Chapter 538 School-Based Health Services Physical Therapy Billing Form
22 Slides155.31 KB
Chapter 538 School-Based Health Services Physical Therapy Billing Form Effective August 1, 2019
Consent to Bill Medicaid Prior to billing parents must provide written consent to release information and to bill for Medicaid reimbursement. Consent is only good for one calendar year. Parents are to be provided an annual notice. 2
Plan of Care Services must be documented on the Plan of Care signed by the parent and therapist. Effective August 1, 2019 Service Plan is now called a Plan of Care. This provides more consistency and avoids a terminology conflict with private school service plans. There is not a need to have a new one signed if it says Service Care Plan. The IEP Program has been adjusted to reflect the change in terminology. Specific ICD-10 diagnosis codes are required. ICD-10 codes must relate to the specific type of therapy being provided. Think of these more as treatment diagnosis codes. All appropriate diagnosis codes need to be listed on the Plan of Care. A global code such as Cerebral Palsy would not be appropriate. 3
Physician Authorization Form Physician Authorization is required annually to bill for occupational therapy. The Physical Therapist is to document suggested ICD-10 diagnosis codes that specifically relate to the therapy being provided. When the physician signs the authorization form they are confirming the therapist’s code(s). Authorizations can be signed by a Physician (MD or DO), Physician’s Assistant (PA) or by an Advanced Practice Registered Nurse (APRN). 4
Student Demographics Use the student’s real name as listed in WVEIS The diagnosis code is to be an ICD-10 code that matches the need for occupational therapy. County and school names can be written out or use the county and school WVEIS codes. For provider name print the name of the person providing the service. 5
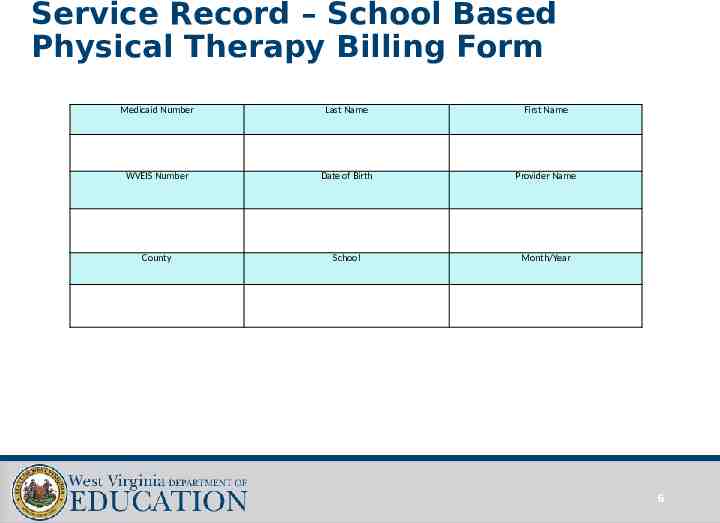
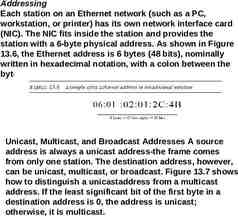
Service Record – School Based Physical Therapy Billing Form Medicaid Number Last Name First Name WVEIS Number Date of Birth Provider Name County School Month/Year 6
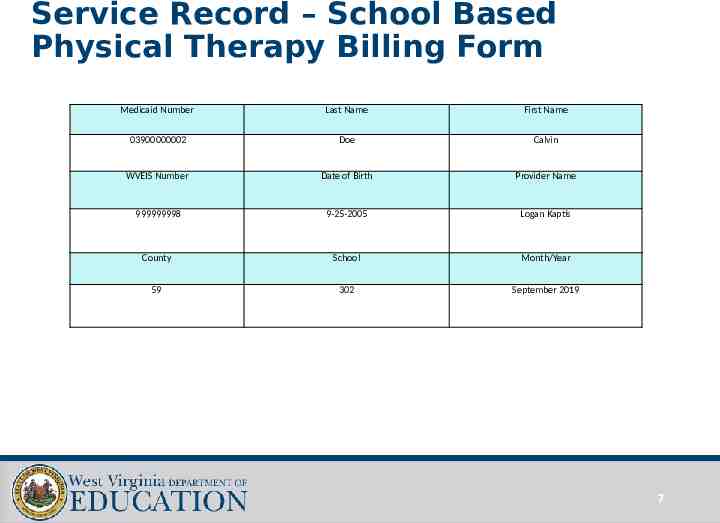
Service Record – School Based Physical Therapy Billing Form Medicaid Number Last Name First Name 03900000002 Doe Calvin WVEIS Number Date of Birth Provider Name 999999998 9-25-2005 Logan Kaptis County School Month/Year 59 302 September 2019 7
Diagnosis Codes Enter the PT specific ICD 10 Diagnosis Codes on the form starting with box number one. Enter the codes that are directly associated with the therapy sessions and/or assessments. 8
ICD 10 Diagnosis Codes LIST ALL DIAGNOSIS CODES RELATED TO PHYSICAL THERAPY 1. 2. 3. 4. 5. 6. 9
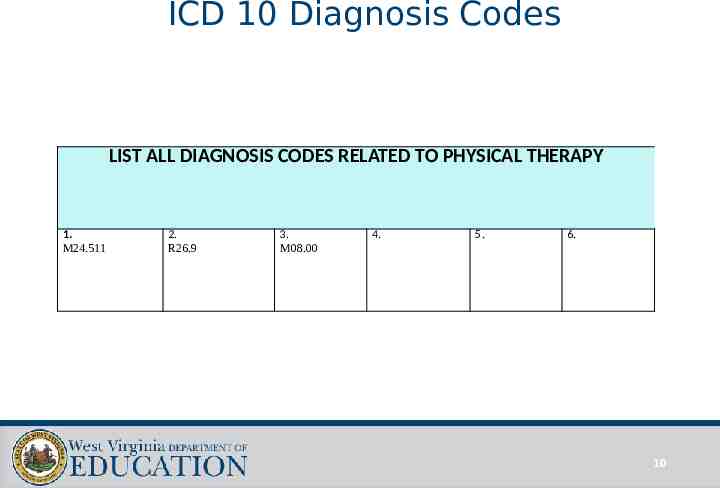
ICD 10 Diagnosis Codes LIST ALL DIAGNOSIS CODES RELATED TO PHYSICAL THERAPY 1. M24.511 2. R26.9 3. M08.00 4. 5. 6. 10
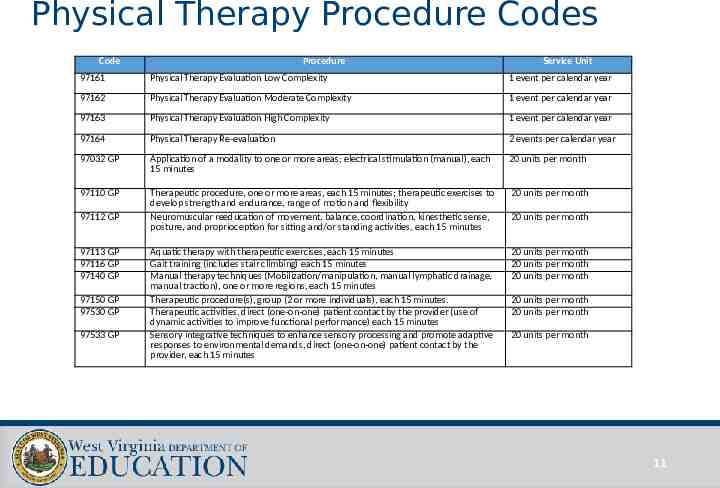
Physical Therapy Procedure Codes Code Procedure Service Unit 97161 Physical Therapy Evaluation Low Complexity 1 event per calendar year 97162 Physical Therapy Evaluation Moderate Complexity 1 event per calendar year 97163 Physical Therapy Evaluation High Complexity 1 event per calendar year 97164 Physical Therapy Re-evaluation 2 events per calendar year 97032 GP Application of a modality to one or more areas; electrical stimulation (manual), each 15 minutes 20 units per month 97110 GP Therapeutic procedure, one or more areas, each 15 minutes; therapeutic exercises to develop strength and endurance, range of motion and flexibility Neuromuscular reeducation of movement, balance, coordination, kinesthetic sense, posture, and proprioception for sitting and/or standing activities, each 15 minutes 20 units per month Aquatic therapy with therapeutic exercises, each 15 minutes Gait training (includes stair climbing) each 15 minutes Manual therapy techniques (Mobilization/manipulation, manual lymphatic drainage, manual traction), one or more regions, each 15 minutes Therapeutic procedure(s), group (2 or more individuals), each 15 minutes. Therapeutic activities, direct (one-on-one) patient contact by the provider (use of dynamic activities to improve functional performance) each 15 minutes Sensory integrative techniques to enhance sensory processing and promote adaptive responses to environmental demands, direct (one-on-one) patient contact by the provider, each 15 minutes 20 units per month 20 units per month 20 units per month 97112 GP 97113 GP 97116 GP 97140 GP 97150 GP 97530 GP 97533 GP 20 units per month 20 units per month 20 units per month 20 units per month 11
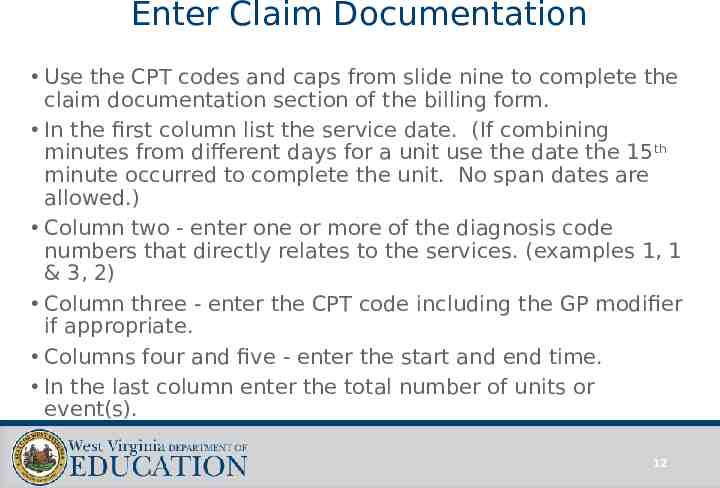
Enter Claim Documentation Use the CPT codes and caps from slide nine to complete the claim documentation section of the billing form. In the first column list the service date. (If combining minutes from different days for a unit use the date the 15 th minute occurred to complete the unit. No span dates are allowed.) Column two - enter one or more of the diagnosis code numbers that directly relates to the services. (examples 1, 1 & 3, 2) Column three - enter the CPT code including the GP modifier if appropriate. Columns four and five - enter the start and end time. In the last column enter the total number of units or event(s). 12
Claim Documentation Service Date List Diagnosis Code Number(s) Procedure code Start Time End Time Units/Event 13
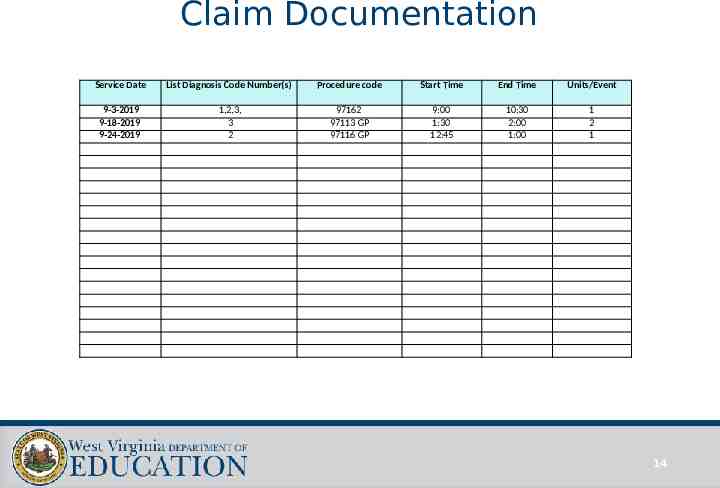
Claim Documentation Service Date List Diagnosis Code Number(s) Procedure code Start Time End Time Units/Event 9-3-2019 9-18-2019 9-24-2019 1,2,3, 3 2 97162 97113 GP 97116 GP 9:00 1:30 12:45 10:30 2:00 1:00 1 2 1 14
Procedure Code Changes Procedure Code 97532 GP is no longer valid. 15
Third Party Billing At times a student may be eligible for Medicaid as the secondary insurance. Medicaid is the payer of last resort for direct services (OT, PT, Speech, Audiology, Psychological, and Nursing). If the student has special transportation services, the direct billing should be submitted. The claim will be denied but will justify claiming transportation billing for that instructional day. Medicaid will pay ancillary services (TCM, personal care aide and special transportation) as the secondary insurance. Occasionally a student may be eligible for Medicaid under two numbers. In this case district’s should always use the primary Medicaid number. 16
Physical Therapy Assistant (PTA) PTAs can only bill for therapy when an Physical Therapist (PT) certified by the WV Board of Examiners is directly supervising. Directly supervising requires the Board Certified PT to be on site when the therapy is being provided. PTA progress/therapy logs are to be co-signed by the supervising OT for therapy dates that are billed for Medicaid. This only applies to dates when the PT was directly supervising the PTA. To make this clear to the person entering billing, the PT should initial the days that they provided direct supervision. PTAs can not bill for evaluations.
Signature and Credentials Staff who provided or directly supervised the service will sign the form and list credentials. For PTAs, the supervising PT must co-sign the billing form and initial specific claims directly supervised. An PT is considered to be directly supervising when in the building at the time of the service. Claims initialed by the PT can be submitted for billing.
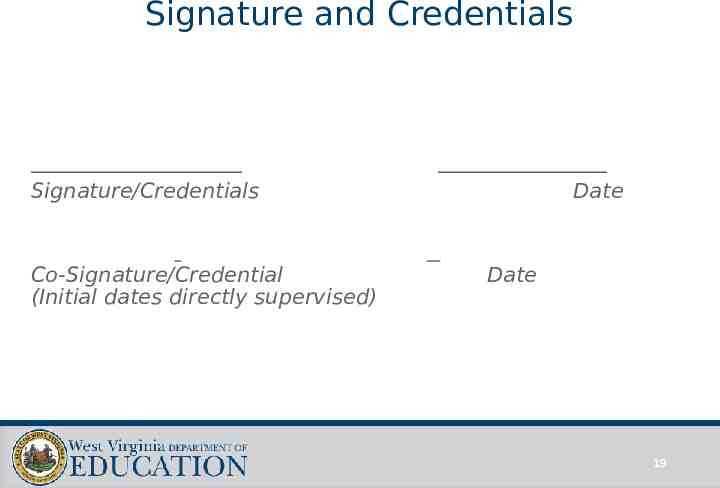
Signature and Credentials Signature/Credentials Co-Signature/Credential (Initial dates directly supervised) Date Date 19
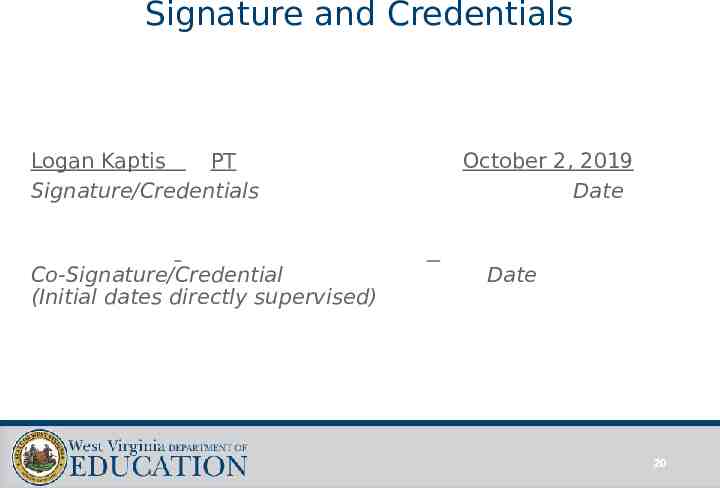
Signature and Credentials Logan Kaptis PT Signature/Credentials Co-Signature/Credential (Initial dates directly supervised) October 2, 2019 Date Date 20
Additional Documentation Progress/therapy logs will also be required. Original copies of progress/therapy logs must be on file in the special education central office. There is not a required form for documentation of progress/therapy logs.

Kelley Johnson – Coordinator Office of Special Education [email protected] 304-558-2696 ext 53539 WVDE Medicaid Website: https://wvde.us/special-education/Medic aid/