estimates Based on Risk Based Capital Model ACO Payment Method Expected Costs Levels Other Assumed Capital 2 x Company Action Level RBC 100% of ACO services are paid FFS 90% of benchmark None 27 million 100% of ACO services are sub-capitated 95% of benchmark None 11 million Required capital is lower if all ACO services are capitated because the capitated providers are assuming the risk “The Two Medicare ACO Programs: Medicare Shared Savings and Pioneer – Risk Actuarial Differences” Milliman, Inc, July 8, 2011 HEALTH CAPITAL CONSULTANTS 48
Cost for Providers AHA’s Pilot Project Start up costs and operational costs far exceed CMS estimate of 1.7 million Factors that determine Start-up and Ongoing cost: o Size and composition of the patient population served o Geographic area being served o Characteristics of the organization that is undertaking the ACO development o Extent to which some of the needed infrastructure is already in place “From Volume to Value: The Transition to Accountable Care Organizations,” By Keith D. Moore and Dean C. Coddington, American Hospital Association, April 2011. HEALTH CAPITAL CONSULTANTS 49

Cost for Providers AHA Pilot Project: Two Proposed Prototypes “From Volume to Value: The Transition to Accountable Care Organizations,” American Hospital Association, April 2011. HEALTH CAPITAL CONSULTANTS 50
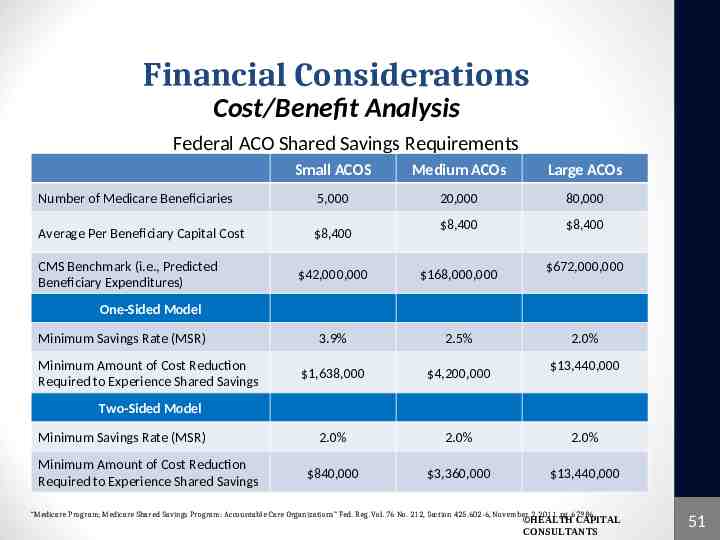
Financial Considerations Cost/Benefit Analysis Federal ACO Shared Savings Requirements Small ACOS Medium ACOs Large ACOs Number of Medicare Beneficiaries 5,000 20,000 80,000 Average Per Beneficiary Capital Cost 8,400 8,400 8,400 CMS Benchmark (i.e., Predicted Beneficiary Expenditures) 672,000,000 42,000,000 168,000,000 3.9% 2.5% 1,638,000 4,200,000 2.0% 2.0% 2.0% 840,000 3,360,000 13,440,000 One-Sided Model Minimum Savings Rate (MSR) Minimum Amount of Cost Reduction Required to Experience Shared Savings 2.0% 13,440,000 Two-Sided Model Minimum Savings Rate (MSR) Minimum Amount of Cost Reduction Required to Experience Shared Savings “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations” Fed. Reg. Vol. 76 No. 212, Section 425.602-6, November 2, 2011, pg. 67986. HEALTH CAPITAL CONSULTANTS 51

Feasibility Analysis Cost / Benefit Analysis: Best Case Scenario There is a Cap on how amount of shared savings an ACO can achieve o One-Sided – 10% of Benchmark o Two-Sided – 15% of Benchmark Reaching this cap is the Best-Case Scenario for ACO benefits “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations” Fed. Reg. Vol. 76 No. 212, Section 425.602-6, November 2, 2011, pg. 67986. HEALTH CAPITAL CONSULTANTS 52

Feasibility Analysis Cost / Benefit Analysis: Best Case Scenario Small ACOS Medium ACOs Large ACOs 10% for One-Sided ACO 4,200,000 16,800,000 67,200,000 15% for Two-Sided ACO 6,300,000 25,200,000 100,800,000 One-Sided Model Percentage of Shared Savings Given to ACO Two-Sided Model Small Medium Large Small Medium Large 50.0% 50.0% 50.0% 60.0% 60.0% 60.0% Cost Reduction Required 8,400,000 33,600,000 134,400,000 10,500,000 42,000,000 168,000,000 Actual Expenditures 33,600,000 134,400,000 537,600,000 31,500,000 126,000,000 504,000,000 Percentage Cost Reduction 20% 20% 20% 25% 25% 25% “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations” Fed. Reg. Vol. 76 No. 212, Section 425.602-6, November 2, 2011, pg. 67986. HEALTH CAPITAL CONSULTANTS 53
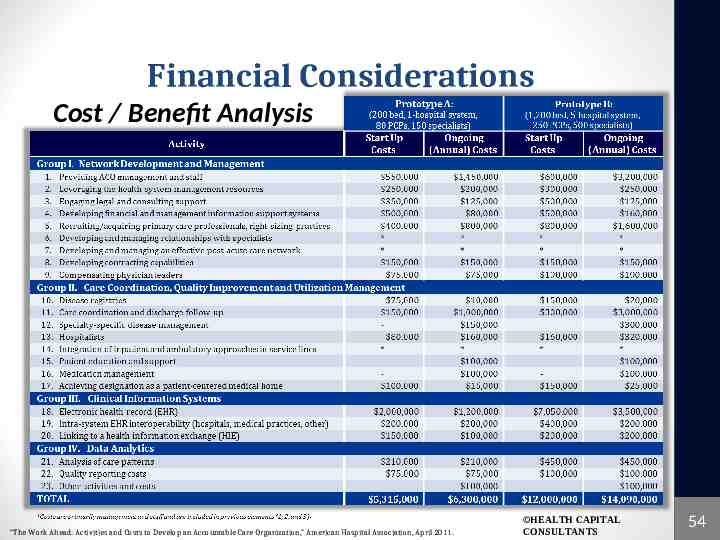
Financial Considerations Cost / Benefit Analysis “The Work Ahead: Activities and Costs to Develop an Accountable Care Organization,” American Hospital Association, April 2011. HEALTH CAPITAL CONSULTANTS 54

Feasibility Analysis NPV Analysis NPV analysis may determine at what size a healthcare enterprise should pursue ACO status Shared savings justify initial capital investments o Incorporates cash flow over three year contract “The Dictionary of Health Economics” By Anthony J. Culyer, Second Edition, Edward Elgar Publishing Limited, 2010, p. 347; “Dictionary of Health Economics and Finance” By David E. Marcinko and Hope R. Hetico, New York, NY: Spring Publishing Company, LLC, p. 251. HEALTH CAPITAL CONSULTANTS 55
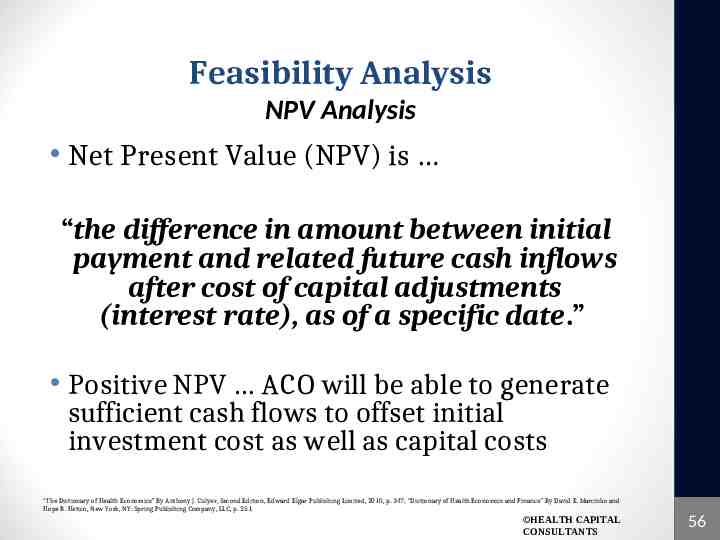
Feasibility Analysis NPV Analysis Net Present Value (NPV) is “the difference in amount between initial payment and related future cash inflows after cost of capital adjustments (interest rate), as of a specific date.” Positive NPV ACO will be able to generate sufficient cash flows to offset initial investment cost as well as capital costs “The Dictionary of Health Economics” By Anthony J. Culyer, Second Edition, Edward Elgar Publishing Limited, 2010, p. 347; “Dictionary of Health Economics and Finance” By David E. Marcinko and Hope R. Hetico, New York, NY: Spring Publishing Company, LLC, p. 251. HEALTH CAPITAL CONSULTANTS 56

Feasibility Analysis NPV Analysis NET PRESENT VALUE OF ACO INVESTMENT – ONE-SIDED MODEL Number of Beneficiaries Required for an ACO to be Profitable "The Work Ahead: Activities and Costs to Develop an Accountable Care Organization" By Keith D. Moore and Dean C. Coddington, American Hospital Association, April 2011, p. 2; “Ibbotson SBBI: Cost of Capital” Morningstar, Chicago, IL: Morningstar, Inc., 2012; Please note that the weighted average cost of capital used is an industry average as reported in Ibbotson – this value will vary for each specific ACO investor; “Selected Interest Rates (Weekly) – H.15” Federal Reserve, April 9, 2012, http://federalreserve,gov/releases/H15/20120409/ (Accessed 4/18/2012). HEALTH CAPITAL CONSULTANTS 57
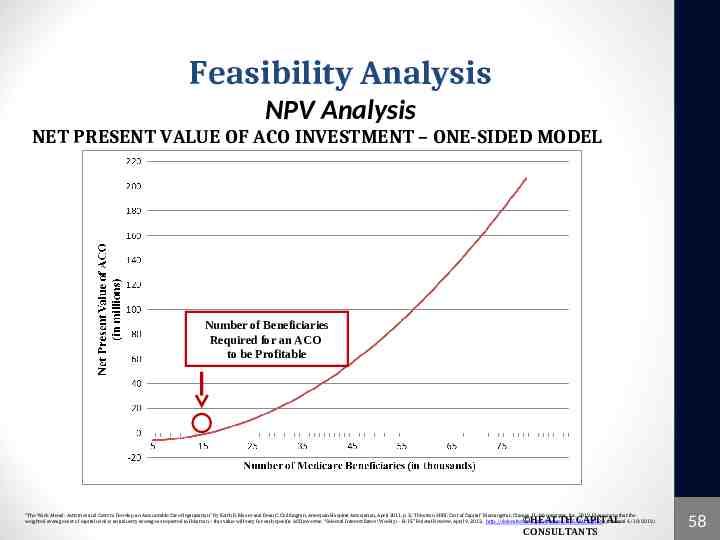
Feasibility Analysis NPV Analysis NET PRESENT VALUE OF ACO INVESTMENT – ONE-SIDED MODEL Number of Beneficiaries Required for an ACO to be Profitable "The Work Ahead: Activities and Costs to Develop an Accountable Care Organization" By Keith D. Moore and Dean C. Coddington, American Hospital Association, April 2011, p. 2; “Ibbotson SBBI: Cost of Capital” Morningstar, Chicago, IL: Morningstar, Inc., 2012; Please note that the weighted average cost of capital used is an industry average as reported in Ibbotson – this value will vary for each specific ACO investor; “Selected Interest Rates (Weekly) – H.15” Federal Reserve, April 9, 2012, http://federalreserve,gov/releases/H15/20120409/ (Accessed 4/18/2012). HEALTH CAPITAL CONSULTANTS 58
Feasibility Analysis NPV Analysis Positive NPV requires One-Sided – 39,000 Beneficiaries Two-Sided – 16,000 Beneficiaries There is a greater opportunity to have increased shared savings under the twosided model In exchange, it also exposes ACOs to risk (i.e., Potential shared losses) “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations” Fed. Reg. Vol. 76 No. 212, Section 425.602-6, November 2, 2011, pg. 67986. HEALTH CAPITAL CONSULTANTS 59
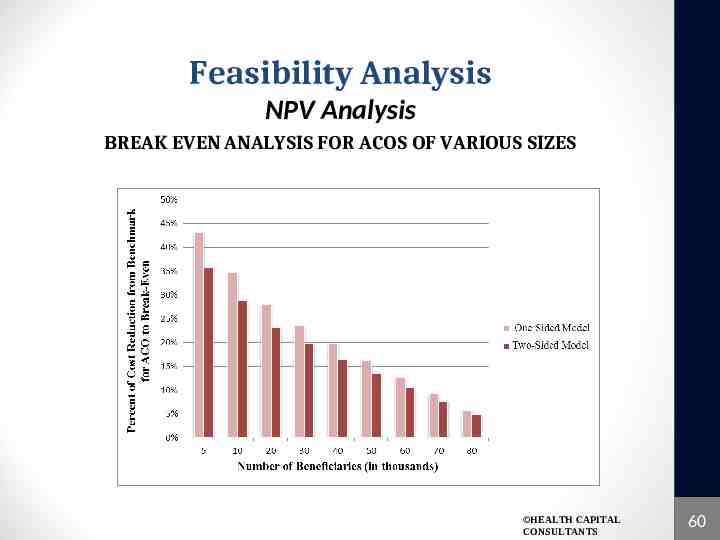
Feasibility Analysis NPV Analysis BREAK EVEN ANALYSIS FOR ACOS OF VARIOUS SIZES HEALTH CAPITAL CONSULTANTS 60
Feasibility Analysis NPV Analysis One-sided o Small and Medium (5,000-20,000 beneficiaries) not feasible Two-sided o Small (5,000 – 10,000 beneficiaries) not feasible HEALTH CAPITAL CONSULTANTS 61
Feasibility Analysis NPV Conclusions Large ACOs most likely to succeed o 4% reduction in expenditures vs. 22% o Added consideration – more likely to have previous integration (i.e., specialties, primary care, healthcare information technology) o More likely to meet quality goals and reporting requirements Poor quality can lower shared savings HEALTH CAPITAL CONSULTANTS 62

COST FOR PATIENTS: CONTROLLING HEALTHCARE COSTS HEALTH CAPITAL CONSULTANTS 63
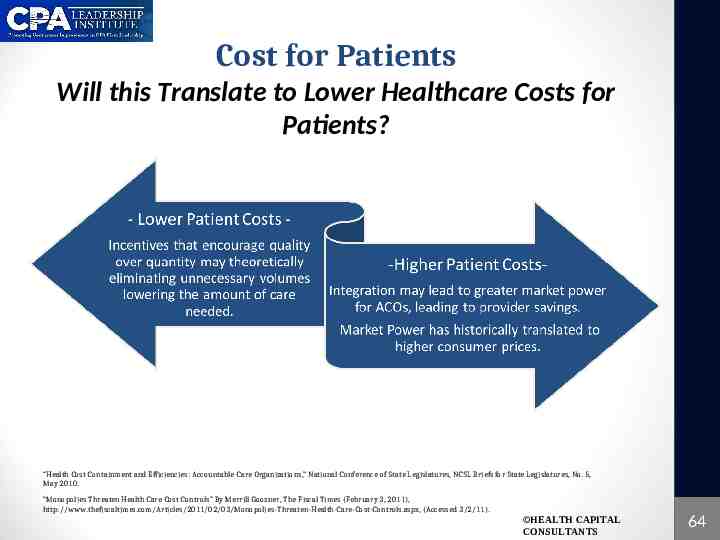
Cost for Patients Will this Translate to Lower Healthcare Costs for Patients? “Health Cost Containment and Efficiencies: Accountable Care Organizations,” National Conference of State Legislatures, NCSL Briefs for State Legislatures, No. 5, May 2010. “Monopolies Threaten Health Care Cost Controls” By Merrill Goozner, The Fiscal Times (February 3, 2011), http://www.thefiscaltimes.com/Articles/2011/02/03/Monopolies-Threaten-Health-Care-Cost-Controls.aspx, (Accessed 3/2/11). HEALTH CAPITAL CONSULTANTS 64
Cost for Patients Controlling Healthcare Costs ACOs may provide framework to control costs “Health care providers sign an agreement to participate with the ACO. Spending targets are set based on past years’ data. If total spending comes in under target, providers share the savings. Savings come from better chronic care management, compliance with preventive care guidelines and better care coordination among ACO providers.” - Health Policy Expert, Steven Shortell “Health Cost Containment and Efficiencies: Accountable Care Organizations,” National Conference of State Legislatures, NCSL Briefs for State Legislatures, No. 5, May 2010. HEALTH CAPITAL CONSULTANTS 65
Cost for Patients Controlling Healthcare Costs Congressional Budget Office estimates potential savings from ACOs could reach approximately 5.3 billion between 2010-2019 Net savings will not be realized until 2013 Despite These Estimates Demonstration program outcomes: “It is questionable whether the PGP [Physician Group Practice Demonstration] has saved money.” “Health Cost Containment and Efficiencies: Accountable Care Organizations,” National Conference of State Legislatures, NCSL Briefs for State Legislatures, No. 5, May 2010. HEALTH CAPITAL CONSULTANTS 66
Cost for Patients Value Metrics for Accountable Care Value is the expectation of future economic benefit In healthcare value has two components: o Value to Society: future benefit to the population as a whole o Value to Providers: emphasizes economic returns to individual enterprises, assets, and services “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” Federal Register, Vol. 76, No. 67 (April 7, 2011), pg. 19531 HEALTH CAPITAL CONSULTANTS 67

Cost for Patients Value Metrics for Accountable Care “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” Federal Register, Vol. 76, No. 67 (April 7, 2011), pg. 19531 “Investors Not Likely to Provide ACO Funding Under Proposed Rule, Venture Capitalist Says” By Sara Hansard, Bureau of National Affairs, Health Law Reporter, Vol. 20, No. 1026, 2011. HEALTH CAPITAL CONSULTANTS 68
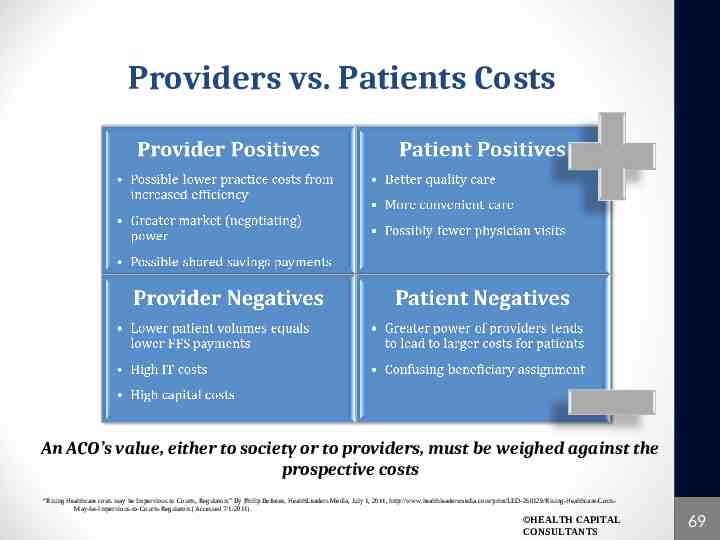
Providers vs. Patients Costs An ACO’s value, either to society or to providers, must be weighed against the prospective costs “Rising Healthcare costs may be Impervious to Courts, Regulators” By Philip Betbeze, HealthLeaders Media, July 1, 2011, http://www.healthleadersmedia.com/print/LED-268129/Rising-Healthcare-CostsMay-be-Impervious-to-Courts-Regulators (Accessed 7/1/2011). HEALTH CAPITAL CONSULTANTS 69

IMPACT OF ACOs HEALTH CAPITAL CONSULTANTS 70
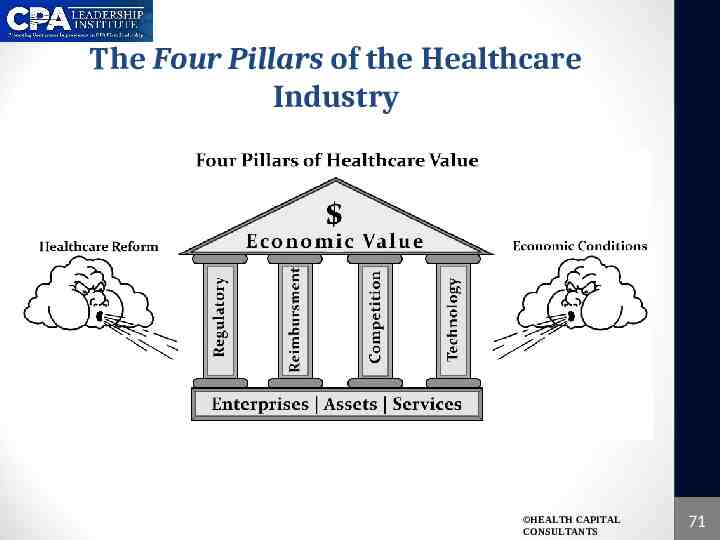
The Four Pillars of the Healthcare Industry HEALTH CAPITAL CONSULTANTS 71
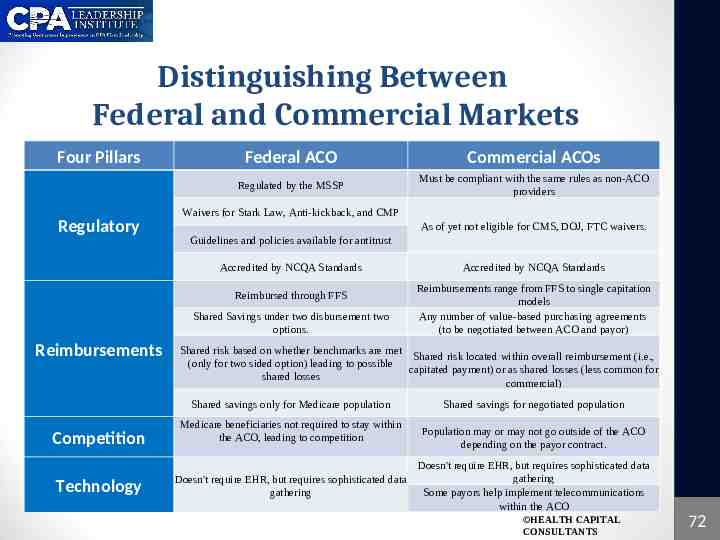
Distinguishing Between Federal and Commercial Markets Four Pillars Federal ACO Commercial ACOs Regulated by the MSSP Must be compliant with the same rules as non-ACO providers Waivers for Stark Law, Anti-kickback, and CMP Regulatory As of yet not eligible for CMS, DOJ, FTC waivers. Guidelines and policies available for antitrust Accredited by NCQA Standards Reimbursed through FFS Shared Savings under two disbursement two options. Reimbursements Accredited by NCQA Standards Reimbursements range from FFS to single capitation models Any number of value-based purchasing agreements (to be negotiated between ACO and payor) Shared risk based on whether benchmarks are met Shared risk located within overall reimbursement (i.e., (only for two sided option) leading to possible capitated payment) or as shared losses (less common for shared losses commercial) Shared savings only for Medicare population Competition Medicare beneficiaries not required to stay within the ACO, leading to competition Technology Doesn't require EHR, but requires sophisticated data gathering Shared savings for negotiated population Population may or may not go outside of the ACO depending on the payor contract. Doesn't require EHR, but requires sophisticated data gathering Some payors help implement telecommunications within the ACO HEALTH CAPITAL CONSULTANTS 72
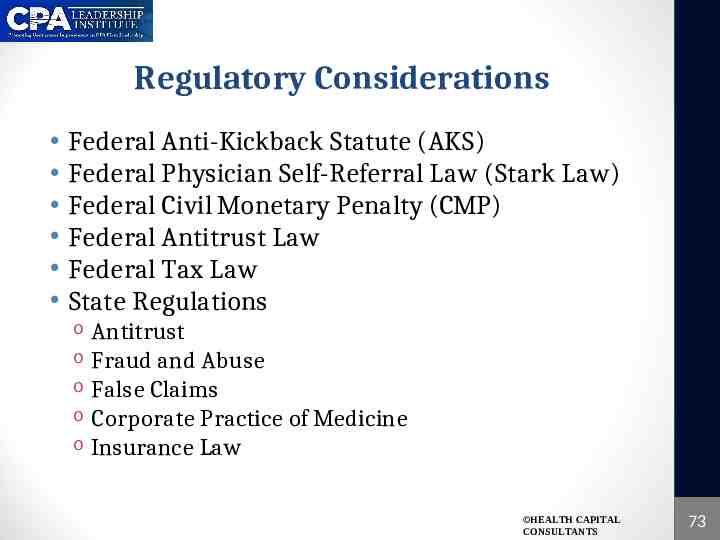
Regulatory Considerations Federal Anti-Kickback Statute (AKS) Federal Physician Self-Referral Law (Stark Law) Federal Civil Monetary Penalty (CMP) Federal Antitrust Law Federal Tax Law State Regulations Antitrust o Fraud and Abuse o False Claims o Corporate Practice of Medicine o Insurance Law o HEALTH CAPITAL CONSULTANTS 73

Regulatory Considerations Federal AKS “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” Federal Register, Vol. 76, No. 67 (April 7, 2011). HEALTH CAPITAL CONSULTANTS 74
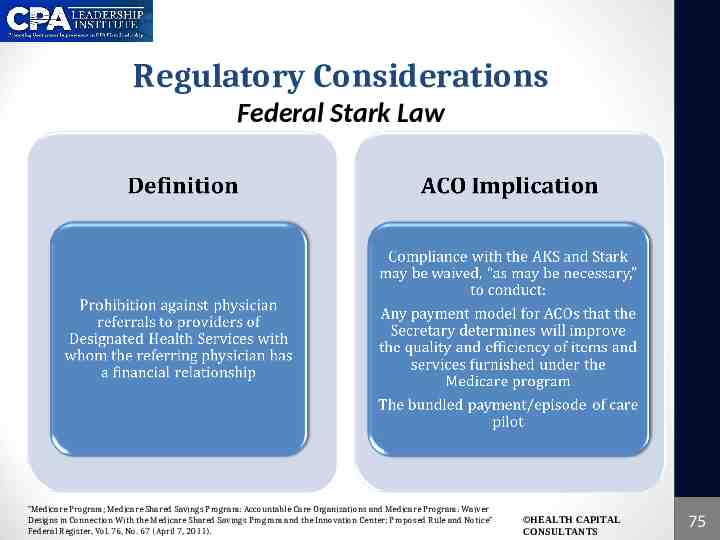
Regulatory Considerations Federal Stark Law “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” Federal Register, Vol. 76, No. 67 (April 7, 2011). HEALTH CAPITAL CONSULTANTS 75
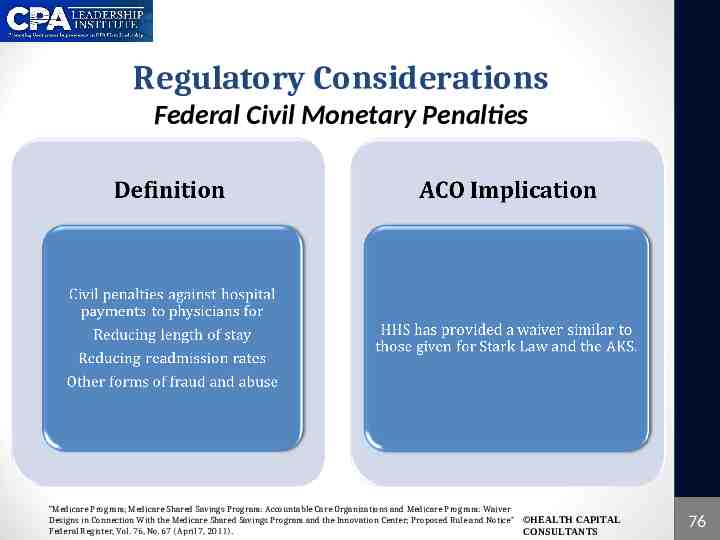
Regulatory Considerations Federal Civil Monetary Penalties “Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations and Medicare Program: Waiver Designs in Connection With the Medicare Shared Savings Program and the Innovation Center; Proposed Rule and Notice” HEALTH CAPITAL Federal Register, Vol. 76, No. 67 (April 7, 2011). CONSULTANTS 76
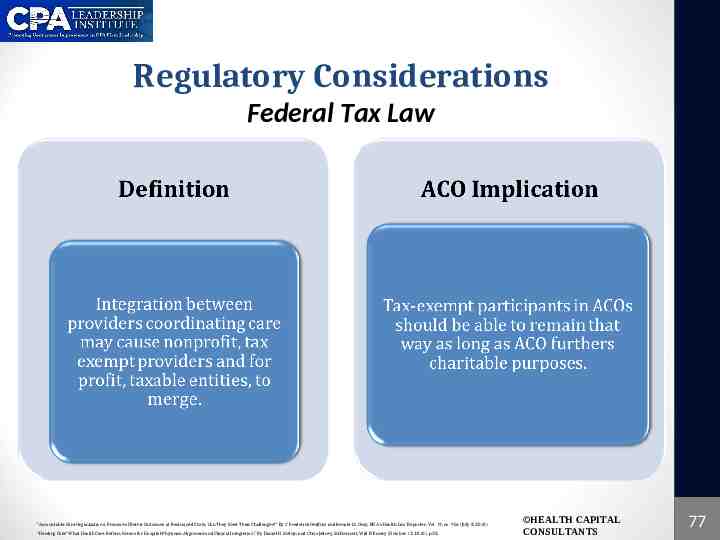
Regulatory Considerations Federal Tax Law “Accountable Care Organizations: Promise of Better Outcomes at Restrained Costs; Can They Meet Their Challenges?” By C. Frederick Geilfuss and Renate M. Gray, BNA’s Health Law Reporter, Vol. 19, no. 956 (July 8, 2010). “Herding Cats? What Health Care Reform Means for Hospital-Physician Alignment and Clinical Integration,” By Daniel H. Melvin and Chris Jedrey, McDermott, Will & Emery (October 13, 2010), p.38. HEALTH CAPITAL CONSULTANTS 77
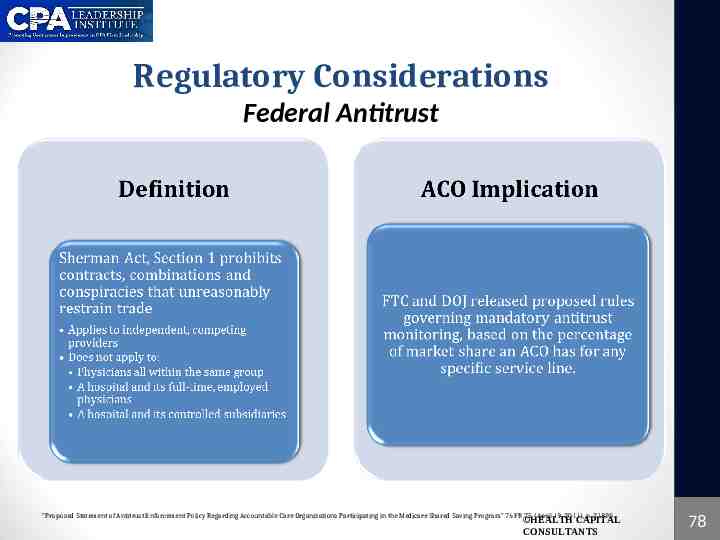
Regulatory Considerations Federal Antitrust “Proposed Statement of Antitrust Enforcement Policy Regarding Accountable Care Organizations Participating in the Medicare Shared Saving Program” 76 FR 75 (April 19, 2011), p. 21895. HEALTH CAPITAL CONSULTANTS 78
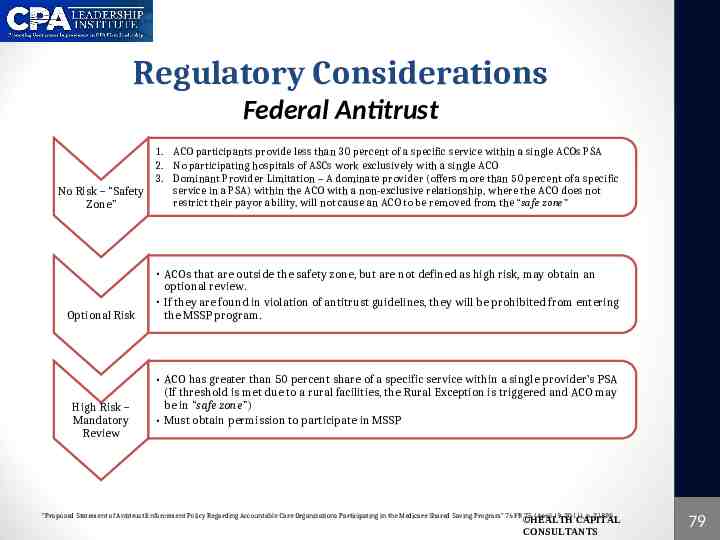
Regulatory Considerations Federal Antitrust 1. ACO participants provide less than 30 percent of a specific service within a single ACOs PSA 2. No participating hospitals of ASCs work exclusively with a single ACO 3. Dominant Provider Limitation – A dominate provider (offers more than 50 percent of a specific service in a PSA) within the ACO with a non-exclusive relationship, where the ACO does not No Risk – “Safety restrict their payor ability, will not cause an ACO to be removed from the “safe zone” Zone” Optional Risk High Risk – Mandatory Review ACOs that are outside the safety zone, but are not defined as high risk, may obtain an optional review. If they are found in violation of antitrust guidelines, they will be prohibited from entering the MSSP program. ACO has greater than 50 percent share of a specific service within a single provider’s PSA (If threshold is met due to a rural facilities, the Rural Exception is triggered and ACO may be in “safe zone”) Must obtain permission to participate in MSSP “Proposed Statement of Antitrust Enforcement Policy Regarding Accountable Care Organizations Participating in the Medicare Shared Saving Program” 76 FR 75 (April 19, 2011), p. 21895. HEALTH CAPITAL CONSULTANTS 79
Regulatory Considerations State Laws State “Corporate Practice of Medicine” (CPOM) laws prohibit the practice of medicine or the employment of physicians by business corporations A variety of care models and structures for hospital-physician relationships have been developed to comply with state statutes, which may not fit easily with the structure or goals of an ACO CPOM laws could prevent some ACOs from hiring physicians to work directly with provider participants in managing and better coordinating the provision of health services “AAMC Statement on Legal Issues Related to Accountable Care Organizations (ACOs) and Healthcare Innovation Zones (HIZs),” Association of American Medical Colleges, October 5, 2010, https://www.aamc.org/download/151426/data/aamc comment on legal issues related to accountable care organi.pdf (Accessed 09/14/2011); “Toolkit”, Accountable Care Organization Learning Network, The Brookings Institute, 2010,http://www.nachc.com/client/documents/ACOToolkitJanuary2011.pdf#page 6 (Accessed 9/14/2011); “Accountable Care Organizations in California: Programmatic and Legal Considerations” By: William S. Bernstein et al., California HealthCare Foundation, July 2011, http://www.chcf.org/ /media/MEDIA%20LIBRARY%20Files/PDF/A/PDF%20ACOProgrammaticLegalConsiderations.pdf (Accessed 09/14/2011) HEALTH CAPITAL CONSULTANTS 80
Regulatory Considerations State Regulation Physician-self referral, anti-kickback, or related fraud and abuse laws Private Inurement/Private Benefit Issues o 501(c)(3) organizations cannot be organized or operated for the benefit of private interests State Insurance Laws o Some states require that health care providers assume financial risks, and that employer groups be regulated as health insurers Can entail risk-based capital reserve requirements and other state law obligations, making it difficult for provider organizations (and ACO components) to enter into risk-sharing agreements “AAMC Statement on Legal Issues Related to Accountable Care Organizations (ACOs) and Healthcare Innovation Zones (HIZs),” Association of American Medical Colleges, October 5, 2010, https://www.aamc.org/download/151426/data/aamc comment on legal issues related to accountable care organi.pdf (accessed 09/14/2011). “Toolkit”, Accountable Care Organization Learning Network, The Brookings Institute, 2010,http://www.nachc.com/client/documents/ACOToolkitJanuary20111.pdf#page 6 (accessed 9/14/2011). HEALTH CAPITAL CONSULTANTS 81
Regulatory Considerations Fair Market Value and Commercial Reasonableness ACOs involve coordinated care covering a variable and wide range of services o o Quantifying opportunity cost and other marginal costs incurred by physicians during a transition to an ACO Determining the Fair Market Value attributable to the savings that accrue from this new system (which may result in compensation to physicians) may be difficult Proposed Stark Law waiver: shared savings earned by ACOs is not subject to FMV and commercially reasonable scrutiny AAMC Statement on Legal Issues Related to Accountable Care Organizations (ACOs) and Healthcare Innovation Zones (HIZs),” Association of American Medical Colleges, October 5, 2010, https://www.aamc.org/download/151426/data/aamc comment on legal issues related to accountable care organi.pdf (accessed 09/14/2011) The Proposed Waivers of the Fraud & Abuse Laws for ACOs: Have OIG and CMS Gone Far Enough?, By Daniel Melvin and Webb Millsaps, McDermott Will & Emery, http://www.mwe.com/info/news/wp0511b.pdf (Accessed 09/14/2011). HEALTH CAPITAL CONSULTANTS 82
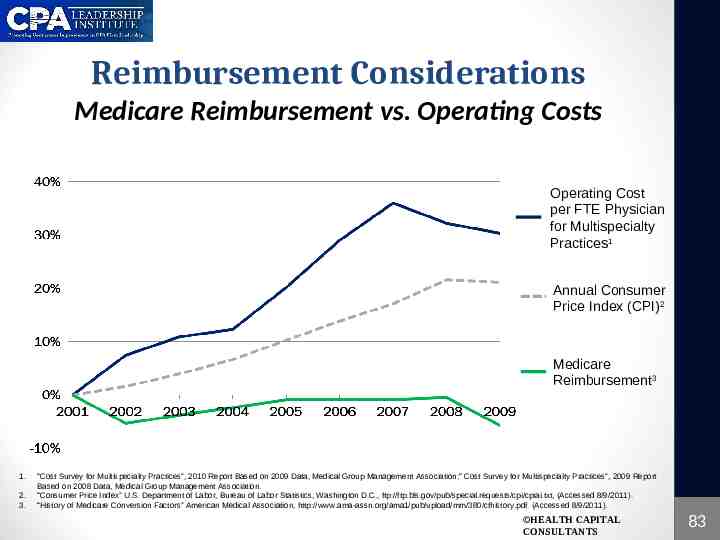
Reimbursement Considerations Medicare Reimbursement vs. Operating Costs Operating Cost per FTE Physician for Multispecialty Practices1 Annual Consumer Price Index (CPI)2 Medicare Reimbursement3 1. 2. 3. “Cost Survey for Multispecialty Practices”, 2010 Report Based on 2009 Data, Medical Group Management Association;“ Cost Survey for Multispecialty Practices”, 2009 Report Based on 2008 Data, Medical Group Management Association. “Consumer Price Index” U.S. Department of Labor, Bureau of Labor Statistics, Washington D.C., ftp://ftp.bls.gov/pub/special.requests/cpi/cpiai.txt, (Accessed 8/9/2011). “History of Medicare Conversion Factors” American Medical Association, http://www.ama-assn.org/ama1/pub/upload/mm/380/cfhistory.pdf (Accessed 8/9/2011). HEALTH CAPITAL CONSULTANTS 83
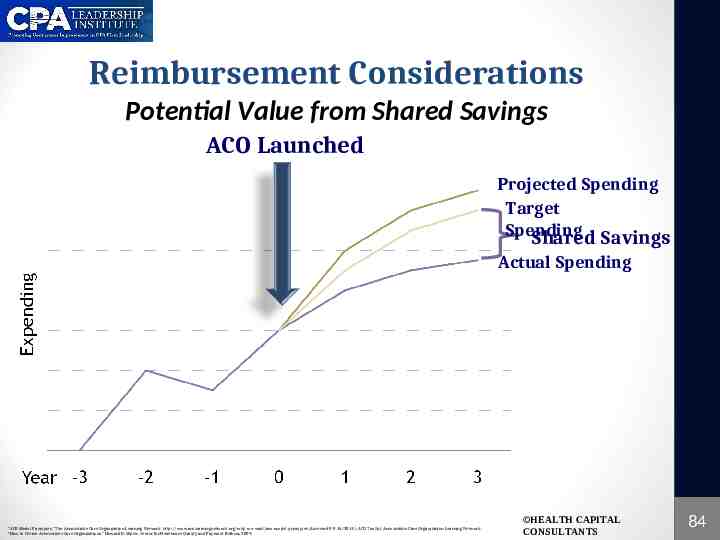
Reimbursement Considerations Potential Value from Shared Savings ACO Launched Projected Spending Target Spending Shared Savings Actual Spending “AC0 Model Principles,” The Accountable Care Organization Learning Network, http://www.acolearningnetwork.org/why-we-exist/aco-model-principles (Accessed 09/16/2011); ACO Toolkit, Accountable Care Organization Learning Network ; “How to Create Accountable Care Organizations,” Howard D. Miller, Center for Healthcare Quality and Payment Reform, 2009. HEALTH CAPITAL CONSULTANTS 84
Reimbursement Considerations Hospitals Large health systems may be in best position for form ACOs Attract more PCPs o Vertical Integration will likely aid in transition to ACO o May easily meet quality requirements o Greater access to capital and IT requirements o Potential Hurdles: o May need to lower cost or increase private insurers’ cost to generate shared savings “Investors Not Likely to Provide ACO Funding Under Proposed Rule, Venture Capitalist Says” By Sara Hansard, Bureau of National Affairs, Health Law Reporter, Vol. 20, No. 1026, 2011; “Quality over Quantity” By Bryn Nelson, The Hospitalist (December 2009), www.the-hospitalist.org/details/article/477391/quality over quantity.html, (Accessed 2/28/11).; “Will Mayo Clinic save money as an ACO?” By Christopher Snowbeck and Don McCanne, Physicians for a National Health Program (February 8, 2011), www.pnhp.org/print/news/2011/february/will-mayo-clinic-save-money-as-an-aco, (Accessed 2/28/11). HEALTH CAPITAL CONSULTANTS 85

Reimbursement Considerations Physician Practices Increasing hospital - physician alignment “ACOs can work with physicians in charge” By Victoria Stagg Elliott, American Medical News (January 31, 2011), www.ama-assn.org/amednews/2011/01/31/bisa0131.htm, (Accessed 2/7/11). HEALTH CAPITAL CONSULTANTS 86

Reimbursement Considerations ASCs & Outpatient Providers Requires linking clinical and cost systems to the ACO’s information on the patient population through the implementation of electronic health record (EHR) system (Note: expensive proposition as there are no “meaningful use” subsidies for ASCs) Volume of services for ASCs may actually increase as providers look for ways to decrease hospital costs, depending on how ACOs react to the incentive to decrease costs “Surgery Centers Play an Important Role in ACOs” By Andrew Hayek, Surgical Care Affiliates (January 3, 2011), www.beckersasc.com(Accessed 1/21/11). “4 Ways ACOS Could Affect ASCs” By Leigh Page, Becker’s ASC Review (December 20, 2010). “Accountable Care Organizations: Implications for Ambulatory Surgery Centers” By Healthcents (January 25, 2011), p. 26, 29. HEALTH CAPITAL CONSULTANTS 87

Reimbursement Considerations Medical Homes ACA does not include section specific to Patient-Centered Medical Homes (PCMH), but PCMH’s are promoted throughout health reform legislation PCMHs may likely be stepping stone to the formation of an ACO infrastructure PCMH Structure: team-based model that is run by primary care physicians who are in charge of providing a continuum of care for all aspects of healthcare throughout a patient’s life. o Requires streamline infrastructure PCMH Primary Goal: coordinate the care of a patient while reducing unnecessary duplication of services and therefore increasing cost of care “New Payment and Delivery Models Under Health Reform Require New Relationships Between Physicians and Hospitals” By Janice A. Anderson and Heidi R. Shaw, BNA’s Health Law Reporter, Vol. 19, no. 1612 (November 18, 2010). HEALTH CAPITAL CONSULTANTS 88
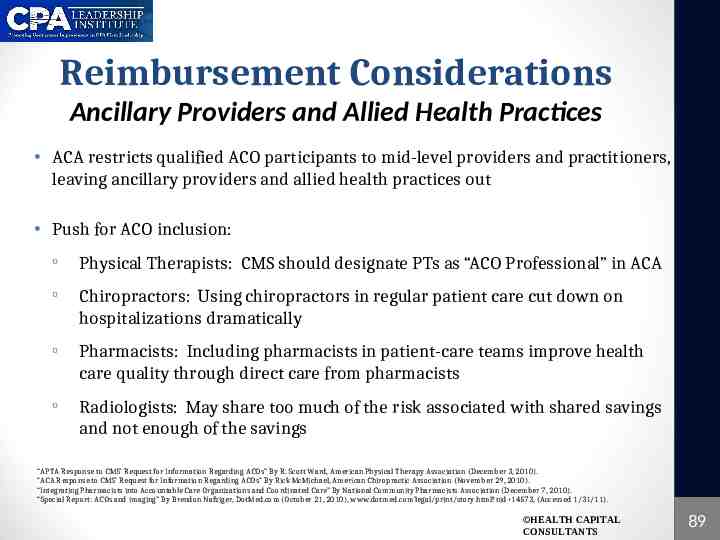
Reimbursement Considerations Ancillary Providers and Allied Health Practices ACA restricts qualified ACO participants to mid-level providers and practitioners, leaving ancillary providers and allied health practices out Push for ACO inclusion: o o o o Physical Therapists: CMS should designate PTs as “ACO Professional” in ACA Chiropractors: Using chiropractors in regular patient care cut down on hospitalizations dramatically Pharmacists: Including pharmacists in patient-care teams improve health care quality through direct care from pharmacists Radiologists: May share too much of the risk associated with shared savings and not enough of the savings “APTA Response to CMS’ Request for Information Regarding ACOs” By R. Scott Ward, American Physical Therapy Association (December 3, 2010). “ACA Response to CMS’ Request for Information Regarding ACOs” By Rick McMichael, American Chiropractic Association (November 29, 2010). “Integrating Pharmacists into Accountable Care Organizations and Coordinated Care” By National Community Pharmacists Association (December 7, 2010). “Special Report: ACOs and imaging” By Brendon Nafziger, DotMed.com (October 21, 2010), www.dotmed.com’legal/print/story.html?nid 14573, (Accessed 1/31/11). HEALTH CAPITAL CONSULTANTS 89

Reimbursement Considerations Impact on Payers Private Insurance Primary Concerns: o Increased market power by providers leading to increased charges to private insurers o Insufficient accountable care progress for ACOs contracting with health systems Contracts move away from FFS reimbursement models hoping to achieve cost and clinical efficiencies Government Goal to reduce Medicare spending Congressional Budget Office CBO estimates ACOs will save Medicare 4.9 billion through 2019, (1% of spending) “Insurers, Healthcare Providers Spar Over ACO Regulations” By Lindsey Dunn, Beckers Hospitals Review (January 10, 2011). “Monopolies Threaten Health Care Cost Controls” By Merrill Goozner, The Fiscal Times (February 3, 2011), http://www.thefiscaltimes.com/Articles/2011/02/03/Monopolies-Threaten-Health-Care-Cost-Controls.aspx, (Accessed 3/2/11). “Insurers Work With Providers On Crucial ACO Components” ACO Business News, Vol. 1, No. 1, November 2010, p. 5. HEALTH CAPITAL CONSULTANTS 90

Competition Considerations Porter’s Five Forces HEALTH CAPITAL CONSULTANTS 91
Technology Considerations Electronic Medical Records o Significant cost o Help eliminate silos and increase continuity of care o Meaningful use standards The technological impacts on providers choosing to participate in an ACO are rooted in the primary issue of purchasing or updating an EHR system o Costly o Must meet meaningful use standards to be eligible for savings EHR integration and alignment among ACO participants is critical to ensure benefits of HIT utilization are obtained “Technology Fundamentals for Realizing ACO Success”, Medicity, September 2010, http://www.himss.org/content/files/Medicity ACO Whitepaper.pdf, (Accessed June 30, 2011). HEALTH CAPITAL CONSULTANTS 92
CONCLUDING REMARKS HEALTH CAPITAL CONSULTANTS 93
Concluding Remarks With the MSSP receiving poor support due to theoretical savings, yet very real costs, providers looking to transition to an ACO have been doing so through the commercial market o Some insurers negotiating ACO-like contracts include: BCBS MA (the alternative quality contract), Aetna, Human, and Wellpoint. To succeed, ACOs will need what managed care lacked: public understanding, payor support, partnerships between physicians and hospitals, up-front financial resources, and time for integration. “Accountable Care Organizations: Whatever Its Growing Pains, The Concept is Too Vitally Important to Fail” By Francis J. Crosson, Health Affairs, Vol. 30, No. 7, July 2011, p. 1250-1255. HEALTH CAPITAL CONSULTANTS 94

Concluding Remarks “Love everyone, trust no one, and paddle your own canoe.” HEALTH CAPITAL CONSULTANTS 95