The Leader’s Role in Quality Improvement Education: A Framework for
37 Slides595.50 KB
The Leader's Role in Quality Improvement Education: A Framework for Change Insert Facilitators: Name, Title Insert Sponsoring Healthcare Institution Insert Date, Location
Welcome! Pre-session Assessment Please take a moment to complete the short pre-session assessment before we begin. Thank you
Changing Paradigms Increased diversity Less predictability Relationships and coalitions are critical Systems are unstable/ambiguous Small differences often produce large consequences
How does change feel? Exercise – patterns of behavioral change
Learning Objectives: Identify leadership behaviors to enhance team performance Discuss how leadership behaviors affect change and manage conflict Recognize the affect of human factors in quality improvement Examine educational leadership strategies in a QI case study when leading the change process Promote reflective practices for selfimprovement in leading the education team
WORKSHEET #1 Individual Activity List characteristics of effective leaders Identify at least two barriers in leading healthcare teams How might you overcome these barriers?
Activity Debriefing List characteristics of effective leaders What are at least two barriers to leading quality improvement for multidisciplinary health care teams? How might we overcome these barriers?
Team Characteristics What is a team? What are key attributes of effective teams? What are key aspects of ineffective teams?
Key Aspects of Team Leadership There is no ‘one best’ style Understand yourself first Value others’ perspectives and differences Strive for shared leadership Build and sustain trust Demonstrate courage Reflect and improve
Leadership Provides direction and influences individuals or teams to achieve goals; the capacity to lead Process to create an organization that aligns people with an inspiring vision that overcomes barriers to change
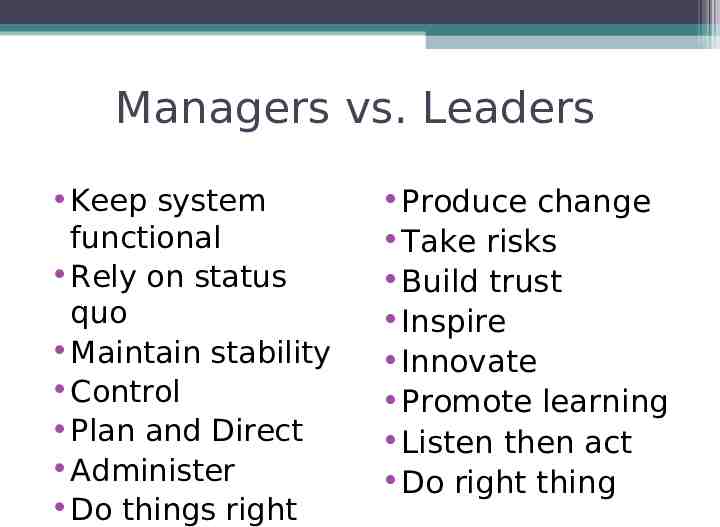
Managers vs. Leaders Keep system functional Rely on status quo Maintain stability Control Plan and Direct Administer Do things right Produce change Take risks Build trust Inspire Innovate Promote learning Listen then act Do right thing
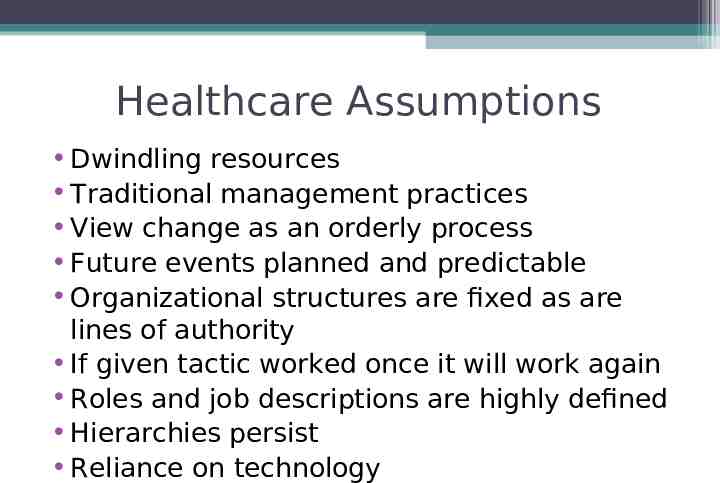
Healthcare Assumptions Dwindling resources Traditional management practices View change as an orderly process Future events planned and predictable Organizational structures are fixed as are lines of authority If given tactic worked once it will work again Roles and job descriptions are highly defined Hierarchies persist Reliance on technology
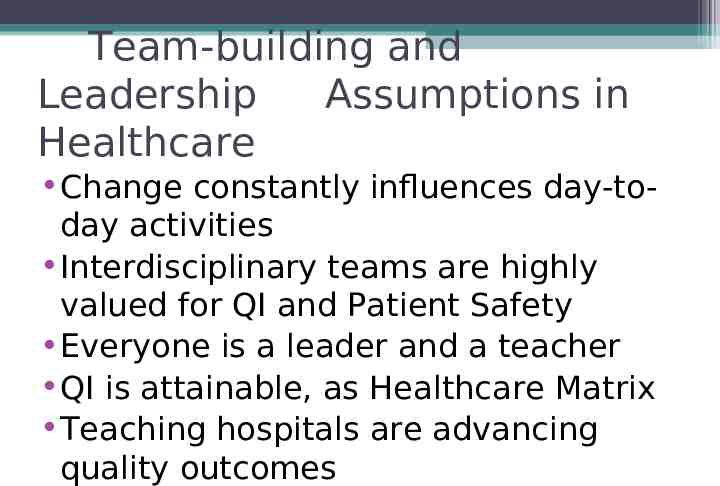
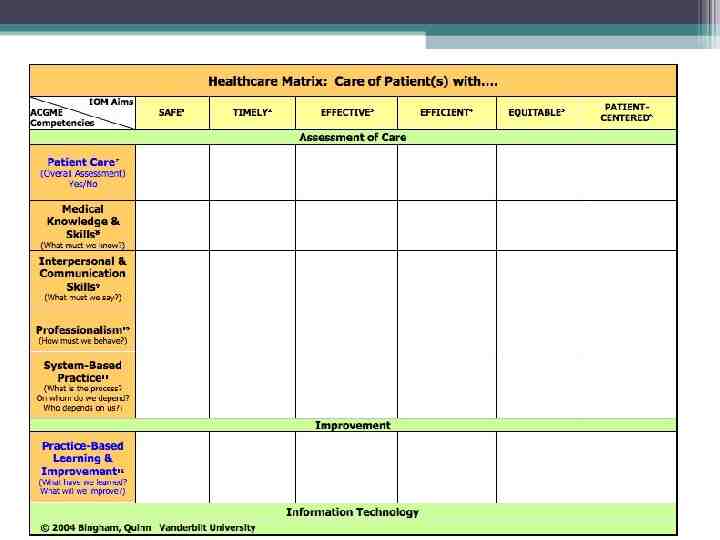
Team-building and Leadership Assumptions in Healthcare Change constantly influences day-today activities Interdisciplinary teams are highly valued for QI and Patient Safety Everyone is a leader and a teacher QI is attainable, as Healthcare Matrix Teaching hospitals are advancing quality outcomes
Model for Improvement IHI Set Aims– What will learners achieve from the learning opportunity? Establish Measures– How instructional goal will be accomplished or measured? How do we know when we get there? Select Changes – What changes in learning strategies will result in improvement? www.ihi.org
Human Factors Influence QI and Change Management Human strengths/limitations for team effectiveness: Predisposing factors – biologic, psychosocial Impact on decision-making – cognition; culture; judgment, hierarchy Impact on execution and performanceability; skills; motivation; self-efficacy
People and organizations change when they: Have a compelling reason Expect personal benefits (WIIFM) Have ownership in the change process Recognize their leaders as role-models with serious conviction for initiating and sustaining change Recognize consequences of errors in patient care
Organizational change fostered by leaders who: Articulate a clear and inspiring vision Challenge the process and embrace change Enable and value each individual Align people and purpose Build enduring teams and coalitions Model effective communication Foster trust
Kotter’s Change Model Sense of urgency Form a powerful coalition Create a vision for change Communicate the vision Empower action – remove obstacles Create short-term, quick wins Build on change momentum Anchor new approaches in the culture
Worksheet #2 Case Study You have twenty-five minutes to review this Quality Improvement case and respond to the prompts. Make notes and share with your small group. Sample case study slides (blood specimen mislabeling) attached. Apply Kotter’s leadership stages (e.g., urgency, coalitions, vision/strategy, communicate change, empower, short-term wins and create change)
Case Study Debriefing How did the education leader create: Sense of urgency Guiding coalition Create a vision for change and communicate Empower others Create short-term, quick wins Build on change momentum Institutionalize changes in the culture?
Educational Professionalism Honesty and integrity Compassion and accountability Respect for others Patient confidentiality Know ‘the rules’ and align our moral compass AVOID: abuse of power (coercive, authoritative), greed, deception, impairment and conflict of interest/non-disclosure
Summary Points Reflect on your daily leadership successes and short-comings for self-improvement. What are important lessons learned and what to change next time? Everyone can be a leader and sustain change Know your leadership strengths and limitations Plan for your success as an education leader to improve quality of patient care! Post-session assessment – Please complete What was most beneficial about the session? What could be improved upon?
Comments and Questions References: Leading for Change1996; Kotter, J. H C Manage Rev 1997; 22 McDaniel, R. Acad Med 1999; 74 (Bland, et al) Jrnl Quality Pt Safety 2005; 31 (Bingham, et al) J Health Organ Manag 2005;19 Ovretveit, J. Adv Hlth Sci Ed 2006; 11 (Bakken, et al) Acad Med 2007; 82 (Loeser, O’Sullivan , Irby) Acad Med 2012; 87 (Neeman, et al) Am J Med 2012; 125 (Van Hoof, et al) Acad Med 2012; 87 (Lingard, et al) Agency for Healthcare Research and Quality. (2010). http://grants.nih.gov/grants/guide/rfa-files/RFA-HS-11-002.ht ml . (p. 5).
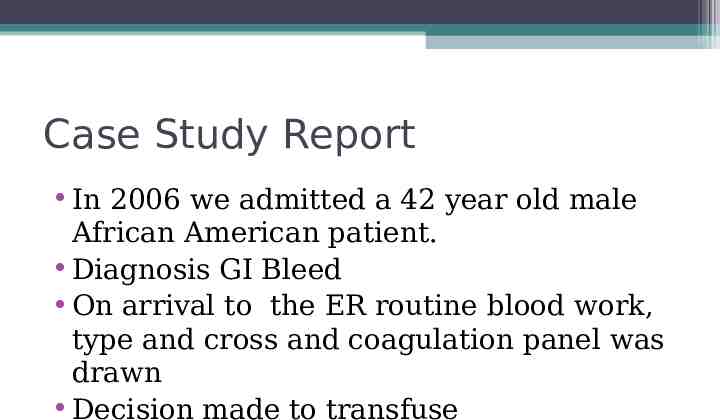
Optional: Sample Case Study Description Use these slides to review essential details in the Blood Specimen Mislabeling, if you so desire. The level of detail and processes may be useful for selected target audiences. This is optional.
Case Discussion 1. A type and cross was sent form the ER trama room 2. Resulted in type A positive(A ) with negative antibodies 3. There also was no blood bank history for this patient and a unit of compatible blood was released and started at 17:30 completed @ 18:45.
Case Discussion @1830, 1 milligram of Dilaudid is given for rigors and abdominal pain. The transfusion was still infusing @1850, he becomes hypotensive and is treated with a bolus of normal saline STAT CBC is sent to lab @1956
Case Discussion @2020 the MICU is notified the repeat CBC has resulted with Red cell indices markedly different from previously values In addition the chemistry specimen was hemolyzed.
Case Discussion The patient1. 2. 3. 4. 5. Is bleeding from the IV site Coagulation is now grossly abnormal with an INR53.9 Fibrinogen -200mg/dL and his D-Dimer is 1262ng/mL Platelets from 73 to 43 K/uL. He is transfused by a blood pressure cuff another unit of blood and then four more between 2050 and 2140 Disseminated intravascular coagulation (DIC) is considered , blood transfusion reaction is considered –Hematology consult called THE BLOOD BANK WAS NOT NOTIFIED
Investigation Improper patient identification by the health care provider Improper label check on pretransfusion specimen-lab staff Possible failure to identify a transfusion reaction Failure to alert the blood bank when the reaction was suspected
Investigation Starting at the beginning The patient’s blood tube had two labels on the type and cross. Two different names. One label was the patient who had the reaction. (Patient-1) the other to patient 2 who had a blood transfusion history. Patient 1 was O patient 2 was A
Investigation In 2006, there were no labels printed until after the patient had been registered. Labels could be prolonged-Patients were treated pre registration.
Investigation Labels for type and screen were hand written signed by the drawer and when the labels became available they were placed on the tube, over the hand written label. The tube had to be signed by the drawer verifying that this was the correct tube for the correct patient with the correct label.
Investigation The Lab Tech also had to go through the same process and did not NO VERIFICATION Failure to follow procedure in performing a second label check of pretransfusion specimen when the reaction was called to the blood bank
Investigation Standard of Practice – when an untoward event occurs in association with a transfusion, the transfusion should be STOPPED and the BLOOD BANK NOTIFIED IMMEDIATELY This was not followed
Policy The Safe Blood Labeling policy has been in effect and all staff education needed to be completed by Oct 15, 2007. The following unacceptable Blood Bank specimen(s) was/were received in the Laboratory. An investigation initiated into the circumstance that may have led to the mislabeled specimen(s) and include training documentation that demonstrates the staff were trained. Your finding may help to identify the root-cause and process failures.
Case Study Report In 2006 we admitted a 42 year old male African American patient. Diagnosis GI Bleed On arrival to the ER routine blood work, type and cross and coagulation panel was drawn Decision made to transfuse