Care of the Post-Bariatric Patient Fall Update in Family Medicine
76 Slides885.93 KB
Care of the Post-Bariatric Patient Fall Update in Family Medicine l October 20-21, 2016 l Andrew Kraftson, MD
Clinical Tips and Pearls from the Post-Bariatric Surgery Clinic Fall Update in Family Medicine l October 20-21, 2016 l Andrew Kraftson, MD

Disclosure(s): co-investigator for a clinical study sponsored by Nestle (Optifast). Fall Update in Family Medicine l October 20-21, 2016 l Andrew Kraftson, MD
How is follow-up of the bariatric patient structured?
How is follow-up of the bariatric patient structured? At my institution? At yours?
Post-Bariatric Endocrinology Clinic Goal: provide structured life-long follow-up for all the post-bariatric patients of the University of Michigan and act as a referral center for patients from other institutions. Team: 3 endocrinologists, 2 dieticians, 4 bariatric surgeons, 2 physician assistants (& close referral contact with 2 therapists, 3 gastroenterologists and 3 plastic surgeons as well as physical therapy and exercise physiology)

However, offering long-term follow-up is atypical for many local/area bariatric centers.

For most, long-term follow-up occurs with the local primary care physician/provider.
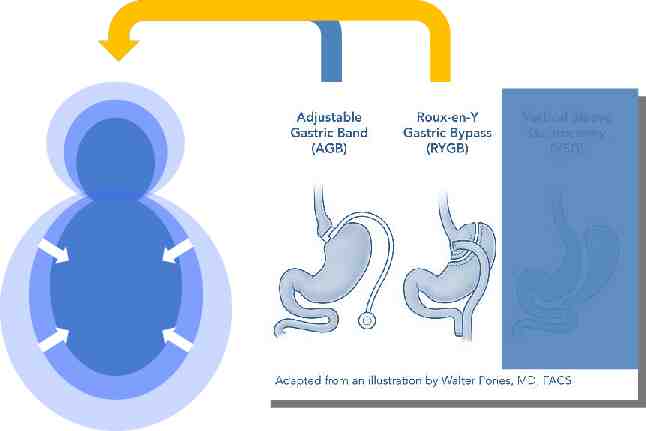
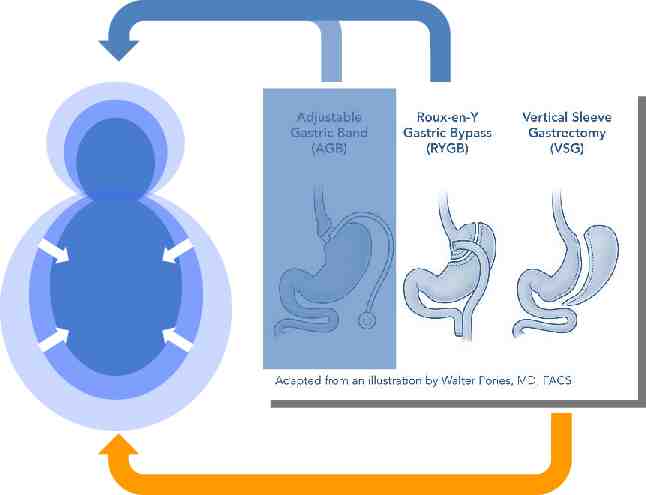
What types of surgery will we be discussing?
Selection of the Bariatric Patient
Remember that effective pre-bariatric work will make your post-bariatric job easier.
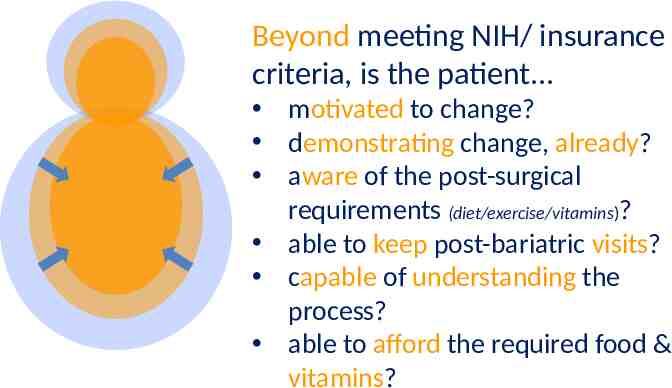
Beyond meeting NIH/ insurance criteria, is the patient.
Beyond meeting NIH/ insurance criteria, is the patient. motivated to change? demonstrating change, already? aware of the post-surgical requirements (diet/exercise/vitamins)? able to keep post-bariatric visits? capable of understanding the process? able to afford the required food & vitamins?
If NOT. motivated to change? demonstrating change, already? aware of the postsurgical requirements (diet/exercise/ vitamins)? able to keep postbariatric visits? capable of understanding the process? able to afford the required food & vitamins? Then NO surgery. Postpone surgery & develop action plan. Provide education of expectations. Address the underlying issue(s). NO surgery until addressed. Involve social work/financial planning.
Some bariatric programs will do a good job of addressing these issues, others will not.
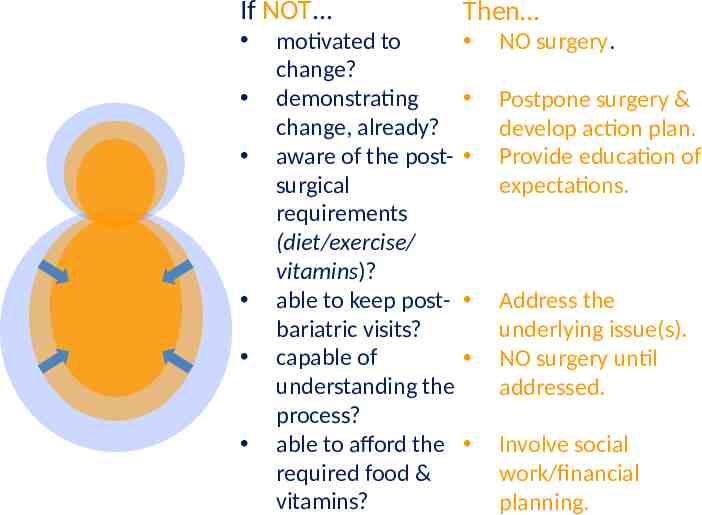
You will know the patient better than the bariatric program – make sure these issues are addressed!
Post-Bariatric Complications

Many are possible

A well-structured visit will help you screen for problems.
Here is an example of my workflow.
Weight Management *recidivism prevention
Weight Management Prior to walking in the room Determine the Pre-surgical weight (Peak) Determine the “Ideal Body Weight” (IBW) Determine the “Excess Body Weight” (EBW) EBW Peak - IBW
Weight Management Prior to walking in the room Obtain the current weight. Determine the % EBW lost (Peak) – (current) EBW

Weight Management Prior to walking in the room Compare to projections*: At 6 months post: expect 30-40% EBW loss** At 12 months post: expect RYGB: 55-70% Sleeve: 45-60% *Can be guided by Michigan Bariatric Surgery Collaborative database comparison **Note: 100% EBW loss is NOT the expectation!
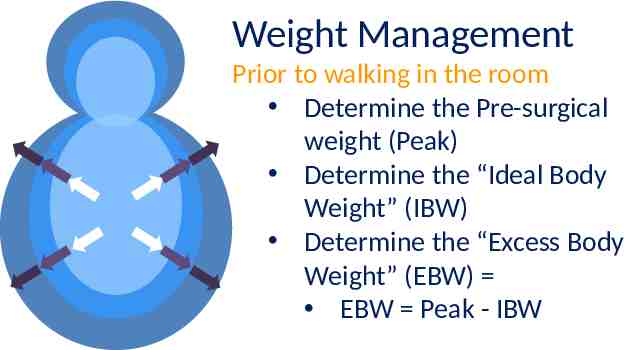
Weight Management Prior to walking in the room This assessment will help direct the visit: Is weight loss too rapid and concerning? Is the rate of weight loss meeting projections? Is the weight loss rate wellbelow projections?
Weight Management Once with the patient The patient’s self-assessment of weight progress should be obtained prior to discussing your assessment of the weight trajectory. This provides information about insight and can help with the feedback process.
Weight Management Once with the patient Diet: You may not have time to conduct a complete dietary assessment. If you have concerns about under/over-nutrition, refer the patient to a dietician.
Weight Management Once with the patient Diet: Otherwise, if weight loss meets projections, try to do a general assessment of dietary composition (well-balanced or not?)
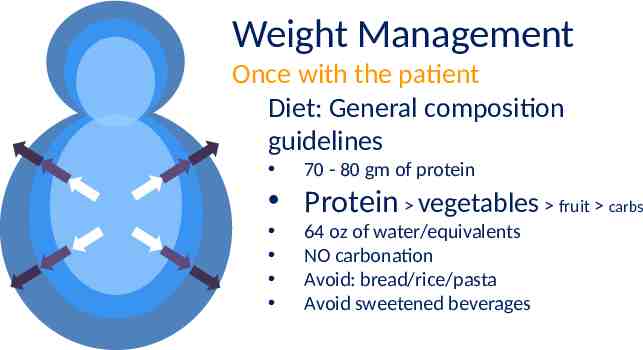
Weight Management Once with the patient Diet: General composition guidelines 70 - 80 gm of protein Protein vegetables fruit carbs 64 oz of water/equivalents NO carbonation Avoid: bread/rice/pasta Avoid sweetened beverages
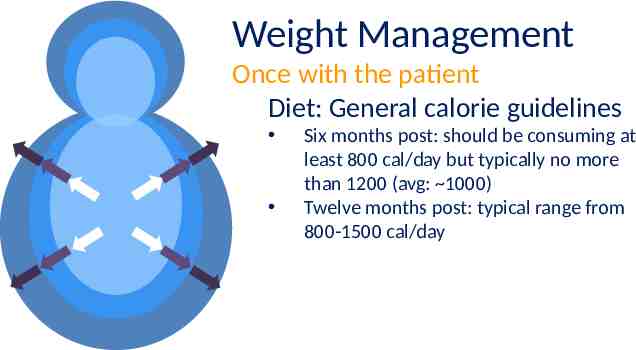
Weight Management Once with the patient Diet: General calorie guidelines Six months post: should be consuming at least 800 cal/day but typically no more than 1200 (avg: 1000) Twelve months post: typical range from 800-1500 cal/day

Weight Management Once with the patient Diet: Red Flags Slow rate of loss from 2 months post- to 6 months post-op. Ill-defined/unrestricted snacking on: carbheavy snacks (eg: crackers), nuts (HIGH caloric density), sweetened beverages. Lack of vegetables/fruit. Prolonging meals to “get around” the physical barriers/restrictions. Resumption of old habits. *But also watch for under/malnutrition!
Vitamin Management *deficiency prevention
If your patient had surgery with the goal of getting off all “pills”, s/he is in for a disappointment

The next step in the visit is to assess the degree of adherence to vitamin supplementation recommendations.
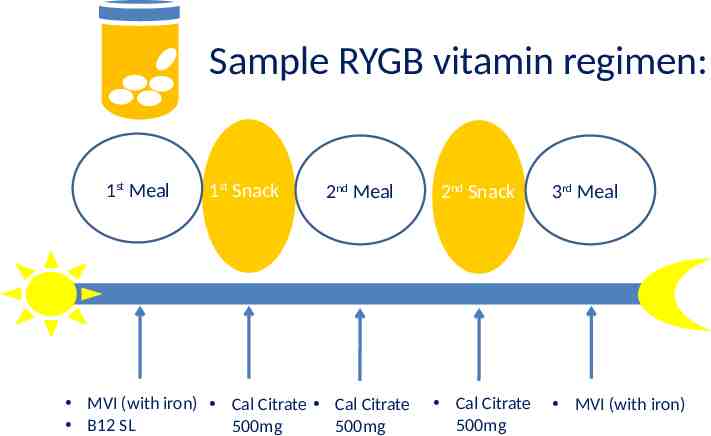
Sample RYGB vitamin regimen: 1st Meal 1st Snack 2nd Meal MVI (with iron) Cal Citrate Cal Citrate B12 SL 500mg 500mg 2nd Snack Cal Citrate 500mg 3rd Meal MVI (with iron)

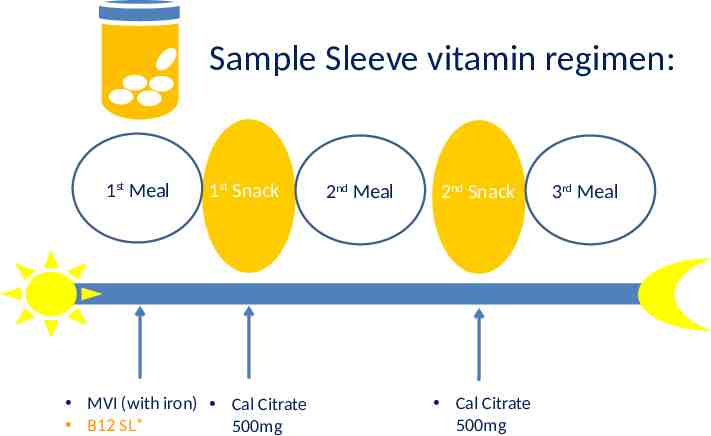
Sample Sleeve vitamin regimen: 1st Meal 1st Snack MVI (with iron) Cal Citrate B12 SL* 500mg 2nd Meal 2nd Snack Cal Citrate 500mg 3rd Meal

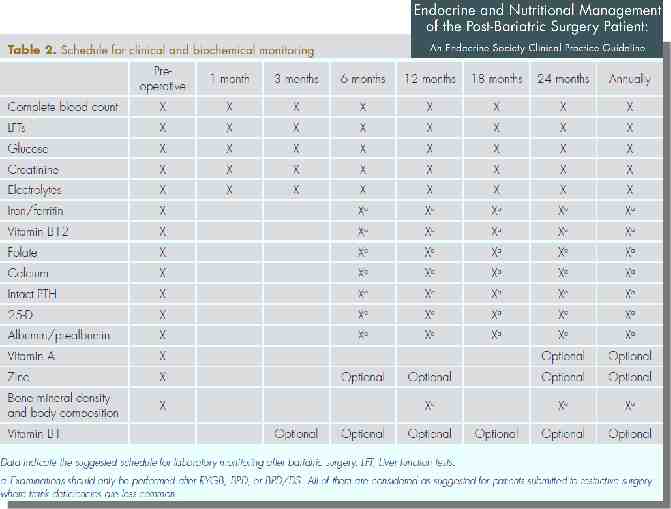
Biochemical Monitoring:
Quick Tips: For your self-study – we do not have time to cover them in the presentation, today. SELF-STUDY
Quick Tips: Calcium: Please do not discontinue supplements just because the lab results are normal. We are trying to prevent problems! Calcium type: Carbonate (eg: Caltrate): 10% is absorbed and it can increase the risk of kidney stones. Citrate (eg: Citracal): USE this! 40-50% is absorbed Should not increase stone risk Does not require food or gastric acid for absorption There are formulation options – but need to watch that they are not taking carbonate. SELF-STUDY

Quick Tips: Calcium: Reasons to discontinue: Frank hypercalcemia Complete intolerance to all formulations (unable to afford them) – though some insurers (and some medicaid options?) may provide coverage for calcium. NOT reasons to discontinue: Normal calcium levels Kidney stones: most post-bariatric stones are cal-oxalate. Holding calcium may cause calcium deficiency and this will precipitate oxalate! SELF-STUDY
Quick Tips: Vitamin D: Many will obtain adequate amounts through: diet and the calcium D (combination) supplements. However, for a significant number of patients, deficiency will occur despite these efforts (especially in Michigan!) SELF-STUDY
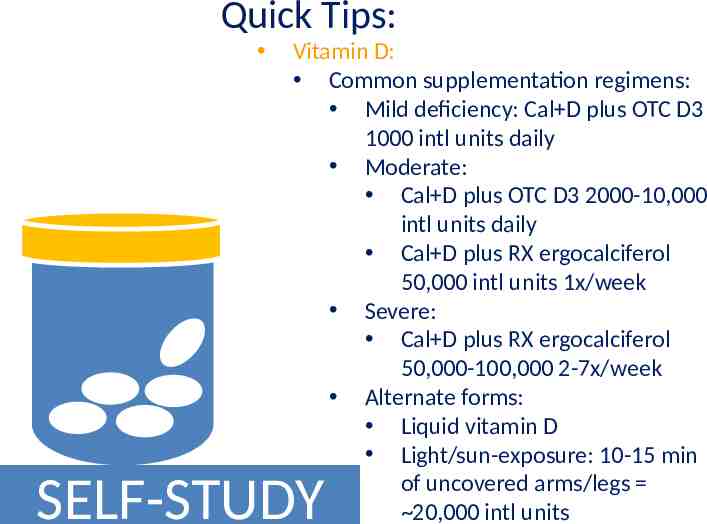
Quick Tips: Vitamin D: Common supplementation regimens: Mild deficiency: Cal D plus OTC D3 1000 intl units daily Moderate: Cal D plus OTC D3 2000-10,000 intl units daily Cal D plus RX ergocalciferol 50,000 intl units 1x/week Severe: Cal D plus RX ergocalciferol 50,000-100,000 2-7x/week Alternate forms: Liquid vitamin D Light/sun-exposure: 10-15 min of uncovered arms/legs 20,000 intl units SELF-STUDY
Quick Tips: Vitamin D: Example of a common replacement error I see made: “Jane Smith” was deficient despite being on Cal D and vit D3 1000 intl units daily. Her PCP decides to raise her level by prescribing ergo 50,000 intl units weekly x 8 weeks. However, after completion she is then advised to go back to the old D3 1000 for maintenance. This will usually result in a return to the problem. RAISE the maintenance dose after you have “tanked her up”! SELF-STUDY
Quick Tips: Vitamin D: Example of a common lab interpretation error I see: “Jane Smith” has labs drawn and was found to have elevated PTH levels. Her physician jumps to the conclusion that she has pathologic hyperparathyroidism. Remember: interpret in the CONTEXT of calcium and 25hydroxyvitamin D SELF-STUDY
Quick Tips: Vitamin D: Remember: interpret in the CONTEXT of calcium and 25- hydroxyvitamin D: Normal calcium with low 25HD appropriate secondary hyperparathyroidism need to replace D Low calcium with normal 25HD appropriate secondary hyperparathyroidism need to take/replace calcium. Low/normal calcium –orlow/normal 25HD try to increase the levels and see the effect on the PTH HIGH calcium and high PTH PTHdependent hyperparathyroidism SELF-STUDY
Quick Tips: B12: You cannot become B12 toxic so there is generally no need to intervene when levels are elevated – let them continue on the regimen. Use sublingual B12 instead of oral B12 to avoid issues with gut absorption. Sublingual B12 is CHEAP! ( 1/MONTH) Q: Why do I recommend sleeve patients take B12? A: We analyzed our patient population data and saw a general trend of falling B12 levels – some to frankly low. Therefore, we made the programmatic decision to institute prophylactic therapy. SELF-STUDY
Quick Tips: B12: IM injections: For deficiency despite SL B12 To improve adherence Per patient preference I often teach my patients to selfadminister. However, you can bring them to the clinic for injections. SELF-STUDY
Quick Tips: Iron: I encourage patients to take ironcontaining MVIs Most senior (eg: centrum silver) MVIs do NOT contain iron If deficient despite dietary iron and iron-containing MVI, then I move to replacement. I start with oral iron and encourage patients to try different ones if there are tolerance issues. SELF-STUDY
Quick Tips: Iron: Iron infusion therapy should be used in cases of refractory iron deficiency anemia (despite oral therapy –or- if intolerant to oral therapy). This is usually facilitated by: A post-bariatric physician A hematologist A gastroenterologist SELF-STUDY
After assessing the diet/activity progress and the vitamin regimen adherence, I will then move to specific complication screening.
“How are you and others adapting to the changes you are going through?”
Screens for: Mood disorder Sabotage Relationship strain Feelings of isolation Domestic abuse
“How well are your bowels moving (frequency, consistency)? Any abdominal discomfort? Any nausea/ vomiting? Any food intolerances?”
Screens for: Constipation (& possibly related to pelvic floor dysfunction) SIBO Biliary disease Dumping (if applicable)
“Ever feel episodes of shakiness, sweating, anxiety – particularly after eating?”

Screens for: Post-bariatric hypoglycemia Can occur in up to 30% of malabsorptive surgeries (like RYGB) Typical onset is 1 year post-surgery
Post-bariatric hypoglycemia: Detection Whipple’s triad Get objective evidence with glucose meter Symptoms and values must correlate
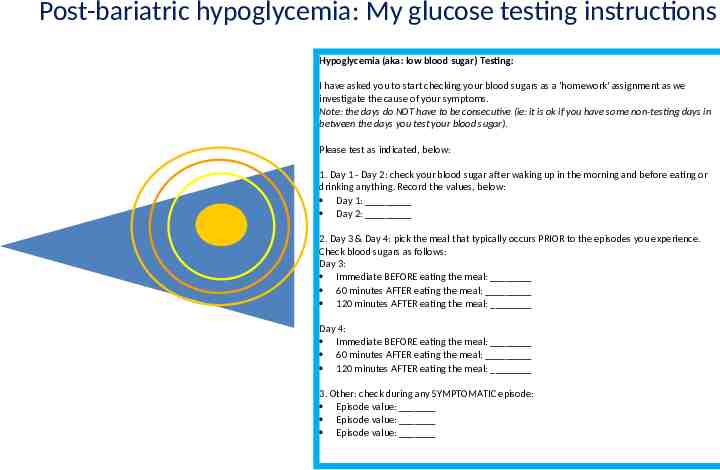
Post-bariatric hypoglycemia: My glucose testing instructions Hypoglycemia (aka: low blood sugar) Testing: I have asked you to start checking your blood sugars as a 'homework' assignment as we investigate the cause of your symptoms. Note: the days do NOT have to be consecutive (ie: it is ok if you have some non-testing days in between the days you test your blood sugar). Please test as indicated, below: 1. Day 1 - Day 2: check your blood sugar after waking up in the morning and before eating or drinking anything. Record the values, below: Day 1: Day 2: 2. Day 3 & Day 4: pick the meal that typically occurs PRIOR to the episodes you experience. Check blood sugars as follows: Day 3: Immediate BEFORE eating the meal: 60 minutes AFTER eating the meal: 120 minutes AFTER eating the meal: Day 4: Immediate BEFORE eating the meal: 60 minutes AFTER eating the meal: 120 minutes AFTER eating the meal: 3. Other: check during any SYMPTOMATIC episode: Episode value: Episode value: Episode value:
Post-bariatric hypoglycemia: Detection “Dynamic” testing can be performed for confirmation (eg: mixedmeal tolerance testing but NOT oral glucose tolerance testing)
Post-bariatric hypoglycemia: Detection Patient should NOT have fasting or fastingnocturnal episodes. If s/he does, need to rule out other causes (insulinoma)
Post-bariatric hypoglycemia: Management Dietary changes cornerstone of therapy Medications can be considered if this is insufficient
Post-bariatric hypoglycemia: Management Dietary changes: AVOID simple carbs. Carbs consumed should be complex. Have protein with each meal/snack Eat 3 meals 3 snacks per day (reg spaced) Can try corn-starch 1-3x/day

Post-bariatric hypoglycemia: Management Medications: Acarbose: first line Verapamil: as monotherapy or added to acarbose Diazoxide: less tolerable for elderly Octreotide Other (anecdotal experiences)
Post-bariatric hypoglycemia: Management Surgical management (ie: “reversal” and/or partial pancreatectomy) had been considered as “last resort” but has, itself, fallen out-of-favor; even for severe cases.

“Regarding diabetes, are you still taking any medications? Are you checking your blood sugars? Have you had any symptoms of high and/or low sugars?”

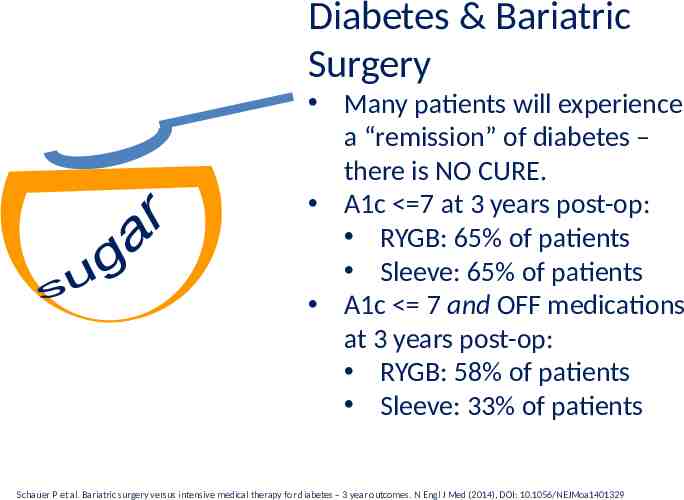
Diabetes & Bariatric Surgery Many patients will experience a “remission” of diabetes – there is NO CURE. A1c 7 at 3 years post-op: RYGB: 65% of patients Sleeve: 65% of patients A1c 7 and OFF medications at 3 years post-op: RYGB: 58% of patients Sleeve: 33% of patients Schauer P et al. Bariatric surgery versus intensive medical therapy for diabetes – 3 year outcomes. N Engl J Med (2014), DOI: 10.1056/NEJMoa1401329

Diabetes & Bariatric Surgery IF your patient has poor glycemic control after surgery, you should analyze WHY. Schauer P et al. Bariatric surgery versus intensive medical therapy for diabetes – 3 year outcomes. N Engl J Med (2014), DOI: 10.1056/NEJMoa1401329
Other Issues (beyond the scope of this talk): Risk of addiction transference

Other Issues (beyond the scope of this talk): Risk of bone thinning/ osteoporosis
Other Issues (beyond the scope of this talk): Risk of excess skin-related issues.
Summary: Screen patients carefully. Familiarize yourself with the post-surgical recommendations. If the bariatric program does not provide lifetime follow-up, conduct a visit dedicated to post-bariatric care. Be aware of possible complications and screen. Fall Update in Family Medicine l October 20-21, 2016 l Andrew Kraftson, MD

Thank you for your attention! Questions? Fall Update in Family Medicine l October 20-21, 2016 l Andrew Kraftson, MD