The Qualified Clinical Data Registry Overview of the Problem
41 Slides1.73 MB

The Qualified Clinical Data Registry Overview of the Problem Richard P. Dutton, M.D., M.B.A. aqihq.org
“Pay for Performance” Federal programs to promote quality over quantity in the delivery of healthcare. Based on measuring outcomes o Public reporting o Payment incentives and penalties Hospitals Physicians 2014 ANESTHESIA QUALITY INSTITUTE 2
Key Points Pay for Performance programs are evolving over time What was true last year will not be true next year Complexity is increasing ASA (and all physician societies) must seize opportunities to guide this evolution ASA has worked hard to keep up 2014 ANESTHESIA QUALITY INSTITUTE 3
The Evolution of P4P From Process Measures To Outcomes 2014 ANESTHESIA QUALITY INSTITUTE 4
The Evolution of P4P From Big hospitals To Small hospitals, surgery centers, clinics and offices 2014 ANESTHESIA QUALITY INSTITUTE 5
The Evolution of P4P From Inpatients To All patients 2014 ANESTHESIA QUALITY INSTITUTE 6
The Evolution of P4P From Medicare only To Medicare Advantage, Medicaid, and all payers 2014 ANESTHESIA QUALITY INSTITUTE 7
The Evolution of P4P From Incentives To Penalties 2014 ANESTHESIA QUALITY INSTITUTE 8
The Evolution of P4P From Clinical Safety Focused To Patient Centered 2014 ANESTHESIA QUALITY INSTITUTE 9
The Evolution of P4P From Individuals To Teams 2014 ANESTHESIA QUALITY INSTITUTE 10
The Evolution of P4P From Paper To Electrons 2014 ANESTHESIA QUALITY INSTITUTE 11
The Evolution of P4P From Individual reporting To Group and registry reporting 2014 ANESTHESIA QUALITY INSTITUTE 12
The Evolution of P4P From A demonstration project To The way we do business 2014 ANESTHESIA QUALITY INSTITUTE 13
Physician Quality Reporting System (PQRS) Defining PQRS o “Paid under or based on the Physician Fee Schedule” o Eligible Professionals (EPs) Common Measures Reported by Anesthesiologists o #30 (NQF #0269): Timing of Prophylactic Antibiotic o #44 (NQF #0236): Preoperative Beta-Blocker in Patients with Isolated CABG Surgery o #76 (NQF #0464): Central Venous Catheter (CVC) Insertion Protocol o #193 (NQF #0454): Perioperative Temperature Management Anesthesiology PQRS Participation Rate (2012) 2014 ANESTHESIA QUALITY INSTITUTE 14
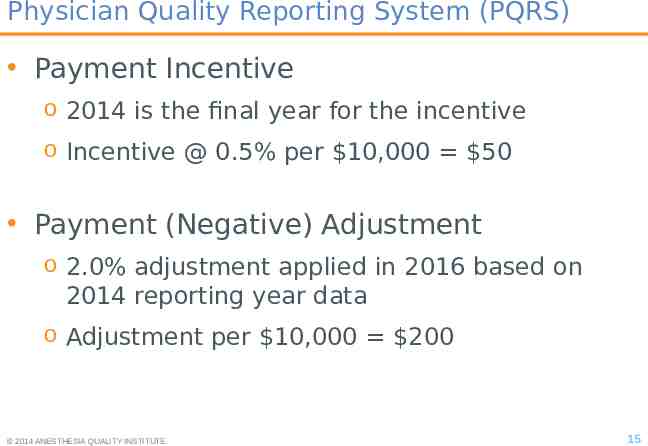
Physician Quality Reporting System (PQRS) Payment Incentive o 2014 is the final year for the incentive o Incentive @ 0.5% per 10,000 50 Payment (Negative) Adjustment o 2.0% adjustment applied in 2016 based on 2014 reporting year data o Adjustment per 10,000 200 2014 ANESTHESIA QUALITY INSTITUTE 15
Satisfactorily Report Avoid the Payment Adjustment Reporting Options o o o o Claims Qualified Clinical Data Registry (QCDR) “Traditional” Qualified Registry Other Reporting Options Alignment of Measure Reporting Requirements o Nine (9) quality measures o Three (3) National Quality Strategy (NQS) domains 2014 ANESTHESIA QUALITY INSTITUTE 16
Satisfactorily Report Avoid the Payment Adjustment Satisfactorily Reporting – Claims (2014): o EPs must report 9 PQRS measures covering 3 NQS domains to qualify for an incentive payment for 50% of Medicare Part B patients for whom the measure applies If fewer than 9 measures, then EP is subject to the Measure-Applicability Validation (MAV) process o EPs must report 3 measures in order to avoid the payment adjustment for 2016 Subject to MAV process Claims-Based Reporting Challenges (Beyond 2014): o PQRS Measures for Consideration o PQRS #30, PQRS #109 o Narrowing of Reporting Options 2014 ANESTHESIA QUALITY INSTITUTE 17
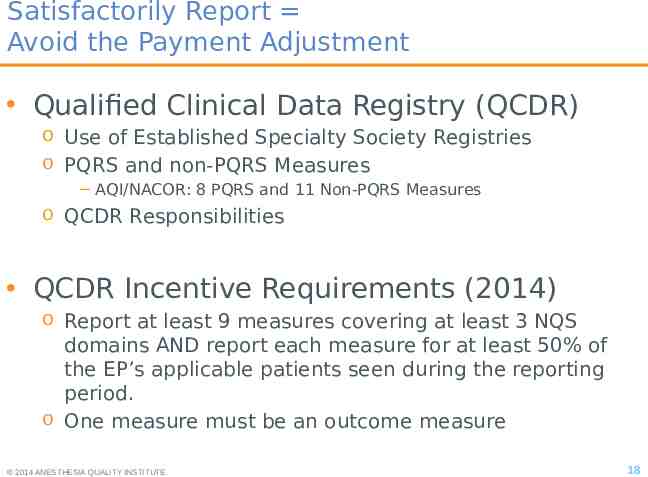
Satisfactorily Report Avoid the Payment Adjustment Qualified Clinical Data Registry (QCDR) o Use of Established Specialty Society Registries o PQRS and non-PQRS Measures AQI/NACOR: 8 PQRS and 11 Non-PQRS Measures o QCDR Responsibilities QCDR Incentive Requirements (2014) o Report at least 9 measures covering at least 3 NQS domains AND report each measure for at least 50% of the EP’s applicable patients seen during the reporting period. o One measure must be an outcome measure 2014 ANESTHESIA QUALITY INSTITUTE 18
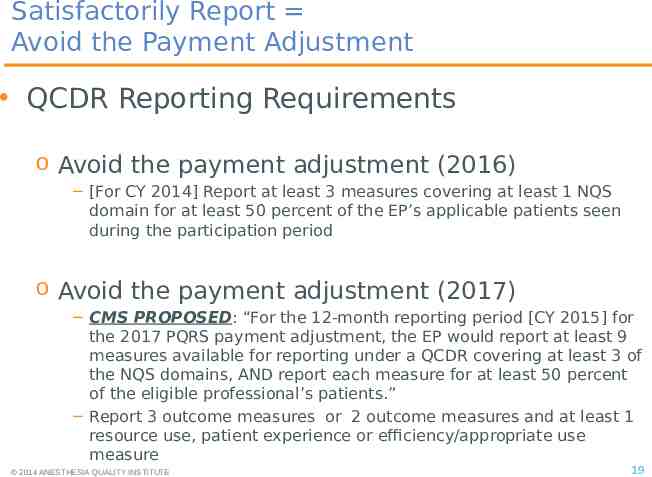
Satisfactorily Report Avoid the Payment Adjustment QCDR Reporting Requirements o Avoid the payment adjustment (2016) [For CY 2014] Report at least 3 measures covering at least 1 NQS domain for at least 50 percent of the EP’s applicable patients seen during the participation period o Avoid the payment adjustment (2017) CMS PROPOSED: “For the 12-month reporting period [CY 2015] for the 2017 PQRS payment adjustment, the EP would report at least 9 measures available for reporting under a QCDR covering at least 3 of the NQS domains, AND report each measure for at least 50 percent of the eligible professional’s patients.” Report 3 outcome measures or 2 outcome measures and at least 1 resource use, patient experience or efficiency/appropriate use measure 2014 ANESTHESIA QUALITY INSTITUTE 19
Physician Quality Reporting System Preparing for the Future Learn and Understand PQRS o CMS PQRS Website (www.cms.gov/pqrs) o CMS QualityNet Help Desk (866-288-8912 or [email protected]) Member Resources o Quality and Regulatory Affairs ([email protected]) o Anesthesia Quality Institute ( http://www.aqihq.org/qcdr) Prepare for PQRS Reporting in 2015 2014 ANESTHESIA QUALITY INSTITUTE 20
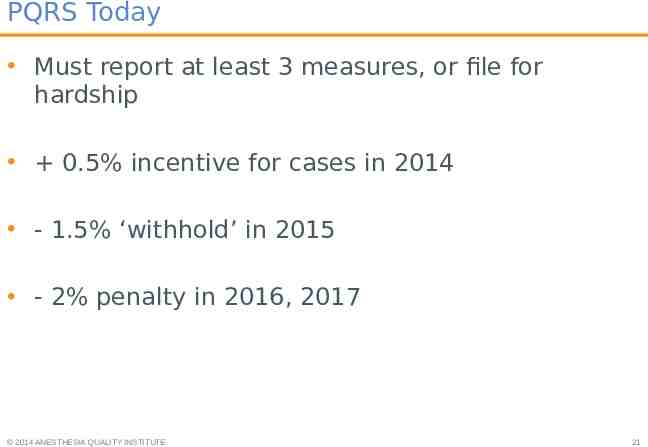
PQRS Today Must report at least 3 measures, or file for hardship 0.5% incentive for cases in 2014 - 1.5% ‘withhold’ in 2015 - 2% penalty in 2016, 2017 2014 ANESTHESIA QUALITY INSTITUTE 21
PQRS Participation 54% of eligible anesthesiologists submitted data in 2011 (61% in 2013) 84% of this group received an incentive Average 400 per provider (max: 14,000) 2014 ANESTHESIA QUALITY INSTITUTE 22
Value Based Modifier (VM) Also based on the PQRS measure set Requires 9 measures o 3 domains o at least 1 outcome o or hardship exemption 2% penalty in 2014 for not participating; escalates in future years Losers pay for winners! 2014 ANESTHESIA QUALITY INSTITUTE 23
Domains Patient safety Patient and caregiver experience Care coordination Clinical care Population health Efficiency and cost reduction 2014 ANESTHESIA QUALITY INSTITUTE 24
The QCDR Qualified Clinical Data Registry New in 2014 A reporting mechanism for registry participants Similar to the group reporting option for PQRS / VM Can use PQRS measures Can use non-PQRS, specialty specific measures 2014 ANESTHESIA QUALITY INSTITUTE 25
More about the QCDR New method for satisfactorily reporting PQRS a CMS-approved entity that collects clinical data for patient/disease tracking for quality improvement QCDRs are typically specialty society registries like AQI’s National Anesthesia Clinical Outcomes Registry (NACOR) Measure data across multiple payers, not limited to Medicare beneficiaries Allowed to report “non-PQRS” and PQRS measures for successful PQRS reporting 2014 ANESTHESIA QUALITY INSTITUTE 26
Why the QCDR is a big deal Measure definition by the specialty, for the specialty Data collection and scoring moves from CMS to the registry “One stop shop” for all requirements Public reporting by the society 2014 ANESTHESIA QUALITY INSTITUTE 27
Benefits of using a QCDR Greater potential to meet the 9/3 reporting requirements; increasing strictness with other reporting mechanisms. Support better outcome under the Value Modifier program; using a QCDR, quality scores: Are easier to monitor and improve throughout the reporting year Could be higher because of the frequent feedback/monitoring Greater choice of measures to report potential higher quality scores. 2014 ANESTHESIA QUALITY INSTITUTE 28
The Anesthesiology Perspective The National Anesthesia Clinical Data Registry is certified as a QCDR Available measures for perioperative care increased from 4-8 in PQRS to 19 4 domains, multiple outcome measures 2014 ANESTHESIA QUALITY INSTITUTE 29
PQRS reporting through AQI AQI has partnered with ASA to offer a mechanism for anesthesia EP’s to satisfactorily report for PQRS New offering - ASA QCDR ASA will signup the groups/participants o Free to ASA members, Fee for non-members AQI will collect and analyze the data, and report the data to CMS 2014 ANESTHESIA QUALITY INSTITUTE 30
Where Did New Anesthesia Measures Come From? Existing in PQRS o Solves the stewardship problem Existing in NQF New measures mostly developed by ASA’s Committee on Performance and Outcome Measures (CPOM) Developed, but never selected Developed, but never submitted Subspecialty possibilities Aspirational measures 2014 ANESTHESIA QUALITY INSTITUTE 31
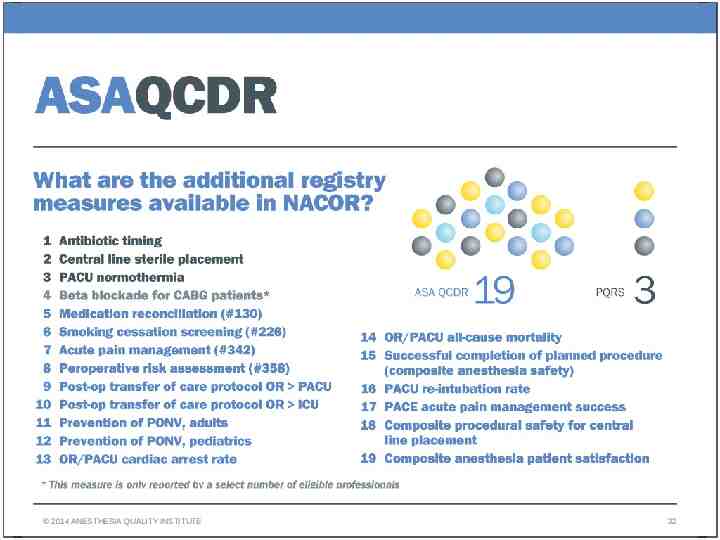
2014 ANESTHESIA QUALITY INSTITUTE 32
AQI as a QCDR The Centers for Medicare and Medicaid Services (CMS) introduced the Qualified Clinical Data Registry (QCDR) as a reporting option in 2014. 2014 QCDR reporting: o EPs must report on 9 measures including 1 outcome across 3 NQS domains. o EPs that successfully report are eligible for a payment incentive. 2015 Medicare Physician Fee Schedule Proposed Rule: o To avoid future payment adjustments an EP will have to report on 9 measures including 3 outcomes across 3 NQS domains. The addition of QCDR reporting allows specialty societies to develop measures that reflect profession-specific priorities. 2014 ANESTHESIA QUALITY INSTITUTE 33
QCDR reporting through AQI AQI only reports on measures for Anesthesia o 8 existing PQRS measures o 11 non-PQRS QCDR measures No Measure Groups, GRPO, or eRx Working with ASA on additional measures for 2015 Reports for Eligible Anesthesia Providers: MD, DO, and CRNA 2014 ANESTHESIA QUALITY INSTITUTE 34
Performance Reporting through the QCDR 2015 Anesthesia QCDR reporting is a product of ASA o ASA sells it o AQI delivers the goods Groups must be participating in AQI Free to ASA members who are participating in NACOR Additional charge for non-ASA members (i.e CRNAs) 2014 ANESTHESIA QUALITY INSTITUTE 35
QCDR Reporting Requirements. You Must: Be a NACOR participant. If you are not already participating in NACOR steps include: o Completion of a Business Associate Agreement with the AQI o Payment of fees (AQI participation is free to ASA members and any EPs working with them in the care team model.) o Completion of the AQI practice profile o Transmission of electronic data to the registry beginning in January 2015 Self-nomination with AQI for QCDR reporting in early 2015 Work with AQI to ensure proper data is being sent Approve the final transmission of EP performance data to CMS 2014 ANESTHESIA QUALITY INSTITUTE 36
What to do next – 2 of 3 If your group already sends data to AQI Thank you for your support Go to next step Or Else Contact AQI to become an AQI Participant Participation is required for AQI to report on your behalf 2014 ANESTHESIA QUALITY INSTITUTE 37
What to do next – 3 of 3 Does your group collect clinical outcomes intraoperatively and in the PACU? Yes - you are well on your way to satisfactorily report for PQRS via QCDR No – work to get a process in place to collect the appropriate outcomes 2014 ANESTHESIA QUALITY INSTITUTE 38

Upcoming Webinar 2014 ANESTHESIA QUALITY INSTITUTE 39
Additional Resources AQI website: http://aqihq.org/ AQI PQRS: http://aqihq.org/PQRSOverview.aspx AQI QCDR – http://aqihq.org/qcdr ASA QCDR: http://asahq.org/qcdr 2014 ANESTHESIA QUALITY INSTITUTE 40
Questions? www.aqihq.org or [email protected] @ASALifeline Fb.me/AmericanSocietyofAnesthesiologists g