CAA Provider Update on PQRS Reporting Topics covered CMS
24 Slides1.97 MB
CAA Provider Update on PQRS Reporting Topics covered CMS Physician Quality Reporting System (PQRS) Anesthesia Quality Institute (AQI) Qualified Clinical Data Registry (QCDR) Data Capture Instructions Quality Measures (PQRS & Anesthesia Specific) Reporting Quality Measure Details 1
Update on PQRS Reporting CMS Physician Quality Reporting System Quality measures updated annually In 2015 lack of reporting financial penalties Applicable to all MDs, DOs & CRNAs New paperwork 2
CAA will use the AQI QCDR The only anesthesia Qualified Clinical Data Registry for reporting measures to CMS Includes anesthesia specific measures (CPOM*) Includes clinical outcomes (e.g. reintubation rate) vs process measures (e.g. admin of abx) *developed by the ASA Committee on Performance Outcome Measurements (CPOM) 3
Data Capture and Entry Paper based collection (until AIMS are updated/installed) 2 forms Non-cardiac (no beta blocker or central line measures) Cardiac (includes beta blockers & central line measures) Optical Mark Recognition (OMR) form “bubble sheet” Forms completed at facility, sent to RESULT and scanned. 4
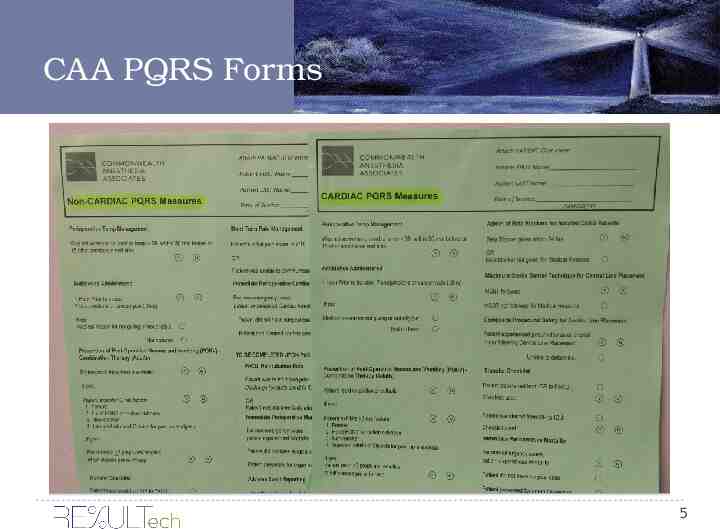
CAA PQRS Forms 5
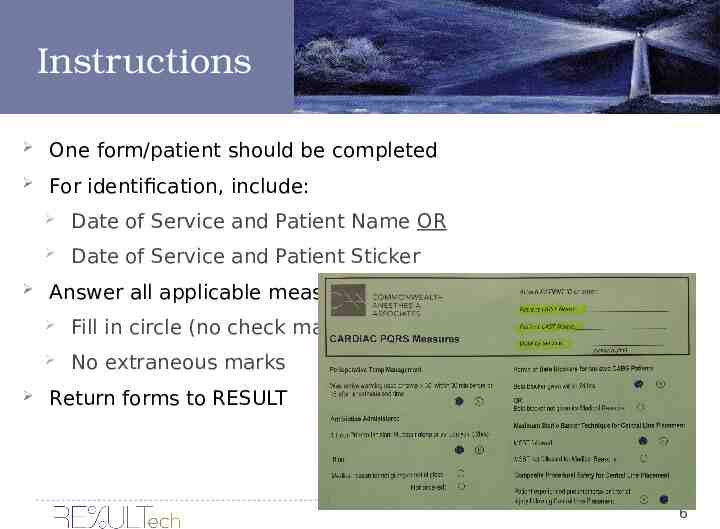
Instructions One form/patient should be completed For identification, include: Date of Service and Patient Name OR Date of Service and Patient Sticker Answer all applicable measures Fill in circle (no check marks) No extraneous marks Return forms to RESULT 6
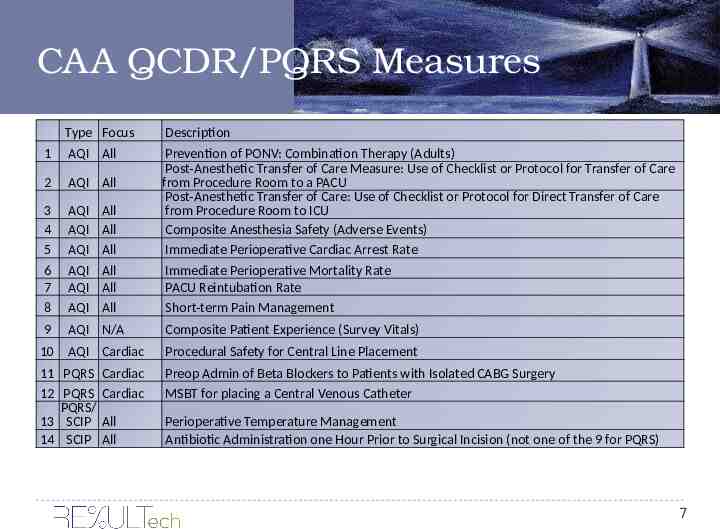
CAA QCDR/PQRS Measures 1 Type Focus AQI All 2 AQI All 3 4 5 6 7 8 AQI AQI AQI AQI AQI AQI 9 AQI N/A Composite Patient Experience (Survey Vitals) 10 AQI Cardiac Procedural Safety for Central Line Placement 11 PQRS Cardiac 12 PQRS Cardiac PQRS/ 13 SCIP All 14 SCIP All Preop Admin of Beta Blockers to Patients with Isolated CABG Surgery MSBT for placing a Central Venous Catheter All All All All All All Description Prevention of PONV: Combination Therapy (Adults) Post-Anesthetic Transfer of Care Measure: Use of Checklist or Protocol for Transfer of Care from Procedure Room to a PACU Post-Anesthetic Transfer of Care: Use of Checklist or Protocol for Direct Transfer of Care from Procedure Room to ICU Composite Anesthesia Safety (Adverse Events) Immediate Perioperative Cardiac Arrest Rate Immediate Perioperative Mortality Rate PACU Reintubation Rate Short-term Pain Management Perioperative Temperature Management Antibiotic Administration one Hour Prior to Surgical Incision (not one of the 9 for PQRS) 7
Details on Measures Measure Specifications are included on subsequent slides and the CAA website. For More info: Contact Michelle Lilly, 594-1390 [email protected] or https://www.aqihq.org/PQRSOverview.aspx 8
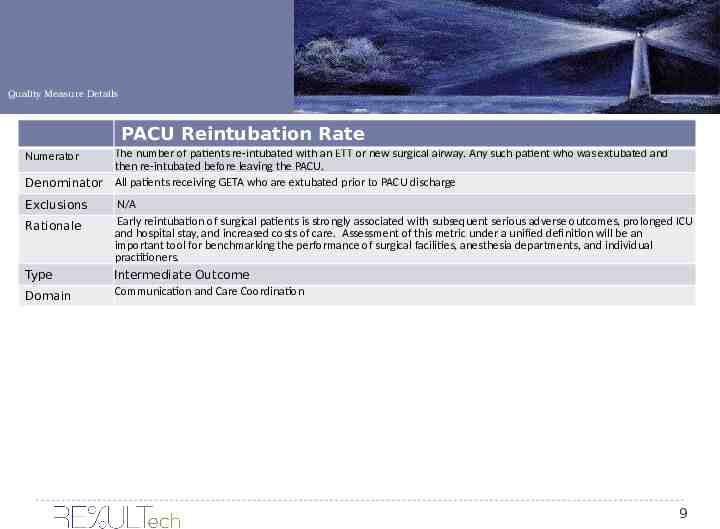
Quality Measure Details PACU Reintubation Rate The number of patients re-intubated with an ETT or new surgical airway. Any such patient who was extubated and then re-intubated before leaving the PACU. Denominator All patients receiving GETA who are extubated prior to PACU discharge Numerator Exclusions Rationale Type Domain N/A Early reintubation of surgical patients is strongly associated with subsequent serious adverse outcomes, prolonged ICU and hospital stay, and increased costs of care. Assessment of this metric under a unified definition will be an important tool for benchmarking the performance of surgical facilities, anesthesia departments, and individual practitioners. Intermediate Outcome Communication and Care Coordination 9
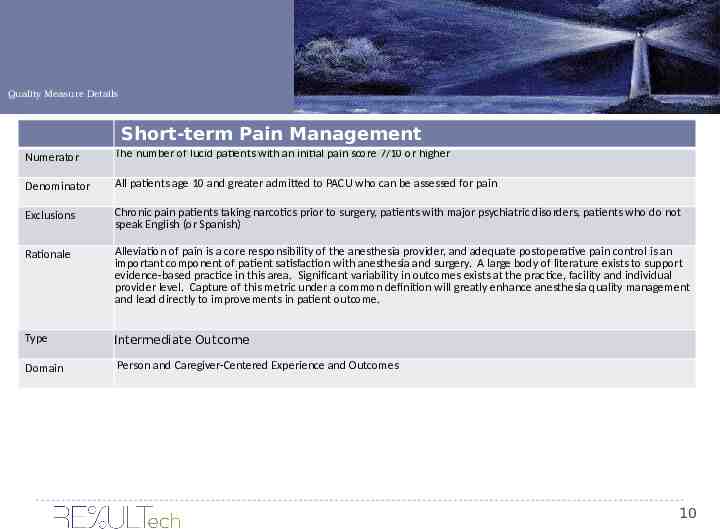
Quality Measure Details Short-term Pain Management Numerator The number of lucid patients with an initial pain score 7/10 or higher Denominator All patients age 10 and greater admitted to PACU who can be assessed for pain Exclusions Chronic pain patients taking narcotics prior to surgery, patients with major psychiatric disorders, patients who do not speak English (or Spanish) Rationale Alleviation of pain is a core responsibility of the anesthesia provider, and adequate postoperative pain control is an important component of patient satisfaction with anesthesia and surgery. A large body of literature exists to support evidence-based practice in this area. Significant variability in outcomes exists at the practice, facility and individual provider level. Capture of this metric under a common definition will greatly enhance anesthesia quality management and lead directly to improvements in patient outcome. Type Intermediate Outcome Domain Person and Caregiver-Centered Experience and Outcomes 10
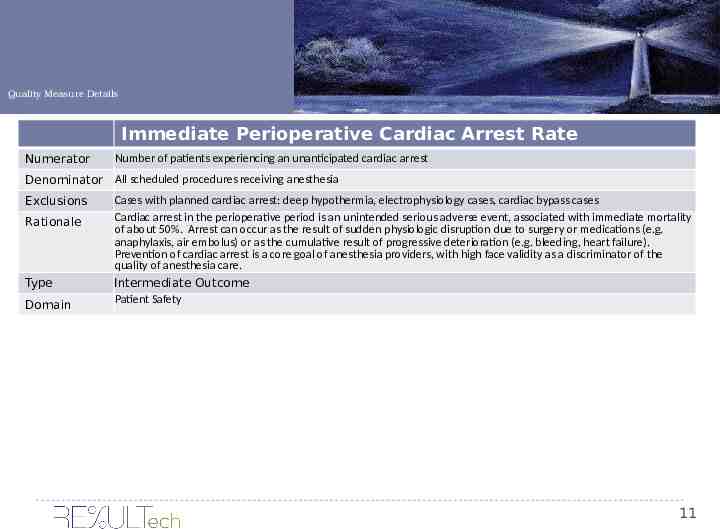
Quality Measure Details Immediate Perioperative Cardiac Arrest Rate Numerator Number of patients experiencing an unanticipated cardiac arrest Denominator All scheduled procedures receiving anesthesia Exclusions Rationale Type Domain Cases with planned cardiac arrest: deep hypothermia, electrophysiology cases, cardiac bypass cases Cardiac arrest in the perioperative period is an unintended serious adverse event, associated with immediate mortality of about 50%. Arrest can occur as the result of sudden physiologic disruption due to surgery or medications (e.g. anaphylaxis, air embolus) or as the cumulative result of progressive deterioration (e.g. bleeding, heart failure). Prevention of cardiac arrest is a core goal of anesthesia providers, with high face validity as a discriminator of the quality of anesthesia care. Intermediate Outcome Patient Safety 11
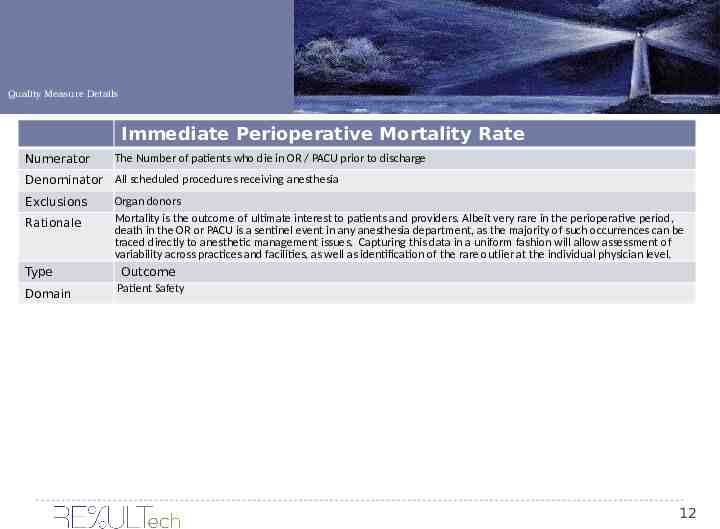
Quality Measure Details Immediate Perioperative Mortality Rate Numerator The Number of patients who die in OR / PACU prior to discharge Denominator All scheduled procedures receiving anesthesia Exclusions Rationale Type Domain Organ donors Mortality is the outcome of ultimate interest to patients and providers. Albeit very rare in the perioperative period, death in the OR or PACU is a sentinel event in any anesthesia department, as the majority of such occurrences can be traced directly to anesthetic management issues. Capturing this data in a uniform fashion will allow assessment of variability across practices and facilities, as well as identification of the rare outlier at the individual physician level. Outcome Patient Safety 12
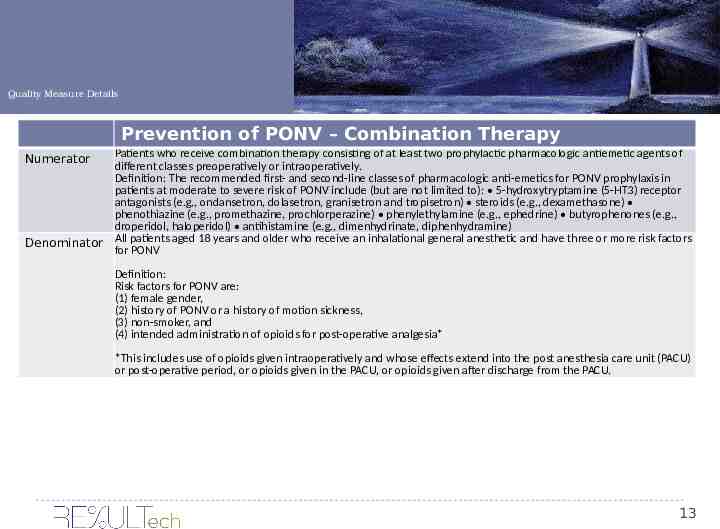
Quality Measure Details Prevention of PONV – Combination Therapy Patients who receive combination therapy consisting of at least two prophylactic pharmacologic antiemetic agents of different classes preoperatively or intraoperatively. Definition: The recommended first- and second-line classes of pharmacologic anti-emetics for PONV prophylaxis in patients at moderate to severe risk of PONV include (but are not limited to): 5-hydroxytryptamine (5-HT3) receptor antagonists (e.g., ondansetron, dolasetron, granisetron and tropisetron) steroids (e.g., dexamethasone) phenothiazine (e.g., promethazine, prochlorperazine) phenylethylamine (e.g., ephedrine) butyrophenones (e.g., droperidol, haloperidol) antihistamine (e.g., dimenhydrinate, diphenhydramine) Denominator All patients aged 18 years and older who receive an inhalational general anesthetic and have three or more risk factors for PONV Numerator Definition: Risk factors for PONV are: (1) female gender, (2) history of PONV or a history of motion sickness, (3) non-smoker, and (4) intended administration of opioids for post-operative analgesia* *This includes use of opioids given intraoperatively and whose effects extend into the post anesthesia care unit (PACU) or post-operative period, or opioids given in the PACU, or opioids given after discharge from the PACU. 13
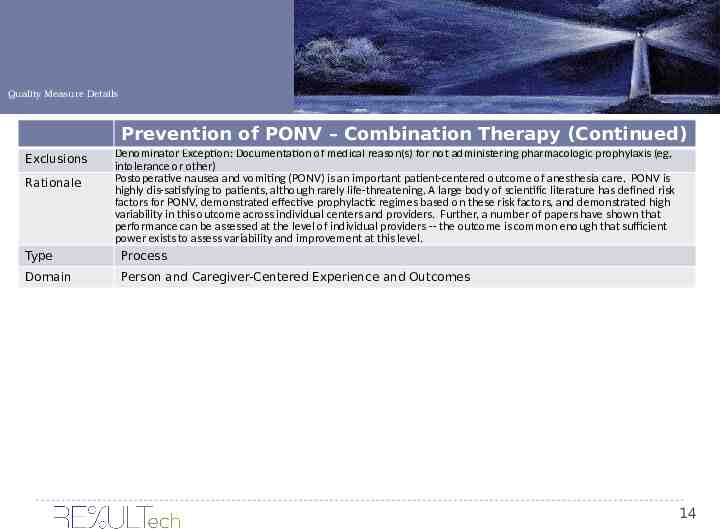
Quality Measure Details Prevention of PONV – Combination Therapy (Continued) Exclusions Rationale Type Domain Denominator Exception: Documentation of medical reason(s) for not administering pharmacologic prophylaxis (eg, intolerance or other) Postoperative nausea and vomiting (PONV) is an important patient-centered outcome of anesthesia care. PONV is highly dis-satisfying to patients, although rarely life-threatening. A large body of scientific literature has defined risk factors for PONV, demonstrated effective prophylactic regimes based on these risk factors, and demonstrated high variability in this outcome across individual centers and providers. Further, a number of papers have shown that performance can be assessed at the level of individual providers -- the outcome is common enough that sufficient power exists to assess variability and improvement at this level. Process Person and Caregiver-Centered Experience and Outcomes 14
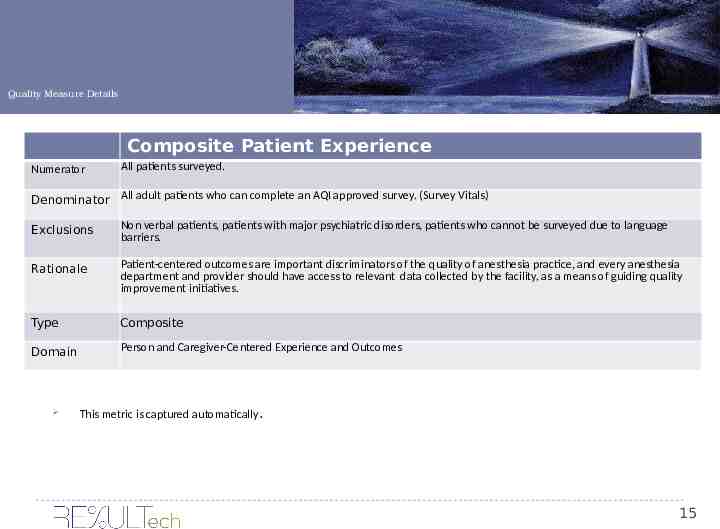
Quality Measure Details Composite Patient Experience Numerator All patients surveyed. Denominator All adult patients who can complete an AQI approved survey. (Survey Vitals) Exclusions Non verbal patients, patients with major psychiatric disorders, patients who cannot be surveyed due to language barriers. Rationale Patient-centered outcomes are important discriminators of the quality of anesthesia practice, and every anesthesia department and provider should have access to relevant data collected by the facility, as a means of guiding quality improvement initiatives. Type Composite Domain Person and Caregiver-Centered Experience and Outcomes This metric is captured automatically. 15
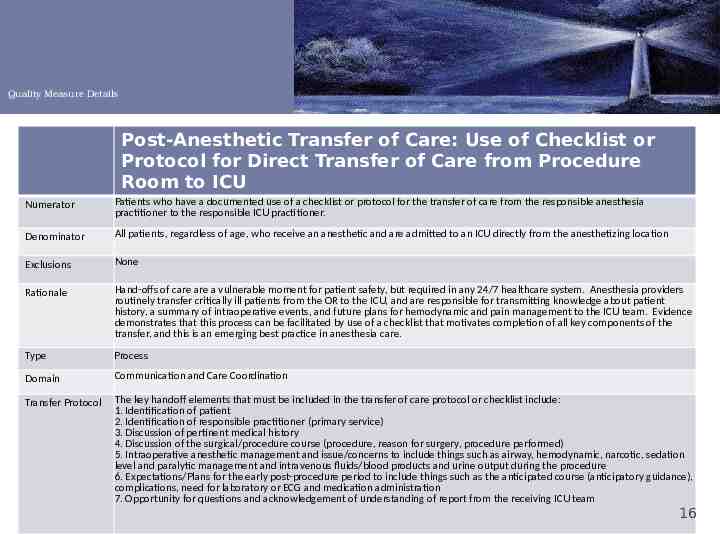
Quality Measure Details Post-Anesthetic Transfer of Care: Use of Checklist or Protocol for Direct Transfer of Care from Procedure Room to ICU Numerator Patients who have a documented use of a checklist or protocol for the transfer of care from the responsible anesthesia practitioner to the responsible ICU practitioner. Denominator All patients, regardless of age, who receive an anesthetic and are admitted to an ICU directly from the anesthetizing location Exclusions None Rationale Hand-offs of care are a vulnerable moment for patient safety, but required in any 24/7 healthcare system. Anesthesia providers routinely transfer critically ill patients from the OR to the ICU, and are responsible for transmitting knowledge about patient history, a summary of intraoperative events, and future plans for hemodynamic and pain management to the ICU team. Evidence demonstrates that this process can be facilitated by use of a checklist that motivates completion of all key components of the transfer, and this is an emerging best practice in anesthesia care. Type Process Domain Communication and Care Coordination Transfer Protocol The key handoff elements that must be included in the transfer of care protocol or checklist include: 1. Identification of patient 2. Identification of responsible practitioner (primary service) 3. Discussion of pertinent medical history 4. Discussion of the surgical/procedure course (procedure, reason for surgery, procedure performed) 5. Intraoperative anesthetic management and issue/concerns to include things such as airway, hemodynamic, narcotic, sedation level and paralytic management and intravenous fluids/blood products and urine output during the procedure 6. Expectations/Plans for the early post-procedure period to include things such as the anticipated course (anticipatory guidance), complications, need for laboratory or ECG and medication administration 7. Opportunity for questions and acknowledgement of understanding of report from the receiving ICU team 16
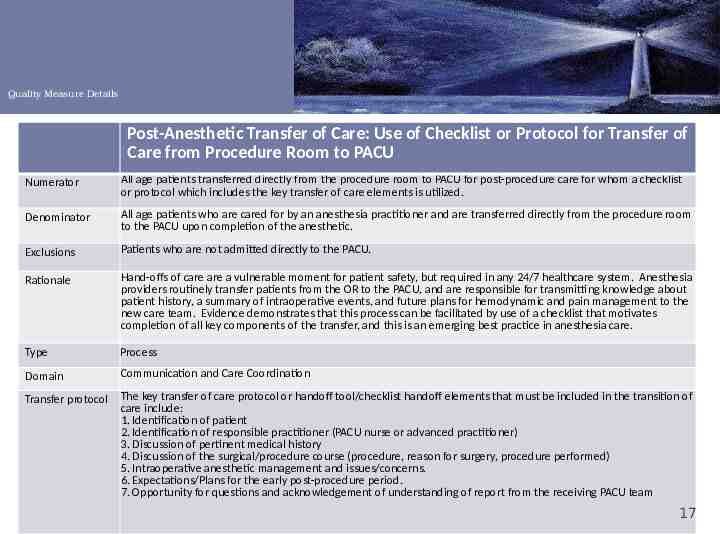
Quality Measure Details Post-Anesthetic Transfer of Care: Use of Checklist or Protocol for Transfer of Care from Procedure Room to PACU Numerator All age patients transferred directly from the procedure room to PACU for post-procedure care for whom a checklist or protocol which includes the key transfer of care elements is utilized. Denominator All age patients who are cared for by an anesthesia practitioner and are transferred directly from the procedure room to the PACU upon completion of the anesthetic. Exclusions Patients who are not admitted directly to the PACU. Rationale Hand-offs of care are a vulnerable moment for patient safety, but required in any 24/7 healthcare system. Anesthesia providers routinely transfer patients from the OR to the PACU, and are responsible for transmitting knowledge about patient history, a summary of intraoperative events, and future plans for hemodynamic and pain management to the new care team. Evidence demonstrates that this process can be facilitated by use of a checklist that motivates completion of all key components of the transfer, and this is an emerging best practice in anesthesia care. Type Process Domain Communication and Care Coordination Transfer protocol The key transfer of care protocol or handoff tool/checklist handoff elements that must be included in the transition of care include: 1. Identification of patient 2. Identification of responsible practitioner (PACU nurse or advanced practitioner) 3. Discussion of pertinent medical history 4. Discussion of the surgical/procedure course (procedure, reason for surgery, procedure performed) 5. Intraoperative anesthetic management and issues/concerns. 6. Expectations/Plans for the early post-procedure period. 7. Opportunity for questions and acknowledgement of understanding of report from the receiving PACU team 17
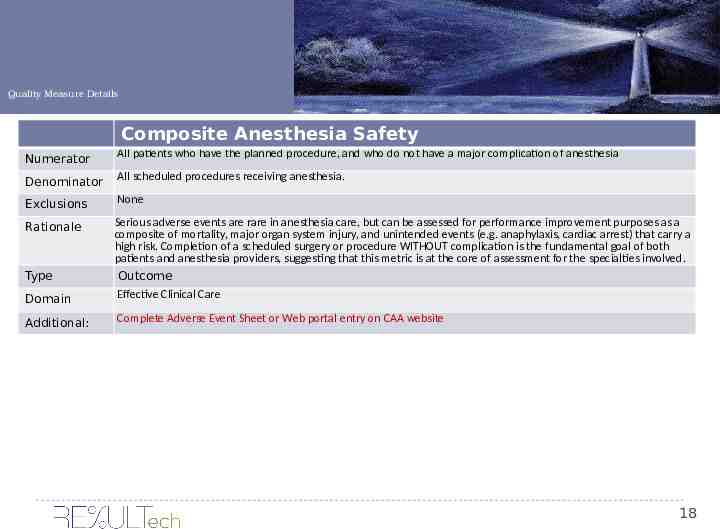
Quality Measure Details Composite Anesthesia Safety Numerator All patients who have the planned procedure, and who do not have a major complication of anesthesia Denominator All scheduled procedures receiving anesthesia. Exclusions None Rationale Domain Serious adverse events are rare in anesthesia care, but can be assessed for performance improvement purposes as a composite of mortality, major organ system injury, and unintended events (e.g. anaphylaxis, cardiac arrest) that carry a high risk. Completion of a scheduled surgery or procedure WITHOUT complication is the fundamental goal of both patients and anesthesia providers, suggesting that this metric is at the core of assessment for the specialties involved. Outcome Effective Clinical Care Additional: Complete Adverse Event Sheet or Web portal entry on CAA website Type 18
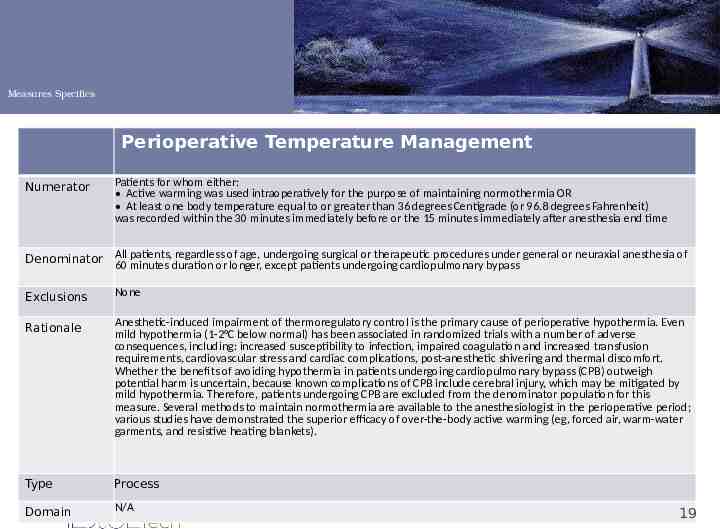
Measures Specifics Perioperative Temperature Management Numerator Patients for whom either: Active warming was used intraoperatively for the purpose of maintaining normothermia OR At least one body temperature equal to or greater than 36 degrees Centigrade (or 96.8 degrees Fahrenheit) was recorded within the 30 minutes immediately before or the 15 minutes immediately after anesthesia end time Denominator All patients, regardless of age, undergoing surgical or therapeutic procedures under general or neuraxial anesthesia of 60 minutes duration or longer, except patients undergoing cardiopulmonary bypass Exclusions None Rationale Anesthetic-induced impairment of thermoregulatory control is the primary cause of perioperative hypothermia. Even mild hypothermia (1-2 C below normal) has been associated in randomized trials with a number of adverse consequences, including: increased susceptibility to infection, impaired coagulation and increased transfusion requirements, cardiovascular stress and cardiac complications, post-anesthetic shivering and thermal discomfort. Whether the benefits of avoiding hypothermia in patients undergoing cardiopulmonary bypass (CPB) outweigh potential harm is uncertain, because known complications of CPB include cerebral injury, which may be mitigated by mild hypothermia. Therefore, patients undergoing CPB are excluded from the denominator population for this measure. Several methods to maintain normothermia are available to the anesthesiologist in the perioperative period; various studies have demonstrated the superior efficacy of over-the-body active warming (eg, forced air, warm-water garments, and resistive heating blankets). Type Process Domain N/A 19
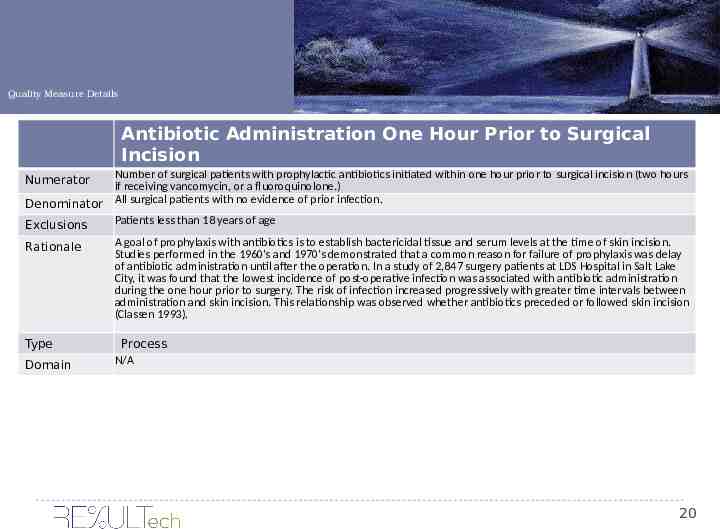
Quality Measure Details Antibiotic Administration One Hour Prior to Surgical Incision Number of surgical patients with prophylactic antibiotics initiated within one hour prior to surgical incision (two hours if receiving vancomycin, or a fluoroquinolone.) Denominator All surgical patients with no evidence of prior infection. Patients less than 18 years of age Exclusions Numerator Rationale A goal of prophylaxis with antibiotics is to establish bactericidal tissue and serum levels at the time of skin incision. Studies performed in the 1960’s and 1970’s demonstrated that a common reason for failure of prophylaxis was delay of antibiotic administration until after the operation. In a study of 2,847 surgery patients at LDS Hospital in Salt Lake City, it was found that the lowest incidence of post-operative infection was associated with antibiotic administration during the one hour prior to surgery. The risk of infection increased progressively with greater time intervals between administration and skin incision. This relationship was observed whether antibiotics preceded or followed skin incision (Classen 1993). Type Process N/A Domain 20
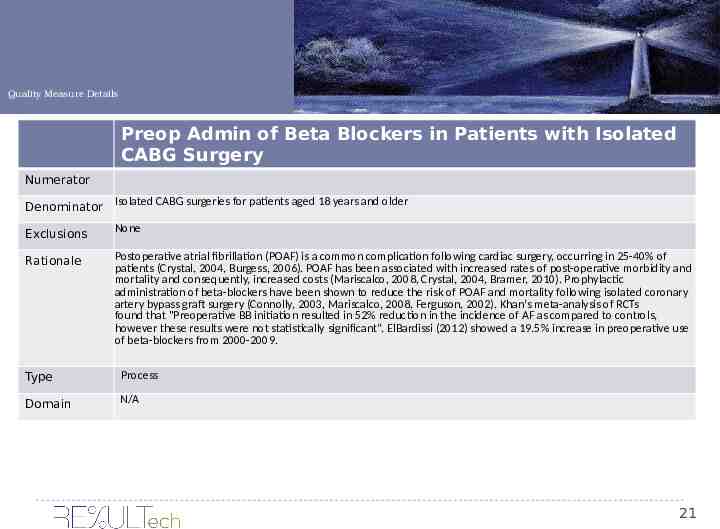
Quality Measure Details Preop Admin of Beta Blockers in Patients with Isolated CABG Surgery Numerator Denominator Isolated CABG surgeries for patients aged 18 years and older Exclusions None Rationale Postoperative atrial fibrillation (POAF) is a common complication following cardiac surgery, occurring in 25-40% of patients (Crystal, 2004, Burgess, 2006). POAF has been associated with increased rates of post-operative morbidity and mortality and consequently, increased costs (Mariscalco, 2008, Crystal, 2004, Bramer, 2010). Prophylactic administration of beta-blockers have been shown to reduce the risk of POAF and mortality following isolated coronary artery bypass graft surgery (Connolly, 2003, Mariscalco, 2008, Ferguson, 2002). Khan’s meta-analysis of RCTs found that "Preoperative BB initiation resulted in 52% reduction in the incidence of AF as compared to controls, however these results were not statistically significant”. ElBardissi (2012) showed a 19.5% increase in preoperative use of beta-blockers from 2000-2009. Type Process Domain N/A 21
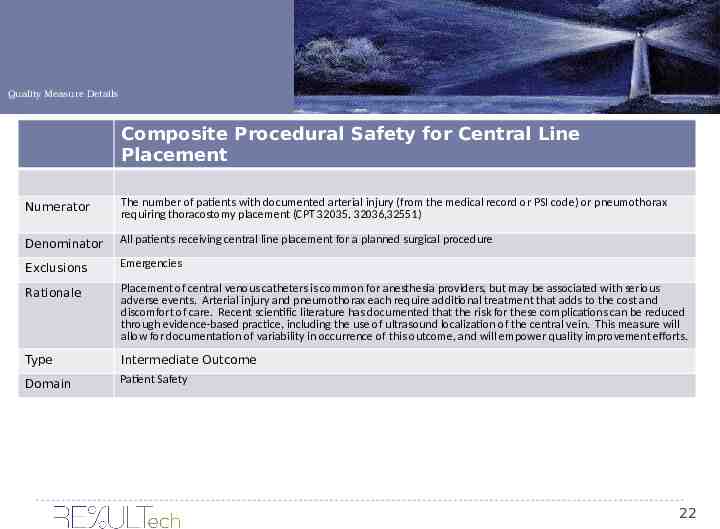
Quality Measure Details Composite Procedural Safety for Central Line Placement Numerator The number of patients with documented arterial injury (from the medical record or PSI code) or pneumothorax requiring thoracostomy placement (CPT 32035, 32036,32551) Denominator All patients receiving central line placement for a planned surgical procedure Exclusions Emergencies Rationale Placement of central venous catheters is common for anesthesia providers, but may be associated with serious adverse events. Arterial injury and pneumothorax each require additional treatment that adds to the cost and discomfort of care. Recent scientific literature has documented that the risk for these complications can be reduced through evidence-based practice, including the use of ultrasound localization of the central vein. This measure will allow for documentation of variability in occurrence of this outcome, and will empower quality improvement efforts. Type Intermediate Outcome Domain Patient Safety 22
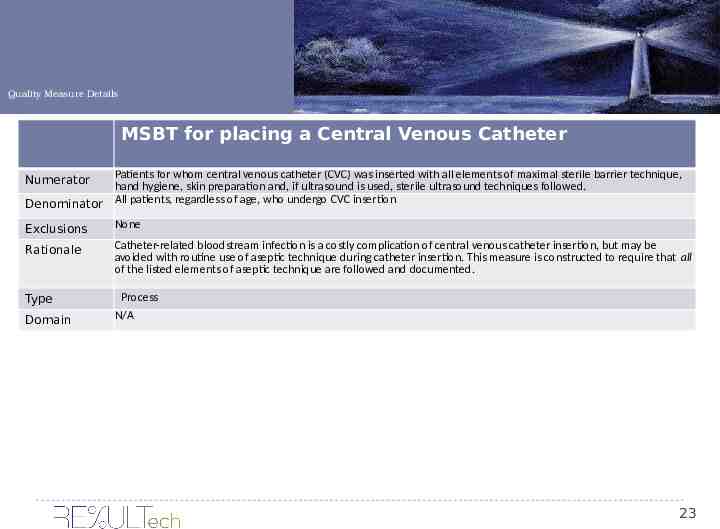
Quality Measure Details MSBT for placing a Central Venous Catheter Patients for whom central venous catheter (CVC) was inserted with all elements of maximal sterile barrier technique, hand hygiene, skin preparation and, if ultrasound is used, sterile ultrasound techniques followed. Denominator All patients, regardless of age, who undergo CVC insertion Numerator Exclusions None Rationale Catheter-related bloodstream infection is a costly complication of central venous catheter insertion, but may be avoided with routine use of aseptic technique during catheter insertion. This measure is constructed to require that all of the listed elements of aseptic technique are followed and documented. Type Domain Process N/A 23
For more info: Questions: Contact Michelle Lilly, Director of Quality Programs at [email protected] or 594-1390 24