Addiction is Addiction LIC 6 Lifestyle Intervention Conference 2016
99 Slides3.42 MB
Addiction is Addiction LIC 6 Lifestyle Intervention Conference 2016 October 17 Presented by Dr. Raju Hajela www.healthupwardlymobile.net E-mail: [email protected] or [email protected] Phone: 403-536-2480 Fax: 403-536-2482
Addiction Is Check all that apply Bad behaviour or a vice Self-medication Just wanting to get ‘high’ Wrong choices Just excessive substance use Something that can be fixed or cured Controllable About enjoying one’s vice Bad choices Wilful ignorance of reality Being selfish Caused by something else (i.e., trauma) Substance Abuse Loss of morals A psychiatric disorder
Addiction and Mental Health Cause or effect? Addiction/substance use occurs because of underlying psychiatric problems, OR Addiction/substance use results in psychiatric problems
Intoxication Use of substances - stimulants, depressants, opioids, hallucinogens and inhalants - continuous or intermittent, may cause – – – – – Thought disorders Mood disorders Perceptual disorders Neurological damage End-organ damage
Withdrawal Opposite of the drug effect Depressant withdrawal – most dangerous – seizures, Delerium Tremens - increased mortality Stimulants – craving Opioids – most uncomfortable but can be managed “cold-turkey” even in pregnancy – recurrent relapse is the problem if no treatment or engagement in recovery Hallucinogens – subtle Non-specific – nausea, vomiting, sleep disturbance, temp intolerance, irritability, mood swings, acting out
Addiction & Mental Health Addiction underlies many psychiatric conditions (e.g., Anxiety, Mood disorders, Psychosis, Conduct disorder, Personality Disorders like Borderline or Antisocial, ADHD) Treating the psychiatric disorder does not make substance related problems or Addiction go away Many treatments focus on behaviour only. Changing behaviour alone does not provide full treatment!
Stress, Anxiety & Depression Symptoms of intoxication and withdrawal manifest as stress, anxiety, and/or depression Fear of the future anxiety Shame from the past depression Anger about the present stress Feelings of hopelessness, worthlessness are part of Addictionwill all be and will be exacerbated in the absence of absence of healthy recovery, especiaally especially with no substance use or escape/or escape/relief
Substance Use Continuum Low-risk use Hazardous use Harmful use Abuse – continued use despite negative consequences Dependence – pre-occupation, compulsion, obsession (craving) – loss of control
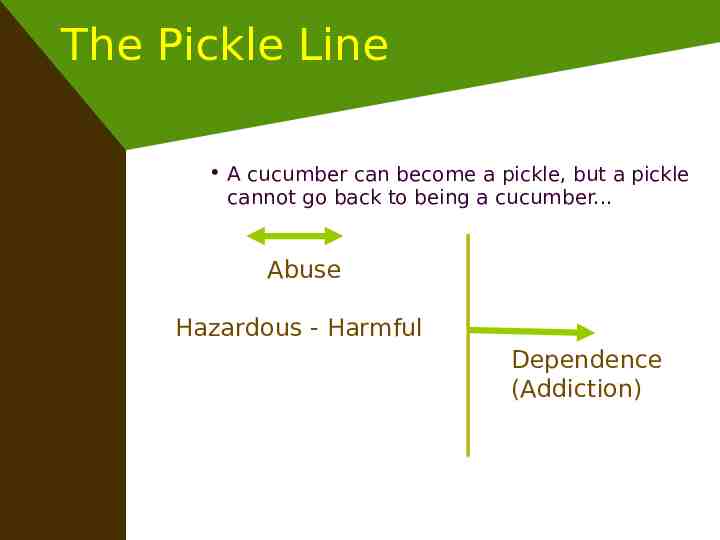
The Pickle Line A cucumber can become a pickle, but a pickle cannot go back to being a cucumber. Abuse Hazardous - Harmful Dependence (Addiction)
Dependence Characteristics Withdrawal Tolerance Use of larger amounts or over a longer period than intended Persistent desire for the substance (or process) or unsuccessful attempts to cut down A great deal of time is spent in securing access to substance/process Social or other activities are given up or reduced due to use Use despite recurrent or persistent problems (family, social, work)

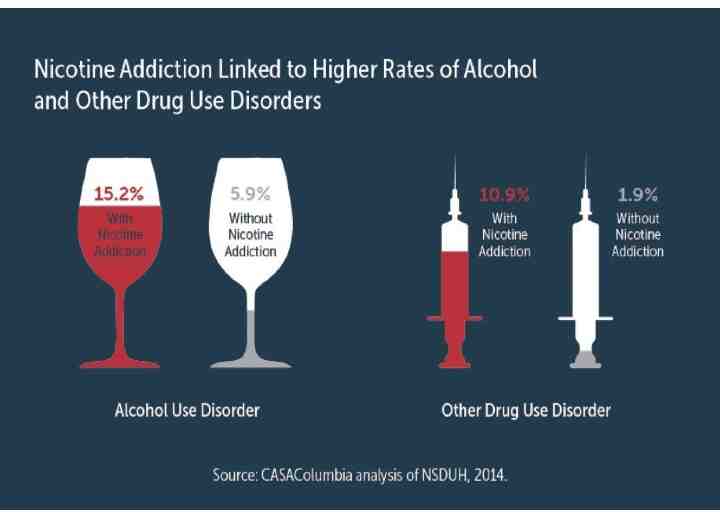
Addiction is Addiction Addiction is not limited to alcohol and illicit drugs. It can include: Gambling Food/Eating disorders Sex, love, relationships Internet/video games Shopping Exercise/sports Work Caffeine Nicotine Prescription medication
Cravings When compulsive and obsessive thought revolves around a desire, craving and ritualized behavior often evolves The drive to appease craving leads to powerlessness and unmanageability. Sign that Addiction and substance dependence are present May continue for months into abstinence. Can be physiological and/or psychological Drug/Problem behaviour Survival
Cravings Cravings are relieved when a person anticipates using or has acquired their substance of choice This anticipation releases dopamine, chemical hit from the drug is a ‘bonus’ Relief from cravings is not directly tied to ingestion of substance or engagement in behaviour!
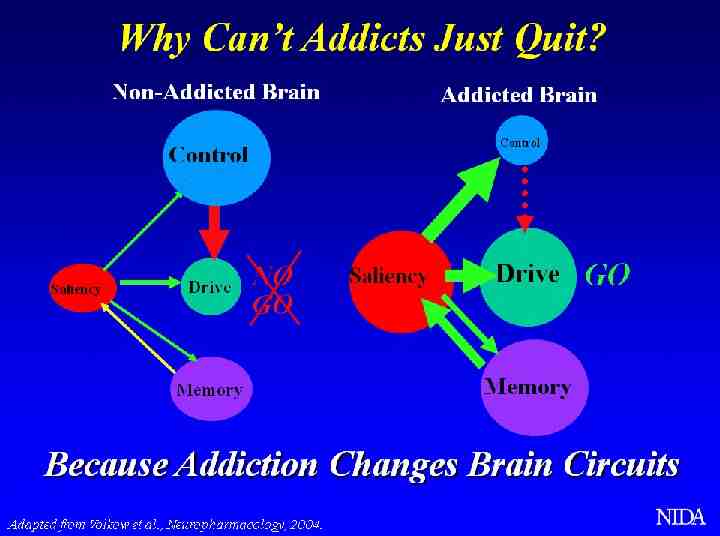
The Brain The brain operates differently with Addiction (hippocampus, VTA, nucleus accumbens, amygdala, and frontal cortex are impacted) Neurotransmitters are involved, particularly dopamine and glutamate
Neurotransmitters Neurotransmitters are natural chemicals that transmit signals from a neuron to a target cell across a synapse. They carry information There are many types of neurotransmitters. Important ones in Addiction are Dopamine and Glutamate, but opioid peptides, GABA, norepinephrine, and serotonin are also impacted
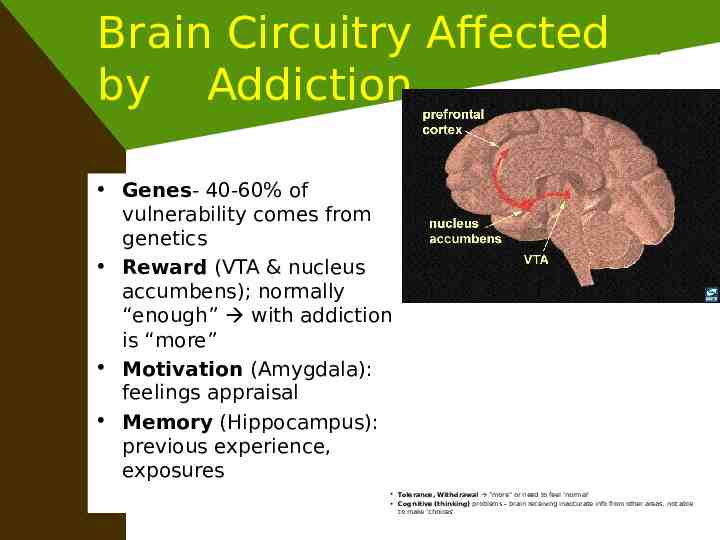
Brain Circuitry Affected by Addiction Genes- 40-60% of vulnerability comes from genetics Reward (VTA & nucleus accumbens); normally “enough” with addiction is “more” Motivation (Amygdala): feelings appraisal Memory (Hippocampus): previous experience, exposures Tolerance, Withdrawal “more” or need to feel ‘normal’ Cognitive (thinking) problems – brain receiving inaccurate info from other areas, not able to make ‘choices’
Addictive Thinking by Abraham Twerski Addictive Thinking irrational, distorted thoughts Everyone on the planet has Addictive Thinking in some form or another Difference with Addiction is: – It escalates and becomes unmanageable – Consequences are more severe (i.e., relapse) – Feels overwhelming – Leads to persistent obsession that takes you away from reality
Characteristics of Addictive Thinking Irrational Contradictory Rationalization Minimization Denial All-or-nothing Catastrophizing Skewed time Hypersensitivity Illusion of control Guilt
Hearing Addictive Thinking If you are hearing addictive thinking in someone else you may feel: – Confused/puzzled – Irritated/annoyed/angry – Physically upset (e.g., sick in the stomach) These feelings may precede your awareness of what you are
Addiction is Addiction Brain cannot distinguish between substances or processes like eating, gambling, sex, relationships all impact dopamine and other neurotransmitters in the brain Therefore abstinence from all illicit drugs, alcohol, and certain prescriptions (i.e., ones that impact reward circuitry) are important to form a foundation of recovery Can look at abstinence from ‘bottom line behaviours’ that increase vulnerability
REWARD and ANALGESIA Most rewarding (addictive) drugs produce analgesia (opioids and cannabinoids) Natural rewards, notably highly palatable foods such as chocolate, milk or sucrose, can produce a naloxone-reversible analgesic effect Consumption or anticipation of reward can inhibit responses to pain » Howard L. Fields, 2004 (Proceedings of the 11th World Congress on Pain)
Common Reward Circuitry High levels of dopamine receptors seem to protect against Addiction, while low levels increase vulnerability – including obesity and drug abuse – levels are affected by genetics and experience (exposure) (Volkow, 2006) Relapse associated with re-exposure to substance/behaviour, environment or increased stressors
Deficiency? Receptors – quantity? Function? Withdrawal symptoms? Anxiety? Depression? Psychosis? Social isolation? Criminal behaviour? Disruptions in Life Meaning, Values, Purpose? INTERNAL MECHANISMS DEFICIENT IN MAINTAINING
Addiction Is Check all that apply A primary, chronic disease About brain dysfunction About pathologically seeking reward About memory distortion About seeking relief About neglecting self About motivation problems About distortions in thinking, feeling, and perception About impaired behavioural control About cravings Lifelong
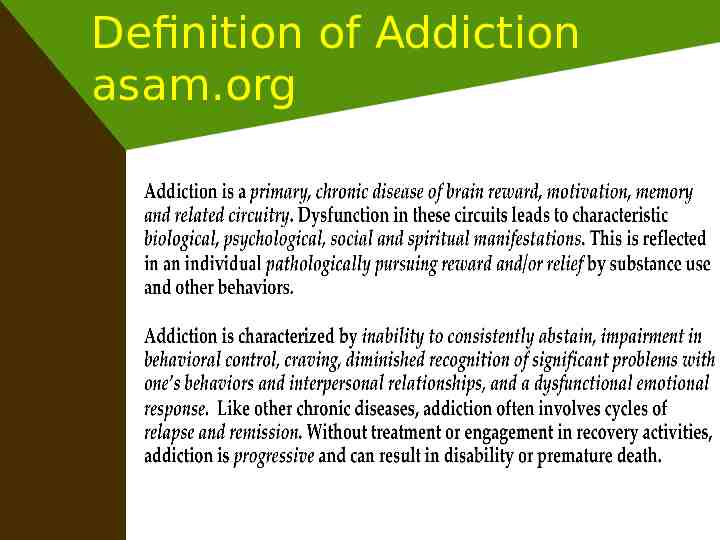
Definition of Addiction asam.org Addiction is a primary, chronic disease of brain reward, motivation, memory and related circuitry. Dysfunction in these circuits leads to characteristic biological, psychological, social and spiritual manifestations. This is reflected in the individual pursuing reward and/ or relief by substance use and other behaviors. Addiction is characterized by impairment in cognition and related behavioral control, craving, inability to consistently abstain, impairment in executive functioning and diminished recognition of significant problems with one’s behaviors and interpersonal relationships. Like other chronic diseases, addiction involves cycles of relapse and remission. Addiction is progressive, and can result in disability or premature death.
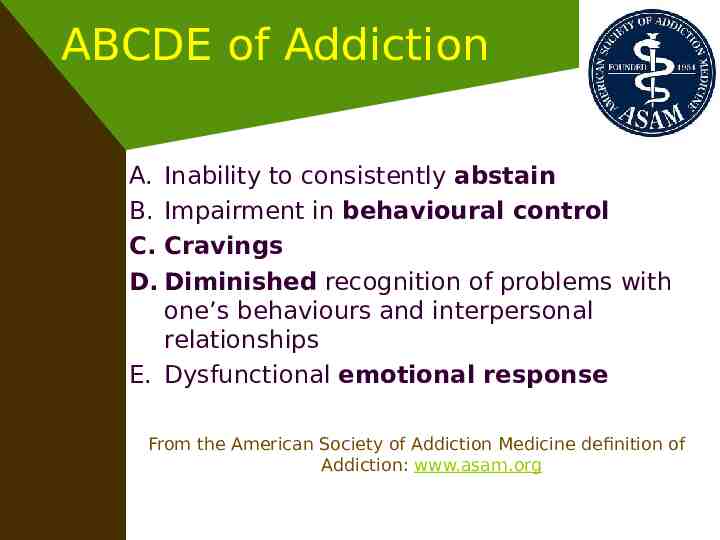
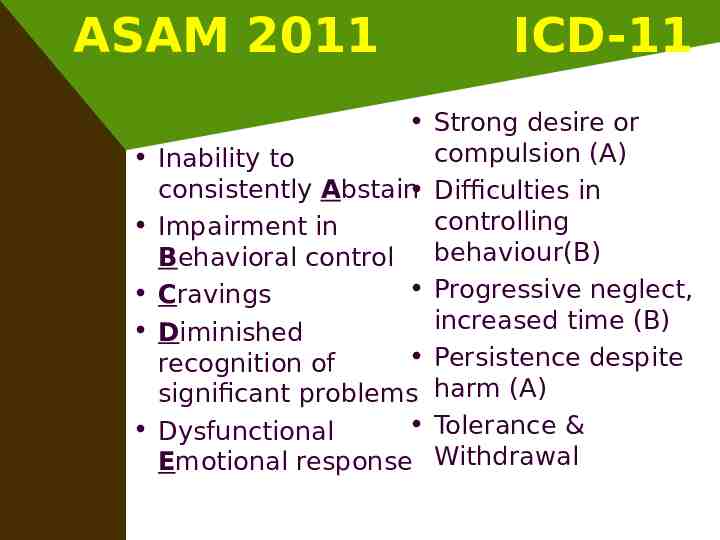
ABCDE of Addiction A. Inability to consistently abstain B. Impairment in behavioural control C. Cravings D. Diminished recognition of problems with one’s behaviours and interpersonal relationships E. Dysfunctional emotional response From the American Society of Addiction Medicine definition of Addiction: www.asam.org
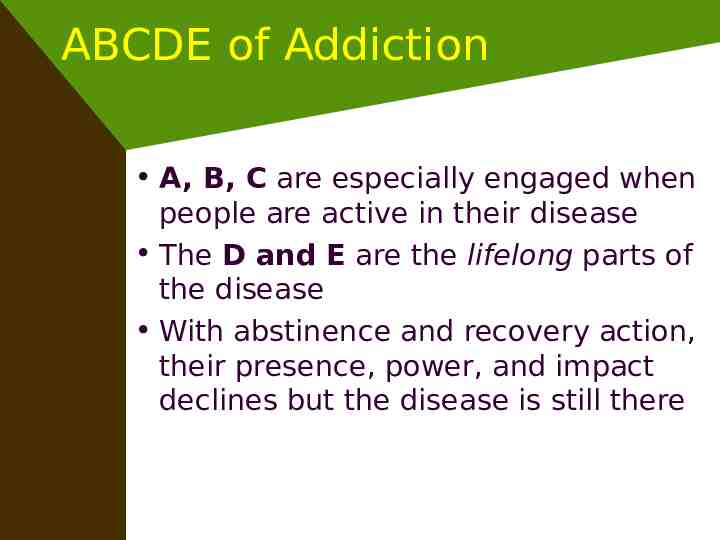
ABCDE of Addiction A, B, C are especially engaged when people are active in their disease The D and E are the lifelong parts of the disease With abstinence and recovery action, their presence, power, and impact declines but the disease is still there
ASAM 2011 ICD-11 Strong desire or compulsion (A) Inability to consistently Abstain Difficulties in controlling Impairment in behaviour(B) Behavioral control Progressive neglect, Cravings increased time (B) Diminished Persistence despite recognition of significant problems harm (A) Tolerance & Dysfunctional Emotional response Withdrawal
Role of Genetics Even if a family history of Addiction is not known or apparent, there was likely a relative at some point in the family lineage who struggled with the disease There is no untainted gene pool in the world when it comes to Addiction Not important to figure out how or who or why, focus on recovery
Brain and Behaviour Behaviours are NOT the disease nor do they cause the disease, they are SYMPTOMS of the disease Behaviours can aggravate the disease or help lead to recovery! Many healthcare providers and families believe that if behaviours are changed, the disease is fixed or cured It is impossible to fix or cure the brain completely. Behavioural remission helps emotional, social, and spiritual growth if action is taken Reading recommendation: The Selfish Brain by Robert DuPont
Impact of Problem Behaviours Problem behaviours, such as eating, sexual activity, shopping, gambling, being in a relationship, playing video games, and working can all have the same impact on the brain as substances Brain will release dopamine in the same way as with substance, telling the brain “I want more”
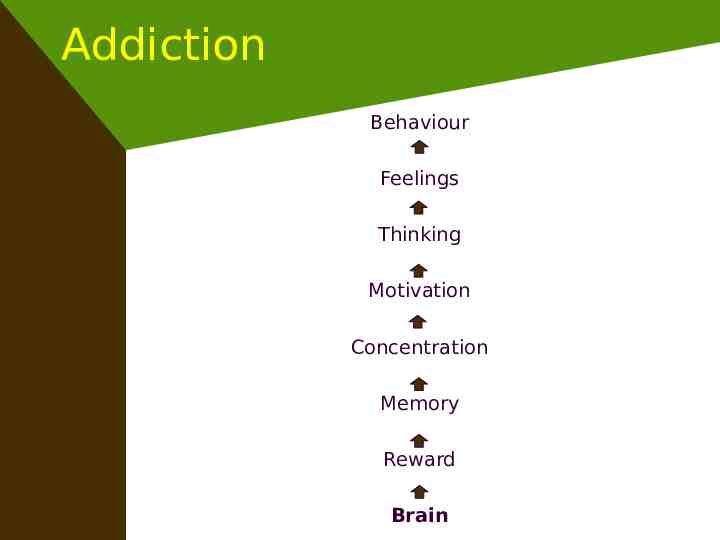
Addiction Behaviour Feelings Thinking Motivation Concentration Memory Reward Brain
Recovery Behaviour Feelings Thinking Motivation Concentration Memory Reward Brain
Addiction As Addiction is rooted in the brain and there is a genetic predisposition, the disease exists from birth Often parents will notice oddities or differences in children who later develop active Addiction: behavioural issues, conduct problems, obsession, rumination, emotional instability How it manifests depends on environment, exposure to substance, trauma, stress, life events
Addiction Beyond Substance Myth: Substances cause Addiction Fact: Substance use is the behavioural manifestation of Addiction and can aggravate the disease that already existed, plus have additional effects on the body and mind due to chemicals
Choice? Or Disease? Myth: Addiction and substance use are a choice Fact: Neither are a choice. The brain is vulnerable to Addiction from birth. Even using drugs or alcohol for the first time is not necessarily a ‘choice’ as brain is seeking escape, reward, relief Recommendation: Watch Pleasure Unwoven by Kevin McCauley on YouTube
A Key Message Addiction is a Primary, Chronic Brain Disease, NOT a behavioural disorder. A biological predisposition to the disease is passed on genetically. Other factors (environment, exposure to substance, trauma, etc.) impact how the disease manifests “The disease of addiction is part of you, not all of you”
Mental Health Some individuals will have Addiction and another mental health issue However, without stabilization of Addiction you will not know if other issues persist! Addiction must be treated first with holistic recovery abstinence
Another Key Message Addiction is NOT the result of other mental health conditions but a disease in and of itself. Treating Addiction will help alleviate mental health symptoms including: depression, anxiety, antisocial tendencies, difficulties in relationships, psychosis, lack of interest, lack of motivation, and many others! Treating mental health issues only will NOT facilitate recovery for Addiction
Another Key Message Addiction is Addiction! Brain does not distinguish between substance or process Addiction without the “s” “Cunning and Baffling”disease Addicted to something versus Addiction Cross, Multiple, Co are misleading terms Whack a Mole Reading recommendation: ASAM Definition of Addiction from www.asam.org
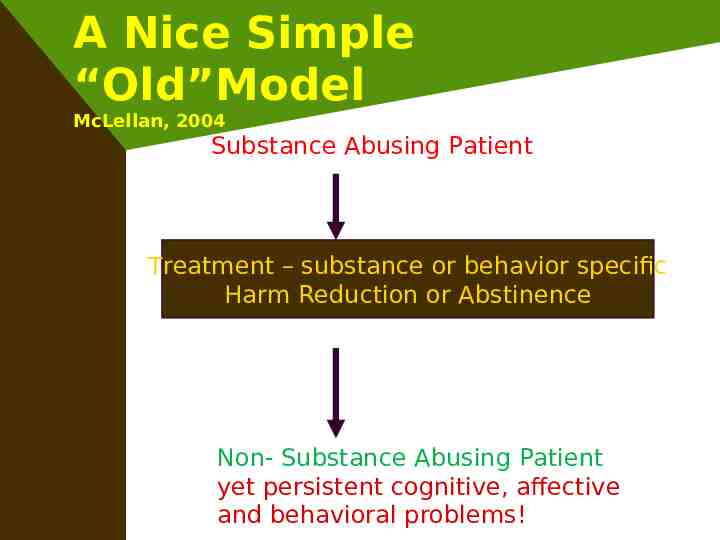
A Nice Simple “Old”Model McLellan, 2004 Substance Abusing Patient Treatment – substance or behavior specific Harm Reduction or Abstinence Non- Substance Abusing Patient yet persistent cognitive, affective and behavioral problems!
Addiction is not the same as intoxication When anyone experiences mild intoxication through the use of alcohol or other drugs, or when one engages non-pathologically in potentially addictive behaviors such as gambling or eating, one may experience a “high”, felt as a “positive” emotional state associated with increased dopamine and opioid peptide activity in reward circuits. After such an experience, there is a neurochemical rebound, in which the reward function does not simply revert to baseline, but often drops below the original levels. This is usually not consciously perceptible by the individual and is not necessarily associated with functional impairments.
A Continuing Care ASSESSMENT: Motivational Interviewing, Model Tailoring Treatment Withdrawal management, “Detox” “Rehab” – Outpatient, Residential, TC etc. Continuing Care Recovering Patient - Community Addiction is Addiction - Thinking, Feeling, Behaviors Concurrent Disorders – Bio-Psyhco-Social- Spiritual Medications, Therapy, Mutual Support, Monitoring
Addiction Concepts Harm Reduction Treat harm reduction as a means to an end, not an end in itself Viewed as what more needs to be done or what needs to be done differently rather than be the end treatment goal Moderate use/consumption is not possible if someone has Addiction

Harm Reduction A treatment and prevention approach that encompasses individual and public health needs, aiming to decrease the health and socio-economic costs and consequences of addiction-related problems, especially medical complications and transmission of infectious diseases, without necessarily requiring abstinence. Abstinence-based treatment approaches are themselves a part of comprehensive Harm Reduction strategies. A range of recovery activities may be included in every Harm Reduction strategy.
Definition of Abstinence More than ‘not using substance’ ASAM definition: intentional and consistent restraint from the pathological pursuit of reward and/or relief that involves the use of substances and other behaviors The pursuit of abstinence is important, which can exist even in the context of substance use/relapse
Addiction Concepts Abstinence Alone Is Not Enough Abstinence is a central component of long- term sobriety Need to incorporate focus on whole being There is no such thing as a bad feeling Life into Recovery compared to recovery into life Recovery Supports “It works if you work it”
Addiction Concepts Relapse: What to Look For An increase in addictive thinking (precedes all relapse behaviour) Continuum of Relapse: Spiritual-Emotional-Cognitive-SocialBehavioural
Relapse Persistent risk and/or recurrence of relapse, after periods of abstinence, is another fundamental feature of addiction. This can be triggered by exposure to rewarding substances and behaviors, by exposure to environmental cues to use, and by exposure to emotional stressors that trigger heightened activity in brain stress circuits. (Eliot Gardner)
Relapse Relapse triggered by exposure to addictive/ rewarding drugs, including alcohol, involves the nucleus accumbens and the VTA-MFB-Nuc Acc neural axis (the brain's mesolimbic dopaminergic "incentive salience circuitry”). Reward-triggered relapse also is mediated by glutamatergic circuits projecting to the nucleus accumbens from the frontal cortex. (George Koob)
Disease progression Over time, repeated experiences with substance use or addictive behaviors are not associated with ever increasing reward circuit activity and are not as subjectively rewarding. Once a person experiences withdrawal from drug use or comparable behaviors, there is an anxious, agitated, dysphoric and labile emotional experience, related to suboptimal reward and the recruitment of brain and hormonal stress systems, which is associated with withdrawal from virtually all pharmacological classes of addictive drugs.
Disease progression While tolerance develops to the “high,” tolerance does not develop to the emotional “low” associated with the cycle of intoxication and withdrawal. Thus, in addiction, persons repeatedly attempt to create a “high”--but what they mostly experience is a deeper and deeper “low.” While anyone may “want” to get “high”, those with addiction feel a “need” to use the addictive substance or engage in the addictive behavior in order to try to resolve their dysphoric emotional state or their physiological symptoms of withdrawal.
Disease progression Persons with addiction compulsively use even though it may not make them feel good, in some cases long after the pursuit of “rewards” is not actually pleasurable. Although people from any culture may choose to “get high” from one or another activity, it is important to appreciate that addiction is not solely a function of choice. Simply put, addiction is not a desired condition A B C D E
Medication Assisted Recovery (MAR) A transitional term to help the general public, recipients of health care services, and professional health care service providers understand that pharmacotherapy can be helpful in supporting recovery. The manifestations of addiction-related problems are addressed in their biological, psychological, social and spiritual dimensions during addiction treatment, in treatment approaches that are abstinence-based, and in treatment approaches that are harm-reduction-based. MAR is one component of the treatment and recovery process. Medication Assisted Treatment (MAT), another variation on the concept of MAR, may involve pharmacotherapy alone. It is essential that addiction treatment and recovery approaches address the various aspects of biological, psychological, social and spiritual dimensions for optimum health and wellness. It is hoped that as the public and professionals recognize that recovery and treatment need to be holistic, appropriate pharmacotherapy would be well accepted as part of treatment and recovery, such that the terms MAR and MAT would be deemed unnecessary.
Maintenance Treatments Pharmacotherapy on a consistent schedule for persons with addiction, usually with an agonist or partial agonist, which mitigates against the pathological pursuit of reward and/or relief and allows for remission of overt addiction-related problems. Maintenance Treatments of addiction are associated with the development of a pharmacological steady-state such that addictive substances are no longer sought for reward and/or relief. Maintenance Treatments of addiction are also designed to mitigate against the risk of overdose. Depending on the circumstances of a given case, a care plan including Maintenance Treatments can be time-limited or can remain in place life-long. Integration of pharmacotherapy via Maintenance Treatments with psychosocial treatments generally are associated with the best clinical results. Maintenance Treatments can be part of an individual’s treatment plan in abstinencebased recovery activities or can be a part of harm reduction strategies.
Provider Dr. Feelgood - opioids are good for pain relief, so prescribe short-acting opioids (patient controlled) – If you have pain, you can’t be addicted – What would you like? I want you to like me! Dr. Fingerwagger – opioids are dangerous and must be used very sparingly, if at all – If you take opioids, you will be addicted! – Motivation through shame and fear Dr. Compass – check all directions when prescribing opioids or any other psychoactive or psychotropic meds – Opioids are useful meds that require great care in prescribing and ongoing monitoring is essential! Dr. Reality Check – patient-centred care
Readiness to Change Resistant “Get off my back”-gather information, develop rapport Ambivalent “I am not sure I can ” provide information, preparation Action “I really want to, who can help ” alone we can’t, together we can Maintenance “My new lifestyle is more natural ” watch out for stressors and/or complacency
Motivational Interviewing Miller & Rollnick, 2009: collaborative, person-centred, guiding to elicit and strengthen motivation for change, improve outcomes – SAMHSA www.motivationalinterview.org Motivation is dynamic, awareness leads to action leads to awareness, repetition leads to conditioning; insight is not enough; amotivation & barriers are bio-psychosocial-spiritual!
Motivational Interviewing Task is to create discrepancy between where the patient is at and where she wants to be Realistic planning? Support self-efficacy, express empathy, roll with resistance Open ended questions, affirmations, reflections, summaries Desire, Ability, Reason, Need Commitment, Activation, Taking Steps
Decisional Balance Positives of changing, negatives of not-changing Positives of not-changing, negatives of changing (withdrawal, pain, PAWS)
Hajela & Irons, 1998 Psychotherapy Reflect – What I am hearing is? What exactly are you saying? Can you tell me more? Feelings? Thoughts? Interpret – This is what it means to me What does it mean to you? Reframe – Are there other ways to look at this? Humanize – Many people in this situation think this feel this do this
Recovery A process of sustained action that addresses the biological, psychological, social and spiritual disturbances inherent in addiction. Recovery aims to improve the quality of life by seeking balance and healing in all aspects of health and wellness, while addressing an individual’s consistent pursuit of abstinence, impairment in behavioral control, dealing with cravings, recognizing problems in one’s behaviors and interpersonal relationships, and dealing more effectively with emotional responses. An individual’s recovery actions lead to reversal of negative, self-defeating internal processes and behaviors, allowing healing of relationships with self and others. The concepts of acceptance and surrender are also useful in this process. Since some prescribed and non-prescribed medications can interfere with recovery, it would be prudent to consult with an Addiction Specialist Physician in selected cases.
Like Minded Docs www.likemindeddocs.com
Addiction Concepts Holistic Recovery Therefore, recovery must be holistic (biopsycho-social-spiritual) in the context of abstinence Abstinence from all substances is essential, even if it was not your substance of choice as consumption puts you at risk Recovery for problem behaviours is more complicated, must look at bottom line behaviours
Physical Prognosis: Brain Proper nutrition for neurotransmitter production and function Exercise promotes healthy circulation and release of “feel good” chemicals (endorphins and endocannabinoids) Development of new synaptic pathways with reinforcement of healthy thinking, dealing with feelings, and behaviours
Physical Prognosis: Body Improved heart function and circulation to all organs to carry oxygen that is necessary for repair and function Organ healing (e.g., liver function restored over time although some cells may become scarred/cirrhosed) Improved lung function – healthy breathing (connection to relaxation and meditation)
Prognosis Addiction cannot be ‘cured’ or ‘fixed’ but it can be managed or dealt with treatment and support! Is progressive (think of a downwards escalator that people are climbing up) Holistic recovery can provide a quality of life and healthy lifestyle people never thought possible!
Holistic Recovery Biological: Regular exercise/physical activity (20-30 minutes/day, 3-4x/week) – Walking, yoga, cardio, weights, organized sports, Tai Chi, etc. Healthy, balanced diet – Lots of water, fruit, vegetables, lean protein – May or may not include supplements such as Omega, Vitamins Medication management (if needed)
Holistic Recovery Psychological: Focus on identifying and processing emotions – Journalling, talking Individual and group counselling Exploration of trauma, mental health and coping mechanisms – Relaxation, meditation, breathing
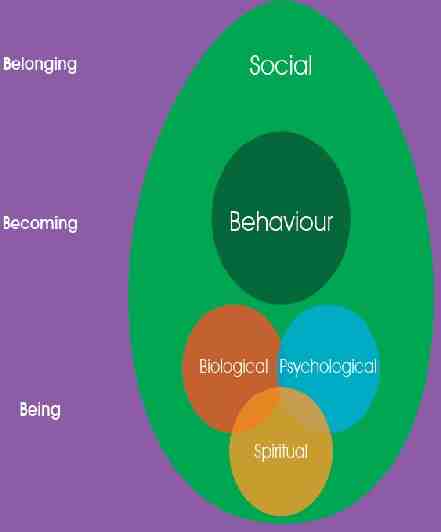
Holistic Recovery Social: 12 Step meetings Developing recovery peer supports Addressing relationship issues Work, school, volunteering Engagement with others to minimize isolation and stigma FUN! “From isolation to connectedness ”
Holistic Recovery Spiritual: Re-establishing connection with spirituality through individual reflection, prayer, ceremonies, group gatherings, etc. Reconnecting with universe, idea that you are supported and not alone
Characteristics of Addiction Key feelings with Addiction are: Shame, anger, and fear Isolation Lack of connection with self, others, and the universe Holistic recovery provides a platform of healthy coping with these challenges

Remission A state of wellness where there is an abatement of signs and symptoms that characterize active addiction. Many individuals in a state remission state remain actively engaged in the process of recovery. Reduction in signs or symptoms constitutes improvement in a disease state, but remission involves a return to a level of functioning that is free of active symptoms and/or is marked by stability in the chronic signs and symptoms that characterize active addiction.
Relapse A process in which an individual who has established abstinence or sobriety experiences recurrence of signs and symptoms of active addiction, often including resumption of the pathological pursuit of reward and/or relief through the use of substances and other behaviors. When in relapse, there is often disengagement from recovery activities. Relapse can be triggered by exposure to rewarding substances and behaviors, by exposure to environmental cues to use, and by exposure to emotional stressors that trigger heightened activity in brain stress circuits. The event of using or acting out is the latter part of the process, which can be prevented by early intervention.
Sobriety A state of sustained abstinence with a clear commitment to and active seeking of balance in the biological, psychological, social and spiritual aspects of an individual’s health and wellness that were previously compromised by active addiction. Abstinence Recovery Sobriety!
Johari Window
Johari Window Disease of Addiction thrives in the ‘blind’ and ‘secret’ panes As families/supports are so focused on the addict, life may be in the ‘blind’, ‘secret’, or ‘unknown’ unknown pane Recovery goal for everyone is to shed light on challenges and move to the ‘open’ pane
Lifestyle Move from looking at behavioural change to lifestyle change with holistic recovery Life may look completely different than in active Addiction, which can fuel fear and apprehension Important that the whole family system look at healthy change, not just the person with identified Addiction

Transition The transition to this new lifestyle can be difficult, comes with lots of challenges and emotions Important that each family member focus on their own personal journey – try not to blame, shame, judge, or critique others
Supporting Loved Ones Establish an alcohol-free home Learn about the disease of Addiction Avoid policing/monitoring your loved one Don’t encourage your loved one to ‘just try harder’ or control their disease, as this will fuel feelings of shame Support their recovery actions Set boundaries Engage in your own process of recovery and self-care
Resources Addictive Thinking by Abraham Twerski The Selfish Brain by Robert DuPont www.asam.org Melody Beattie books on Codependence such as The Codependent’s Guide to the 12 Steps, Codependent No More, and The Language of Letting Go Al-Anon and Nar-Anon National Institute on Drug Abuse (NIDA): www.drugabuse.org Hazelden for books, CDs, DVDs on Addiction & Recovery Desire, when sex meets addiction by Susan Cheever Facing Life by Nancy Brown Deceived: Facing Sexual Betrayal, Lies, and Secrets by Claudia Black Facing Codependence and Facing Love Addiction by Pia Mellody
Remember Key Messages: – Addiction is a brain disease – It is not the person’s fault they have this disease – Addiction is not about bad choices or wanting to hurt loved ones – Addiction impacts the whole family unit and everyone plays a role in recovery

Addiction in the Family Often the dynamic in families shifts to a focus on the identified person with Addiction Time, energy, money, and other resources go into helping care for this individual Meanwhile, the care of other family members is not prioritized Healthy recovery for the struggling addict involves everyone taking steps to be healthy
Addiction in the Family With genetic predisposition, everyone in the biological family unit may be at risk of developing the disease, or other behavioural, emotional, or thinking patterns may be present that are counterproductive If you are the partner or non-biological relative of someone struggling with Addiction, it is important for you to look honestly at your genetic risk as well as current health
Addiction in the Family The Family Laws of Addiction: – Don’t Talk – Don’t Trust – Don’t Feel (It Will Never Happen to Me by Claudia Black) The Family Laws of Recovery: – Talk – Trust – Feel
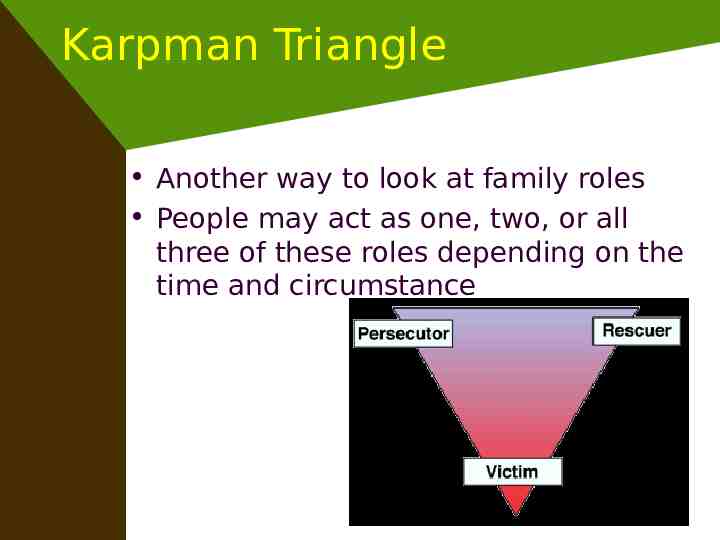
Karpman Triangle Another way to look at family roles People may act as one, two, or all three of these roles depending on the time and circumstance
Karpman Triangle Perpetrator: Blames and pressures the person who is struggling – Drawback: Perpetuates shame Rescuer: Wants to fix, caretake, keep the peace – Drawback: Enabling of behaviour Victim: Feeling hopeless, worthless, punished, and in an unfair position over which they have no power. Vulnerable to persecution and often looking for rescuing – Drawback: Lack of personal accountability
Boundaries Personal boundaries are: guidelines, rules or limits that a person creates to identify for him- or herself what are reasonable, safe and permissible ways for other people to behave around him or her and how he or she will respond when someone steps outside those limits
Boundaries Important to remember that boundaries are internal – we cannot force someone to respect our boundary! This is our responsibility to ourselves Difference between boundaries and expectations Expectations: when we expect somebody else to act differently Boundaries: when we act differently as a result of an internal line we have set
Boundaries Are: Yours Internal What you will/will not accept for yourself Do not need to be respected by others Are set by you, for you
Boundaries Become more clearly defined as you gain clarity on who you are What gives me meaning? What do I value? What is healthy for me? These questions help define boundaries in the context of spirituality
Boundaries & Communication You have the right to vocalize your needs to others, but don’t expect them to change as a result It is also important to have a plan of action in case the verbalization of your boundary is not accepted – “Please do not raise your voice with me. If you do, I will step away from this conversation”
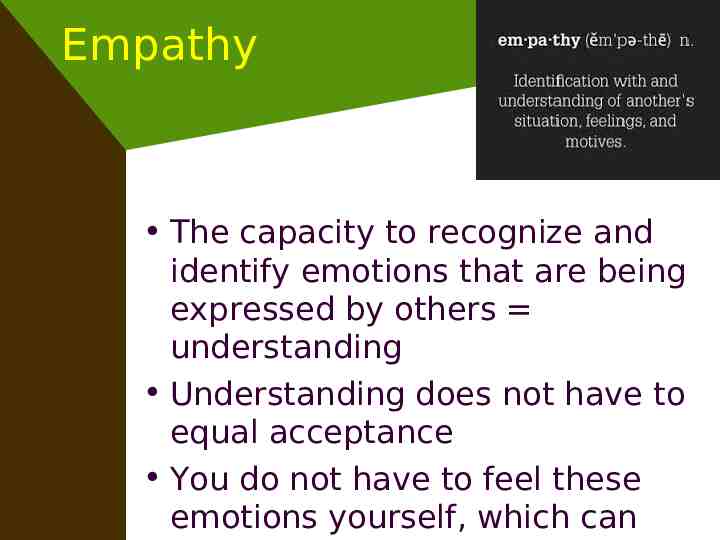
Empathy The capacity to recognize and identify emotions that are being expressed by others understanding Understanding does not have to equal acceptance You do not have to feel these emotions yourself, which can

Paradigm shift Addicted to needs to change to Addiction involving “Alcohol is but a symptom of our disease” AA Big Book RAiAR – Remember Addiction is Addiction Responsible Recovery – 9 steps – 1,2,3 – willing to consider ; 4,5,6 – can and will (action); and 7,8,9 – responsibility Outcomes to be determined by the grace of our Higher Power
Addiction Treatment There is no such thing as “treatment failure” Only failure of providing the appropriate treatment Treatment has to be comprehensive, ongoing, in the chronic disease framework, with holistic – biological, psychological, social and spiritual recovery!
Addiction is Addiction www.addictionisaddictionbook.com Addiction is Addiction: Understanding the disease in oneself and others for a better quality of life Raju Hajela Sue Newton Paige Abbott Friesen Press, 2015