Step by Step: Initiating and/or Enhancing Billable Services Module
48 Slides7.30 MB
Step by Step: Initiating and/or Enhancing Billable Services Module 1: Building Your Internal Billing Infrastructure
RR Health Strategies Pam D’Apuzzo, CPC, ACS-EM, ACS-MS, CPMA Jean Davino, DHA, MS, CLT 2
Learning Objectives Describe billable services and providers Discuss carrier contracting Describe provider credentialing Explore IT (information technology) infrastructure Discuss general billing considerations 3

Services and Providers 4
Services and Providers Select the type of services to be provided at the Practice/Clinic. Medical Services: Outpatient/Ambulatory Health Services (general medicine, specialty care such as neurology, OBGYN, dermatology) Mental Health Services (including Behavioral) Home and Community-Based Health Services (physical medicine and rehabilitation) Substance Abuse Outpatient Care 5

Services and Providers Expanded services to enhance quality and access to care: Preventive Services - (Outpatient/Ambulatory Health Services) Diabetes Education (Health Education/Risk Reduction or Medical Nutrition Therapy) Vaccines (Outpatient/Ambulatory Health Services) Telehealth Home Health Care Laboratory Testing- (Outpatient/Ambulatory Health Services) Medical Nutrition Therapy 6
Services and Providers Select the provider type(s) to render services at your Practice/Clinic. Provider Types: Physician (MD, DO) NPP (non-physician practitioners) PA, NP, Chiropractor, Acupuncturist Psychologist, Clinical Social Worker, Licensed Mental Health Counselor, Substance Abuse Counselor Nutritionists, Registered Dieticians Diabetic Counselors 7
Services and Providers Licensing and Scope of Practice Individual states have a Department of Education and Licensing (Office of the Professions) The scope of practice for each provider type describes the procedures, actions, and processes that the practitioner is permitted to undertake in keeping with the terms of their professional license The practitioner’s scope of practice is limited to that which the law allows for their specific education and experience, and demonstrated competency 8

Carrier Contracting 9
Carrier Contracting Key Definitions Health Maintenance Organization (HMO) HMOs offer comprehensive coverage for both hospital and physician services. They may contract for either capitated or fee-for service reimbursements. Typically, HMO patients have restricted (or no) access to out-of-network services, and may require primary care physicians to act as “gatekeepers” of medically necessary care (referrals). Preferred Provider Organization (PPO) PPOs offer patient benefits at a reasonable cost by providing incentives to use in-network providers. These incentives can be lower deductibles and copays. Physician reimbursement is usually fee-for-service. Patients who wish to access physicians outside the network usually may do so at a higher out of pocket expense. Point of Service (POS) A point-of-service plan is a type of managed care plan that is a hybrid of HMO and PPO plans. Like an HMO, participants designate an in-network physician to be their primary care provider. But like a PPO, patients may go outside of the provider network for health care services. 10
Carrier Contracting Key Definitions Medicare/Medicaid These programs have traditional delivery systems and also managed care models in some areas. The managed care products are contracted through various managed care organizations and may require additional contracts and credentialing. Managed Care Organization (MCO) An organization that combines the functions of health insurance, delivery of care, and administration. Examples include the independent practice association (IPA), third-party administrator, management service organization, and physician-hospital organization. 11
Carrier Contracting The following factors should be considered when determining carrier participation: Patient population Medicare and Medicaid Local Carriers Existing contracted carriers and payor mix (if an established practice/clinic) Carrier reimbursement rates Covered plan benefits 12
Carrier Contracting Research Carriers in your area. Consider the following: Market share Do they have group contracts and are these agreements with large or small employers? Proximity of other participating providers, including specialists to whom you may refer Local in-network hospitals Contact the Provider Relations Department Inquire how applications are handled (paper, electronic, Council for Affordable Quality Healthcare - CAQH) Request a copy of the plan’s fee schedule Review your local Medicare Administrative Contractor (MAC) covered services and fee schedule(s) Research regional Managed Care Plans and fee schedules Research regional Local and Union Plans and fee schedules Research regional ACO (Accountable Care Organizations)/IPAs 13
Carrier Contracting Important Tips: Compile a list of the practice/clinic’s billing CPT codes in order to review and compare carrier fee schedules Compare your local MAC’s fee schedule(s) to the commercial/managed care fee schedules Confirm coverage for any highly specialized services performed If your practice/clinic is providing a highly specialized service not readily offered by other providers in your area, be sure to advise the carrier during your contract negotiations Obtain data from your billing system and review payment history by: (1) Carrier (2) CPT-4 procedure code Develop a carrier grid by plan and CPT code to review and compare reimbursement rates for the various plans Review and compare existing contracts to identify variances in reimbursement rates and determine which contract terms may need to be reevaluated 14
Carrier Contracting The following standards should be clearly listed in the managed care contract: Covered Services: Confirm that all services provided by the practice/clinic are considered a covered benefit Medically Necessary: Confirm the list of services and exclusions from coverage Reimbursement guidelines must be clearly outlined The carrier fee schedule should be attached to the contract as an Exhibit or Addendum Termination clause: The practice/clinic and provider rights, as well as the MCO’s guidelines for contract termination should be clearly noted All relevant documents referenced in the contract, but not immediately available, must be requested for review and approval prior to contract execution 15
Carrier Contracting Accountable Care Organizations (ACO) The Federal Government, in an effort to improve outcomes and keep down costs, has proposed a value-based payment form of reimbursement as an alternative and potential replacement for feefor-service reimbursement Value-based care is a form of reimbursement that connects payments for delivery of care to the quality of care provided and rewards providers for both efficiency and effectiveness The traditional fee-for-service reimbursement model was based upon quantity of services An ACO is a group of healthcare providers who voluntarily come together to coordinate healthcare services and engage in valuebased payment models 16
Carrier Contracting Accountable Care Organizations (ACO) CMS designed the program to help providers ensure that patients receive the most appropriate care at the right time. ACOs also aim to prevent unnecessary and redundant services while reducing medical errors Providers who participate in ACOs are still paid on a fee-for-service basis, but the programs create an incentive to be more efficient by offering bonuses when providers keep costs down. Doctors and hospitals have to meet specific quality benchmarks, focusing on prevention and carefully managing patients with chronic diseases. Providers get paid more for keeping their patients healthy and out of the hospital On the other hand, providers in most ACOs must assume some financial risk for joining. While the potential of savings could be great depending on the agreement, there is also a potential for shared losses. Providers may have to repay Medicare for not providing value-based care to patients Additional information on the ACO programs that Medicare offers can be found at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/ 17
Carrier Contracting Independent Practice Associations (IPA) An IPA is a business entity organized and owned by a network of independent physician practices for many purposes, including negotiating contracts with Managed Care Organizations Physician members of an IPA maintain control of their individual businesses, and receive support on enhanced contracting, cost containment measures, improving quality measures and general practice support An IPA may offer discounts on malpractice insurance, and group purchasing 18
Carrier Contracting Independent Practice Associations (IPA) Before joining an IPA, a practice/clinic needs to consider many factors including: How long has the IPA been in existence? What plans do they contract with? Can the rates for plans be reviewed prior to contracting? Can we join and only participate in some of the contracts? Do we need to have privileges in contracted hospitals? What is the cost to join and maintain membership in the IPA? Can I also participate with other IPAs? Who manages the IPA? How does this affiliation affect Accountable Care Organization (ACO Participation)? 19
Medicaid Billing State governments administer Medicaid programs and regulations and billing requirements vary state-by-state Medicaid is the last payer to be billed for a service Prior to billing Medicaid, investigate the following: Claim specifics – forms and formats both for paper and electronic claim submission Covered services, thresholds and authorization procedures Fee schedules Clearinghouse functions as they relate to processing Medicaid claims 20

Provider Credentialing 21
Provider Credentialing Credentialing is a process used to evaluate the qualifications and practice/clinic history of a provider This process includes a review of completed education, training, residency, board certification and licenses The information obtained from the State Licensing Department/Office of the Professions will provide information regarding the licensing and/or professional certification requirements for individual provider types The credentialing process may take several weeks to months to complete 22
Provider Credentialing A provider should refrain from rendering services without proper credentialing in place. Insurance carriers will not reimburse any services performed by a non-credentialed provider According to the Federal Register, it is considered fraudulent to bill for the services of a provider under another provider’s name and carrier ID number due to credentialing status Some insurance carriers will backdate the contract effective date. However, this is not common practice 23
Provider Credentialing The Council for Affordable Quality Healthcare (CAQH) is a non-profit alliance of health plans and networks nationwide. CAQH works with partner health plans to streamline the credentialing process for those plans through a database ( www.caqh.org) Carrier application processes vary and may include completion of a unique credentialing application or a state standardized application Due to the complexity of the provider credentialing process, one person in an organization should be designated to handle the process If it is a large practice/clinic, more than one staff member should be involved to handle the process and a Credentialing Committee should be formed to oversee the process Some practices/clinics elect to outsource credentialing to vendors specializing in this area 24
Provider Credentialing Curriculum Vitae (months & years required) Hospital Affiliations & Privileges Proof of Continuing Education Malpractice Face Sheet Explanation of any pending or settled malpractice cases during the last five years Clinical Laboratory Improvement Amendments (CLIA) Certification W-9 Current drivers license State License Drug Enforcement Administration (DEA) Certificate Board Certification Diploma-(copy of highest level of education completed) Educational Commission for Foreign Medical Graduates (ECFMG) Certificate (required if educated outside of the US) Certificates of completion for all medical training (internship, residency, fellowship) National Provider Identification (NPI) Professional credentialing verification and documentation requirements will vary according to carrier specific credentialing guidelines. 25
Provider Credentialing A spreadsheet should be developed to better track your practice/clinic’s credentialing efforts. In addition to the credentialing items noted in the previous slide, the spreadsheet should include the following fields: Carrier Name Application Type (paper, CAQH, electronic) Submission Date Verification of Submission Additional Information Requested Carrier Contact Information Notes 26
Provider Credentialing Once the application process has begun, record the names of the insurance carriers, and the date the applications were completed Create a “NOTES” section to maintain pertinent information regarding the process Be sure to maintain meticulous records for submissions (copies of the application, electronic confirmation sheet, CAQH reference number, etc.) If mailing information, issue all correspondence via Certified mail, Return Receipt Requested 27
Provider Credentialing Follow-up within two weeks of submission to confirm receipt of the application Inquire with Carrier regarding their Credentialing Committee meeting schedule Document missing information requests in the spreadsheet, along with the corresponding subsequent submission dates of these documents Be sure to obtain confirmation of any follow-up submissions 28
Provider Credentialing The credentialing grid should also be utilized to assist with “expirables management.” The following items will expire and should be carefully tracked to maintain up-to-date Provider credentials: State License DEA License Malpractice Board Certification Hospital Reappointment Driver’s License CLIA Certificate Cardiopulmonary resuscitation (CPR)/Automated External Defibrillator (AED) Certification The re-credentialing date for each carrier should also be tracked Re-credentialing dates vary by carrier (e.g., annual, every 2 years) 29

IT Infrastructure 30
IT Infrastructure An IT infrastructure includes Network, Hardware, and Software. Networks: Internet connection Network enablement Firewall Security systems Hardware: Servers Computers Switches, hubs and routers Data centers Offsite storage 31
IT Infrastructure Software: The software needed to perform operational functions for the practice/clinic must be selected prior to developing the IT infrastructure These programs are complicated and require significant hardware to run them efficiently Hardware and Software can be implemented in three (3) distinct ways: In-house implementation Virtual private network Cloud-based 32
IT Infrastructure Software Selection Electronic Medical Records (EMR) Software provides the ability to maintain a digital patient medical record. The key functions of an EMR system include: Physician access to patient information, including diagnoses, allergies, past histories, laboratory results, medications, etc. Access to current and previous test results performed by providers in multiple care settings Computerized provider order entry Computerized decision support systems to prevent drug interactions Secure electronic communication with other providers and patients Patient access to health records, disease management tools, and health information resources Computerized administration processes, such as scheduling Standards-based electronic data storage and reporting for patient safety and disease surveillance efforts 33
IT Infrastructure Software Selection Practice Management (PM) Software provides the mechanism to monitor all operations within the practice/clinic including, but not limited to: Maintaining patient demographic information Appointment scheduling and insurance verification Insurance plan maintenance Billing operations Report generation General Software: Email/Office Programs (Outlook, Microsoft Word, etc.) Security Programs Accounting Software 34
IT Infrastructure Important factors to consider when selecting software: Number and types of providers and clinical support staff Number of non-clinical office staff Financial considerations – short and long-term Security and confidentiality of patient medical records Complexity of the software system – user friendly Training provided – remote, in-person Billing module functionality Flexibility/Scalability Specialty specific software vs. general software EMR templates – ease of creation and use Compliance – Health Insurance Portability and Accountability Act (HIPAA) Service contract costs 35
Software Selection EMR software should have the ability to generate detailed patient and population health reporting data for the quality measures required for value-based programs Discuss the reporting package in detail to ensure the reporting capabilities include data requirements for: Medicare Access and CHIP Reauthorization Act (MACRA)/ Merit-based Incentive Payment System (MIPS) ACO Patient-Centered Medical Home (PCMH) CMS has certain standards for EMR software and has certified the software brands meeting these standards. CMS’ software database may be searched by product or developer. Prior to making a decision, verify the EMR software certification at https://chpl.healthit.gov 36

Considerations 37
Selecting a Clearinghouse A Clearinghouse functions as an intermediary between the practice/clinic and the insurance carriers. The Clearinghouse functionality should include the following key Revenue Cycle features: Eligibility verification File Status Rejection Analysis - Dashboard Secondary Claims Processing Electronic Remittance Advice (ERA)/Payment Processing Proof of Timely Filing Paper Claim Submission 38
Clearinghouse Selection Claim scrubbing through a series of edits prior to claim submission Claim submission to multiple plans simultaneously (837 file) Claim status from the plan allowing for errors to be corrected prior to submission Insurance eligibility ERA (electronic remittance advice – 835 file, electronic Explanation of Benefits which can be uploaded directly to PM system for automated payment posting) Timely filing information for insurance rejections Print and submit paper claims, when necessary Patient statement processing Rejection analysis and reporting tools 39
Selecting a Clearinghouse Additional items to consider when selecting a clearinghouse are: Is the software compatible with your PM system? Are they contracted with the most common carriers for your practice/clinic? What is the clearinghouse’s proficiency level with government plans (Medicare/Medicaid) ? What is the speed of the scrubbing and claim rejection reports? Is the clearinghouse a regional or national company? What are the available days and hours for technical support offered, and what is the turnaround time for support issues? Are there additional costs involved with the various functions (claim submission, eligibility, etc.)? 40
Electronic Funds Transfer (EFT) EFT provides a process for insurance plans to direct deposit claim payments directly to a practice/clinic’s financial institution EFTs offer healthcare organizations a safe, convenient, and timely alternative to paper checks and other manual forms of payment. Standards for electronic payment and remittance were developed under the HIPAA Regulations and Affordable Care Act Payment is processed and deposited into the organization’s bank account in approximately two weeks after “clean claim” submission Utilization of the EFT function allows for practice/clinic efficiencies: Paperwork reduction Staff time for banking reduced Faster access to funds Easier bank statement reconciliation 41
Lockbox A lockbox is a system whereby paper insurance correspondence and payments, patient correspondence and payments, and all other correspondence are issued directly to the practice/clinic’s financial institution, rather than the physical practice/clinic location A lockbox requires the practice utilize a designated Post Office box rather than the physical practice/clinic address for remittances Checks are deposited in the practice/clinic’s designated account, and all related documentation is scanned by the financial institution staff The scanned documents are accessible by the designated practice/clinic personnel A lockbox can ease administrative burdens for office staff by eliminating inefficient in-house manual processes, such as processing mail, photocopying, and making deposits 42
Lockbox Lockbox considerations: Are the checks and explanation of benefits (EOBs) returned to the practice/clinic via paper or an online electronic archiving system? How often does the financial institution download claim correspondence and payments? Are denial files processed separately from claim payment files? What options are available for denials management? Will the financial institution provide the practice/clinic with electronic access to records of claims and payments received? Is the service HIPAA compliant? Does the financial institution provide a temporary solution which enables the practice/clinic to scan EOBs and upload them while the P.O. Box transition is in process? Does the financial institution offer interest on the funds in the lockbox account? Is the solution Cloud-based? Which Lockbox features are standard and which represent additional costs to the practice/clinic? 43
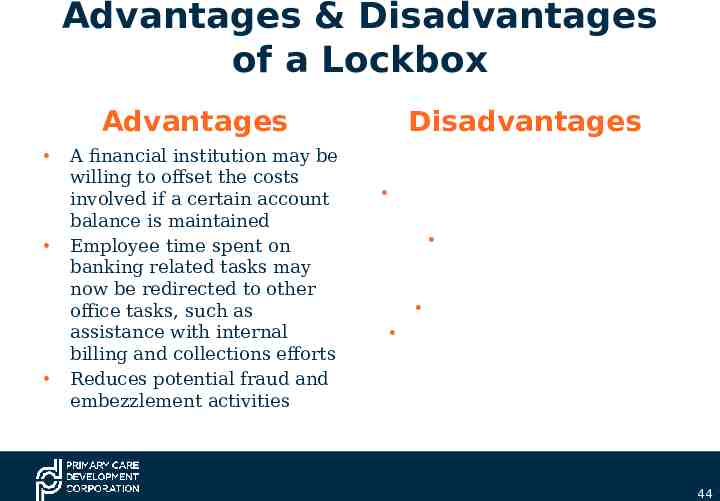
Advantages & Disadvantages of a Lockbox Advantages A financial institution may be willing to offset the costs involved if a certain account balance is maintained Employee time spent on banking related tasks may now be redirected to other office tasks, such as assistance with internal billing and collections efforts Reduces potential fraud and embezzlement activities Disadvantages Funds may be directed to the wrong account Missing EOBs and other documents during the scanning process Receiving incorrect EOBs Potential delays in obtaining copies of EOBs 44
Case Study 45
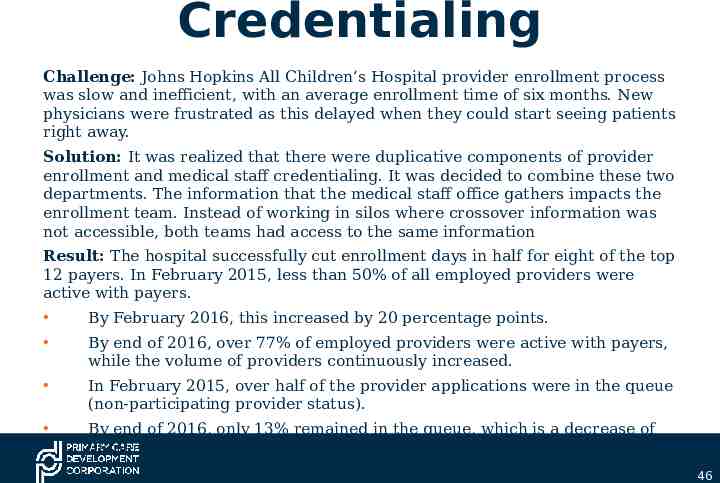
Credentialing Challenge: Johns Hopkins All Children’s Hospital provider enrollment process was slow and inefficient, with an average enrollment time of six months. New physicians were frustrated as this delayed when they could start seeing patients right away. Solution: It was realized that there were duplicative components of provider enrollment and medical staff credentialing. It was decided to combine these two departments. The information that the medical staff office gathers impacts the enrollment team. Instead of working in silos where crossover information was not accessible, both teams had access to the same information Result: The hospital successfully cut enrollment days in half for eight of the top 12 payers. In February 2015, less than 50% of all employed providers were active with payers. By February 2016, this increased by 20 percentage points. By end of 2016, over 77% of employed providers were active with payers, while the volume of providers continuously increased. In February 2015, over half of the provider applications were in the queue (non-participating provider status). By end of 2016, only 13% remained in the queue, which is a decrease of 38 percentage points 46
Module 1 Highlights Selection of medical services and provider types to best suit the Practice/Clinic’s mission and goals Strategies for optimal contract negotiations with carriers Provider credentialing techniques IT Infrastructure development Clearinghouse considerations for positive Revenue Cycle outcomes EFT and the cash flow advantages Utilization of a Lockbox for streamlining the collection and payment processes 47
Module 1 Mini-assignment Prepare a list of proposed services and provider types you are considering for your practice/clinic Create a spreadsheet of your existing carriers, including initial contract dates, expiration dates, and any known CPT Codes and their associated fees or provide your current carrier contract spreadsheet Prepare a provider credentialing grid as described in the “Provider Credentialing” section or review and update your current grid List all current practice/clinic software and any challenges you may be experiencing If you have a Clearinghouse, list the advantages and disadvantages of the system Draft a list of questions regarding utilization of EFT Draft a list of questions regarding utilization of Lockbox 48