YOUTH MENTAL HEALTH FIRST AID® USA FOR ADULTS ASSISTING YOUNG PEOPLE
55 Slides485.34 KB
YOUTH MENTAL HEALTH FIRST AID USA FOR ADULTS ASSISTING YOUNG PEOPLE MENTAL HEALTH FIRST AID USA FIRST EDITION (REVISED) 2016 STATISTICAL UPDATE

PROGRAM OVERVIEW Program Overview: Part 1 What is Youth Mental Health First Aid ? Adolescent development and mental health problems in youth. What you may see: Signs and symptoms. Risk factors and protective factors. Mental Health First Aid Action Plan. MENTAL HEALTH FIRST AID USA 2

PROGRAM Program Overview: Part 2 Using the Mental Health First Aid Action Plan: In non-crisis situations. In crisis situations. MENTAL HEALTH FIRST AID USA 3

WHAT IS YOUTH MENTAL HEALTH FIRST AID? Youth Mental Health First Aid is the help offered to a young person experiencing a mental health challenge, mental disorder or a mental health crisis. The first aid is given until appropriate help is received or until the crisis resolves. Mental Health First Aid does not teach people to diagnose or to provide treatment. MENTAL HEALTH FIRST AID USA 4

WHY YOUTH MENTAL HEALTH FIRST AID? Why Youth Mental Health First Aid ? Mental health problems are common. Mental health problems often develop during adolescence. Youth and young adults may experience mental health problems differently than adults. Youth may not be well informed. The sooner an individual gets help, the more likely they are to have a positive outcome. Stigma is associated with mental health problems. Professional help is not always on hand. MENTAL HEALTH FIRST AID USA 5

YOUR ROLE What is your role? Parent/Guardian/Grandparent. Clergy. Friend or Neighbor. Peer. Professional: “In the place of the parent.” Be aware of: Mandatory reporting laws. Privacy rights of young people. When to communicate with parents and other caregivers. MENTAL HEALTH FIRST AID USA 6

WHAT IS A MENTAL DISORDER? A mental disorder or mental illness is a diagnosable illness that: Affects a person’s thinking, emotional state and behavior. Disrupts the person’s ability to: Work or attend school. Carry out daily activities. Engage in satisfying relationships. MENTAL HEALTH FIRST AID USA 7

TYPES OF MENTAL DISORDERS What Are Some of the Disorders We Might Hear About? ADD/ADHD/ODD. Anxiety Disorders. Bipolar Disorder. Depression. Eating Disorders. Psychosis. Substance Use Disorders. MENTAL HEALTH FIRST AID USA 8

PREVALENCE U.S. Youth with a Mental Disorder During Adolescence (Age 13-18) Prevalence (%) With severe impact (%) Anxiety disorders 31.9 8.3 Behavior disorders 19.1 9.6 Mood disorders 14.3 11.2 Substance use disorders 11.4 n/a Overall prevalence (with severe impact) MENTAL HEALTH FIRST AID USA 22.2 9

PREVALENCE Additional Prevalence Highlights for U.S. Youth 3% of 13-17 year-olds have an eating disorder. 11% of school-aged youth have ADD/ADHD. MENTAL HEALTH FIRST AID USA 10

PREVALENCE Prevalence of Depression in Adolescence MENTAL HEALTH FIRST AID USA 11

AGE OF ONSET Median Age of Onset ½ of all lifetime cases of mental illness begin by age 14; ¾ by age 24. Anxiety Disorders – Age 11. Eating Disorders – Age 15. Substance Use Disorders – Age 20. Schizophrenia – Age 23. Bipolar – Age 25. Depression – Age 32. MENTAL HEALTH FIRST AID USA 12

ADOLESCENT DEVELOPMENT Adolescent Development Physical Changes: Changes in hormones. Increases in height and weight. Mental Changes: Developing more abstract thinking skills. Using more logic and reason in decision making. Forming own beliefs. Questioning authority. Heightened focus on physical concerns. MENTAL HEALTH FIRST AID USA 13

ADOLESCENT Adolescent Development Emotional Changes: Shifts mood quickly. Feels more intensely. Increases in risk-taking and impulsive behavior. Social Changes: Experimentation with different levels of social and cultural identity. Increase in peer influence. Awareness of sexual identity. Learns to manage relationships. MENTAL HEALTH FIRST AID USA 14

RESILIENCY Resiliency Most youth pass through adolescence with relatively little difficulty despite all of these challenges. When difficulties are encountered, youth tend to be quite resilient. They often: Thrive. Mature. Increase their competence. MENTAL HEALTH FIRST AID USA 15

SPECTRUM OF Spectrum of Mental Health Interventions MENTAL HEALTH FIRST AID USA 16

THE ACTION PLAN Mental Health First Aid The Action Plan Assess for risk of suicide or harm. Listen nonjudgmentally. Give reassurance and information. Encourage appropriate professional help. Encourage self-help and other support strategies. MENTAL HEALTH FIRST AID USA 17

SIGNS & Signs & Symptoms: Physical Gastrointestinal: Cardiovascular: choking, dry pounding heart, chest pain, rapid mouth, stomach heartbeat, blushing. pains, nausea, vomiting, diarrhea. Respiratory: fast breathing, Musculoskeletal: shortness of breath. muscle aches and pains, Neurological: restlessness, dizziness, tremors and headache, sweating, tingling, shaking, inability numbness. to relax. MENTAL HEALTH FIRST AID USA 18

SIGNS & Signs & Symptoms: Physical Pattern adjustments: overeating or not eating at all, sleeping much more or much less. Appearance: Change in hygiene, unkempt, eyes bloodshot or glassy, weight gain or loss. Hormonal: irregular menstrual cycle, loss of nocturnal emissions, loss of sexual desire. MENTAL HEALTH FIRST AID USA 19
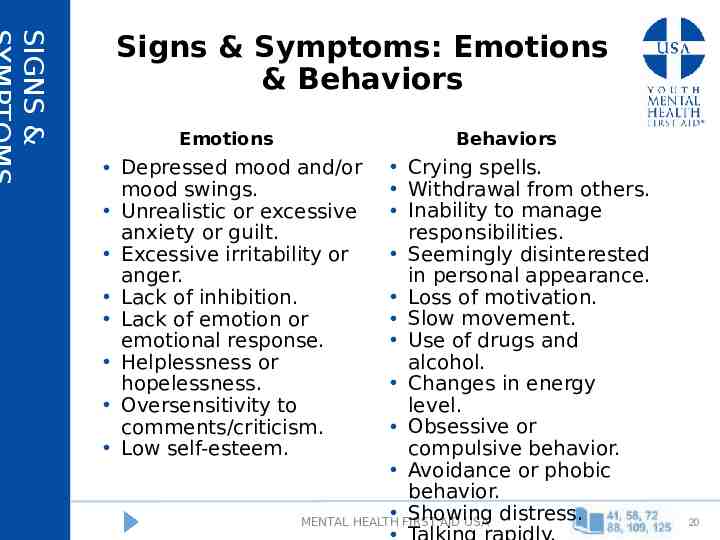
SIGNS & Signs & Symptoms: Emotions & Behaviors Emotions Behaviors Crying spells. Withdrawal from others. Inability to manage responsibilities. Seemingly disinterested in personal appearance. Loss of motivation. Slow movement. Use of drugs and alcohol. Changes in energy level. Obsessive or compulsive behavior. Avoidance or phobic behavior. Showing distress. MENTAL HEALTH FIRST AID USA Depressed mood and/or mood swings. Unrealistic or excessive anxiety or guilt. Excessive irritability or anger. Lack of inhibition. Lack of emotion or emotional response. Helplessness or hopelessness. Oversensitivity to comments/criticism. Low self-esteem. 20

SIGNS & Signs & Symptoms: Thoughts Frequent selfcriticism or selfblame. Pessimism . Difficulty making decisions, concentrating or remembering. Rigid thinking. Racing thoughts. Altered sense of self: tendency to believe others see one in a negative light. Delusions or hallucinations. Odd ideas. Lack of insight. Suspiciousness. Thoughts of death and suicide. MENTAL HEALTH FIRST AID USA 21

WARNING SIGNS Typical Stages vs. Warning Signs Examine the impact of change Is the youth struggling: In school? In social settings? In daily activities? Symptoms of a mental illness can often appear similar to typical development during this period. MENTAL HEALTH FIRST AID USA 22

WARNING SIGNS Typical Behaviors vs. Symptoms Examine the impact of change to see if the youth is struggling. Typical Adolescence Potential Warning Sign Withdrawing from family to Withdrawing from friends, spend more time with friends. family and social activity. Wanting more privacy. Becoming secretive; need for privacy seems to be hiding something. Moving from childhood likes to teen pursuits. Losing interest in favorite activities and not replacing with other pursuits. MENTAL HEALTH FIRST AID USA 23

RISK FACTORS Risk Factors Stressful events, abuse or trauma. Learned behavior. Chemical imbalance. Substance misuse and sensitivity. Seasonal changes. Previous episode of mental illness or presence of another mental illness. Ongoing stress and anxiety. Medical conditions and hormonal changes. Side effects of medication. Illness that is life threatening, chronic, or associated with pain. Brain injury. MENTAL HEALTH FIRST AID USA 24

PROTECTIVE Protective Factors Healthy practices. High self-esteem. Good problem solving skills. Feeling of control in their own life . Spirituality. Avoiding alcohol, tobacco and other drugs . Consistent home/family routine. Parental/familial support. Monitoring of youth’s activities. Regular school attendance and academic performance. Having a good social support system. Economic security. Availability of constructive recreation. Community bonding. Feeling close to at least one adult. MENTAL HEALTH FIRST AID USA 25

THE ACTION PLAN Mental Health First Aid The Action Plan Assess for risk of suicide or harm. Listen nonjudgmentally. Give reassurance and information. Encourage appropriate professional help. Encourage self-help and other support strategies. MENTAL HEALTH FIRST AID USA 26

REACHING OUT Considerations When Reaching Out Role/relationship you have to youth. Ethical Guidelines. Legal Requirements. Professional Restrictions. Role of family. Young person’s right to privacy. Your ability to help. MENTAL HEALTH FIRST AID USA 27

ACTION PLAN: A Assess for Risk of Suicide or Harm Youth may be at risk for a variety of crisis situations: Suicide or suicidal thoughts. Non-suicidal self-injury/other personal safety issues. Medical emergencies. Extreme distress. Aggression. MENTAL HEALTH FIRST AID USA 28

ACTION PLAN: A Assess for Risk of Suicide or Harm Factors that can increase risk for youth: Impulsivity. Lack of awareness of risk involved. Lack of awareness of time. Use of alcohol or other drugs. Influence of peer groups. MENTAL HEALTH FIRST AID USA 29

ACTION PLAN: L Listen Nonjudgmentally Using “I” statements, state nonjudgmentally what you have noticed. Ask questions, but don’t push. Realize it may be a relief for the young person to talk about how s/he feels. Remember it’s about the young person not you. His/her experiences are not the same as yours. His/her perspective is not the same as yours or necessarily of other youth in the family or peer group. His/her culture may not be the same as yours. S/he needs our empathy. S/he may use language that makes you uncomfortable. MENTAL HEALTH FIRST AID USA 30

ACTION PLAN: L Listen Nonjudgmentally How to Effectively Communicate with Youth: Be genuine and respectful. Be careful about using slang. Be comfortable with silence. Be in the present with them without comparing to your own youth. Be aware that the young person’s feelings are very real. Be accepting even though you may not agree. Be aware of your body language and facial expressions. Be positive with your feedback. Be helpful with language without telling them how they feel or “should” feel. MENTAL HEALTH FIRST AID USA 31

ACTION PLAN: G Give Reassurance and Information Do Do Not Have realistic Make promises you cannot keep. expectations. Give advice. Dismiss the problem or emotions. Offer consistent emotional support. Focus on “right” vs. “wrong.” Give the young person Provide practical help. Focus solely on weight, food, drugs, alcohol, injury or specific external factors unless there is an emergency. Provide information. Try to “fix” the problem yourself. hope. Acknowledge the limits of what you can do. Engage in communication that is: belittling, sarcastic, hostile or patronizing. MENTAL HEALTH FIRST AID USA 32

ACTION PLAN: G Information vs. Advice Reassuring Information Advice Breakups can be tough. It’s natural for you to be hurt and upset. I remember my first breakup, here’s what you need to do. I’m here for you if you want to You really need to talk to a talk. There are also people who counselor about that. are trained to help you work through these feelings. You are not alone. You’ll get over it. Just don’t worry about it so much. MENTAL HEALTH FIRST AID USA 33

ACTION PLAN: E Encourage Appropriate Professional Help Individuals with mental disorders are treatable with a variety of therapies and/or supports. Evidence-based practices are interventions for which there is consistent scientific evidence showing that they improve individual outcomes. MENTAL HEALTH FIRST AID USA 34

ACTION PLAN: E Encourage Appropriate Professional Help Types of professionals: Doctors (pediatricians/primary care physicians/psychiatrists). Nurse practitioners/physician assistants. Mental health professionals (e.g. social workers, licensed counselors). Drug and alcohol specialists. School counselors. Nutrition experts. Certified peer specialists. Other professionals. MENTAL HEALTH FIRST AID USA 35

ACTION PLAN: E Encourage Appropriate Professional Help Types of professional help: Individual, family and/or group therapy. Alcohol/drug treatment, withdrawal management. Problem-solving, decision making, or social skills training. Academic counseling. Dietary management. Medication. MENTAL HEALTH FIRST AID USA 36

MEDICATION Medication for Youth Medication is rarely the sole treatment for youth with mental health problems. Medication combined with therapy or other treatment may be more effective than either treatment alone. Discussions regarding the use of medication with the youth should include the family and the healthcare provider. Trials often needed to identify the best medication and dose. Monitoring medication use is critical in youth. Knowledge on the use of medication in youth is limited. MENTAL HEALTH FIRST AID USA 37

ACTION PLAN What if the Person or Family Doesn’t Want Help? Find out why Engage professional intervention if an emergency Address fear of embarrassment or shame Help find solutions to concerns about paying for care or finding a provider Identify resources School Personnel Social Services Hotlines Behavioral Health Providers School Services Call 911 Faith Leaders Peer/Parent Support Groups Organizations and Websites MENTAL HEALTH FIRST AID USA 38

ACTION PLAN: E Encourage Self-Help and Other Support Strategies Identify others who may be helpful. Explore activities that might help manage symptoms. Find strategies that interest the young person. Discuss self-help strategies with a health professional. Engage the family as well as the young person. MENTAL HEALTH FIRST AID USA 39

ACTION PLAN: E Encourage Self-Help and Other Support Strategies Promising self-help strategies: Are interesting to the young person. Promote a sense of satisfaction. Enhance social connectedness. Should be safe. Note: many natural therapies have not been studied thoroughly in youth and may not be suitable for children or young adults. MENTAL HEALTH FIRST AID USA 40

HAVING THE CONVERSATION Let’s Have the Conversation Ask how the youth is feeling. Describe what you’ve seen. Express any concerns. Don’t initially focus on changing the person’s behavior, perspective or symptom. Use “I” statements that are not accusatory. MENTAL HEALTH FIRST AID USA 41

ACTION PLAN: A Assess for Risk of Suicide or Harm Emergency medical services should be sought if the person has any of the following symptoms: Disordered thinking or not making any reasonable sense (may experience delusions or hallucinations). Disorientation–not knowing what day it is, where they are or who they are. Unintentionally throwing up several times a day. Fainting. Collapses or is too weak to walk. Painful muscle spasms. MENTAL HEALTH FIRST AID USA 42

ACTION PLAN: A Assess for Risk of Suicide or Harm Seek emergency help if (cont.): Chest pain or difficulty breathing. Blood in their bowel movements, urine or vomit. A body mass index (BMI) of less than 16. An irregular or very low heartbeat (less than 50 beats per minute). Cold or clammy skin indicating a low body temperature (less than 95 degrees Fahrenheit). MENTAL HEALTH FIRST AID USA 43

ACTION PLAN: A Assess for Risk of Suicide or Harm Important signs that a young person may be suicidal: Threatening to hurt or kill himself/herself. Seeking access to pills, weapons or other means. Talking or writing about death, dying or suicide. Expressing hopelessness, no reason for living or having no sense of purpose in life. Having rage, anger or seeking revenge. Acting recklessly or engaging in risky activities, seemingly without thinking. Feeling trapped. MENTAL HEALTH FIRST AID USA 44

ACTION PLAN: A Assess for Risk of Suicide or Harm Important signs that a young person may be suicidal (cont.): Increasing alcohol or drug use. Withdrawing from friends, family or society. Having a dramatic change in mood. Sleeping all the time or being unable to sleep. Being anxious or agitated. Giving away prized possessions. MENTAL HEALTH FIRST AID USA 45

ACTION PLAN: A How to Talk With Someone who is Suicidal Discuss your observations with the young person. Appear confident, as this can be reassuring. Tell the person that thoughts of suicide are common and do not have to be acted on. Realize the youth may be reluctant to involve family or professional help. Try to involve the person in the decision making about what should be done, who should be told and how to seek professional help. If the person has a weapon or is behaving aggressively, call 911 immediately. MENTAL HEALTH FIRST AID USA 46

ACTION PLAN: A Assess for Risk of Suicide or Harm Ask the Question: “Are you thinking about killing yourself?” If the answer is, “Yes,” then Ask if the person has a plan: “Have you decided how you would kill yourself?” “Have you decided when you would do it?” “Have you taken any steps to secure the things you would need?” Higher level of planning means higher risk. Lower level of planning does not mean there is no risk. MENTAL HEALTH FIRST AID USA 47

ACTION PLAN: A Assess for Risk of Suicide or Harm Additional Questions to Ask: “Have you been using alcohol or other drugs?” “Have you made a suicide attempt in the past?” “Have you had family, friends or heroes die by suicide?” MENTAL HEALTH FIRST AID USA 48

ACTION PLAN: A Assess for Risk of Suicide or Harm If there is a risk of suicide, take immediate action to keep the young person safe: Do not leave him/her alone. Ensure he/she has a safety contact at all times. Discuss past supporters and see if they’re still available. Do not use guilt or threats to prevent suicide. Implement the other steps of the ALGEE Action Plan. Seek additional support if needed, including 911. MENTAL HEALTH FIRST AID USA 49

ACTION PLAN: A Assess for Risk of Suicide or Harm Inform the crisis team if the young person has: Access to a gun, medications, or other means of suicide. Stopped taking prescribed medicines. Stopped seeing a mental or behavioral health provider or physician. Written a suicide note. Given possessions away. Been in or is currently in an abusive relationship. Recently suffered a loss or other traumatic event. An upcoming anniversary of a loss. Started using alcohol or drugs. Recovered well from a previous suicidal crisis following a certain type of intervention. MENTAL HEALTH FIRST AID USA 50

ACTION PLAN: A Try to De-escalate the Situation Speak slowly and confidently with a gentle, caring tone of voice. Do not argue or challenge the person. Do not threaten. Do not raise your voice or talk too fast. Use positive words instead of negative words. Stay calm and avoid nervous behavior. Do not restrict the person’s movement. Try to be aware of what may increase the person’s fear and aggression. Take a break from the conversation. MENTAL HEALTH FIRST AID USA 51

REACHING OUT Key Considerations for Reaching Out Do: Understand the symptoms for what they are. Empathize with how the person is feeling about his or her beliefs and/or experiences. Do not: Confront the person. Criticize or blame. Take delusional comments personally. Use sarcasm. Use patronizing statements. State any judgments about the content of the beliefs and/or experiences. MENTAL HEALTH FIRST AID USA 52

SELF-CARE Taking Care of Yourself as a First Aider Have I decided what I will do for selfcare? Who can I debrief with now? If I feel upset or distressed later, who can I call? If I share with others, how do I ensure the confidentiality of the young person? Do I or my family need a break? MENTAL HEALTH FIRST AID USA 53

YOUTH MENTAL HEALTH FIRST Youth Mental Health First Aid is the help offered to a young person experiencing a mental health challenge, mental disorder, or a mental health crisis. The first aid is given until appropriate help is received or until the crisis resolves. MENTAL HEALTH FIRST AID USA 54

MENTAL HEALTH FIRST Mental Health First Aid USA MENTAL HEALTH FIRST AID USA 55