The national flu immunisation programme 2020 to 2021 Training for
79 Slides2.01 MB

The national flu immunisation programme 2020 to 2021 Training for healthcare practitioners

Flu vaccination programme and COVID-19 The flu vaccination programme for the 2020/21 flu season has been extended, with more groups eligible to receive flu vaccine than in previous years. As COVID-19 is likely to be co-circulating with flu, protecting those at high risk of flu, who are also those most vulnerable to hospitalisation as a result of COVID-19, is vitally important. Control measures to prevent the spread of the SARs-CoV-2 virus such as shielding and social distancing will mean that delivering the flu vaccine this year will be more challenging as flu vaccines are likely to be delivered in a very different way than in previous years and a range of different ways of delivering the programme this year should be considered. Flu immunisers are also likely to need to wear personal protective equipment (PPE) in keeping with the advice that is current at the time of delivering the flu vaccine. This slideset will focus on the childhood flu programme recommendations for 2020/21. Those involved in delivering this year’s flu vaccine programme should ensure that they are aware of the specific guidance that they should follow in order to safely and effectively deliver flu vaccines during the ongoing COVID-19 pandemic. This includes, but is not limited to, guidance on PPE and infection control measures. 2 The national flu immunisation programme 2020/21

Essential further reading Please ensure that you read the national flu immunisation programme 2020/21 letters available on the PHE Annual flu programme webpage ( www.gov.uk/government/collections/a nnual-flu-programme ) In addition to providing key information about this year’s flu programme, these letters also contain links to the relevant coronavirus-related guidance. It is recommended that you regularly check this webpage during the flu vaccination period as any further information that becomes available about the flu vaccine programme will be published there. 3 The national flu immunisation programme 2020/21

Key messages flu immunisation is one of the most effective interventions we can provide to reduce harm from flu and pressures on health and social care services during the winter it is important to increase flu vaccine uptake in clinical risk groups because of increased risk of death and serious illness if people in these groups catch flu for a number of years, only around half of patients aged six months to under 65 years in clinical risk groups have been vaccinated influenza during pregnancy may be associated with perinatal mortality, prematurity, smaller neonatal size, lower birth weight and increased risk of complications for mother vaccination of health and social care workers protects them and reduces risk of spreading flu to their patients, service users, colleagues and family members by preventing flu infection through vaccination, secondary bacterial infections such as pneumonia are prevented. This reduces the need for antibiotics and helps prevent antibiotic resistance 4 The national flu immunisation programme 2020/21

Aims of resource The purpose of this training resource is to: 5 develop the knowledge base of healthcare practitioners regarding the 2020/21 seasonal flu vaccination programme support healthcare practitioners involved in discussing flu vaccination with those eligible by providing evidence based information promote high uptake of flu vaccination in those eligible by increasing the knowledge of those involved in delivering the vaccination programme provide information on the administration of flu vaccines The national flu immunisation programme 2020/21

Learning outcomes On completion of this resource, healthcare practitioners will be able to: describe the cause of flu understand how flu is transmitted and the possible effects of flu understand the evidence base for the administration of flu vaccination to those aged 65 years and over and those in clinical risk groups explain which vaccines will be used and the precautions and contraindications to the administration of flu vaccines explain the sequence of steps in flu vaccine administration explain the possible side effects from flu vaccines understand the importance of their role in promoting and providing evidence based information about flu vaccination to patients identify sources of additional information 6 The national flu immunisation programme 2020/21

Flu overview flu is an acute viral infection of the respiratory tract (nose, mouth, throat, bronchial tubes and lungs) it is a highly infectious illness which spreads rapidly in communities even people with mild or no symptoms can infect others most cases in the UK occur during an 8 to 10 week period during the winter The national flu immunisation programme 2014/15 7 The national flu immunisation programme 2020/21

Influenza viruses A viruses cause outbreaks most years and are the usual cause of epidemics and pandemics live and multiply in many different animals and may spread between them birds, particularly wildfowl, are the main animal reservoir B viruses tend to cause less severe disease and smaller outbreaks predominantly found in humans burden of disease mostly in children 8 The national flu immunisation programme 2020/21

Flu A virus Genetic material (RNA) in the centre Two surface antigens: Haemagglutinin (H) (blue) Neuraminidase (N) (red) There are 18 different types of H and 11 different types of N The role of haemagglutinin is to bind to the cells of the infected person The role of neuraminidase is to release the virus from the cell surface 9 The national flu immunisation programme 2020/21

Genetic changes in the flu virus – what this means Changes in the surface antigens (H and N) result in the flu virus constantly changing antigenic drift: minor changes (natural mutations) in the genes of flu viruses that occur gradually over time antigenic shift: when two or more different strains combine. This abrupt major change results in a new subtype. Immunity from previous flu infections/vaccinations may not protect against the new subtype, potentially leading to a widespread epidemic or pandemic Because of the changing nature of flu viruses, WHO monitors their epidemiology throughout the world. Each year WHO makes recommendations about the strains of influenza A and B which are predicted to be circulating in the forthcoming winter. These strains are then included in the flu vaccine developed each year 10 The national flu immunisation programme 2020/21

Flu vaccine effectiveness 11 efficacy varies from one season to the next. Overall efficacy is calculated at between 30-60% for adults aged 18 to 65 years lower efficacy in elderly although immunisation is shown to reduce incidence of severe disease including bronchopneumonia, hospital admissions and mortality provisional end-of-season adjusted vaccine effectiveness (VE) estimates for 2019/20 showed an overall VE of 42.7% against all laboratory confirmed influenza VE was 22.7% in 65 year olds and 16.2% for those 65 year olds who received the adjuvanted vaccine (aTIV) VE was 44.5% for 2 to 17 year olds receiving quadrivalent live attenuated influenza vaccine (LAIV) there is evidence of overall significant influenza VE in 2019/20, most notably against influenza A(H1N1)pdm09, but as seen in the past two seasons, there was reduced VE against A(H3N2). the new QIVc vaccine provided significant protection for those in the 18-64 age group The national flu immunisation programme 2020/21

Features of flu easily transmitted by droplets, small-particle aerosols and by hand to mouth/eye contamination from a contaminated surface or respiratory secretions of infected person people with mild or no symptoms can still infect others incubation period 1-5 days (average 2-3 days) though may be longer especially in people with immune deficiency Common symptoms include: 10 sudden onset of fever, chills, headache, muscle and joint pain and extreme fatigue dry cough, sore throat and stuffy nose in young children gastrointestinal symptoms such as vomiting and diarrhoea may be seen The national flu immunisation programme 2020/21

Possible complications of flu Common: bronchitis otitis media (children), sinusitis secondary bacterial pneumonia Less common: meningitis, encephalitis, meningoencephalitis primary influenza pneumonia Risk of most serious illness is higher in 13 children under six months older people those with underlying health conditions such as respiratory disease, cardiac disease, long-term neurological conditions or immunosuppression pregnant women (flu during pregnancy may be associated with perinatal mortality, prematurity, smaller neonatal size and lower birth weight) The national flu immunisation programme 2020/21
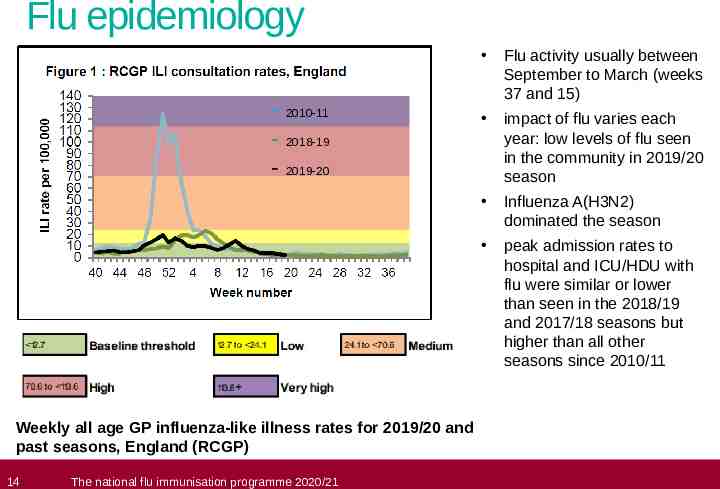
Flu epidemiology - 2010-11 - 2018-19 - 2019-20 Weekly all age GP influenza-like illness rates for 2019/20 and past seasons, England (RCGP) 14 The national flu immunisation programme 2020/21 Flu activity usually between September to March (weeks 37 and 15) impact of flu varies each year: low levels of flu seen in the community in 2019/20 season Influenza A(H3N2) dominated the season peak admission rates to hospital and ICU/HDU with flu were similar or lower than seen in the 2018/19 and 2017/18 seasons but higher than all other seasons since 2010/11

UK flu vaccination programme Late 1960s: annual flu immunisation recommended to directly protect those in clinical risk groups who are at a higher risk of influenza associated morbidity and mortality 2000: flu vaccine policy extended to include all people aged 65 years or over 2010: pregnancy added as a clinical risk category for routine flu immunisation 2013: phased introduction of an annual childhood flu vaccination programme for all children aged 2-16y began with vaccine offered to all children aged 2 and 3 years and seven geographical pilots in primary school aged children 2014: phased introduction of childhood flu vaccination programme continued with vaccine offered to all children aged 2, 3 and 4 years and geographical pilots in primary and secondary school aged children 2015: in addition to vaccinating 2, 3, and 4year olds in primary care, the programme began nationally in primary schools in a phased roll-out starting with the youngest school-aged children first. Between 2016 and 2019: phased introduction of childhood flu vaccination programme continued with a year on year addition of the next school year 2020: offer to all children aged 2 to 11 years old (but not 12 years or older) on 31 August 2020 15 The national flu immunisation programme 2020/21

Flu vaccine eligibility: 2020/21 flu season 16 all those aged two to eleven (but not twelve years or older) on 31 August 2020 people aged six months to under 65 years in clinical risk groups all pregnant women (including those who become pregnant during flu season) people aged 65 years and over (including those becoming 65 years by 31 March 2021) people living in long-stay residential care homes or other long-stay care facilities carers household contacts of those on the NHS shielded patient list and immunocompromised individuals all frontline heath and social care workers individuals between 50 and 64 years may be offered flu vaccine under the NHS flu vaccination programme following prioritisation of other eligible groups and subject to vaccine supply The national flu immunisation programme 2020/21

Frontline health and social care workers All frontline health and social care workers with direct patient/service user contact should be provided with flu vaccination by their employer. This includes staff in all NHS trusts, general practices, care homes, and domiciliary care Employers are encouraged to : Commission a service which makes access to the vaccine easy for all staff Encourage staff to get vaccinated Monitor the delivery of their programme The definition of healthcare workers from the Green Book chapter 12 should be used to identify those eligible as part of the frontline and social care workers programme NHS Trusts are asked to complete a self assessment against best practice checklist (second flu letter dated 5 August 2020) NHS England and Improvement (NHSE/I) will continue to support vaccination of social care and hospice workers, with vaccination available through their employer, community pharmacy or their registered GP practice 17 The national flu immunisation programme 2020/21

Residential care/nursing home residents and staff The community pharmacy seasonal influenza advanced service framework will be amended to enable community pharmacies to vaccinate both residential care/nursing home residents and staff in the home setting in a single visit to increase uptake rates GP practices are also able to vaccinate in the residential/care home, residents and staff who are registered with the practice 18 The national flu immunisation programme 2020/21

Clinical risk groups who should receive flu vaccine (1) Clinical risk category Chronic respiratory disease Examples (this list is not exhaustive and decisions should be based on clinical judgement) Asthma that requires continuous or repeated use of inhaled or systemic steroids or with previous exacerbations requiring hospital admission. Chronic obstructive pulmonary disease (COPD) including chronic bronchitis and emphysema; bronchiectasis, cystic fibrosis, interstitial lung fibrosis, pneumoconiosis and bronchopulmonary dysplasia (BPD). Children who have previously been admitted to hospital for lower respiratory tract disease. Chronic heart disease Chronic kidney disease Chronic liver disease Chronic neurological disease see precautions section on live attenuated influenza vaccine Congenital heart disease, hypertension with cardiac complications, chronic heart failure, individuals requiring regular medication and/or follow-up for ischaemic heart disease. Chronic kidney disease at stage 3, 4 or 5, chronic kidney failure, nephrotic syndrome, kidney transplantation. Cirrhosis, biliary atresia, chronic hepatitis Stroke, transient ischaemic attack (TIA), Parkinson’s disease, motor neurone disease. Conditions in which respiratory function may be compromised due to neurological disease (eg polio syndrome sufferers). Clinicians should offer immunisation, based on individual assessment, to clinically vulnerable individuals including those with cerebral palsy, learning disabilities, multiple sclerosis and related or similar conditions; or hereditary and degenerative disease of the nervous system or muscles; or severe neurological disability Learning disability Diabetes 19 Type 1 diabetes, type 2 diabetes requiring insulin or oral hypoglycaemic drugs, diet controlled diabetes. The national flu immunisation programme 2020/21

Clinical risk groups who should receive flu vaccine (2) Clinical risk category Examples (this list is not exhaustive and decisions should be based on clinical judgement) Immunosuppression (see contraindications and precautions section on live attenuated influenza vaccine) Immunosuppression due to disease or treatment, including patients undergoing chemotherapy leading to immunosuppression, bone marrow transplant, HIV infection at all stages, multiple myeloma or genetic disorders affecting the immune system (eg IRAK-4, NEMO, complement disorders) Individuals treated with or likely to be treated with systemic steroids for more than a month at a dose equivalent to prednisolone at 20mg or more per day (any age), or for children under 20kg, a dose of 1mg or more per kg per day. It is difficult to define at what level of immunosuppression a patient could be considered to be at a greater risk of the serious consequences of influenza and should be offered influenza vaccination. This decision is best made on an individual basis and left to the patient’s clinician. Some immunocompromised patients may have a suboptimal immunological response to the vaccine. Asplenia or dysfunction of the spleen This also includes conditions such as homozygous sickle cell disease and coeliac syndrome that may lead to splenic dysfunction. Pregnant women Pregnant women at any stage ofpregnancy (first, second or third trimesters). (see precautions section on live attenuated influenza vaccine) Morbid obesity (class III obesity)* Defined as a Body Mass Index of 40 and above *Many of this patient group will already be eligible due to complications of obesity that place them in another risk category 20 The national flu immunisation programme 2020/21

Flu immunisation should also be offered to: 21 those living in long-stay residential care homes or other long-stay care facilities where rapid spread is likely to follow introduction of infection and cause high morbidity and mortality (this does not include prisons, young offender institutions, university halls of residence, or boarding schools unless of primary school age) those who are in receipt of a carer’s allowance, or those who are the main carer of an older or disabled person whose welfare may be at risk if the carer falls ill household contacts of patients on the NHS shielded patients list and immunocompromised individuals, specifically those who expect to share living accommodation on most days over the winter and therefore for whom continuing close contact is unavoidable health and social care staff in direct contact with patients/service users should be vaccinated as part of an employer’s occupational health obligation The national flu immunisation programme 2020/21
Other groups who should receive flu vaccine 22 the list of clinical risk groups is not exhaustive healthcare practitioners should apply clinical judgement to take into account the risk of flu exacerbating any underlying disease as well as the risk of serious illness from flu itself flu vaccine should be offered to such cases and will be reimbursed, even if the individual is not in the clinical risk groups specified in the risk groups list child contacts of very severely immunocompromised individuals should be given inactivated vaccine The national flu immunisation programme 2020/21

Why vaccinate these risk groups? Influenza-related population mortality rates and relative risk of death among those aged six months to under 65 years by clinical risk group in England, September 2010 – May 2011 Number of fatal flu cases (%) 23 In a risk group 213 (59.8) Mortality rate per 100,000 population 4.0 Not in any risk group 143 (40.2) 0.4 Baseline Chronic renal disease 19 (5.3) 4.8 18.5 Chronic heart disease 32 (9.0) 3.7 10.7 (7.3-15.7) Chronic respiratory disease 59 (16.6) 2.4 7.4 (5.5-10.0) Chronic liver disease 32 (9.0) 15.8 48.2 (32.8-70.6) Diabetes 26 (7.3) 2.2 5.8 (3.8-8.9) Immunosuppression 71 (19.9) 20.0 47.3 (35.5-63.1) Chronic neurological disease (excluding stroke/transient ischaemic attack) 42 (11.8) 14.7 40.4 (28.7-56.8) Total 378 0.8 The national flu immunisation programme 2020/21 Age-adjusted relative risk 11.3 (9.1-14.0)

Vaccination of clinical risk groups 24 increasing flu vaccine uptake in clinical risk groups is important because of increased risk of death and serious illness if people in these groups catch flu for a number of years only around half of patients aged six months to under 65 in clinical risk groups have been vaccinated vaccine uptake for all clinical risk groups needs to improve for 2020/21, uptake ambition for ‘aged under 65 ‘at risk’, including pregnant women’ is ‘at least 75% in all clinical risk groups, and to maintain higher rates where those have already been achieved Strategies to improve vaccine uptake should be tailored to each risk group to ensure optimum uptake of vaccine in each of them. further information on flu vaccination for those with learning disabilities can be found on the Gov.UK website https://www.gov.uk/government/publications/flu-vaccinations-for-people-with-learning-disabiliti es/flu-vaccinations-supporting-people-with-learning-disabilities The national flu immunisation programme 2020/21

Flu vaccine uptake by individual clinical risk group in 2019/20 (%) GP registered patients aged 6 months to under 65 years Risk group Patients with Diabetes 25 6 months to under 2 years 2 years to under 5 years 17.4 57.7 5 years to under 16 years 16 years to under 65 Total under 65 years 51.9 61.3 61.2 Patients with Chronic Kidney Disease 15.1 43.9 36.7 50.9 50.6 Patients with immunosuppression 13.4 44.9 37.0 44.4 44.0 Patients with Chronic Neurological Disease (including Stroke/TIA, Cerebral Palsy or MS) 12.4 43.8 34.7 43.1 42.3 Patients with Chronic Respiratory Disease 23.5 54.9 45.5 49.3 48.8 Patients with Chronic Heart Disease 17.0 46.2 36.9 41.7 41.1 Patients with Chronic Liver Disease 21.3 50.5 35.8 37.3 37.3 Patients with Asplenia or dysfunction of the spleen 21.0 47.6 32.1 33.2 33.2 Patients with morbid obesity (BMI 40) N/A 34.6 35.1 52.4 52.4 The national flu immunisation programme 2020/21

Flu vaccine uptake in England 2015-2019 (%) Target Group 2019/20 2018/19 2017/18 2016/17 2015/16 % Uptake ambition for 2020/21 Patients aged 65 years or older 72.4 72.0 72.6 70.5 71.0 Patients aged six months to under 65 years in risk groups* 44.9 48.0 48.9 48.6 45.1 Pregnant women in risk group 56.9 60.2 62.1 58.7 40.6 75 Pregnant women NOT in risk group 42.1 43.7 45.7 43.3 55.9 75 All pregnant women 43.7 45.2 47.2 44.9 42.3 75 75 (maintain higher rates where this has already been achieved) 75 (maintain higher rates where this has already been achieved) Health care workers 74.3 70.3 68.7 63.2 50.6 100% offer *The pregnant women and healthcare workers who are also in one or more clinical risk groups may also be included in the 65 years at risk category 26 The national flu immunisation programme 2020/21

Pregnant women All pregnant women are recommended to receive the inactivated flu vaccine irrespective of their stage of pregnancy 27 pregnant women are at increased risk from complications if they contract flu having flu during pregnancy may be associated with premature birth and smaller birth size and weight flu vaccination during pregnancy provides passive immunity against flu to infants in the first few months of life studies on safety of flu vaccine in pregnancy show that inactivated flu vaccine can be safely and effectively administered during any trimester of pregnancy no study to date has demonstrated an increased risk of either maternal complications or adverse fetal outcomes associated with inactivated flu vaccine women should be offered flu vaccine every time they are pregnant The national flu immunisation programme 2020/21

Flu vaccination programme for children Extension of the seasonal flu vaccination programme to children aims to lower the public health impact of flu by: providing direct protection thus preventing a large number of cases of flu infection in children providing indirect protection by lowering flu transmission from children: to other children to adults to those in the clinical risk groups of any age Reducing flu transmission in the community averts many cases of severe flu and flurelated deaths in older adults and people with clinical risk factors Annual administration of flu vaccine to children is expected to substantially reduce flu-related illness, GP consultations, hospital admissions and deaths 28 The national flu immunisation programme 2020/21

Health and social care workers vaccination of health and social care workers protects them and reduces risk of spreading flu to their patients, service users, colleagues and family members evidence that vaccination significantly lowers rates of flu-like illness, hospitalisation and mortality in the elderly in long-term healthcare settings reduces transmission of flu to vulnerable patients, some of whom may have impaired immunity and may not respond well to immunisation frontline health and social care workers have a duty of care to protect their patients and service users from infection vaccination of frontline workers also helps reduce sickness absences and contributes to keeping the NHS and care services running through winter pressures NHS and social care bodies have a responsibility to ensure, as far as is reasonably practicable, that health and social care workers are free of, and are protected from exposure to infections that can be caught at work (Health and Social Care Act 2008, Code of Practice on the prevention and control of infections) The national flu immunisation programme 2020/21

Health and social care workers (2) During the 2019/20 flu season flu vaccine uptake in health care workers with direct patient contact was below the 100% ambition - 74.3% of HCWs were vaccinated (range between regions 69.3% - 78.1%) All doctors 76% GPs 67.2% Total qualified nurses 73.2% Practice nurses 71.7% 30 trusts/employers must ensure that 100% of health and social care staff directly involved in delivering care are offered flu vaccine and encouraged to be immunised in 2020/21, NHS England will continue to support vaccination of social care and hospice workers. Eligible groups will remain the same as in 2019/20 and vaccination will be available through community pharmacy or their registered general practice. This scheme is intended to complement, not replace, any established occupational health schemes that employers have in place to offer flu vaccination to their workforce see Public Health England's Campaign Resource Centre for further information and resources for health and social care worker vaccination The national flu immunisation programme 2020/21

Key messages to health and social care workers getting vaccinated against flu can help protect you, your patients and family everyone is susceptible to flu, even if you are in good health and eat well you can be infected with the virus and have no symptoms but can still pass flu virus to others including patients or residents good infection control measures reduce spread of flu and other acute respiratory infections in healthcare settings but are not sufficient alone to prevent them throughout the last ten years there has generally been a good to moderate match between the strains of flu virus in the vaccine and those that subsequently circulated impact of flu on frail and vulnerable patients can be fatal and outbreaks can cause severe disruption in communities, care homes and hospitals flu vaccine has a good safety record and will help protect you. It cannot give you flu. Having the vaccination can encourage your colleagues to do likewise staff act as positive role models for patients aged 65 and over, those with long-term health conditions and pregnant women to take up the offer too duty of care as professionals to patients or residents to do everything in your power to protect them against infection, including being immunised against flu 31 The national flu immunisation programme 2020/21

When to vaccinate 32 those eligible should be given flu vaccination as soon as vaccine is available so that people are protected when flu begins to circulate in the community ideally most vaccination should be completed before the end of December before flu circulation usually peaks flu can circulate considerably later than this however so clinical judgement should be applied to assess needs of individual patients and whether it is appropriate to continue to offer vaccination from January to March this decision should take into account level of flu-like illness in community and fact that the immune response following flu vaccination takes about two weeks to develop fully as antibody levels likely to reduce in subsequent seasons and there may be changes to circulating strains from one season to next, annual revaccination is important The national flu immunisation programme 2020/21

Which flu vaccine should be used? 33 The national flu immunisation programme 2020/21

Types of flu vaccines Two main types of vaccine available: inactivated – given by injection live attenuated – given by nasal application None of the flu vaccines can cause clinical influenza in those that can be vaccinated Trivalent: flu vaccines contain two subtypes of Influenza A and one type B virus Quadrivalent vaccines contain two subtypes of Influenza A and both B virus types As quadrivalent vaccines contain both lineages of B viruses and therefore may provide better protection against the circulating B strain(s) than trivalent flu vaccines, the live intranasal vaccine offered to children aged 2 years and over is a quadrivalent vaccine Quadrivalent vaccines are now recommended for pregnant women and individuals in risk groups aged 6 months to under 65 years In 2019/20 flu season, a cell based quadrivalent vaccine became available for both under 65 years at risk groups and all 65y and over 34 The national flu immunisation programme 2020/21

Live attenuated influenza vaccine (LAIV) 35 a live attenuated intranasal spray is the recommended vaccine for the childhood flu programme the live attenuated (weakened) influenza vaccine (LAIV) has been shown to be more effective in children compared with inactivated influenza vaccines it may offer some protection against strains not contained in the vaccine as well as to those that are and has the potential to offer better protection against virus strains that have undergone antigenic drift since this vaccine is comprised of weakened whole live virus, it replicates natural infection which induces better immune memory (thereby offering better long-term protection to children than from the inactivated vaccines) in addition to being attenuated, the live viruses in LAIV have been adapted to cold so that they cannot replicate efficiently at body temperature LAIV has a good safety profile in children aged two years and older The national flu immunisation programme 2020/21

Inactivated flu vaccines 36 a number of different manufacturers produce flu vaccines. Those available for 2020/21 season are listed in the “National flu immunisation programme 2020 to 2021’ letter available on PHE website inactivated influenza vaccines are administered by intramuscular injection most currently available flu vaccines are prepared from viruses grown in embryonated hens’ eggs and details of the ovalbumin content of each vaccine is made available on the PHE flu webpage some flu vaccines are restricted for use in particular age groups the SPC for individual products should always be referred to when ordering vaccines for particular patients The national flu immunisation programme 2020/21

Summary of vaccines to be used for the 2020/21 flu programme 37 at risk children aged 6 months to 2 years offer QIVe at risk children aged 2 years up to 18th birthday, offer live attenuated influenza vaccine (LAIV) unless contraindicated* aged 2 and 3 years on 31 August 2020, all primary school aged children and those in year 7 (ages 4 to 11 on 31 August 2020) offer LAIV unless contraindicated at risk adults aged 18 to 64 year olds, including pregnant women, HCWs and carers, offer QIVc or, as an alternative QIVe aged 65 years and over (including those who become 65 before 31 March 2021), offer adjuvanted trivalent influenza vaccine (aTIV) or QIVc if aTIV is unavailable The national flu immunisation programme 2020/21

Vaccine effectiveness in those aged 65 years and over 38 vaccine effectiveness (VE) varies from one season to the next. Overall effectiveness has been estimated at between 30-60% for adults aged 18 to 65 years for flu infection in primary care there is lower effectiveness in older people although immunisation can provide important protection against flu GP consultation and severe disease such as flu confirmed hospital admission in the last decade, there has generally been a good match between the strains of flu in the vaccine and those circulating but there has often been poorer effectiveness against influenza A (H3N2), particularly in the elderly, where burden of infection from that strain is highest the JCVI noted potential explanations for the low effectiveness against influenza A(H3N2). These include immunosenescence (age related reduction in immune response) genetic drift of the circulating viral strain (compared to the vaccine strain e.g. in 2014/15) egg adaptation (in recent seasons, changes to the virus during the manufacturing process have arisen with A(H3N2) strain when flu vaccine strains are propagated in eggs which means that the vaccines do not work as well) The national flu immunisation programme 2020/21

How do we improve vaccine effectiveness in those aged 65 and over? There are a number of potential factors leading to reduced vaccine effectiveness: Factor Explanation Solution Immunosenescence Age related reduction in immune response to vaccination May be addressed by the use of an adjuvanted or higher dose vaccine to boost response in those over 65 years of age against all vaccine strains Genetic drift of the circulating strain Genetic changes in the flu virus can create a mismatch between the vaccine virus strains and the circulating wild type strains The WHO recommendations for the vaccine strains for the forthcoming flu season reflect any changes seen in circulating flu viruses Egg adaptation To produce most flu vaccines, the flu viruses are injected into eggs to generate large amounts of flu virus. However, the viruses adapt to live in the egg, leading to changes in the viruses which means they may not exactly match the circulating strain, thus resulting in reduced vaccine effectiveness Egg adaptation can be addressed using cell based vaccines which do not require the use of eggs in the manufacturing process 39 The national flu immunisation programme 2020/21

2020/21 flu vaccine recommendations for those aged 65 years and over aTIV should be offered as it is considered to be more effective than standard dose non-adjuvanted trivalent and egg-based quadrivalent influenza vaccines 40 QIVc is suitable for use in this age group if aTIV is not available. * it is recommended that those who become 65 before 31 March 2021 are offered aTIV ‘off-label’ (as license is from 65 years) evidence suggests that these vaccines are superior to standard egg-based inactivated trivalent and quadrivalent vaccines (TIVe/QIVe) in terms of effectiveness for those aged 65 years and over the two vaccines use different technologies to overcome the factors highlighted previously. The key characteristics of the two vaccines are described on following slides The national flu immunisation programme 2020/21

Adjuvanted influenza vaccine (aTIV) aTIV (previously marketed as Fluad) was used in the UK in the 2018/19 and 2019/20 flu seasons in 65y and over age group and is used widely elsewhere. It has been used for 20 years and over 93 million doses have been distributed worldwide aTIV has an excellent safety record it has higher immunogenicity and effectiveness than non-adjuvanted, normal dose vaccines in older people aTIV is a trivalent inactivated flu vaccine containing two subtypes of Influenza A (H3N2 and H1N1pdm09) and one type B virus an adjuvant (MF59) has been added to the vaccine to enhance the immune response to counter the effect of immunosenescence (age related reduction in immune response) MF59 adjuvant is an oil-in-water emulsion of squalene oil which is a naturally occurring substance found in humans, animals and plants. In humans, it is made in the liver and circulates in the bloodstream aTIV is made using an egg-based manufacturing process 41 The national flu immunisation programme 2020/21

Quadrivalent influenza cell culture vaccine (QIVc) QIVc (Flucelvax TETRA) was first licenced in the US in 2016 and was licensed in the UK in December 2018 for adults and children from 9 years of age Flucelvax TETRA is a quadrivalent vaccine containing two subtypes of Influenza A (H3N2 and H1N1pdm00) and both B virus lineages. As the vaccine contains both lineages of B viruses it may provide better protection against circulating flu B strain(s) than trivalent flu vaccines QIVc has a similar safety profile to other flu vaccines (similar rate and type of adverse reactions reported). More than 36 million doses of cell-based vaccine have been administered with no serious safety concerns the cell-based vaccine manufacturing process uses an animal cell line (Madin-Darby Canine Kidney, or MDCK) to grow the influenza virus rather than the traditional egg based manufacturing methods this manufacturing process eliminates the risk of egg-adaptation and may result in the vaccine containing virus that is a closer match to wild-type circulating flu viruses 42 The national flu immunisation programme 2020/21

High dose trivalent influenza vaccine (TIV-HD) Trivalent Influenza Vaccine High Dose (TIV-HD) was first licenced in the US in 2009 and was licensed in the UK in January 2019 TIV-HD is a trivalent inactivated flu vaccine containing two subtypes of Influenza A and one type B virus TIV-HD contains four times the amount of antigen contained in standarddose inactivated influenza vaccines. The additional antigen content is intended to enhance the immune response to counter the effect of immunosenescence in those aged 65 and over TIV-HD has been proven to be safe and effective TIV-HD is made using an egg-based manufacturing process High dose trivalent influenza vaccine is not being commissioned by NHSE/I and will not be reimbursed by NHSE/I during 2020/21 43 The national flu immunisation programme 2019/20
Flu vaccine for adults aged 18 to under 65 year olds in clinical risk groups two vaccines will be available for the 2020/2021 flu season for this patient group: 1. The cell cultured quadrivalent influenza cell culture vaccine (QIVc) 2. The egg grown quadrivalent inactivated influenza vaccine (QIVe) as an alternative to QIVc quadrivalent vaccines are recommended as these may provide better protection against the circulating flu B strain(s) which are more likely to affect this younger patient group than older people evidence to date suggests that QIVc is as effective in this patient group as QIVe. However there may be a potential advantage to the use of QIVc as there is no risk of egg adaptation causing a reduction in vaccine effectiveness 44 The national flu immunisation programme 2020/21

Summary of flu vaccines recommended in 2020/21 All those aged 65 years and over Two vaccines are recommended and will be reimbursed on the NHS o The adjuvanted trivalent inactivated influenza vaccine (aTIV) o The quadrivalent influenza cell culture vaccine (QIVc) Evidence suggests that these two vaccines are all superior to standard egg-based inactivated trivalent and quadrivalent vaccines (TIVe/QIVe) in terms of effectiveness for those aged 65 years and over Note: The TIV-HD vaccine is not eligible for reimbursement on the NHS Adults aged 18 to under 65 years old in clinical risk groups (including pregnant women and all health care workers in this age group) Two vaccines are recommended and will be reimbursed on the NHS o The quadrivalent influenza cell culture vaccine (QIVc) o The egg grown quadrivalent inactivated influenza vaccine (QIVe), as an alternative to QIVc 45 The national flu immunisation programme 2020/21

Eligible group At risk children aged from 6 months to less than 2 years Summary table of which flu vaccines to offer children and adults At risk children aged 2 to under 18 years Type of flu vaccine Offer QIVe. LAIV and QIVc are not licenced for children under 2 years of age. Offer LAIV If LAIV is contraindicated or otherwise unsuitable offer: QIVe to children less than 9 years of age. QIVc should ideally be offered to children aged 9 years and over who access the vaccine through general practice. Where QIVc vaccine is unavailable, GPs should offer QIVe. It is acceptable to offer only QIVe to the small number of children contraindicated to receive LAIV aged 9 years and over who are vaccinated in a school setting. Aged 2 and 3 years on 31 August 2020 All primary school aged children and those in Year 7 (aged 4 to 11 on 31 August 2020) Offer LAIV If child is in a clinical risk group and is contraindicated to LAIV (or it is otherwise unsuitable) offer inactivated influenza vaccine (see above). For children not in at risk groups, this year if a parent refuses LAIV in some areas an alternative QIVe or QIVc vaccine may be offered to them where possible. At risk adults (aged 18 to 64), including pregnant women Those aged 65 years and over Offer: QIVc QIVe (as an alternative to QIVc) Offer: aTIV* should be offered as it is considered to be more effective than standard dose non-adjuvanted trivalent and egg-based quadrivalent influenza vaccines. QIVc is suitable for use in this age group if aTIV is not available. * It is recommended that those who become 65 before 31 March 2021 are offered aTIV ‘offlabel’. 46 The national flu immunisation programme 2020/21

Flu vaccine composition 2020/21 Quadrivalent Egg-based vaccines A/Guangdong-Maonan/SWL1536/2019 (H1N1)pdm09-like virus A/Hong Kong/2671/2019 (H3N2)-like virus B/Washington/02/2019 (B/Victoria lineage)-like virus B/Phuket/3073/2013 (B/Yamagata lineage)-like virus Quadrivalent Cell or recombinant-based vaccines A/Hawaii/70/2019 (H1N1)pdm09-like virus A/Hong Kong/45/2019 (H3N2)-like virus B/Washington/02/2019 (B/Victoria lineage)-like virus B/Phuket/3073/2013 (B/Yamagata lineage)-like virus 47 The national flu immunisation programme 2020/21

Trivalent flu vaccine composition 2020/21 The influenza B component in the 2020/21 trivalent vaccines will be the B/Washington/02/2019 (B/Victoria lineage)-like virus so they will not contain B/Phuket/3073/2013-like virus (B/Yamagata/16/88 lineage) More detailed information on the characteristics of the available vaccines, including age indications can be found in the Influenza chapter of the Green Book (Immunisation against infectious disease) and the individual product SPCs 48 The national flu immunisation programme 2020/21

Storage of flu vaccine Efficacy, safety and quality may be adversely affected if vaccines are not stored at the temperatures specified in the licence Flu vaccines must be stored in accordance with manufacturer’s instructions: store between 2⁰C and 8⁰C do not freeze store in original packaging protect from light Check expiry dates regularly: the LAIV has an expiry date 18 weeks after manufacture – this is much shorter than inactivated flu vaccines it is important that the expiry date on the nasal spray applicator is checked before use 49 The national flu immunisation programme 2020/21

Flu vaccine presentation and dosage 50 inactivated influenza vaccines are for intramuscular (IM) administration and are supplied as suspensions in pre-filled syringes containing a 0.5ml dose if the SmPC for IM inactivated flu vaccine states young children can be given either a 0.25ml or a 0.5ml dose, JCVI have advised that 0.5ml dose should be given the live intranasal flu vaccine is supplied as a nasal spray suspension in a single use, pre-filled, nasal applicator with a divider clip. No reconstitution or dilution is required. Each vaccine contains 0.2ml (administered as 0.1 ml per nostril) The national flu immunisation programme 2020/21

Vaccine administration (inactivated vaccines) inactivated flu vaccines should be given intramuscularly into the upper arm (deltoid muscle) of those aged 12 months or older and into the anterolateral aspect of the thigh in infants aged six months to one year of age due to the presence of adjuvant and therefore increased potential for more local reactions if administered by subcutaneous injection, aTIV should only be administered intramuscularly using a 25mm length needle inactivated and live flu vaccines can be given at the same time as, or at any interval before or after, other currently used live and inactivated vaccines if any new vaccines are introduced during the flu vaccination season, please ensure any specific guidance given about concomitant administration for these is followed if given at the same time, different vaccines should be given at separate sites, preferably in a different limb. If given in the same limb, they should be given at least 2.5cm apart 51 The national flu immunisation programme 2020/21

Patients taking anticoagulants or with a bleeding disorder 52 Individuals on stable anticoagulation therapy (including individuals on warfarin who are up-to-date with their scheduled INR testing and whose latest INR was below the upper threshold of their therapeutic range) can receive intramuscular vaccination if in any doubt, consult with the clinician responsible for prescribing or monitoring the individual’s anticoagulant therapy Individuals with bleeding disorders may be vaccinated intramuscularly if, in the opinion of a doctor familiar with the individual's bleeding risk, vaccines or similar small volume intramuscular injections can be administered with reasonable safety by this route if the individual receives medication/treatment to reduce bleeding, for example treatment for haemophilia, intramuscular vaccination can be scheduled shortly after such medication/treatment is administered a fine needle (equal to 23 gauge or finer calibre) should be used for the vaccination, followed by firm pressure applied to the site (without rubbing) for at least 2 minutes influenza vaccines licensed for intramuscular or subcutaneous administration may alternatively be administered by the subcutaneous route. aTIV, Fluarix Tetra and Flucelvax Tetra are not licensed for subcutaneous administration so should only be administered intramuscularly The national flu immunisation programme 2020/21

Administration of Live Attenuated Influenza vaccine (LAIV) LAIV is different from other flu vaccines – it is a live attenuated nasal vaccine and must not be injected do not attempt to attach a needle LAIV can be administered at the same time as, or at any interval from other currently used vaccines including live vaccines the applicator has a divider clip to enable one application in each nostril the patient should breathe normally - they do not need to actively inhale or sniff the vaccine is rapidly absorbed so there is no need to repeat either half of dose if patient sneezes, blows their nose or their nose drips following administration 53 The national flu immunisation programme 2020/21

Supply and administration of flu vaccines A range of mechanisms can be used for the supply and administration of vaccines, including: Patient prescription written manually or electronically by a registered medical practitioner or other authorised prescriber Patient Specific Direction (PSD) Patient Group Direction (PGD) PGD templates for the administration of the live and inactivated flu vaccines are available on the PHE website: https://www.gov.uk/government/collections/immunisation-patient-group-direction-pgd Those using national immunisation PGDs developed by PHE must ensure that each PGD is organisationally authorised and signed in section 2 by an appropriate authorising person, in accordance with Human Medicines Regulations 2012 (HMR2012) Without such authorisation, the PGD is not legal or valid 54 The national flu immunisation programme 2020/21

Contraindications (inactivated vaccine and LAIV) there are very few individuals who cannot receive any flu vaccine where there is doubt, expert advice should be sought promptly so that the period the individual is left unvaccinated is minimised for children aged 2 years up to their 18th birthday, where live flu vaccine cannot be given, it is likely that inactivated vaccine could be given instead None of the influenza vaccines should be given to those who have had: 55 confirmed anaphylactic reaction to a previous dose of the vaccine confirmed anaphylactic reaction to any component of the vaccine The national flu immunisation programme 2020/21

Contraindications to LAIV confirmed anaphylactic reaction to a previous dose of flu vaccine confirmed anaphylactic reaction to a component of LAIV (for example to gelatine) or residue from the manufacturing process (gentamicin), except egg proteins (see subsequent slide on egg allergy) clinically severely immunocompromised due to a condition or immunosuppressive therapy such as: acute and chronic leukaemias lymphoma HIV infection not on highly active antiretroviral therapy (HAART) cellular immune deficiencies high dose corticosteroids receiving salicylate therapy known to be pregnant Also contraindications for children with acute and severe asthma - see subsequent specific slide 56 TheThe national national flu immunisation childhood flu programme immunisation 2020/21 programme 2014/15

Precautions to flu vaccines Acutely unwell: defer until recovered Heavy nasal congestion: defer live intranasal vaccine until resolved or, if the child is in a risk group, consider inactivated flu vaccine to provide protection without delay Use with antiviral agents against flu: live flu vaccine (LAIV) should not be administered at the same time or within 48 hours of cessation of treatment with flu antiviral agents administration of flu antiviral agents within two weeks of administration of LAIV may adversely affect the effectiveness of the vaccine 57 The national flu immunisation programme 2020/21

Acute and severe asthma in 2019, JCVI advised that children with asthma on inhaled corticosteroids may safely be given LAIV irrespective of the dose prescribed LAIV is not recommended for children and adolescents currently experiencing an acute exacerbation of symptoms including those who have had increased wheezing and/or needed additional bronchodilator treatment in the previous 72 hours Such children should be offered a suitable inactivated influenza vaccine to avoid a delay in protection children who require regular oral steroids for maintenance of asthma control, or have previously required intensive care for asthma exacerbation should only be given LAIV on the advice of their specialist As these children may be at higher risk from influenza infection, those who cannot receive LAIV should receive a suitable inactivated influenza vaccine Children with significant asthma and aged under nine years who have not been previously vaccinated against influenza will require a second dose (of either LAIV or inactivated vaccine as appropriate). 58 The national flu immunisation programme 2020/21

Egg allergy in adults 59 most flu vaccines are prepared from flu viruses grown in embryonated hens’ eggs – the final vaccine products contains varying amounts of egg protein as ovalbumin adults with egg allergy can be immunised in any setting using an ovalbumin-free vaccine (QIVc) or an inactivated flu vaccine with an ovalbumin content less than 0.12 µg/ml (equivalent to 0.06µg for 0.5ml dose) adults with severe anaphylaxis to egg that has previously required intensive care should be referred to a specialist for assessment with regard to receiving immunisation in hospital or given QIVc adults with egg allergy can also be given the quadrivalent inactivated egg-free vaccine, Flucelvax Tetra (QIVc) ovalbumin content for the 2020/21 flu vaccines is published on PHE Annual flu programme webpage The national flu immunisation programme 2020/21

Egg allergy in children children with an egg allergy can be safely vaccinated with LAIV in any setting (including primary care and schools) children who have required admission to intensive care for a previous severe anaphylaxis to egg should be given LAIV in the hospital setting children with both egg allergy and a clinical risk factor that contraindicate LAIV (such as immunosuppression) should be offered an inactivated flu vaccine* with a very low ovalbumin content (less than 0.12μg/ml) children over age nine years with egg allergy can also be given the quadrivalent inactivated egg-free vaccine, Flucelvax TETRA egg-allergic children with asthma can receive LAIV if their asthma is well-controlled (see previous slide on severe asthma) *Children in a clinical risk group and aged under nine years who have not been previously vaccinated against influenza will require a second dose whether given LAIV or inactivated vaccine 60 The national flu immunisation programme 2020/21

Ovalbumin content of vaccines available for 2020/21 61 The national flu immunisation programme 2020/21

Risk of transmission of live vaccine virus 62 there is a theoretical potential for transmission of live attenuated flu virus to immunocompromised contacts transmission risk is for one to two weeks following vaccination following extensive use of the live attenuated influenza vaccine in US, there have been no reported instances of illness or infections from the vaccine virus among immunocompromised patients inadvertently exposed to vaccinated children however, if close contact with very severely immunocompromised patients (such as bone marrow transplant patients requiring isolation) is likely or unavoidable (for example other household members) consider an appropriate inactivated flu vaccine instead The national flu immunisation programme 2020/21

Exposure of healthcare workers to live attenuated influenza vaccine viruses theoretically there may be some low level exposure to the vaccine viruses during administration of LAIV and/or from recently vaccinated patients risk of acquiring vaccine viruses from the environment is unknown but probably low the vaccine viruses are cold-adapted and attenuated and therefore unlikely to cause symptomatic influenza in the US, where there has been extensive use of LAIV: no transmission of vaccine virus in healthcare settings has ever been reported no reported instances of illness or infections from the vaccine virus among healthcare workers inadvertently exposed 63 as a precaution, very severely immunosuppressed individuals should not administer LAIV other healthcare workers who have less severe immunosuppression or are pregnant, should follow normal clinical practice to avoid inhaling the vaccine and ensure that they themselves are appropriately vaccinated The national flu immunisation programme 2020

Inadvertent administration of LAIV 64 if an immunocompromised individual receives LAIV, the degree of immunosuppression should be assessed if patient is severely immunocompromised, antiviral prophylaxis should be considered otherwise they should be advised to seek medical advice if they develop flu-like symptoms in the four days following administration of the vaccine if antivirals are used for prophylaxis or treatment, patient should also be offered inactivated flu vaccine in order to maximise their protection in the forthcoming flu season (this can be given straight away) The national flu immunisation programme 2020/21

Commonly reported adverse reactions Following inactivated flu vaccine: pain, swelling or redness at the injection site, low grade fever, malaise, shivering, sweating, fatigue, headache, myalgia and arthralgia a small painless nodule may also form at the injection site these symptoms usually disappear within one to two days without treatment Due to the MF59 adjuvant, a higher incidence of mild post-immunisation reactions has been reported with aTIV, compared to non-adjuvanted influenza vaccines Following live attenuated flu vaccine: nasal congestion/rhinorrhoea, reduced appetite, weakness and headache Rarely, after live or inactivated vaccine, immediate reactions such as urticaria, angiooedema, bronchospasm and anaphylaxis can occur 65 The national flu immunisation programme 2020/21

Reportingsuspectedadversereactions All serious suspected reactions following flu vaccination should be reported to the Medicines and Healthcare products Regulatory Agency using the Yellow Card scheme at http://yellowcard.mhra.gov.uk/ Five of the flu vaccines recommended for use during 2020/21 carry a black triangle symbol ( ) (as do all vaccines during the earlier stages of their introduction) This is to encourage reporting of all suspected adverse reactions 66 The national flu immunisation programme 2020/21

Vaccine ordering DHSC has procured additional national supply of adult vaccine to support the expected increased demand for flu vaccine across all cohorts and the expanded flu programme PHE centrally purchases flu vaccines (live and inactivated) for: all children aged 2 and 3 years and all children of primary school age children in clinical risk groups aged 6 months to less than 18 years 67 flu vaccines for children can be ordered through the ImmForm website as for other centrally purchased vaccines (www.immform.dh.gov.uk) providers are responsible for ordering sufficient flu vaccine for all other eligible patients aged 18 years and older directly from manufacturers providers should ensure they are able to offer the most effective vaccine for each eligible group consistent with national guidance provided a patient is offered a recommended vaccine for their age, providers are not expected to have to offer a choice between vaccines there is always the possibility that initial batches of vaccine may be subject to delay, or that fewer doses than planned may be available initially. Providers should remain flexible when scheduling vaccination sessions and be prepared to reschedule if necessary The national flu immunisation programme 2020/21

Inactivated influenza vaccine for children contraindicated to receive LAIV children for whom LAIV is medically contraindicated should be offered a suitable alternative inactivated flu vaccine for children in clinical risk groups under 18 years of age where LAIV is contraindicated or otherwise unsuitable: QIVe should be offered to children less than 9 years of age QIVc (locally procured) should ideally be offered to children aged 9 years and over who access the vaccine through general practice. Where QIVc vaccine is unavailable, GPs should offer QIVe (supplied free of charge by PHE) it is acceptable to offer QIVe to the small number of children contraindicated to receive LAIV aged 9 years and over who are vaccinated in a school setting 68 if the inactivated vaccine supplied by PHE is not used, please be aware that not all inactivated flu vaccines are licensed for children and some contain too much ovalbumin for egg allergic children always check SPC for vaccine suitability before administration The national flu immunisation programme 2020/21

Recording flu vaccine given As a wide variety of influenza vaccines are on the UK market each year, it is especially important that the following information be recorded: vaccine name, product name, batch number and expiry date dose administered date immunisation given route/site used name and signature of vaccinator This information should be recorded in: 69 patient's GP record (or other patient record, depending on location) personal Child Health Record (the ‘Red Book’) if a child practice computer system Child Health Information System if a child Information on flu vaccines administered outside general practice (e.g. maternity providers, pharmacies) must be passed back to the patient’s GP practice in a timely manner (within 48 hours) so patient records can be updated The national flu immunisation programme 2020/21

Data collection 70 flu vaccine uptake data is collected via the web-based ImmForm system ( www.immform.dh.gov.uk) where it is managed and published by PHE over 95% GP practices are able to make automated data returns where the number of their patients vaccinated is directly extracted from their IT system and put into ImmForm for data to be accurate and complete, it is critical that vaccines given outside the surgery, such as in antenatal clinics or pharmacies, are reported to the patient’s GP uptake data for HCWs is manually submitted by trusts and area teams via ImmForm data is collected and published monthly at national level and local NHS England team level for all the groups for whom flu vaccine is indicated to enable performance to be reviewed and time to take action if needed The national flu immunisation programme 2020/21

Achieving high flu vaccine uptake many of the groups who are vulnerable to flu are also more vulnerable to COVID-19. Not only is it important to help protect those most at risk of flu, it is also important to protect the health of those who are vulnerable to hospitalisation and death from COVID-19 by ensuring they do not get flu for the 2020/21 flu season, immunisers are being asked to make a concerted effort to significantly increase flu vaccination coverage and achieve a minimum 75% uptake across all eligible groups it is essential to increase flu vaccination levels for those who are living in the most deprived areas and from BAME communities. High quality, dedicated and culturally competent engagement with local communities, employers and faith groups will be required 71 The national flu immunisation programme 2020/21

Achieving high flu vaccine uptake A variety of flu leaflets and posters are available to order in several different languages and for different eligible groups. See PHE immunisation webpage “Annual flu programme” section 72 The national flu immunisation programme 2020/21

Achieving high flu vaccine uptake Dexter et at (2012) identified independent factors associated with higher vaccine uptake in general practice. These were presented as a GP practice checklist in the annual flu letter for 2019/20 and the key findings are summarised below: 73 having a lead staff member for planning the flu campaign and producing a written report of practice performance predicted an 8% higher vaccination rate for at-risk patients aged 65 years sending a personal invitation to all eligible patients and only stopping vaccination when Quality and Outcomes Framework targets were reached, predicted a 7% higher vaccination rate in patients aged 65 years using a lead member of staff for identifying eligible patients, with either a modified manufacturer's or in-house search programme for interrogating the practice IT system, independently predicted a 4% higher vaccination rate in patients aged 65 years the provision of flu vaccine by midwives was associated with a 4% higher vaccination rate in pregnant women The national flu immunisation programme 2020/21

Delivering the programme during the COVID-19 pandemic higher demand for flu vaccine is expected this autumn because of concerns about COVID-19. Patients will need reassurance that appropriate measures are in place to keep them safe from COVID-19, as it is likely to be co-circulating with flu. This reassurance will be especially important for those on the NHS Shielded Patient List. providers will be expected to deliver the programme according to guidelines on social distancing that are current at the time. Standard operating procedures in the context of COVID-19 have been issued for General Practice, community pharmacy, and community health services providers need to be prepared to make adjustments to the programme in the face of any local restrictions to ensure those at highest risk can continue to be vaccinated. 74 The national flu immunisation programme 2020/21

Considerations when delivering the flu vaccine programme during the COVID-19 pandemic careful appointment planning to minimise waiting times and maintain social distancing when attending provide patients with information in advance of their appointment to explain what to expect recall at risk patients if they do not attend consider social distancing innovations such as drive in vaccinations and ‘car as waiting room’ models, if possible for those on the Shielded Patient List who are high risk for COVID-19, consider the use of domiciliary visits for the schools vaccination programme, any social distancing measures will create additional challenges. The expectation is that school estate will still be used in the event of any local school closures where possible 75 The national flu immunisation programme 2020/21

Infection prevention and control when administering vaccines individuals should attend for vaccination at premises that are following the recommended infection prevention and control (IPC) guidance. www.england.nhs.uk/coronavirus/primary-care/infection-control/ those displaying symptoms of COVID-19, or who are self-isolating because they are confirmed COVID-19 cases or are contacts of suspected or confirmed COVID-19 cases, should not attend until they have recovered and completed the required isolation period. healthcare professionals administering the vaccine will need to wear personal protective equipment (PPE) in keeping with current advice at the time. See: www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-pre vention-and-control/covid-19-personal-protective-equipment-ppe 76 The national flu immunisation programme 2020/21

Key messages 77 flu immunisation is one of the most effective interventions we can provide to reduce harm from flu and pressures on health and social care services during the winter but it is important to increase flu vaccine uptake in all groups this year for a number of years, only around half of patients aged six months to under 65 years in clinical risk groups have been vaccinated influenza during pregnancy may be associated with perinatal mortality, prematurity, smaller neonatal size, lower birth weight and increased risk of complications for mother vaccination of health and social care workers protects them and reduces risk of spreading flu to their patients, service users, colleagues and family members by preventing flu infection through vaccination, secondary bacterial infections such as pneumonia are prevented. This reduces the need for antibiotics and helps prevent antibiotic resistance those attending for flu vaccination will need reassurance that appropriate measures are in place to keep them safe from COVID-19 as it is likely to be cocirculating with flu The national flu immunisation programme 2020/21

Resources Letters detailing 2020/21 flu programme Available at: www.gov.uk/government/publications/national-flu-immunisation-programme-plan Green Book Influenza chapter Available at: www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book Leaflets, posters, information materials and other resources to support the annual flu programme Available at: www.gov.uk/government/collections/annual-flu-programme PGD templates for flu vaccines www.gov.uk/government/collections/immunisation-patient-group-direction-pgd A video for health professionals on how to administer the LAIV vaccine produced by NHS Education for Scotland is available at www.nes.scot.nhs.uk/education-and-training/by-theme-initiative/public-health/health-protection/sea sonal-flu/childhood-seasonal-flu-vaccination-programme-resources-for-registered-practitioners.aspx Summary of Product Characteristics (SPC) for flu vaccines are available at www.medicines.org.uk/emc/ Leaflets and posters prepared specifically for the flu programme. Available at: www.gov.uk/government/organisations/public-health-england/series/annual-flu-programme Healthcare Workers Flu Immunisation resources (leaflets, posters, guides and resource packs) available at https://campaignresources.phe.gov.uk/resources/campaigns/92-healthcare-workers-flu-immunisation-/resources 78 To order leaflets, posters and download translations visit: [email protected] You will need to register for the free service The national flu immunisation programme 2020/21

About Public Health England Public Health England exists to protect and improve the nation's health and wellbeing, and reduce health inequalities. It does this through world-class science, knowledge and intelligence, advocacy, partnerships and the delivery of specialist public health services. PHE is an operationally autonomous executive agency of the Department of Health. Public Health England Wellington House 133-155 Waterloo Road London SE1 8UG Tel: 020 7654 8000 www.gov.uk/phe Twitter: @PHE uk Facebook: www.facebook.com/PublicHealthEngland For enquiries relating to this document, please contact: [email protected] Crown copyright 2020 You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0. To view this licence, visit OGL or email [email protected]. Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned. Published August 2020 PHE publications gateway number: 2020201 79 The national flu immunisation programme 2020/21