1 The Impact of Video Monitoring on Patient Falls and Cost of Care
38 Slides3.15 MB
1 The Impact of Video Monitoring on Patient Falls and Cost of Care Ellen BarringtonApril DNP, RN-BC, NEA-BC Marie Foley-Danecker DNP, RN, CCRN, NE-BC Cira Fraser PhD., RN, ACNS-BC Janet Mahoney, PhD., RN, APN-C, NEA-BC
2 Presentation Outline 1 Introduction to Falls and Video Monitoring 2 Critique and Review of the Literature 3 Methods 4 Data Collection and Analysis 5 Results 6 Discussion 7 Implications 8 Limitations 9 Conclusions
3 The purpose of this study was to examine the impact of video monitoring on patient falls and cost of care.
4 Background and Significance Hundreds of thousands of Video monitoring - patients fall, newest technology 30-50% result in injury to prevent patient annually (The Joint falls Commission, 2015) Since 2009, 465 falls Prevention Strategies - with injury, 63% low-cost personal alarms, costly 1:1 direct observation (Rausch, Bjorkland, 2010) resulted in death (The Cost of inpatient falls 54.9 Joint Commission, billion by 2020 (CDC, 2013) 2015)
5 PICOT Question In hospitalized adults (P), how does the use of a patient video monitoring system (I) versus the usual care (C), impact patient falls and affect the cost of care (O) over a six-month period in two hospitals (T)?
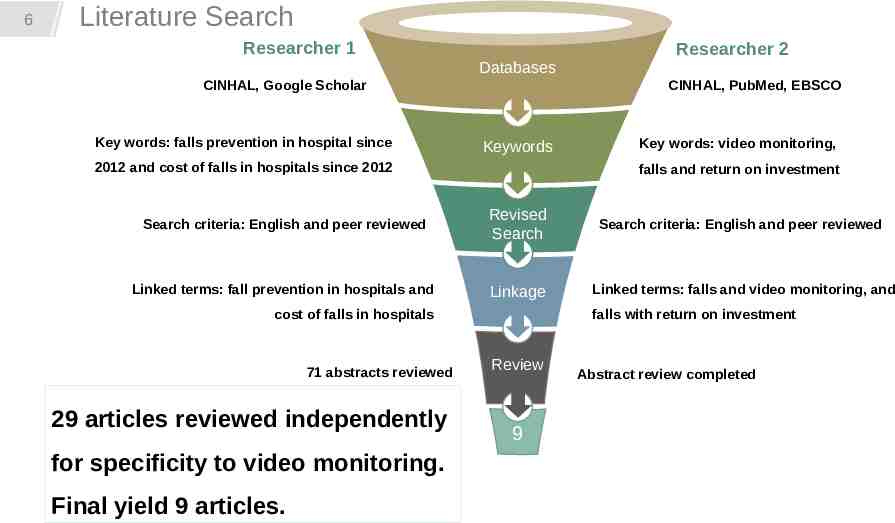
6 Literature Search Researcher 1 Researcher 2 Databases CINHAL, Google Scholar Key words: falls prevention in hospital since CINHAL, PubMed, EBSCO Keywords 2012 and cost of falls in hospitals since 2012 Key words: video monitoring, falls and return on investment Search criteria: English and peer reviewed Revised Search Search criteria: English and peer reviewed Linked terms: fall prevention in hospitals and Linkage Linked terms: falls and video monitoring, and cost of falls in hospitals 71 abstracts reviewed 29 articles reviewed independently for specificity to video monitoring. Final yield 9 articles. falls with return on investment Review 9 Abstract review completed
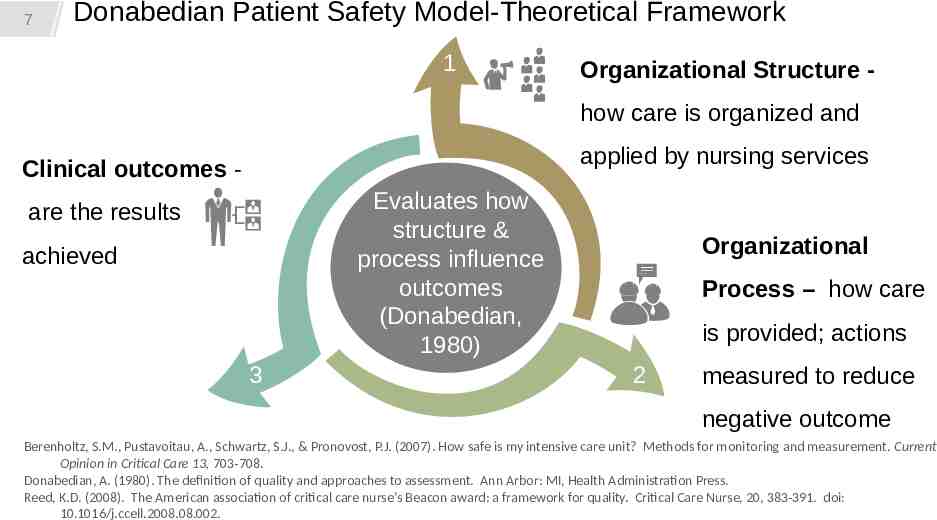
7 Donabedian Patient Safety Model-Theoretical Framework 1 Organizational Structure how care is organized and applied by nursing services Clinical outcomes Evaluates how structure & process influence outcomes (Donabedian, 1980) are the results achieved 3 Organizational Process – how care is provided; actions 2 measured to reduce negative outcome Berenholtz, S.M., Pustavoitau, A., Schwartz, S.J., & Pronovost, P.J. (2007). How safe is my intensive care unit? Methods for monitoring and measurement. Current Opinion in Critical Care 13, 703-708. Donabedian, A. (1980). The definition of quality and approaches to assessment. Ann Arbor: MI, Health Administration Press. Reed, K.D. (2008). The American association of critical care nurse’s Beacon award: a framework for quality. Critical Care Nurse, 20, 383-391. doi: 10.1016/j.ccell.2008.08.002.
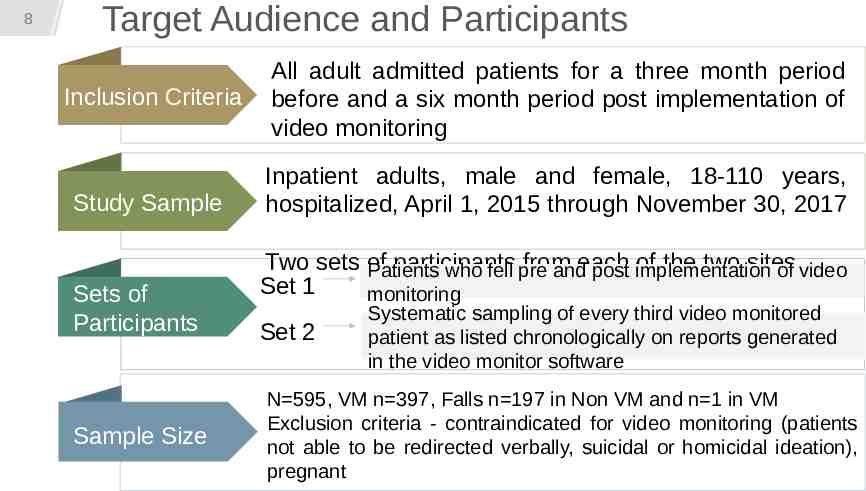
8 Target Audience and Participants Inclusion Criteria Study Sample Sets of Participants Sample Size All adult admitted patients for a three month period before and a six month period post implementation of video monitoring Inpatient adults, male and female, 18-110 years, hospitalized, April 1, 2015 through November 30, 2017 Two sets of participants from of the two sites Patients who fell pre andeach post implementation of video Set 1 monitoring Set 2 Systematic sampling of every third video monitored patient as listed chronologically on reports generated in the video monitor software N 595, VM n 397, Falls n 197 in Non VM and n 1 in VM Exclusion criteria - contraindicated for video monitoring (patients not able to be redirected verbally, suicidal or homicidal ideation), pregnant
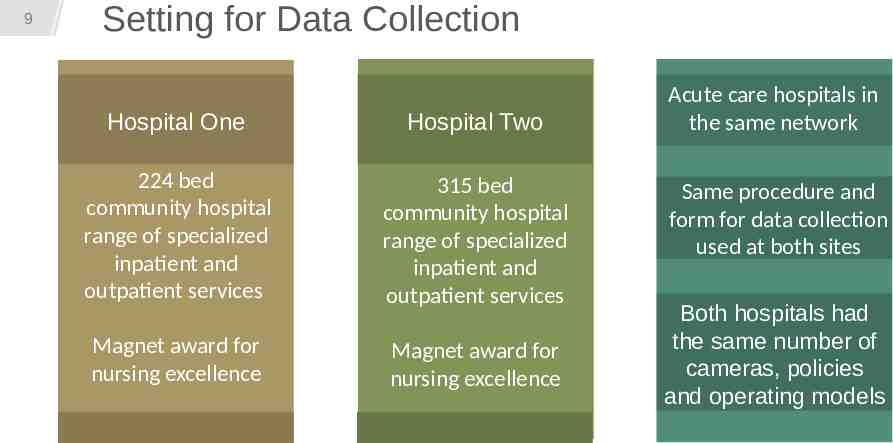
9 Setting for Data Collection Hospital One Hospital Two 224 bed community hospital range of specialized inpatient and outpatient services 315 bed community hospital range of specialized inpatient and outpatient services Magnet award for nursing excellence Magnet award for nursing excellence Acute care hospitals in the same network Same procedure and form for data collection used at both sites Both hospitals had the same number of cameras, policies and operating models
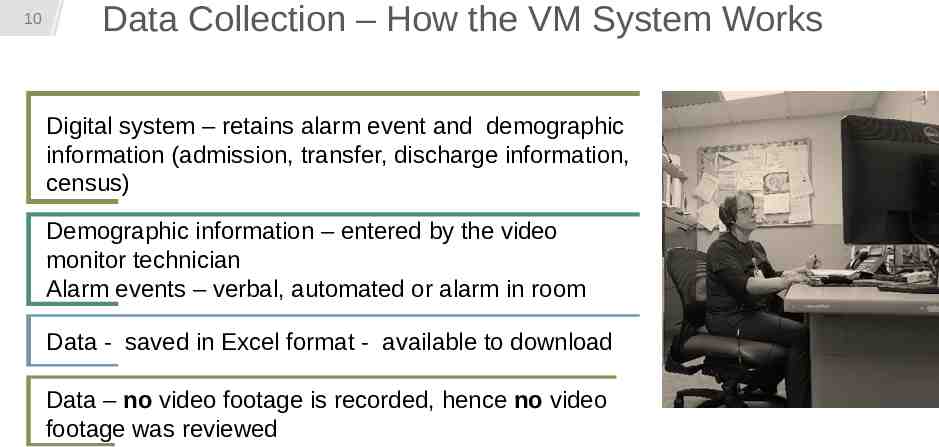
10 Data Collection – How the VM System Works Digital system – retains alarm event and demographic information (admission, transfer, discharge information, census) Demographic information – entered by the video monitor technician Alarm events – verbal, automated or alarm in room Data - saved in Excel format - available to download Data – no video footage is recorded, hence no video footage was reviewed
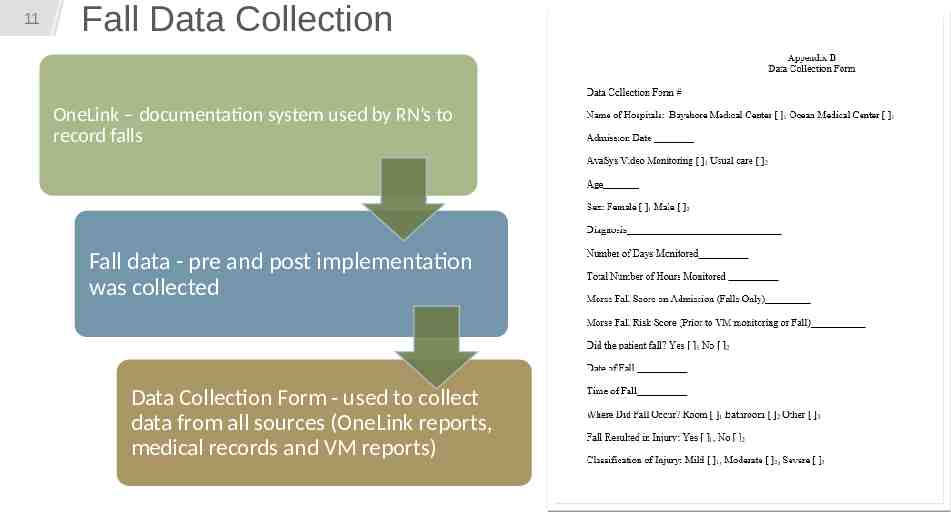
11 Fall Data Collection OneLink – documentation system used by RN’s to record falls Fall data - pre and post implementation was collected Data Collection Form - used to collect data from all sources (OneLink reports, medical records and VM reports)
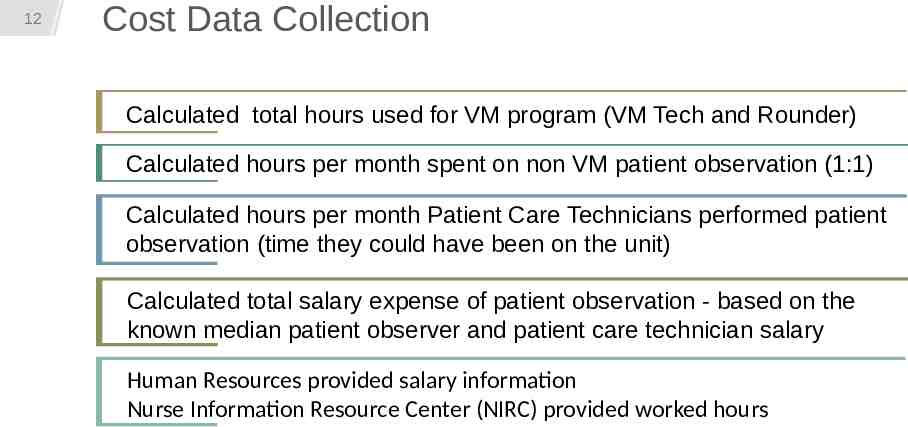
12 Cost Data Collection Calculated total hours used for VM program (VM Tech and Rounder) Calculated hours per month spent on non VM patient observation (1:1) Calculated hours per month Patient Care Technicians performed patient observation (time they could have been on the unit) Calculated total salary expense of patient observation - based on the known median patient observer and patient care technician salary Human Resources provided salary information Nurse Information Resource Center (NIRC) provided worked hours

Cost of Falls to the Organization 30,000 Estimated cost of a fall with injury 41 1,230,000 Falls with injury Financial Risk to the organization In 9-month total sample period 30,000 X 41 Financial risk Burns, E. R., Stevens, J. A., & Lee, R. (2016). The direct costs of fatal and non-fatal falls among older adults – United States. Journal of Safety Research, Sep (58), 99-103. doi: 10.1016/j.jsr.2016.05.001. Centers for Disease Control & Prevention. (2016, August 19). Costs of falls among older adults. Retrieved from https://www.cdc.gov/homeandrecreationalsafety/falls/fallcost.html
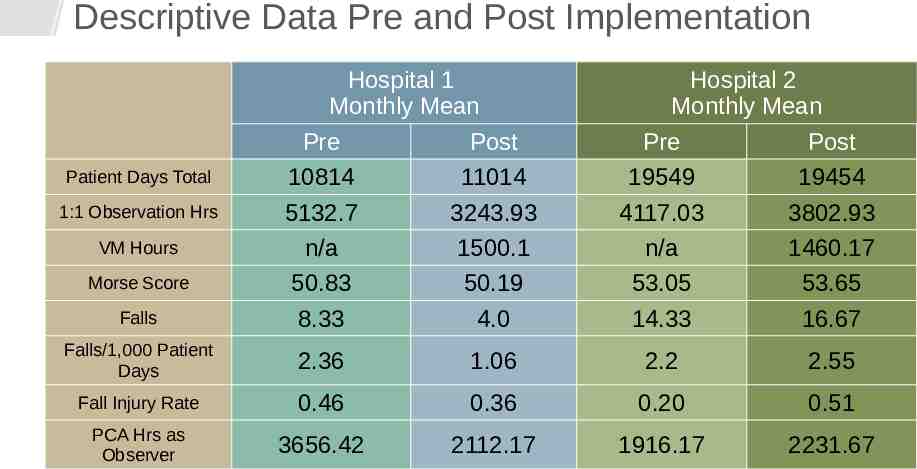
Descriptive Data Pre and Post Implementation Patient Days Total 1:1 Observation Hrs VM Hours Morse Score Falls Hospital 1 Monthly Mean Pre Post 10814 11014 5132.7 3243.93 n/a 1500.1 50.83 50.19 8.33 4.0 Hospital 2 Monthly Mean Pre Post 19549 19454 4117.03 3802.93 n/a 1460.17 53.05 53.65 14.33 16.67 Falls/1,000 Patient Days 2.36 1.06 2.2 2.55 Fall Injury Rate 0.46 0.36 0.20 0.51 PCA Hrs as Observer 3656.42 2112.17 1916.17 2231.67
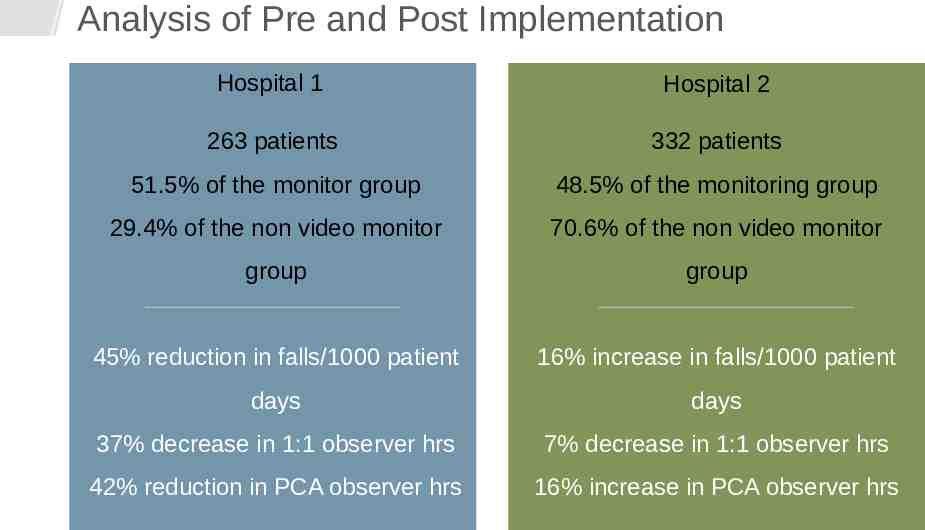
Analysis of Pre and Post Implementation Hospital 1 Hospital 2 263 patients 332 patients 51.5% of the monitor group 48.5% of the monitoring group 29.4% of the non video monitor 70.6% of the non video monitor group group 45% reduction in falls/1000 patient 16% increase in falls/1000 patient days days 37% decrease in 1:1 observer hrs 7% decrease in 1:1 observer hrs 42% reduction in PCA observer hrs 16% increase in PCA observer hrs
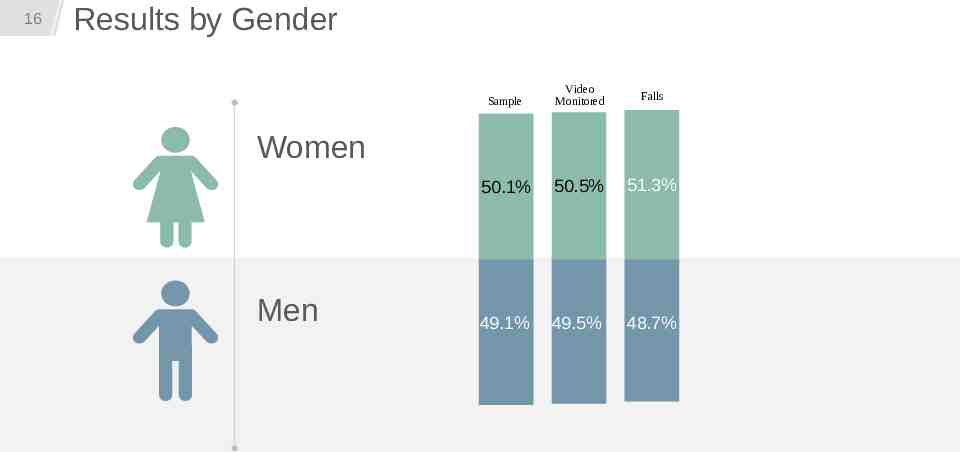
16 Results by Gender Sample Video Monitored Falls 50.1% 50.5% 51.3% 49.1% 49.5% 48.7% Women Men
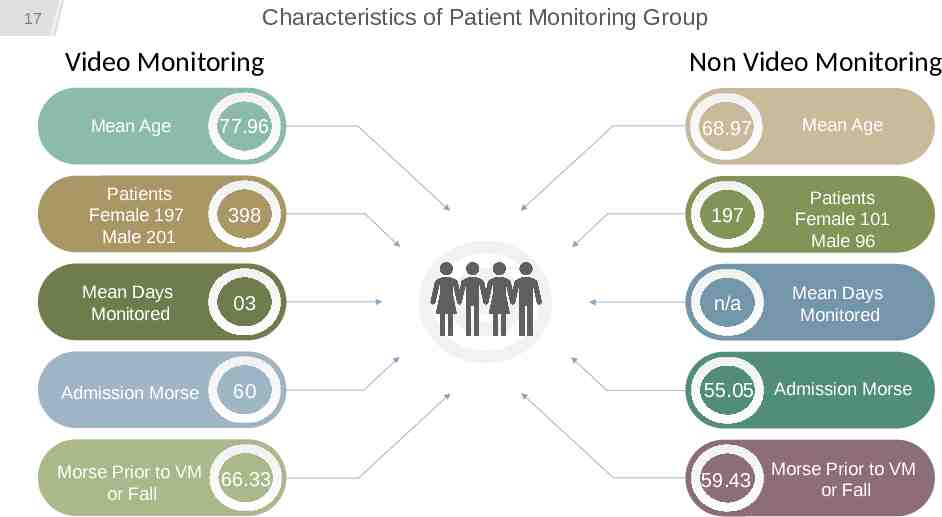
Characteristics of Patient Monitoring Group 17 Video Monitoring Non Video Monitoring 68.97 Mean Age 398 197 Patients Female 101 Male 96 Mean Days Monitored 03 n/a Mean Days Monitored Admission Morse 60 Morse Prior to VM or Fall 66.33 Mean Age Patients Female 197 Male 201 77.96 55.05 Admission Morse 59.43 Morse Prior to VM or Fall
18 Analysis of Patient Monitoring Group Change in Morse The change in Morse score for the patients who fell in the non VM group (n 197) from admission to prior to fall was significant (t 3.279, p 0.001). Gender Slightly more men were video monitored, and marginally more women fell Relationship between falls and Morse score A Pearson's Correlation revealed a strong, positive relationship between falls by month and average Morse scores by month in 2016 (r 0.847, p .000), which explained 72% of the variance. In 2017, 73% of the variance between falls by month and average Morse was explained with the Pearson’s Correlation (r 0.854, p .000). Relationship between volume and falls In 2016, Pearson’s Correlations between patient days by month and falls by month showed a strong positive correlation (r 0.762, p 0.001). In 2017, Pearson’s Correlation between patient days by month and falls by month showed a strong positive correlation (r .904, p 0.000).
19 Fall Severity Pre and Post Video Monitoring 41 falls with injury Fall injury scale 1-3: 1 mild 2 moderate 3 severe Pre-video monitored fall severity average was 1.36. Post video monitored fall severity decreased to 1.24
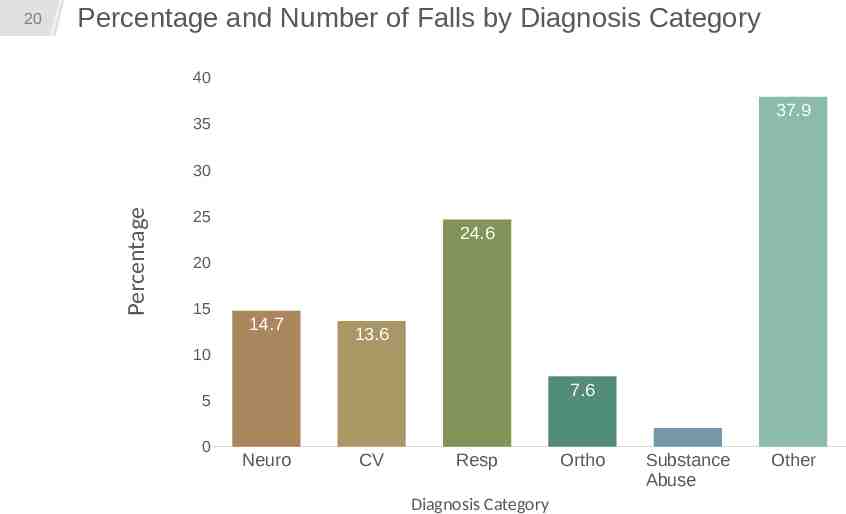
Percentage and Number of Falls by Diagnosis Category 40 37.9 35 30 Percentage 20 25 24.6 20 15 14.7 13.6 10 7.6 5 0 2 Neuro CV Resp Diagnosis Category Ortho Substance Abuse Other
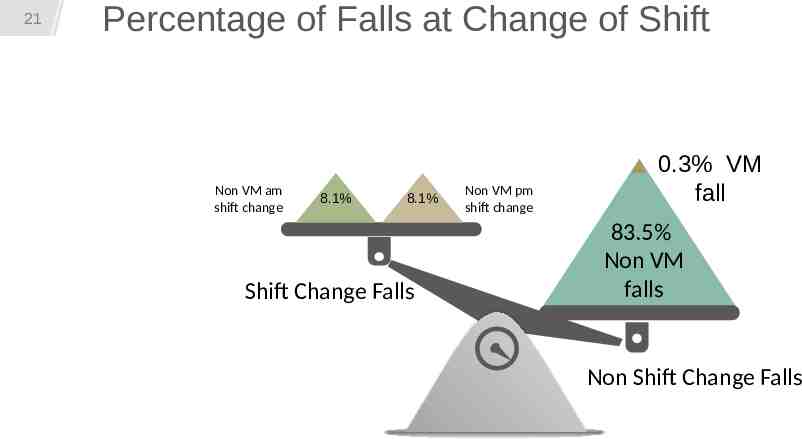
21 Percentage of Falls at Change of Shift 83.5 falls mid shift Non VM am shift change 8.1% 8.1% Shift Change Falls Non VM pm shift change 0.3% VM fall 83.5% Non VM falls Non Shift Change Falls 60 Morse Admission
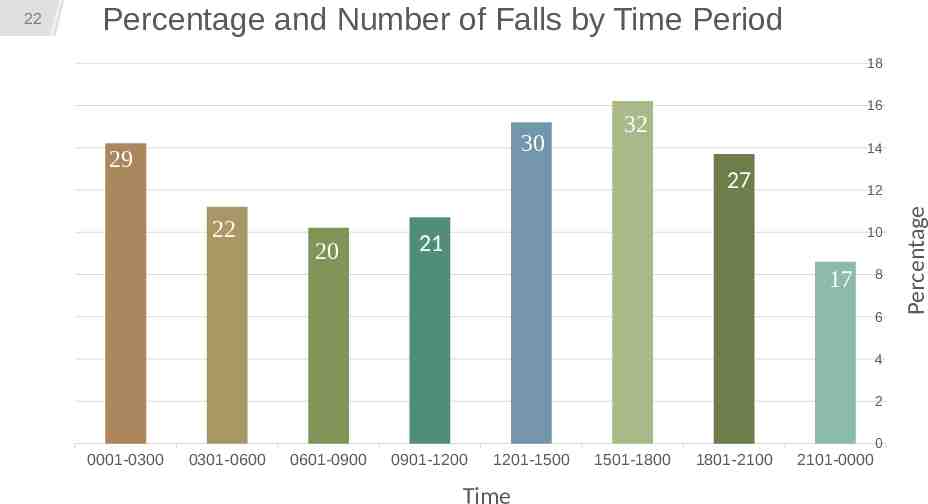
Percentage and Number of Falls by Time Period 18 30 29 16 32 14 27 22 20 12 10 21 17 8 6 4 2 0001-0300 0301-0600 0601-0900 0901-1200 1201-1500 Time 1501-1800 1801-2100 2101-0000 0 Percentage 22
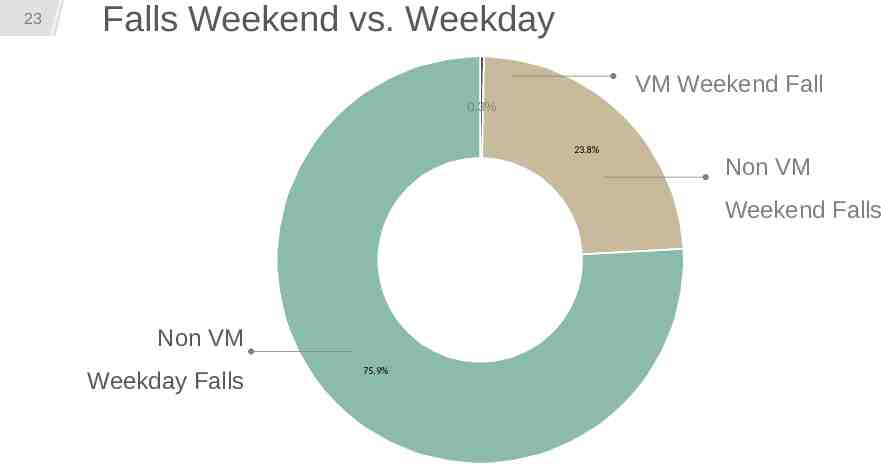
23 Falls Weekend vs. Weekday VM Weekend Fall 0.3% 23.8% Non VM Weekend Falls Non VM Weekday Falls 75.9%
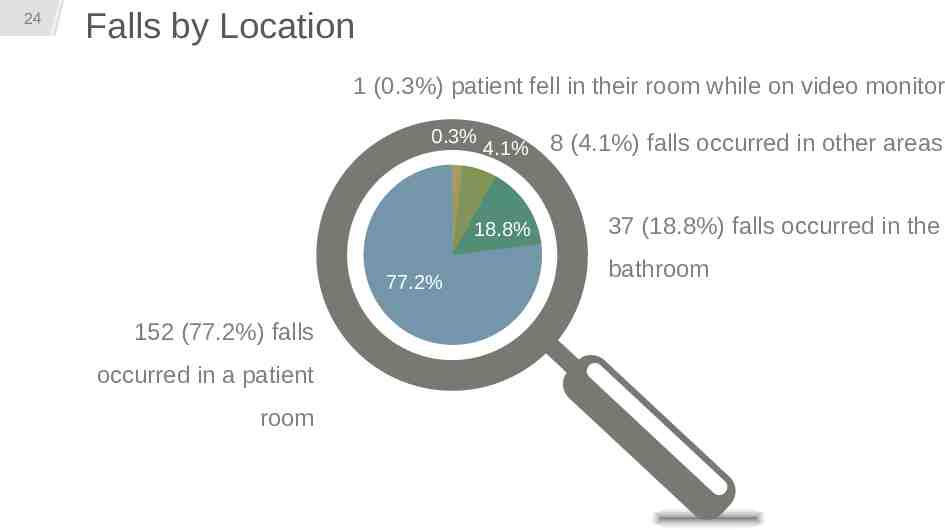
24 Falls by Location 1 (0.3%) patient fell in their room while on video monitor 0.3% 77.2% 152 (77.2%) falls occurred in a patient room 4.1% 8 (4.1%) falls occurred in other areas 18.8% 37 (18.8%) falls occurred in the bathroom
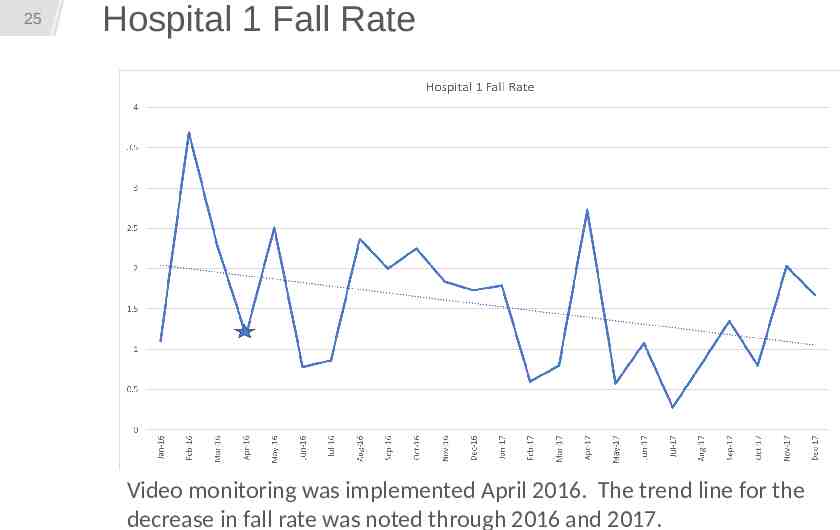
25 Hospital 1 Fall Rate Video monitoring was implemented April 2016. The trend line for the decrease in fall rate was noted through 2016 and 2017.
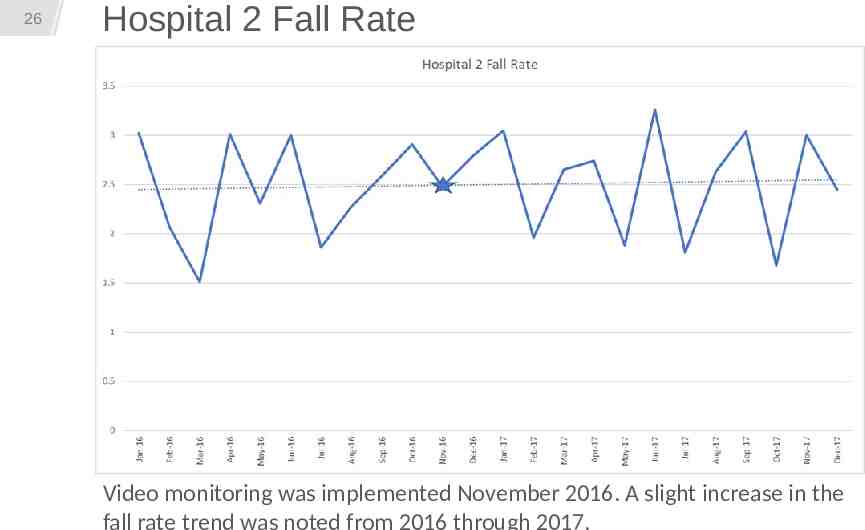
26 Hospital 2 Fall Rate Video monitoring was implemented November 2016. A slight increase in the
Findings 1 2 3 4 5 Hospital 1 Hospital 2 Significant Reduced: Reduced: Reduced: Reduced: change: fall severity 1:1 observation patient 1:1 observation Morse score from 1.36 to hrs 24% falls/1,000 hrs on admission 1.24 cost per patient days Increased: and Morse observed hr one to one patient falls/1,000 score just 20% observation hrs patient days before fall PCA as observer PCA as observer hrs hrs
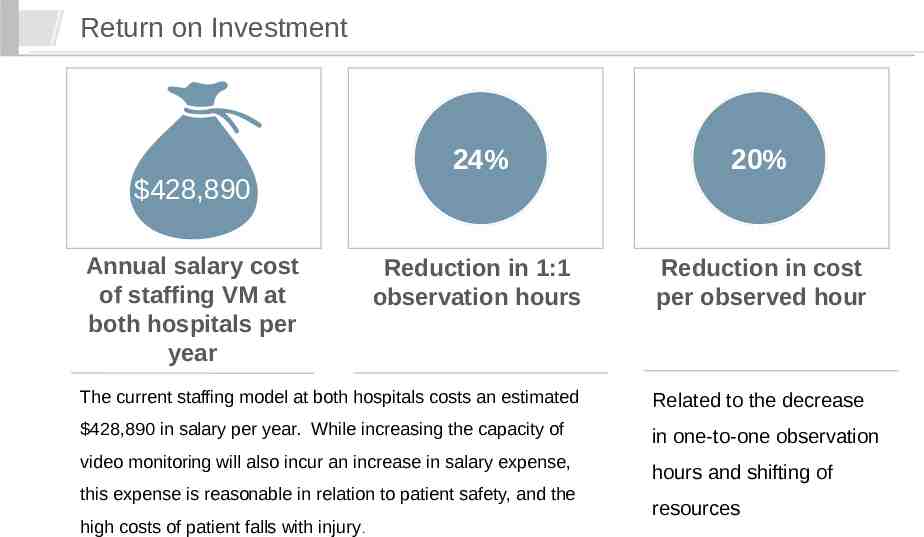
Return on Investment 24% 20% Reduction in 1:1 observation hours Reduction in cost per observed hour The current staffing model at both hospitals costs an estimated Related to the decrease 428,890 in salary per year. While increasing the capacity of in one-to-one observation 428,890 Annual salary cost of staffing VM at both hospitals per year video monitoring will also incur an increase in salary expense, this expense is reasonable in relation to patient safety, and the high costs of patient falls with injury. hours and shifting of resources
29 Discussion The study found a strong positive correlation between patient days and number of patient falls. Hospital 2 had 44% more patient days than Hospital 1. Both Hospital 1 and Hospital 2 implemented the VM program with the same amount of video monitoring cameras. Not evident in the research of the literature is the number of video monitoring cameras based on hospital size necessary to impact patient falls. However, based on the difference in size of the two hospitals, the correlation between patient days and falls, and the impact of ten cameras on the smaller hospital’s fall rate, further exploration is warranted. Hospital 2 used more PCA as observer hours in the post implementation period. Removing frontline caregivers to provide 1:1 observation has been shown to deplete staffing resources (Sand-Jecklin, Johnson, & Tylka, 2016) and does not decrease falls (Boswell, Ramsey, Smith, and Wagers, 2001; Harding, 2010; Tzeng & Yin, 2007). Consistent with the published research, the increase in PCA as observer hours in Hospital 2 could be a confounding factor to explain why falls increased exclusive of VM implementation. Boswell, D. J., Ramsey, J., Smith, M. A., & Wagers, B. (2001). The cost-effectiveness of a patient sitter program in an acute care hospital: A test of the impact of sitters on the incidence of falls and patient satisfaction. Quality Management in Healthcare, 10(1), 10-16. Harding, A. D. (2010). Observation assistants: Sitter effectiveness and industry measures. Nursing Economics, 28(5), 330-336. Sand-Jecklin, K, Johnson, J.R., & Tylka, S. (2016). Protecting patient safety: Can video monitoring prevent falls in high-risk patient populations? Journal of Nursing Care Quality, 31(2), 131-138.
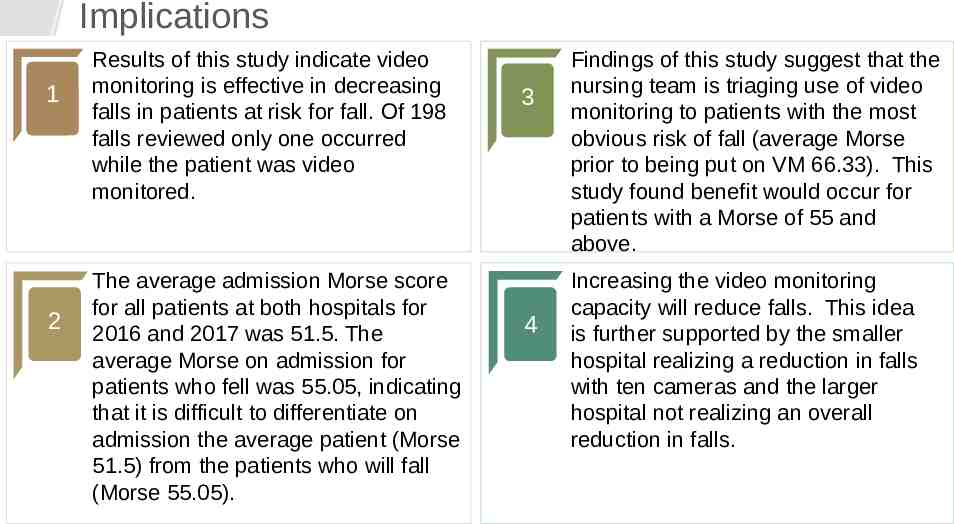
Implications 1 2 Results of this study indicate video monitoring is effective in decreasing falls in patients at risk for fall. Of 198 falls reviewed only one occurred while the patient was video monitored. The average admission Morse score for all patients at both hospitals for 2016 and 2017 was 51.5. The average Morse on admission for patients who fell was 55.05, indicating that it is difficult to differentiate on admission the average patient (Morse 51.5) from the patients who will fall (Morse 55.05). 3 4 Findings of this study suggest that the nursing team is triaging use of video monitoring to patients with the most obvious risk of fall (average Morse prior to being put on VM 66.33). This study found benefit would occur for patients with a Morse of 55 and above. Increasing the video monitoring capacity will reduce falls. This idea is further supported by the smaller hospital realizing a reduction in falls with ten cameras and the larger hospital not realizing an overall reduction in falls.
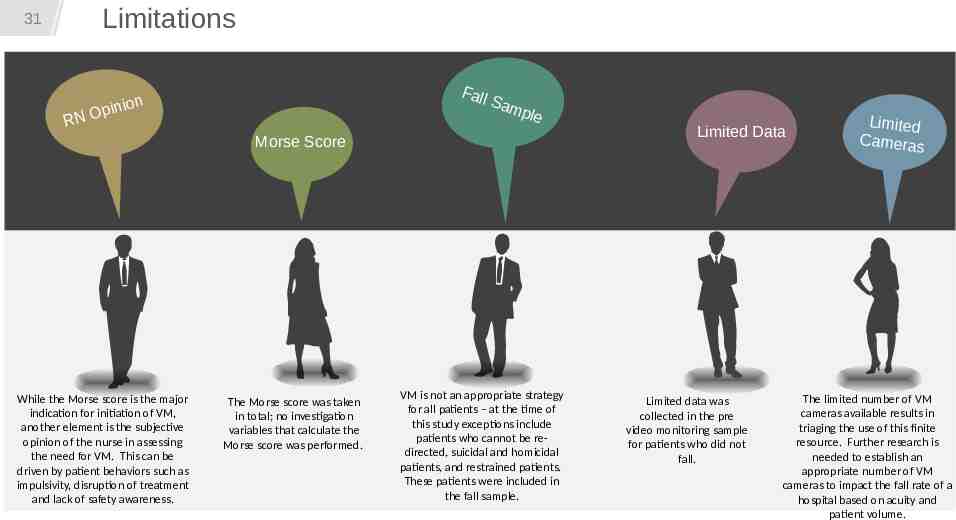
Limitations 31 RN Fall Sam pl ion Opin e Morse Score While the Morse score is the major indication for initiation of VM, another element is the subjective opinion of the nurse in assessing the need for VM. This can be driven by patient behaviors such as impulsivity, disruption of treatment and lack of safety awareness. The Morse score was taken in total; no investigation variables that calculate the Morse score was performed. VM is not an appropriate strategy for all patients – at the time of this study exceptions include patients who cannot be redirected, suicidal and homicidal patients, and restrained patients. These patients were included in the fall sample. Limited Data Limited data was collected in the pre video monitoring sample for patients who did not fall. Limited Cameras The limited number of VM cameras available results in triaging the use of this finite resource. Further research is needed to establish an appropriate number of VM cameras to impact the fall rate of a hospital based on acuity and patient volume.
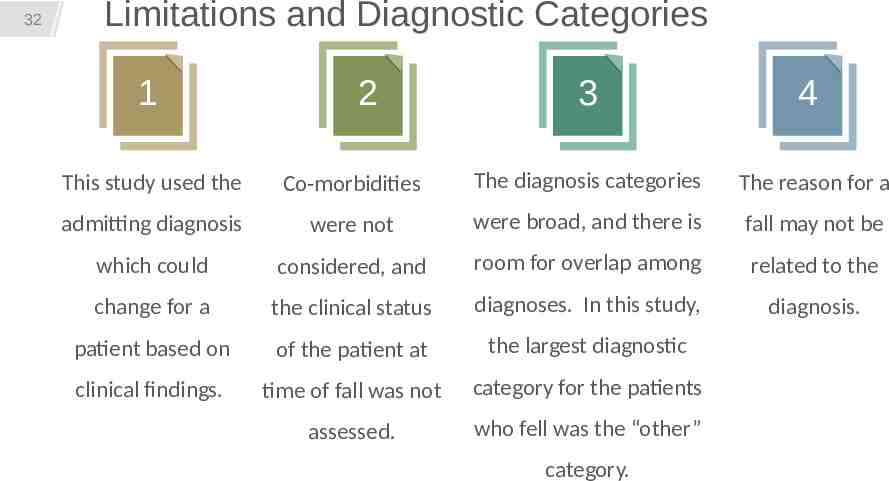
32 Limitations and Diagnostic Categories 1 2 3 4 This study used the Co-morbidities The diagnosis categories The reason for a admitting diagnosis were not were broad, and there is fall may not be which could considered, and room for overlap among related to the change for a the clinical status diagnoses. In this study, diagnosis. patient based on of the patient at the largest diagnostic clinical findings. time of fall was not category for the patients assessed. who fell was the “other” category.
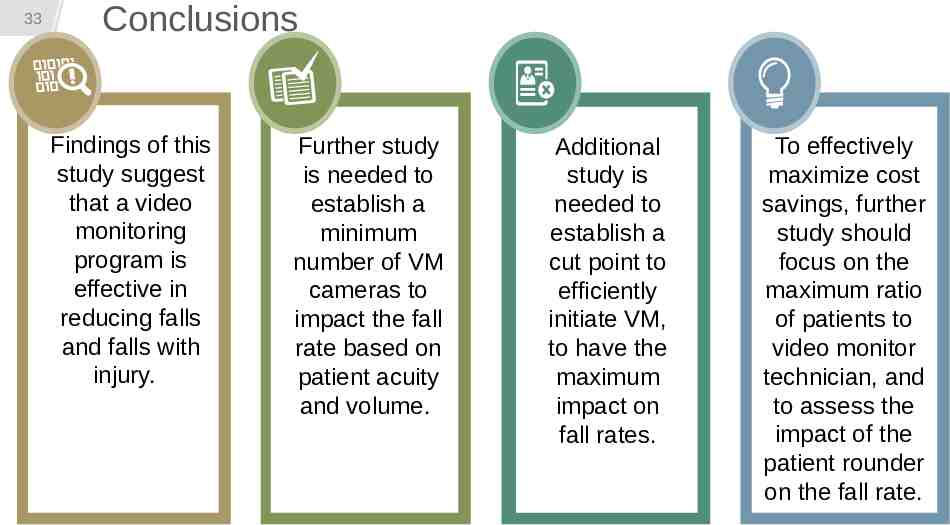
33 Conclusions Findings of this study suggest that a video monitoring program is effective in reducing falls and falls with injury. Further study is needed to establish a minimum number of VM cameras to impact the fall rate based on patient acuity and volume. Additional study is needed to establish a cut point to efficiently initiate VM, to have the maximum impact on fall rates. To effectively maximize cost savings, further study should focus on the maximum ratio of patients to video monitor technician, and to assess the impact of the patient rounder on the fall rate.
34 Any Questions ?
35 Thank you
36 References Aydin, C., Donaldson, N., Aronow, H. U., Fridman, M., & Brown, D. S. (2015). Improving hospital patient falls. Journal of Nursing Administration, 45(5), 254-262. Bayen, E., Jacquemot, J., Netscher, G., Agrawal, P., Noyce, L. T., & Bayen, A. (2017). Reduction in fall rate in dementia managed care through video incident review: Pilot study. Journal of Medical Internet Research, 19(10), 1-16. Berenholtz, S.M., Paustavoitau, A., Schwartz, S.J., & Pronovost, P.J. (2007). How safe is my intensive care unit? Methods for monitoring and measurement. Current Opinion in Critical Care 13, 703-708. Borikova, I., Tomagova, M., Miertova, M., & Ziakova, K. (2017). Predictive value of the Morse fall score. Central European Journal of Nursing and Midwifery, 8(1), 588-595. Boswell, D. J., Ramsey, J., Smith, M. A., & Wagers, B. (2001). The cost-effectiveness of a patient sitter program in an acute care hospital: A test of the impact of sitters on the incidence of falls and patient satisfaction. Quality Management in Healthcare, 10(1), 10-16. Burns, E. R., Stevens, J. A., & Lee, R. (2016). The direct costs of fatal and non-fatal falls among older adults – United States. Journal of Safety Research, Sep (58), 99-103. doi: 10.1016/j.jsr.2016.05.001. Center for Disease Control. (2013). Costs of falls among older adults. Retrieved from http://balancengineering.com/wp-content/uploads/2011/08/cdc-costs-of-falls-among-older-adults.pdf Centers for Disease Control & Prevention. (2016, August 19). Costs of falls among older adults. Retrieved from https://www.cdc.gov/homeandrecreationalsafety/falls/fallcost.html Center for Medicare and Medicaid. (2008). CMS improves patient safety for Medicare and Medicaid patients by addressing never events. Retrieved from https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2008-Fact-sheets-items/2008-08-042.html? DLPage 2&DLEntries 10&DLSort 0&DLSortDir descending
37 References Cournan, M., Fusco-Gessick, B. and Wright, L. (2016). Improving patient safety through video monitoring. Rehabilitation Nursing. doi:10.1002/rnj.308 Davis, J., Kutash, M., & Whyte, J. (2017). A comparative study of patient sitters with video monitoring versus in-room sitters. Journal of Nursing Education and Practice, 7(3), 137-142. Donabedian, A. (1980). The definition of quality and approaches to assessment. Ann Arbor: MI, Health Administration Press. Dunne, T. J., & Gaboury, I., & Ashe, M. C. (2014). Falls in hospital increase length of stay regardless of degree of harm. Journal of Evaluation in Clinical Practice, 20, 396-400. Dunton, N., Gajewski, B., Klaus, S., & Pierson, B. (2007). The relationship of nursing Workforce characteristics to patient outcomes. OJIN: The Online Journal of Issues in Nursing, Vol. 12(3). Available: www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/ OJIN/TableofContents/Volume122007/No3Sept07/NursingWorkforceCharacteristics.aspx Hackensack Meridian Health. (2017). Bayshore Medical Center. Retrieved October 19, 2017, from http://www.bayshorehospital.org/B/aboutus/AwardsandRecognition.cfm Hackensack Meridian Health. (2017). Ocean Medical Center. Retrieved October 20, 2017, from http://www.oceanmedicalcenter.com/OMC/aboutus/AwardsandRecognition.cfm Hardin, S. R., Dienemann, J., Rudisill, P., & Mills K. K. (2013). Inpatient fall prevention: Use of in-room webcams. Journal of Patient Safety, 9(1), 29-35. Harding, A. D. (2010). Observation assistants: Sitter effectiveness and industry measures. Nursing Economics, 28(5), 330-336. Johnson, M., George, A., & Tran, D. T. (2011). Analysis of falls incidents: Nurse and patient preventive behaviours. International Journal of Nursing Practice, 17(1), 60-66.
38 References Klymko, K., Etcher, L., Munchiando, J., & Royce, M. (2016). Video monitoring: A room with a view, or a window to challenges in falls prevention research? MEDSURG Nursing, 25(5), 329-333. Morse, J. M., Black, C., Oberle, K., & Donahue, P. (1989). A prospective study to identify the fall-prone patient. Social Sciences Medicine, 28(1), 81-86. Oliver, D., Healey, F., & Haines, T. P. (2010). Preventing falls and fall-related injuries in hospitals. Clinics in Geriatric Medicine, 26, 645-692. Rausch, D. L., & Bjorklund, P. (2010). Decreasing the costs of constant observation. Journal of Nursing Administration, 40(2), 75-81. Reed, K.D. (2008). The American association of critical care nurse’s Beacon award: a framework for quality. Critical Care Nurse, 20, 383-391. doi: 10.1016/j.ccell.2008.08.002. Robinovitch, S. N., Feldman, F., Yang, Y., Schonnop, R., Leung, P. M., Sarraf, T., Sims-Gould, J., & Loughin, M. (2013). Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. The Lancet, 381, 47-54. Sand-Jecklin, K, Johnson, J.R., & Tylka, S. (2016). Protecting patient safety: Can video monitoring prevent falls in high-risk patient populations? Journal of Nursing Care Quality, 31(2), 131-138. The Joint Commission. (2015, September 28). Preventing falls and fall-related injuries in health care facilities. Sentinel Event Alert, 55. Retrieved from https://www.jointcommission.org/assets/1/18/SEA 55.pdf Tzeng, H., & Yin, C. (2007). Using family visitors, sitters, or volunteers to prevent inpatient falls. Journal of Nursing Administration, 37(7/8), 329334. Votruba, L., Graham, B., Wisinski, J., & Syed, A. (2016). Video monitoring to reduce falls and patient companion costs for adult inpatients. Nursing Economics, 34(4), 185-189.