Care Plans Marianne Cosgrove, CRNA, DNAP, APRN
25 Slides488.00 KB
Care Plans Marianne Cosgrove, CRNA, DNAP, APRN
Care Plans Why? To prepare for the case Delineates procedure How it is performed Pt position Anesthetic considerations and plan for that specific type of surgery Anesthetic considerations for pt co-morbidities, meds To prepare for testing/boards! The initial portion of the care plan is done when you get your assignment before the procedure
Pre-surgical Care Plan Assignment: J. Doe, male, age 49 Laparoscopic cholecystectomy General anesthetic Now what?
Pre-surgical Care Plan, cont’d To be prepared for the AM of surgery: Planned procedure: In a synopsized form, explain the procedure to be done. Add details only if it directly impacts your anesthetic plan of care. If you are doing multiples of the same case, one cover sheet is acceptable for all cases scheduled; write the actual number of cases done that day on the cover sheet and attach each pt done to the procedure sheet before handing in
Pre-surgical Care Plan, cont’d Research the planned procedure Synopsize lap chole: i.e. Laparoscopic approaches are applied to an increasing number of procedures, including cholecystectomy, the surgical excision of the gallbladder. Surgery is performed for acute/chronic cholecystitis and/or cholelithiasis. Benefits of the laparoscopic approach to cholecystectomy include: smaller incision(s) reduced post-operative pain reduced incidence of ileus early ambulation shortened hospital stay earlier return to work and ADLs
Laparoscopic Cholecystectomy, cont’d Synopsis cont’d Operative technique involves the intraperitoneal insufflation of CO2 through a needle inserted through a small infraumbilical incision. Patient positioning in steep Reverse Trendelenberg with a left side-tilt facilitates operative exposure of the gallbladder. Pictures are OK but not necessary!! Check out Google images TM
Pre-surgical Care Plan, cont’d Anesthetic considerations for the procedure: The most important part of your preparation for the case “bullet” list format vs. paragraph may be easier to follow “chunking” of information allows the adult learner to retain information better
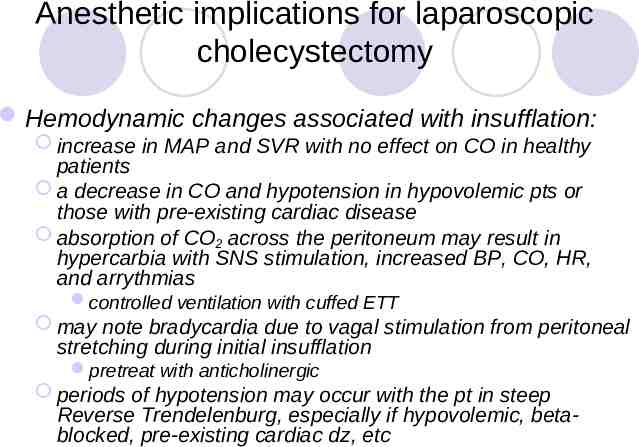
Anesthetic implications for laparoscopic cholecystectomy Hemodynamic changes associated with insufflation: increase in MAP and SVR with no effect on CO in healthy patients a decrease in CO and hypotension in hypovolemic pts or those with pre-existing cardiac disease absorption of CO2 across the peritoneum may result in hypercarbia with SNS stimulation, increased BP, CO, HR, and arrythmias controlled ventilation with cuffed ETT may note bradycardia due to vagal stimulation from peritoneal stretching during initial insufflation pretreat with anticholinergic periods of hypotension may occur with the pt in steep Reverse Trendelenburg, especially if hypovolemic, betablocked, pre-existing cardiac dz, etc
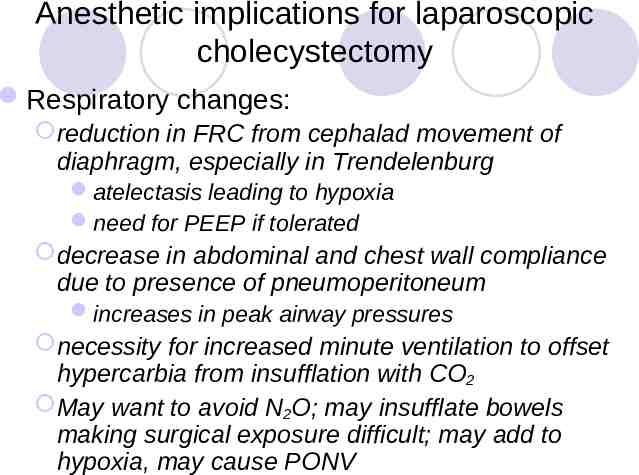
Anesthetic implications for laparoscopic cholecystectomy Respiratory changes: reduction in FRC from cephalad movement of diaphragm, especially in Trendelenburg atelectasis leading to hypoxia need for PEEP if tolerated decrease in abdominal and chest wall compliance due to presence of pneumoperitoneum increases in peak airway pressures necessity for increased minute ventilation to offset hypercarbia from insufflation with CO2 May want to avoid N2O; may insufflate bowels making surgical exposure difficult; may add to hypoxia, may cause PONV
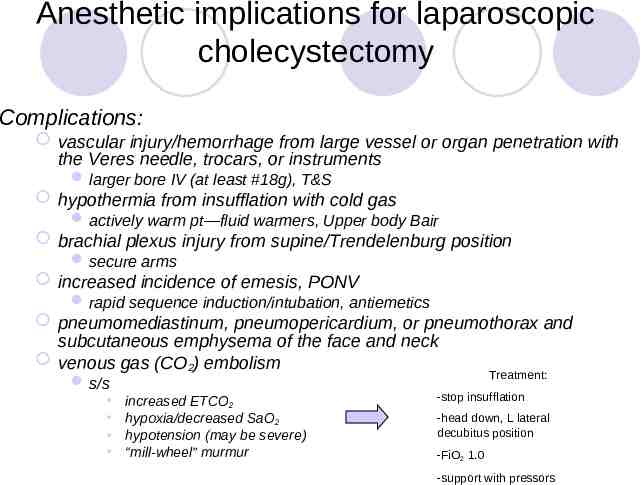
Anesthetic implications for laparoscopic cholecystectomy Complications: vascular injury/hemorrhage from large vessel or organ penetration with the Veres needle, trocars, or instruments larger bore IV (at least #18g), T&S hypothermia from insufflation with cold gas actively warm pt—fluid warmers, Upper body Bair brachial plexus injury from supine/Trendelenburg position secure arms increased incidence of emesis, PONV rapid sequence induction/intubation, antiemetics pneumomediastinum, pneumopericardium, or pneumothorax and subcutaneous emphysema of the face and neck venous gas (CO2) embolism Treatment: s/s increased ETCO2 hypoxia/decreased SaO2 hypotension (may be severe) “mill-wheel” murmur -stop insufflation -head down, L lateral decubitus position -FiO2 1.0 -support with pressors
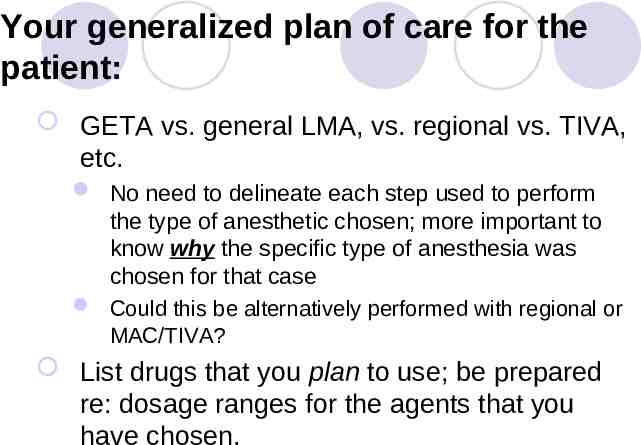
Your generalized plan of care for the patient: GETA vs. general LMA, vs. regional vs. TIVA, etc. No need to delineate each step used to perform the type of anesthetic chosen; more important to know why the specific type of anesthesia was chosen for that case Could this be alternatively performed with regional or MAC/TIVA? List drugs that you plan to use; be prepared re: dosage ranges for the agents that you have chosen.
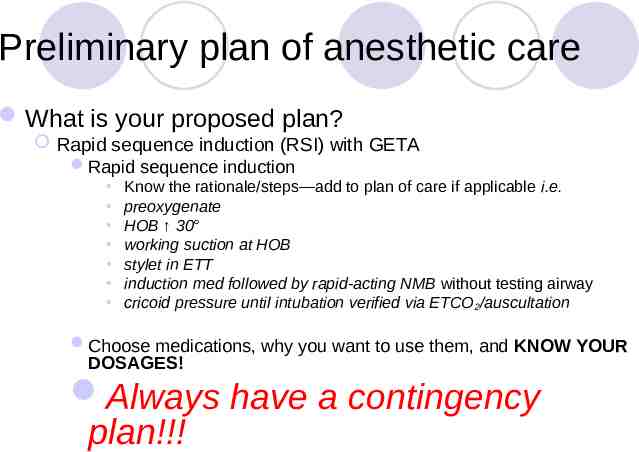
Preliminary plan of anesthetic care What is your proposed plan? Rapid sequence induction (RSI) with GETA Rapid sequence induction Know the rationale/steps—add to plan of care if applicable i.e. preoxygenate HOB 30 working suction at HOB stylet in ETT induction med followed by rapid-acting NMB without testing airway cricoid pressure until intubation verified via ETCO 2/auscultation Choose medications, why you want to use them, and KNOW YOUR DOSAGES! Always have a contingency plan!!!
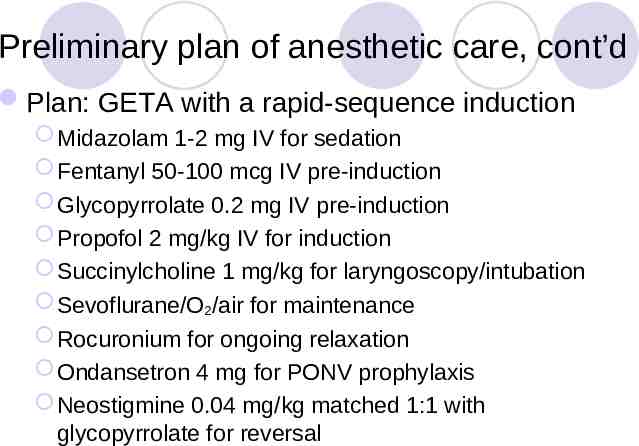
Preliminary plan of anesthetic care, cont’d Plan: GETA with a rapid-sequence induction Midazolam 1-2 mg IV for sedation Fentanyl 50-100 mcg IV pre-induction Glycopyrrolate 0.2 mg IV pre-induction Propofol 2 mg/kg IV for induction Succinylcholine 1 mg/kg for laryngoscopy/intubation Sevoflurane/O2/air for maintenance Rocuronium for ongoing relaxation Ondansetron 4 mg for PONV prophylaxis Neostigmine 0.04 mg/kg matched 1:1 with glycopyrrolate for reversal
References Must have at least two references 1 web reference is acceptable Hurford, W.E. Clinical Anesthesia Procedures of the Massachusetts General Hospital. Philadelphia, Lippincott, Williams & Wilkins, 2002. pp 318-320 Roizen MF, Fleisher, LA. The Essence of Anesthesia Practice. Philadelphia: W.B. Saunders Company, 2002. pg 384
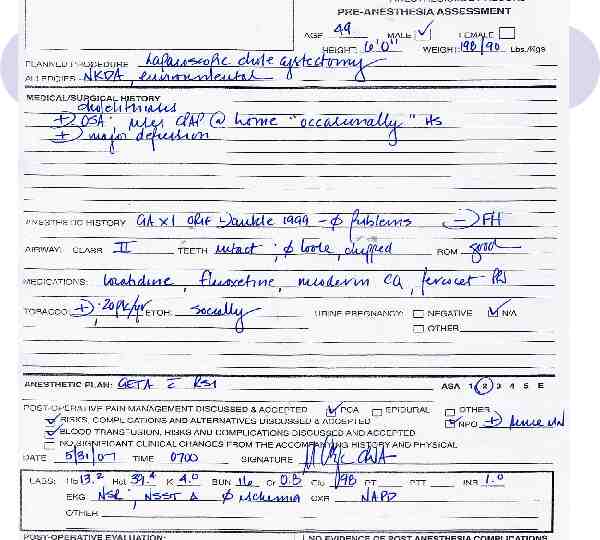
Day of surgery Now what? Patient contact is made, chart review is done Wt 198# / 90 kg Ht 6’0” Pt history remarkable for smoking, major depression, OSA Medications: Prozac, loratidine and percocet PRN, nicotine patch Labs all WNL transcribe all pertinent history onto care plan
During the case: note anesthetic technique used note medications/dosages used at the end of the care plan, you will list these meds as “actual”; note if there is a deviation from your original plan jot down any interesting, unexpected, untoward events (including mishaps!) anecdotal information will be added to finalize the CP before handing in—makes it more personalized and meaningful will end up with a “journal” of anesthetic experiences
After the case is finished: Revisit the care plan to review and add anesthetic implications for patient co-morbidities and meds, i.e. OSA-obstructive sleep apnea-a disorder in which excessive soft tissue in E B D L U !! D O SH LETE L U B the upper airway intermittently obstructs the airway during sleep. Prevalence is more common in obese pts. Pts report snoring, daytime somnolence, intellectual impairment, repeated AM headaches. More serious cases may lead to RVH from increases in pulmonary vascular resistance during apneic/hypoxic periods. May lead to cor pulmonale and eventual L-sided heart failure. Other resultant comorbidities may include HTN, cardiac arrythmias, polycythemia, and vascular disease. may be a difficult airway—both bag/mask ventilation, laryngoscopy/intubation, and after extubation have a variety of airway implements on hand may use a nasal airway before extubation may be sensitive to the respiratory depressant effects of opioids use opioids/sedatives with caution
After the case is finished, cont’d: Smoking Cigarette smoke contains 3000 identifiable constituents, many of which are toxic (most notable are nicotine, CO, and cyanide). Smokers have: increased airway irritability and secretions, decreased ciliary activity; potential for post-op pulmonary complications humidify gases lidocaine pre-intubation and extubation hydration ? use of anticholinergics ET suction before extubation ? deep extubation COPD I:E ratio which allows for longer expiratory phase watch PIP carboxyhemoglobinemia (COHb) Monitor SaO2 incidence of HTN, CAD, PVD, from SNS stimulation from nicotine ? use of β-blockers
Medications Fluoxetine (Prozac) A selective inhibitor of serotonin reuptake used to treat major depression, OCD, bulemia anesthetic considerations: pt may be anxious use of benzodiazepenes pt may have extrapyramidal reactions avoid dopaminergic blockers (droperidol, metoclopramide) serotonin syndrome with concomitant use of MAOIs, tricyclics, meperidine monitor temperature avoid use of meperidine SIADH watch U/O if applicable may inhibit cytochrome P-450 and potentiate the effects of phenytoin, benzos, beta-blockers due to increased plasma levels of these drugs
Finally Please complete these sections before re-submitting to your preceptor for signature Post-op visit *If the pt is in STS, make an attempt to re-connect before their discharge to home; assess for pain, PONV, untoward reaction to anesthesia, etc. extremely important
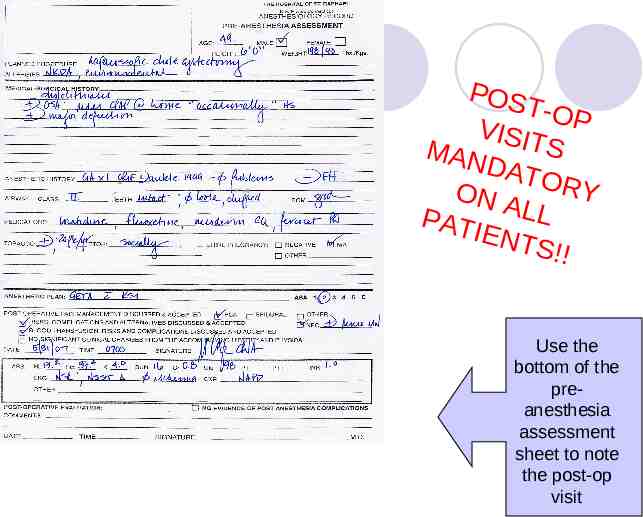
POS T-OP VISIT S MAN DAT ON A ORY PATI LL ENT S!! Use the bottom of the preanesthesia assessment sheet to note the post-op visit
Hints for success Save all of your co-morbidities and medications in a file folder on your computer may re-submit on future care plans—work will already be done! do not “trade” with peers want to build your own library Ultimate goal—to formulate a plan of care off of the top of your head
Care Plan CHECKLIST Keeps track of cases Based on the CCNAs outline for boards All case types not mandatory but will give you an idea as to what needs to be focused on for studying later Mandatory to have 3 OB rotation (1 C/S, 1 co-morbidity, 1 laboring epidural/vaginal delivery and 1 care plan/WEEK from rotation sites
Care Plan CHECKLIST Before graduation, you must have at least one CP completed for each of the categories listed Will upload/submit to the school as an electronic file, either separately or as a component of your e-portfolio