The Electronic Medical Record and the Practicing Physician:
62 Slides7.60 MB
The Electronic Medical Record and the Practicing Physician: an Oxymoron? Carol Steltenkamp, M.D., MBA Chief Medical Information Officer

An Equal Opportunity University 2

Objectives Discuss the role of the Electronic Medical Record (EMR) in the office setting Identify what to look for in an EMR Review implementation challenges and understand post-implementation outcomes

Clinical Mission: Ambulatory A multispecialty group practice providing primary & specialty care 106 Best Doctors 80 specialized clinics, 150 outreach programs Provide services primarily in Lexington and Central and Eastern Kentucky 400,000 outpatient visits (2007) at main campus locale Greater than 1 million outpatient visits across the Enterprise UK Chandler Hospital

Clinical Mission: Inpatient 800 beds 35, 000 discharges Level 1 Trauma Center Centers of Excellence in Cardiology, Oncology, and Neurosciences Kentucky Children’s Hospital

Research Mission 127.5 million grants & contracts awarded at UK College of Medicine*; 62.8 million in NIH funding UK’s medical center colleges account for more than 55% of UK total research dollars Research figures prominently in quest for Top 20 status *2007

Educational Mission Six colleges: Medicine Nursing Pharmacy Dentistry Health Sciences Public Health 1000 clinical faculty 500 physicians in residency
WHY Health Information Technology (HIT)? Implementation of HIT is proposed as a way to provide additional information to clinicians to facilitate a reduction in serious medical errors, rising healthcare costs and system inefficiencies. (Thompson, 2004) Estimate annual 10.6 billion outpatient savings and 31.2 billion inpatient savings based on HIT efficiency benefits (Girosi, Meili,& Scoville, 2005) President Bush State of the Union “we make wider use of electronic records and other HIT, to help control costs and reduce dangerous medical errors (Jan 2006) An Equal Opportunity University 8

Problem: Increased Costs In 2003, U.S. health spending per capita was 5,635, two and a half times more than the comparable median for industrialized countries ( 2,280 per capita). 15% of US GDP was spent on health care in 2003; other countries median was 8.4% (Anderson et al, 2005) Higher medical care prices make health care unaffordable for many Americans, yet the extra dollars spent are not yielding demonstrably better quality of care or patient satisfaction. (Gerard et al,2005) U.S. spends 2.1 times as much on healthcare as Canada, France, Germany, Italy, Japan and the United Kingdom. Healthcare spending grew “faster than growth in both the aggregate economy and employee compensation, which suggests an increasing burden on sponsors and employers” (Smith et al., 2005, p. 193). An Equal Opportunity University 9

Problem: Information Explosion If only 1% of new literature in Medline is healthcare related, if the clinician reads 2 articles daily for a year, they will be 5 years behind the current state of knowledge. (Masys, 2002) Medline indexes 560,000 new articles, and Cochrane Central adds 20,000 new randomized trials annually 1500 new articles and 55 new trials per day (Glaszious and Haynes, 2005) An Equal Opportunity University

Institute of Medicine “despite more than 30 years of work and millions of dollars, patient care records are predominantly paper, which limits tools for effective decision-making from the bedside to national healthcare policy” (IOM, 1991). “ A highly fragmented delivery system that largely lacks even rudimentary clinical information capabilities results in poorly designed care processes characterized by unnecessary duplication of services, and long waiting times and delays.” (IOM, 2001) Medical errors, rising healthcare costs, and quality problems are cited as widespread issues that need to be addressed (Institute of Medicine, 2001) An Equal Opportunity University
Electronic Health Record The IOM presented eight core functions that should be provided in an electronic health record: health information and data results management order entry/management decision support electronic communication and connectivity patient support administrative support reporting population health management (Institute of Medicine, 2003). An Equal Opportunity University

Current Issues in Ambulatory Care Inability to find critical information quickly 30% of physician time spent searching, up to 81% of time information is still not found in record. JAMA While quality of care is improving, ambulatory care shows the least overall improvement (1.4% between 2003 and 2004). AHRQ An Equal Opportunity University 13
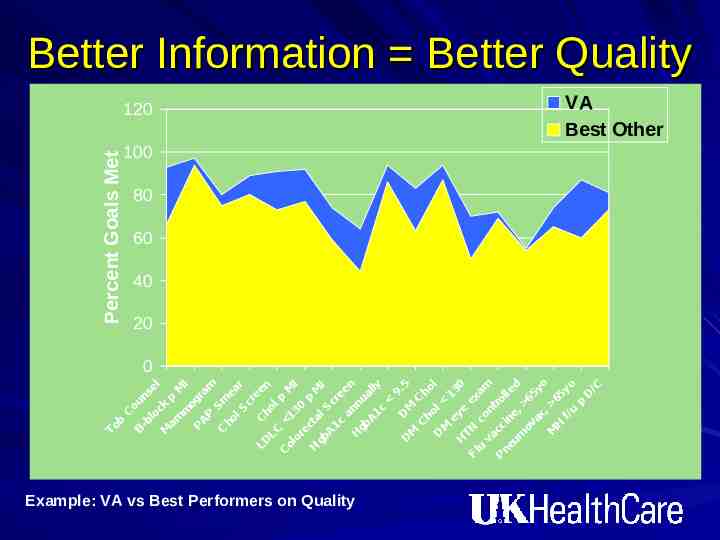
C ou B n -b lo sel ck M am p M m I og P AP ra m Sm C ho e l S ar cr ee LD C n h o LC lp C M ol 1 I 30 or ec p t H M gb al I S A c 1c re an en H gb nu a A 1c lly 9. D 5 D M M C C ho h D ol l M ey 13 0 H TN e e Fl x am u c va on t c r P ne cin olle um e, d ov 6 ax 5y , o M 65 H f/u yo p D /C To b Percent Goals Met Better Information Better Quality 120 Example: VA vs Best Performers on Quality VA Best Other 100 80 60 40 20 0

Percentage of office-based physicians using electronic medical records and using comprehensive electronic medical record systems: United States, 2001–2006

Percentage of medical practices using electronic medical records and using comprehensive electronic medical record systems: United States, 2003–04 through 2006

Percentage of physicians using electronic medical records and using comprehensive electronic medical record systems by practice size: United States, 2006

Estimated Percentage of Office-Based Physicians Using Selected Electronic Medical Record (EMR) Features National Ambulatory Medical Care Survey, United States, 2006

Percent distribution of physicians planning new or replacement electronic medical record systems within next 3 years by whether current system is fully or partially electronic: United States 2006
Barriers to Adoption Capital costs* Not finding a system that meets their needs* Uncertainty about return on investment* Concern that a system would become obsolete* DesRoches, et. al., NEJM, July3, 2008

Facilitators of Adoption Financial incentives for purchase Payment for use of an electronic records system Protecting physicians from personal liability DesRoches, et. al., NEJM, July3, 2008

Effect of Adoption of Electronic Health Records Systems DesRoches, et. al., NEJM, July3, 2008

Case for Change

Case for Change If you can read it, how long did it take you to decipher the handwriting?

A Moment in the Physician Office While promoting medical quality and E/M compliance, in 15 minutes MD must be able to: Perform and complete documentation of a medically indicated, audit-proof, level 4 or level 5 initial patient visit with individualized narrative information in all appropriate areas of the medical record including completion of counseling the patient, ordering tests, ordering treatment, and charge entry.

The Cost/Benefit Ratio Costs Benefits Cash outlay Improved quality of care High initial physician time and decreased patient volume An Equal Opportunity University Improved throughput Charge capture

Getting Started Announce the goal- even if it’s ambitious Test big ideas on a small scale Find best practices and use them as measurements (internal and external) Build the discipline and methods of Project Management into the work Thomas Nolan.The Pursuit Continues. Pursuing Perfection: Raising the Bar for Healthcare Performance. Modern Healthcare, Feb 28, 2005.

Ambulatory Workflow Optimization Together with the progress in medicine, which provides for an earlier diagnosis and intervention, healthcare information technology for process optimization will be the prerequisite to further improve the quality of care while reducing costs
EMR Barriers Implementations are costly Start up, maintenance, workflow changes Organizational influences Level of integration- what user wants globally vs what user expects personally Types of practices Leadership High initial physician time Customization Miller & Sim. Physician’s Use of Electronic Medical Records: Barriers and Solutions. Health Affairs. Vol 23, No 2

Why the reluctance by clinicians to adopt IT systems May partially be a generational issue Main reason may be that so far EMR has not delivered time savings for physicians and nurses, in fact, in many circumstances when not fully deployed, costs time Main justification may be in addressing cost, quality and safety issues

Electronic Medical Record Source: Clinical Advisory Board interviews and analysis.

Leadership, Communication, and Training Dealing with smaller staffs Cooperation and input by all is a ‘must’ Just-in-time training

Current State Workflow Customization for clinics is Key- filters, lists, etc. Role identification Maximize efficiency and clinician focus while patient is in clinic. More chronic, episodic care in clinic 34
Patient Focused Interaction Schedule appointment Register In room Patient/clinician encounter Clinical Documentation Immunizations Pharmacopeia Check-out

Scheduling and Arrival Patient selfscheduling Registration Completion of intake information

Tracking Board

In Room Not all “clinicians” are created equal What type of data entry Considerations about data validity Not all patients or clinicians are comfortable with computer in room Match hardware to clinician job

Patient/Clinician Encounter Clinical Documentation Patient Care Orders Pharmacopeia Immunizations Medications Prescriptions Check-Out

Clinical Documentation Phone note(s) Dictation/transcription or clinical documentation Copy forward Ability to access other clinical data Attestation statements

Clinical Documentation I can type anything in this text box.

Clinical Documentation
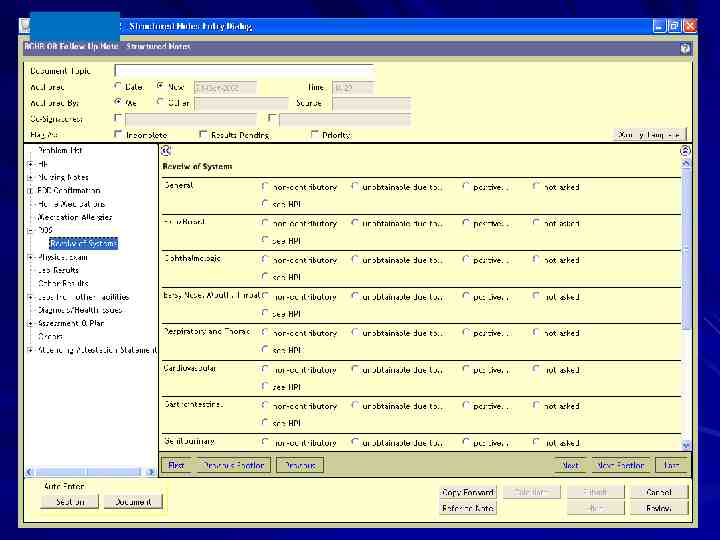
Automated Expansion of Note

Output of Structured Note

Patient Care Orders Does this add value to the outpatient visit? Future dated Legal question- who can “take off order” “CPOE” in Ambulatory Order sets

Medications and Immunizations Documenting med administration Sample management Central repository across all locations Who enters Policy for historical entry Reports

Prescriptions Prescriptionsworkflow is critical Refill request process Who can enter “on behalf of” PHARMACY

Check-out Superbill (Fee Sheet) Patient Name Date of service Level of service/procedure code(s) Diagnosis Goals: Interface with clinician documentation Electronic feed to billing
Clinician Workflow Inbox/Mailbox Results Review Alerts Documents Prescriptions Health Messaging Staffing Billing Encounter Reconciliation Reports

Inbox/Mailbox Results Delegates- “the BOOK” Alerts Documents Rx Refills Health Messaging

Inbox/Mailbox

“The Book” Labor intensive Re-work End of day process Single assigned task Margin for error
Results Delegates Real-time Clinic centric Who can be delegate? Protocols for normal/abnormal

Alerts/Decision Support Management Acknowledgement “on behalf” Maintenance

Documents, Rx Refills, Messaging Documentation Incomplete vs “complete” Rx Refill Clinic protocols Scope of practice Appropriateness of messages Policy & procedure

Staffing Scope of Practice Rx refills Hardware Considerations Types of devices Number of devices Device location

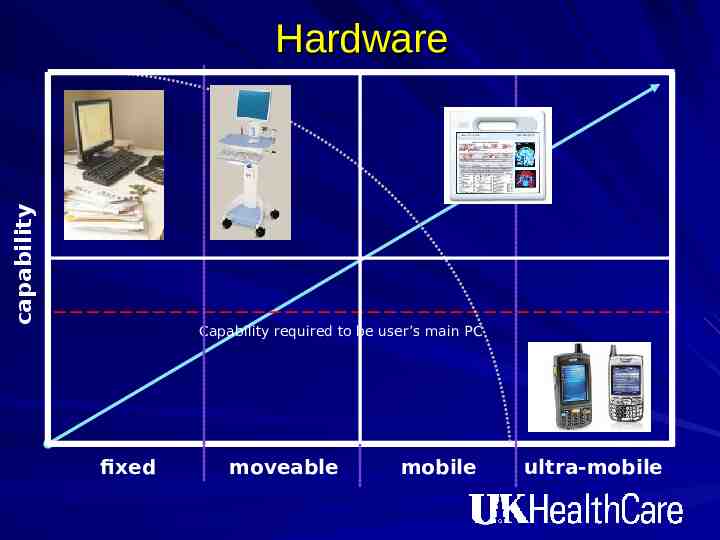
capability Hardware Capability required to be user’s main PC fixed moveable mobile ultra-mobile
Other Considerations Timing of implementation Decision-making authority Budget/Resources Fighting desire for ‘over customization'

Conclusion "We can't solve problems by using the same kind of thinking we used when we created them." -Albert Einstein

Common eHealth Projects An Equal Opportunity University

UK HealthCare Information Technology Guiding Principles Services 2010 Accountability- Based Practice Access to Data at the Point of Service Service Oriented Culture Patient Centric Care Innovation is Rewarded RHIO 2009 Patient Health Record 2008 Clinical Decision Support Data Repository Data Warehouse 2007 CPOE Interdisciplinary Documentation Pre 2007 ED Tracking (ED Manager) Electronic EKG Results TraceMaster Radiology Siemens Registration (PM) McKesson OB QS Fetal Monitoring System Endoscopy Provation Patient Accounts McKesson Citrix Medical Records Soft Med Device Integration Pharmacy Mediware Worx Capacity Command Scanning Center Patient Tracking Other Ancillary Services Sunrise Clinical Viewer Financial Decision Support (SDMS) Portals Web Enablers EMAR OR Management PICIS Cardiology (Witt, Phillips) Remedy Support Center Scheduling RSS Physician Referral Secure Health Messaging Ambulatory Care Barcode ICU Predictor Medication Apache Administration Pathology Laboratory Cerner Mysis CoPathPlus Single Sign On Sentillion Electronic Health Record RFID ERP/ Inventory Mgt. SAP Pharmacy Pyxis Registry’s PACS (Trauma, cancer, OTTR, Tumor) Dictation/ Transcription Soft Med CBORD Diet Office Management Bar-Coding Patient Identification KMSF Physician Billing (SMS) Mobile Devices (Hand held) (wireless) Case Management Soft Med Server Based Infrastructure Utilization Review McKesson Claims/ Billing SSI

President-Elect Obama and Healthcare IT 10 Billion/year for 5 years to help physicians and other providers adopt healthcare IT After the first 5 years, phase in requirements for providers to adopt IT Small providers and those serving rural and underserved populations would receive top priority for financial support