CANCERASSOCIATED THROMBOSIS FOR ONCOLOGY CLINICIANS A d r i a n Ye e,
33 Slides664.25 KB
CANCERASSOCIATED THROMBOSIS FOR ONCOLOGY CLINICIANS A d r i a n Ye e, M D, F RC PC, M E T H e mato lo g ist , V ic to ri a B C
LEARNING OBJECTIVES Identify risk factors and mitigate the risks. Develop a management approach. Develop an individualized management plan for patients in rural and remote 20XX regions. P R E S E N TAT I O N T I T L E 2
TERRITORIAL ACKNOWLEDGEMEN T A V I E W O F F O RT V I C T O R I A A S SEEN FROM THE SONGHEES V I L L A G E , 1 8 5 1 . S K E TC H BY L I N T O N PA L M E R . R OYA L P R E S E N TAT I O N T I T L E 3
CONFLICT OF INTEREST I declare no confl ict of interest relevant to this presentation.
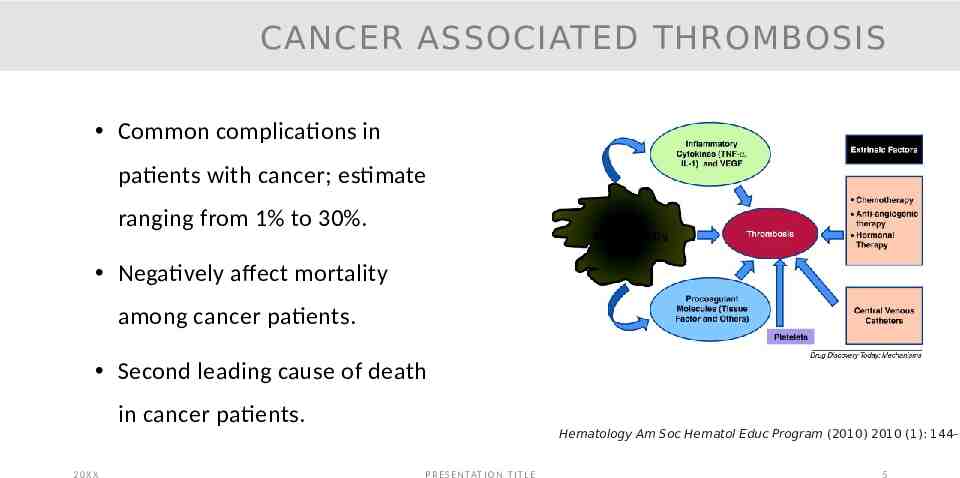
CANCER ASSOCIATED THROMBOSIS Common complications in patients with cancer; estimate ranging from 1% to 30%. Negatively affect mortality among cancer patients. Second leading cause of death in cancer patients. 20XX Hematology Am Soc Hematol Educ Program (2010) 2010 (1): 144–1 P R E S E N TAT I O N T I T L E 5
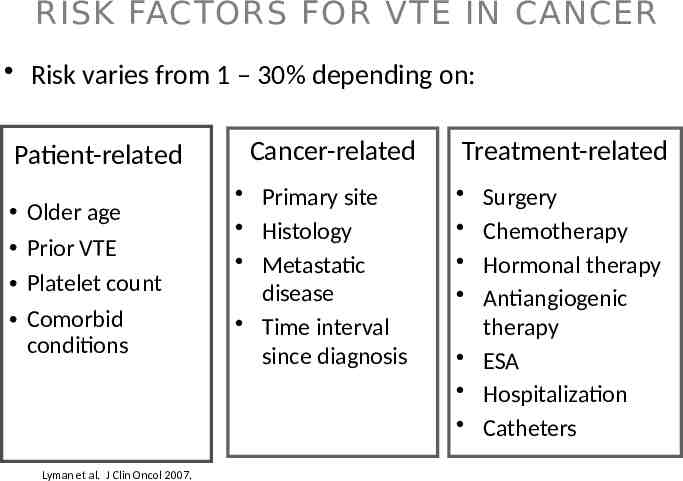
RISK FACTORS FOR VTE IN CANCER Risk varies from 1 – 30% depending on: Patient-related Older age Prior VTE Platelet count Comorbid conditions Lyman et al. J Clin Oncol 2007. Cancer-related Primary site Histology Metastatic disease Time interval since diagnosis Treatment-related Surgery Chemotherapy Hormonal therapy Antiangiogenic therapy ESA Hospitalization Catheters
CASE 1 A 47-year-old patient has a history of increasing abdominal bloating. CT was consistent with an adnexal mass. She has been referred to GyneOncology for surgery due to the concern of 20XX ovarian/fallopian tube cancer. P R E S E N TAT I O N T I T L E 7
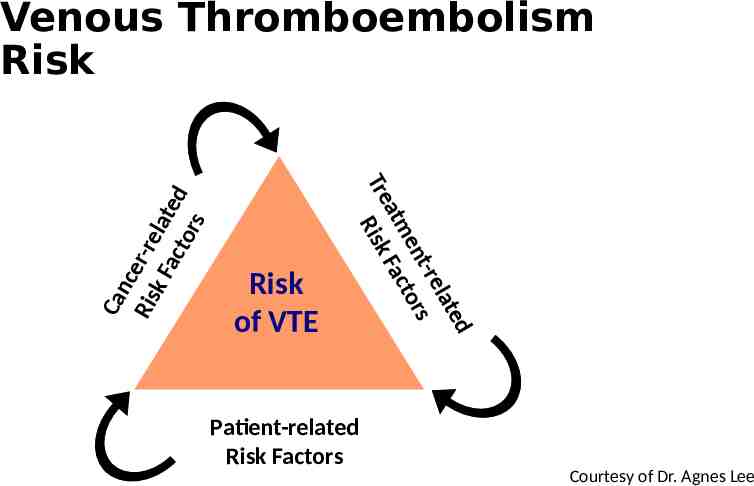
Risk of VTE ed lat t-re en tors atm Fac Tre Risk Ca nce Ris r-re k F lat a ct e d ors Venous Thromboembolism Risk Patient-related Risk Factors Courtesy of Dr. Agnes Lee 8
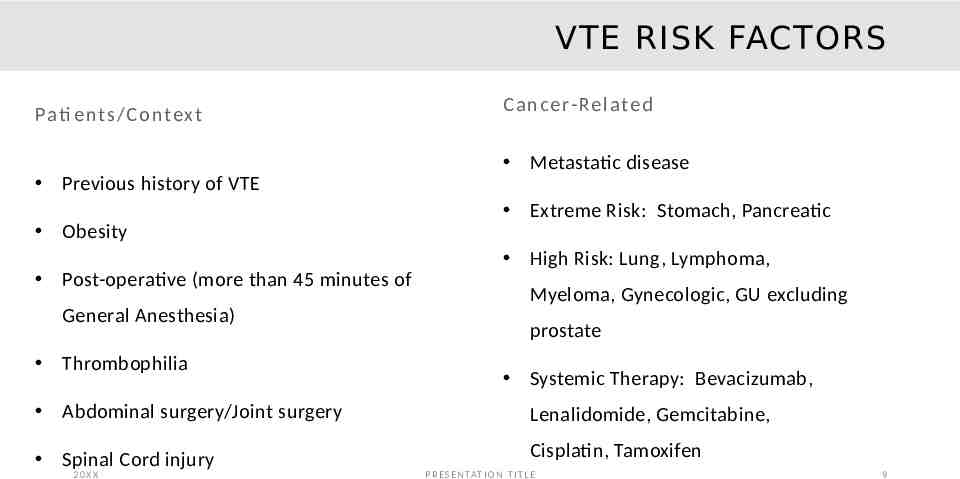
VTE RISK FACTORS Pati e nt s/ C o ntex t Previous history of VTE Obesity Post-operative (more than 45 minutes of General Anesthesia) Thrombophilia C a n c e r-Re late d Metastatic disease Extreme Risk: Stomach, Pancreatic High Risk: Lung, Lymphoma, Myeloma, Gynecologic, GU excluding prostate Systemic Therapy: Bevacizumab, Abdominal surgery/Joint surgery Lenalidomide, Gemcitabine, Spinal Cord injury Cisplatin, Tamoxifen 20XX P R E S E N TAT I O N T I T L E 9
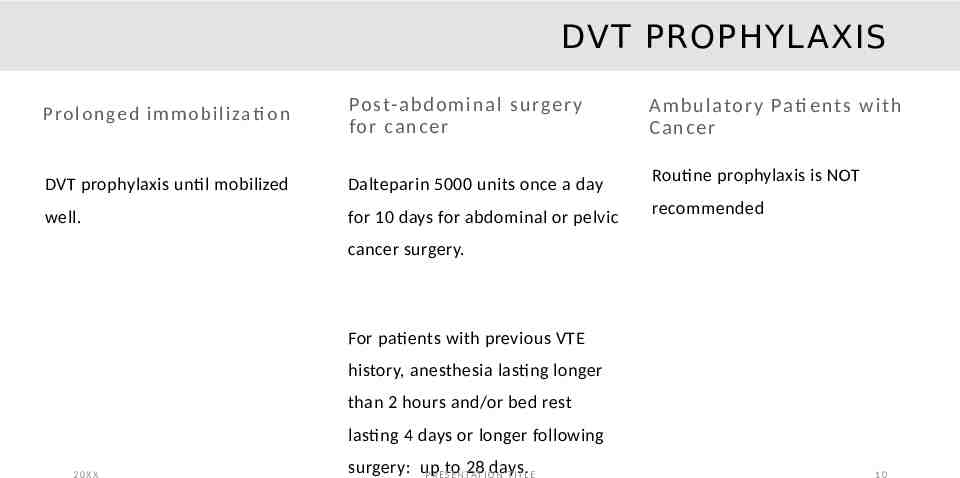
DVT PROPHYLAXIS Pro l o n ge d i m m o b i l i zati o n Po st-a bd o m in a l surge r y fo r ca n c e r A m b u lato r y Pati e nt s w i t h C a n c e r DVT prophylaxis until mobilized Dalteparin 5000 units once a day Routine prophylaxis is NOT well. for 10 days for abdominal or pelvic recommended cancer surgery. For patients with previous VTE history, anesthesia lasting longer than 2 hours and/or bed rest lasting 4 days or longer following 20XX surgery: up 28I Odays P R E to S E N TAT N T I T L. E 10
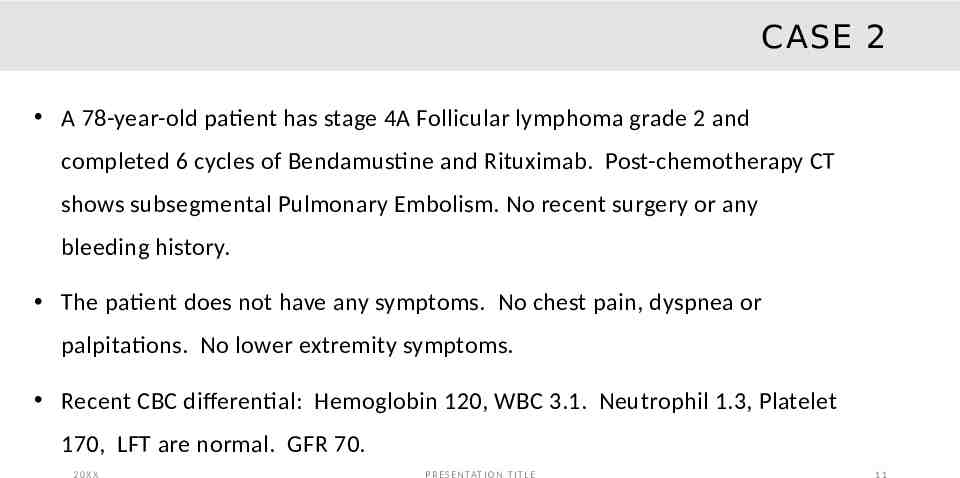
CASE 2 A 78-year-old patient has stage 4A Follicular lymphoma grade 2 and completed 6 cycles of Bendamustine and Rituximab. Post-chemotherapy CT shows subsegmental Pulmonary Embolism. No recent surgery or any bleeding history. The patient does not have any symptoms. No chest pain, dyspnea or palpitations. No lower extremity symptoms. Recent CBC differential: Hemoglobin 120, WBC 3.1. Neutrophil 1.3, Platelet 170, LFT are normal. GFR 70. 20XX P R E S E N TAT I O N T I T L E 11
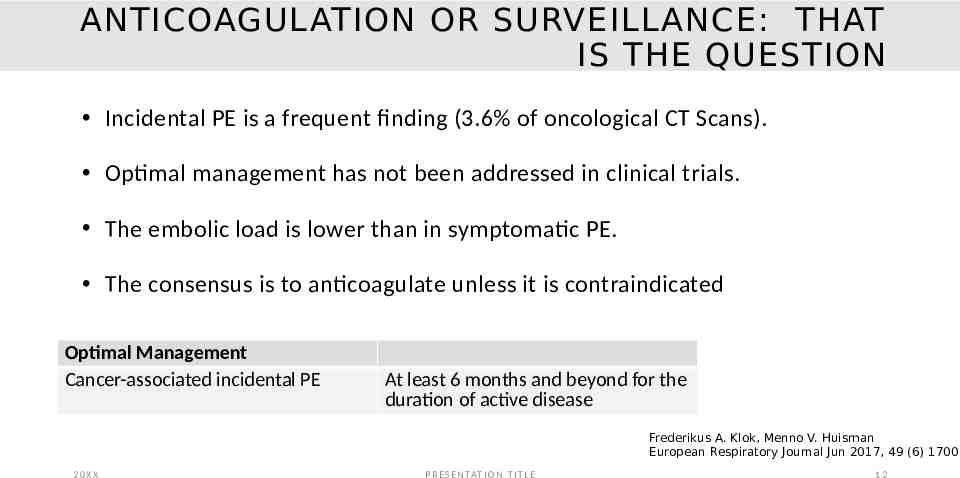
ANTICOAGULATION OR SURVEILLANCE: THAT IS THE QUESTION Incidental PE is a frequent finding (3.6% of oncological CT Scans). Optimal management has not been addressed in clinical trials. The embolic load is lower than in symptomatic PE. The consensus is to anticoagulate unless it is contraindicated Optimal Management Cancer-associated incidental PE At least 6 months and beyond for the duration of active disease Frederikus A. Klok, Menno V. Huisman European Respiratory Journal Jun 2017, 49 (6) 17002 20XX P R E S E N TAT I O N T I T L E 12
CASE 2: SELECTION OF ANTICOAGULANT 69-years-old patients with metastatic colon cancer and on Capecitabine. He has type 2 diabetes and hypertension He has worsening shortness of breath and pleuritic chest pain On examination, he is stable. Chest examination is normal. Cardiac examination is normal Had an urgent Spiral CT – bilateral Pulmonary Embolism. 20XX P R E S E N TAT I O N T I T L E 13
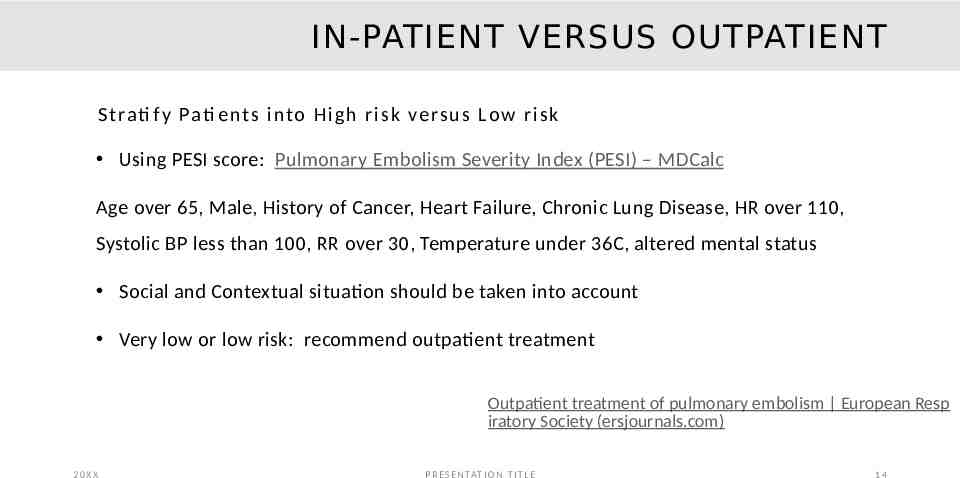
IN-PATIENT VERSUS OUTPATIENT S t rati f y Pati e nt s i nto H ig h r is k versu s Low r i sk Using PESI score: Pulmonary Embolism Severity Index (PESI) – MDCalc Age over 65, Male, History of Cancer, Heart Failure, Chronic Lung Disease, HR over 110, Systolic BP less than 100, RR over 30, Temperature under 36C, altered mental status Social and Contextual situation should be taken into account Very low or low risk: recommend outpatient treatment Outpatient treatment of pulmonary embolism European Resp iratory Society (ersjournals.com) 20XX P R E S E N TAT I O N T I T L E 14
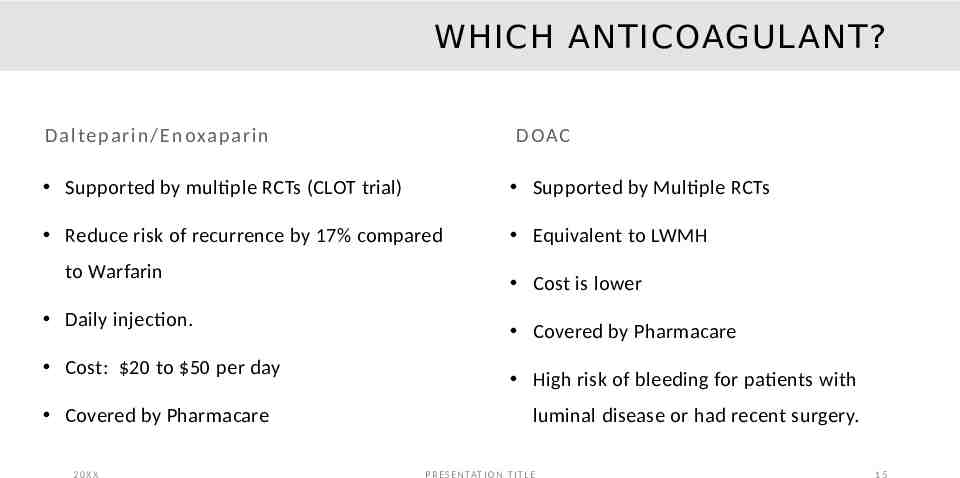
WHICH ANTICOAGULANT? D a l te pa r in / E n oxap ar in D OAC Supported by multiple RCTs (CLOT trial) Supported by Multiple RCTs Reduce risk of recurrence by 17% compared Equivalent to LWMH to Warfarin Daily injection. Cost: 20 to 50 per day Covered by Pharmacare 20XX Cost is lower Covered by Pharmacare High risk of bleeding for patients with luminal disease or had recent surgery. P R E S E N TAT I O N T I T L E 15
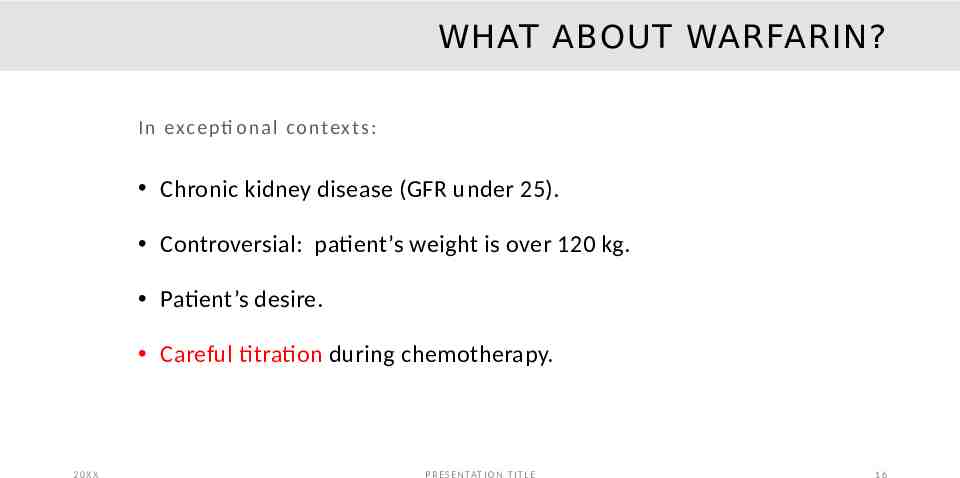
WHAT ABOUT WARFARIN? In exc e pti o n a l co ntex t s: Chronic kidney disease (GFR under 25). Controversial: patient’s weight is over 120 kg. Patient’s desire. Careful titration during chemotherapy. 20XX P R E S E N TAT I O N T I T L E 16
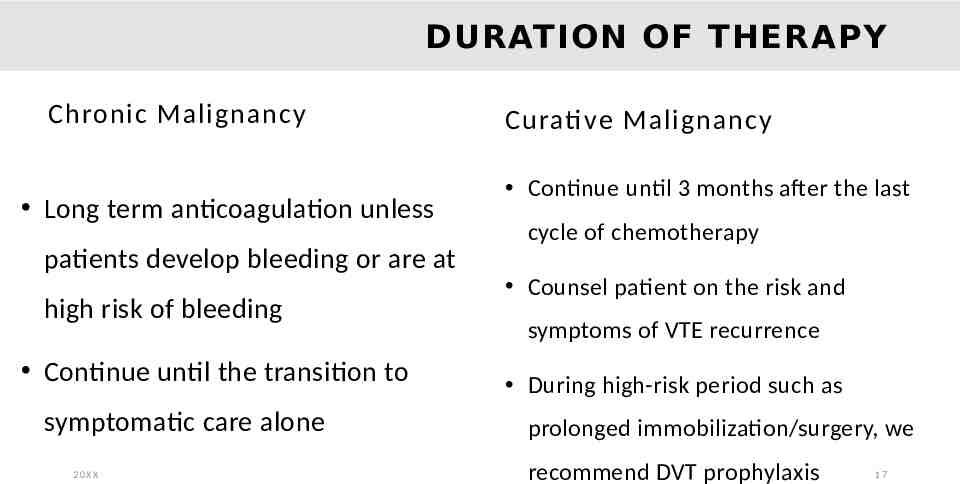
DURATION OF THERAPY Chronic Malignancy Long term anticoagulation unless patients develop bleeding or are at high risk of bleeding Continue until the transition to symptomatic care alone 20XX Curati ve Malignancy Continue until 3 months after the last cycle of chemotherapy Counsel patient on the risk and symptoms of VTE recurrence During high-risk period such as prolonged immobilization/surgery, we recommend DVT prophylaxis 17
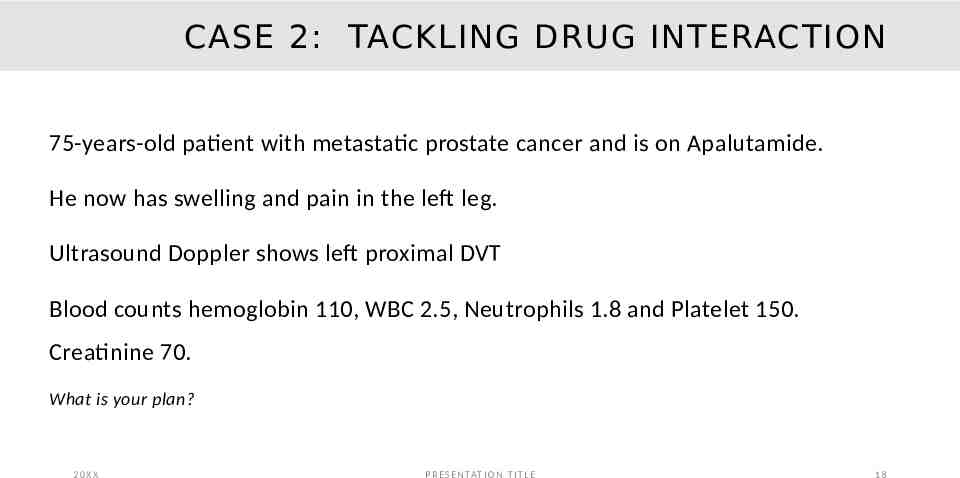
CASE 2: TACKLING DRUG INTERACTION 75-years-old patient with metastatic prostate cancer and is on Apalutamide. He now has swelling and pain in the left leg. Ultrasound Doppler shows left proximal DVT Blood counts hemoglobin 110, WBC 2.5, Neutrophils 1.8 and Platelet 150. Creatinine 70. What is your plan? 20XX P R E S E N TAT I O N T I T L E 18
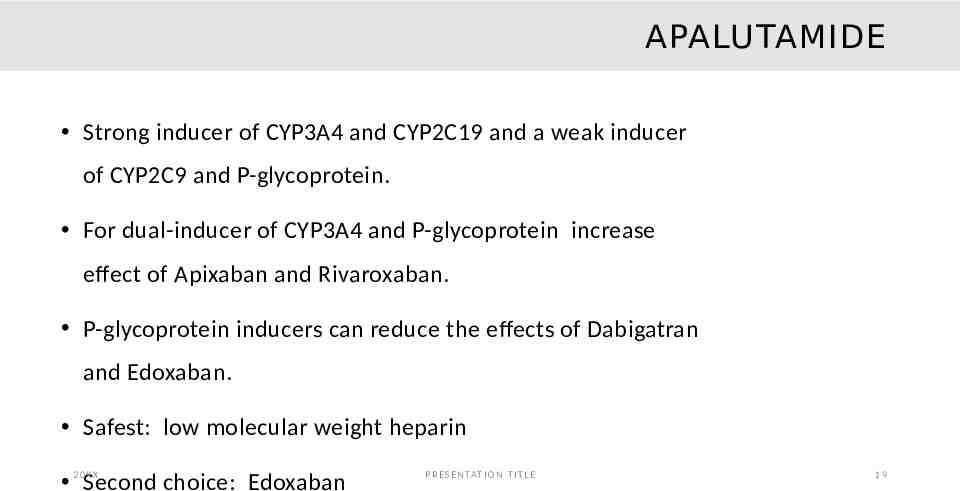
APALUTAMIDE Strong inducer of CYP3A4 and CYP2C19 and a weak inducer of CYP2C9 and P-glycoprotein. For dual-inducer of CYP3A4 and P-glycoprotein increase effect of Apixaban and Rivaroxaban. P-glycoprotein inducers can reduce the effects of Dabigatran and Edoxaban. Safest: low molecular weight heparin XX 2 0Second choice: Edoxaban P R E S E N TAT I O N T I T L E 19
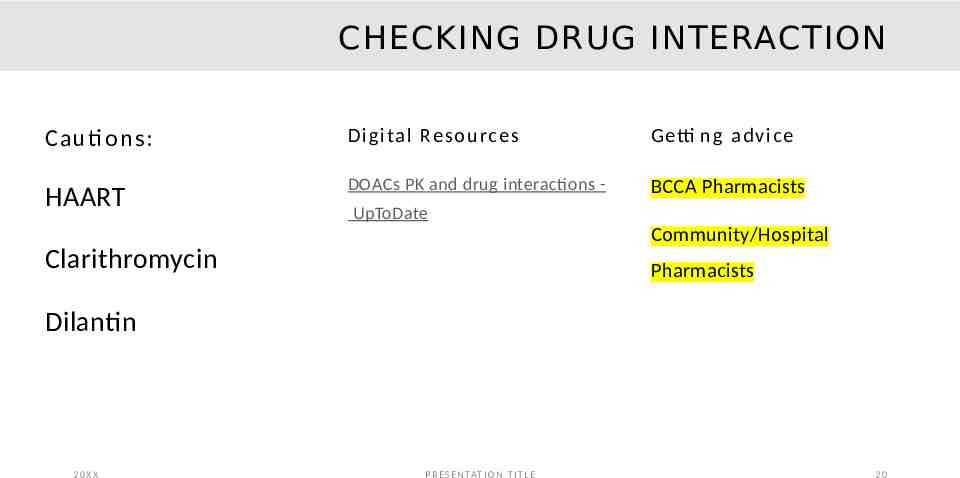
CHECKING DRUG INTERACTION Cauti ons: D i gi ta l Reso u rc e s Getti n g a dv ic e HAART DOACs PK and drug interactions - BCCA Pharmacists UpToDate Community/Hospital Clarithromycin Pharmacists Dilantin 20XX P R E S E N TAT I O N T I T L E 20
CASE 3: MANAGEMENT OF BREAK-THROUGH CLOT. 78-years-old patient with advanced stage Pancreatic cancer. He had right proximal DVT 1 month ago and started on Apixaban 10 mg bid for 7 days and transitioned to Apixaban 5 mg bid. He now has worsening swelling of right leg. Repeat ultrasound Doppler – progression of DVT. What is your plan? 20XX P R E S E N TAT I O N T I T L E 21
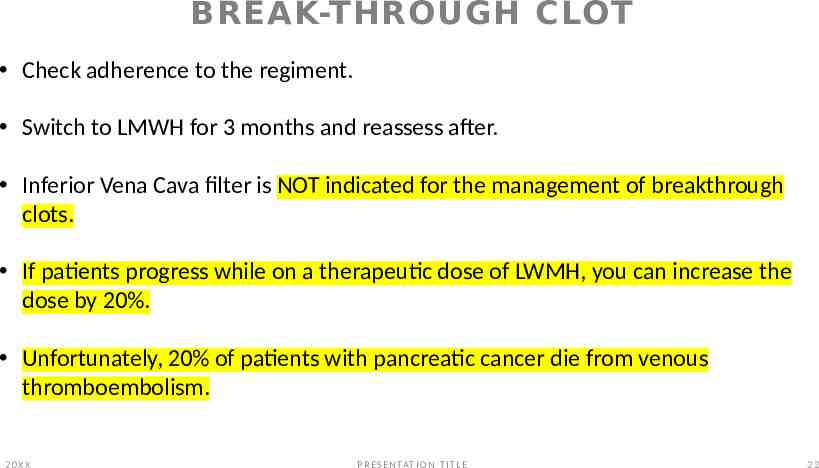
BREAK-THROUGH CLOT Check adherence to the regiment. Switch to LMWH for 3 months and reassess after. Inferior Vena Cava filter is NOT indicated for the management of breakthrough clots. If patients progress while on a therapeutic dose of LWMH, you can increase the dose by 20%. Unfortunately, 20% of patients with pancreatic cancer die from venous thromboembolism. 20XX P R E S E N TAT I O N T I T L E 22
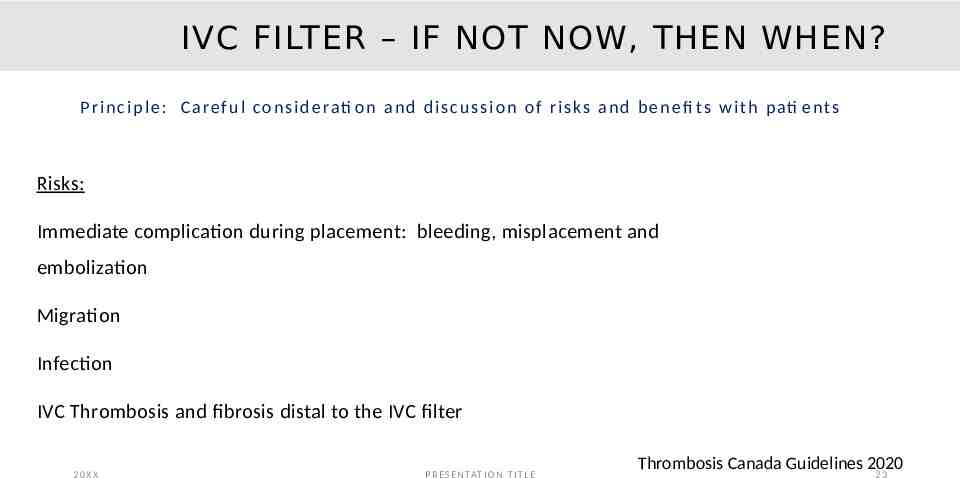
IVC FILTER – IF NOT NOW, THEN WHEN? P r i n c i p l e : C a re f u l c o n s i d e rati o n a n d d i s c u s s i o n o f r i s k s a n d b e n e fi t s w i t h p ati e nt s Risks: Immediate complication during placement: bleeding, misplacement and embolization Migration Infection IVC Thrombosis and fibrosis distal to the IVC filter 20XX P R E S E N TAT I O N T I T L E Thrombosis Canada Guidelines 2020 23
IVC FILTER: CAUTION Only indicated in patients with a recently diagnosed VTE (within 4 weeks) acute proximal DVT or acute PE in whom there is a contraindication to anticoagulation (active bleeding or perioperative) Patients should have the filter removed once appropriate anticoagulation is started. 20XX P R E S E N TAT I O N T I T L E 24
A 69-year-old patient with metastatic breast cancer and is on chemotherapy. She resides in a Northern CASE 4: RURAL AND REMOTE CONTEXT community. She presents with swelling of the left leg for 48 hours. No respiratory symptom. No Chest pain. It will take 9-hours to drive to Prince George for an ultrasound Doppler or transfer to Vancouver General Hospital by flight. 20XX P R E S E N TAT I O N T I T L E 25
WHAT ARE YOUR SUGGESTIONS? 20XX P R E S E N TAT I O N T I T L E 26
NO PERFECT ANSWERS Organize a d-dimer test: Caveats: Not validated for patients with active malignancy and long turnaround time. Arrange POCUS: operator dependent, availability. By application of Well’s criteria and D-Dimer as indicated, POCUS has a sensitivity of 93% and a specificity of 90% Anticoagulated empirically: discuss risk and benefits Varrias, D., Palaiodimos, L., Balasubramanian, P., Barrera, C. A., Nauka, P., Melainis, A. A., Zamora, C., Zavras, P., Napolitano, M., Gulani, P., Ntaios, G., Faillace, R. T., & Galen, B. (2021). The Use of Point-ofCare Ultrasound (POCUS) in the Diagnosis of Deep Vein Thrombosis. Journal of clinical medicine, 10(17), 3903. https://doi.org/10.3390/jcm10173903 20XX P R E S E N TAT I O N T I T L E . 0 27
PERI-OPERATIVE ANTICOAGULATION 65-year-old patients with colon cancer and completed chemotherapy in 2015. He has a history of DVT in 2019 and is on Rivaroxaban 20 mg once daily. He has a 3-cm mass in the retroperitoneal area and will need a CTguided biopsy. What is your plan? 20XX P R E S E N TAT I O N T I T L E 28
ANTICOAGULATION INTERRUPTION Fa c to rs to co n s id e r Re s o u rc e s Renal function Management Guidelines LM v10.2 2015-03 ( Risk of procedure fraserhealth.ca) Risk of VTE recurrence Compressible versus non-compressible sites For patients with prosthetic heart valves, recent VTE (less than 3 months), atrial fibrillation with prior stroke, do NOT stop anticoagulation without consultation with GIM 20XX P R E S E N TAT I O N T I T L E 29
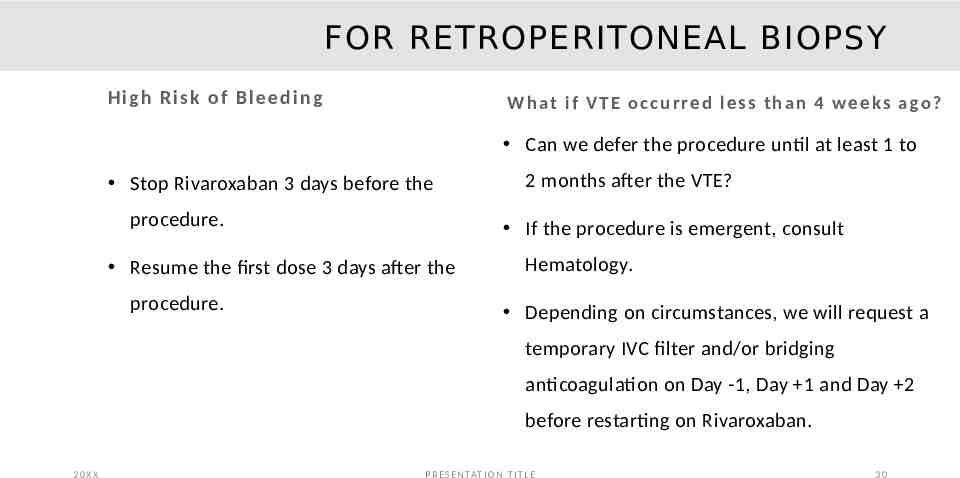
FOR RETROPERITONEAL BIOPSY High R is k o f B l ee d in g W h at i f V T E o c c u r re d l e s s t h a n 4 w e e ks a go ? Can we defer the procedure until at least 1 to Stop Rivaroxaban 3 days before the procedure. If the procedure is emergent, consult Resume the first dose 3 days after the procedure. 2 months after the VTE? Hematology. Depending on circumstances, we will request a temporary IVC filter and/or bridging anticoagulation on Day -1, Day 1 and Day 2 before restarting on Rivaroxaban. 20XX P R E S E N TAT I O N T I T L E 30
SUMMARY Cancer-associated thrombosis is a common complication. DVT prophylaxis is indicated in the postoperative setting or hospitalized patients. Long-term anticoagulation is recommended for patients with chronic malignancy. Avoid using an IVC filter. Follow guidelines on the perioperative procedure. 20XX P R E S E N TAT I O N T I T L E 31

IF YOU NEED ADVICE: 20XX P R E S E N TAT I O N T I T L E 32
THANK YOU! a d r ia n .ye e @ u bc .ca 20XX P R E S E N TAT I O N T I T L E 33