Schizophrenia Chapter 16
55 Slides111.00 KB
Schizophrenia Chapter 16
Schizophrenia Fascinated and confounded healers for centuries One of most severe mental illnesses – 1/3 of population – 2.5% of direct costs of total budget – 46 billion in indirect costs
History of Schizophrenia 1800s - Eugene Kraeplin named it “dementia praecox.” 1900s - Eugen Bleuler named it schizophrenia (split minds). More than one type. Kurt Schneider - First rank (psychosis, delusions) and second rank (all other experiences)
Schizophrenia Diagnosis During a one-month period at least two of the five – Positive (delusions, hallucinations, etc.) – Negative (alogia, anhedonia, flat affect, avolition) One or more areas of social or occupational functioning
Types of Schizophrenia Text Box 16.1 Paranoid Disorganized Catatonic Undifferentiated Residual
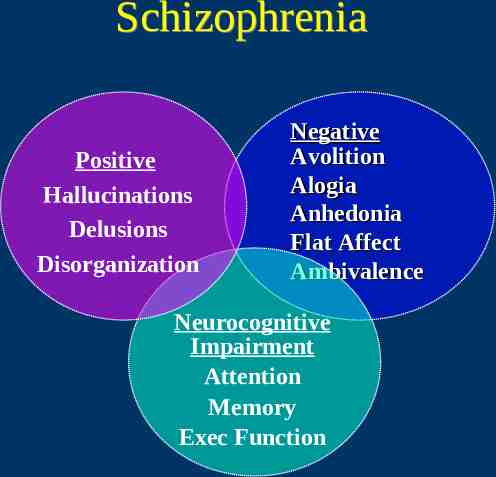
Schizophrenia Positive Hallucinations Delusions Disorganization Negative Avolition Alogia Anhedonia Flat Affect Ambivalence Neurocognitive Impairment Attention Memory Exec Function
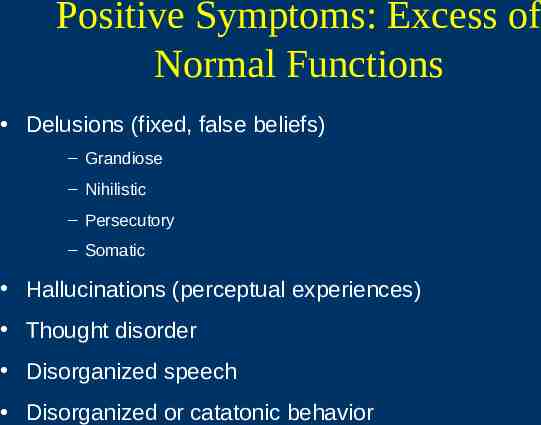
Positive Symptoms: Excess of Normal Functions Delusions (fixed, false beliefs) – Grandiose – Nihilistic – Persecutory – Somatic Hallucinations (perceptual experiences) Thought disorder Disorganized speech Disorganized or catatonic behavior
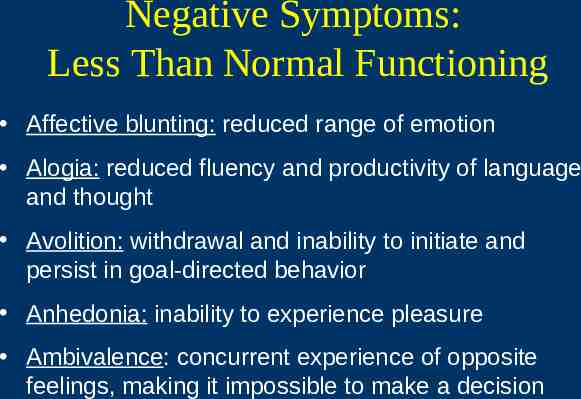
Negative Symptoms: Less Than Normal Functioning Affective blunting: reduced range of emotion Alogia: reduced fluency and productivity of language and thought Avolition: withdrawal and inability to initiate and persist in goal-directed behavior Anhedonia: inability to experience pleasure Ambivalence: concurrent experience of opposite feelings, making it impossible to make a decision
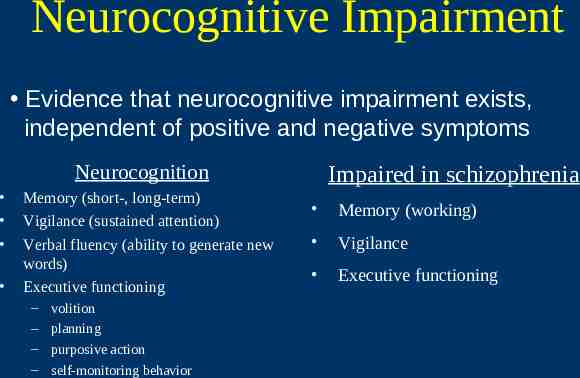
Neurocognitive Impairment Evidence that neurocognitive impairment exists, independent of positive and negative symptoms Neurocognition Memory (short-, long-term) Vigilance (sustained attention) Verbal fluency (ability to generate new words) Executive functioning – – – – volition planning purposive action self-monitoring behavior Impaired in schizophrenia Memory (working) Vigilance Executive functioning
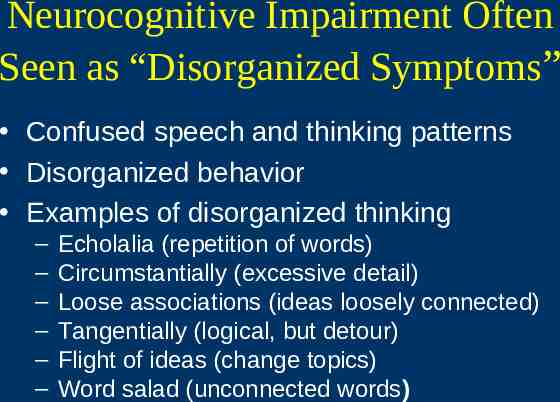
Neurocognitive Impairment Often Seen as “Disorganized Symptoms” Confused speech and thinking patterns Disorganized behavior Examples of disorganized thinking – – – – – – Echolalia (repetition of words) Circumstantially (excessive detail) Loose associations (ideas loosely connected) Tangentially (logical, but detour) Flight of ideas (change topics) Word salad (unconnected words)

Disorganized Symptoms Examples of disorganized thinking (cont.) – Neologisms (new words) – Paranoia (suspiciousness) – References ( special meaning) – Autistic thinking (private logic) – Concrete thinking (lack of abstract thinking) – Verbigeration (purposeless repetition) – Metonymic speech (interchange words)
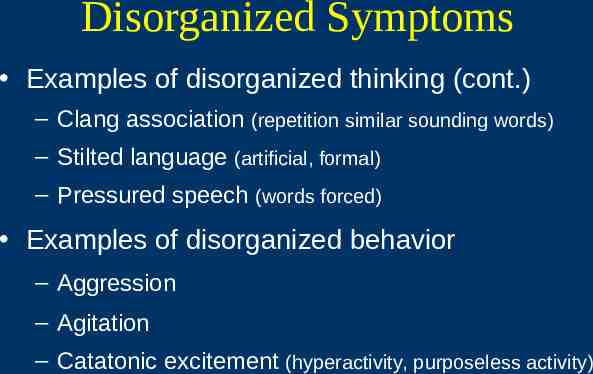
Disorganized Symptoms Examples of disorganized thinking (cont.) – Clang association (repetition similar sounding words) – Stilted language (artificial, formal) – Pressured speech (words forced) Examples of disorganized behavior – Aggression – Agitation – Catatonic excitement (hyperactivity, purposeless activity)
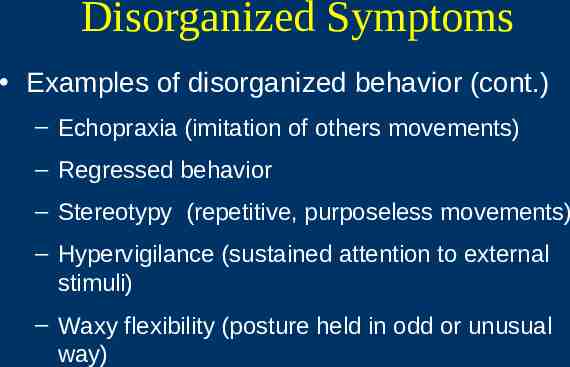
Disorganized Symptoms Examples of disorganized behavior (cont.) – Echopraxia (imitation of others movements) – Regressed behavior – Stereotypy (repetitive, purposeless movements) – Hypervigilance (sustained attention to external stimuli) – Waxy flexibility (posture held in odd or unusual way)
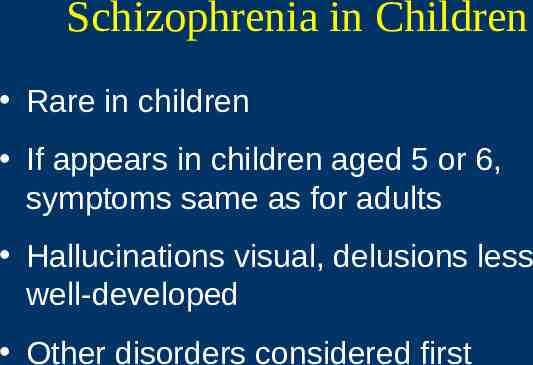
Schizophrenia in Children Rare in children If appears in children aged 5 or 6, symptoms same as for adults Hallucinations visual, delusions less well-developed Other disorders considered first
Schizophrenia in Elderly For those who have had schizophrenia most of their life, this may be a time that they experience improvement in symptoms. Late-onset schizophrenia – Diagnostic criteria met after 45 – Most likely include positive symptoms
Epidemiology 0.5%-1.5% of population 300,000 acute episodes each year Cluster in lower socioeconomic group Homelessness is a problem.
Epidemiology Across all cultures In the United States, African Americans have a higher prevalence rate (thought to be related to racial bias). Men are diagnosed earlier. EOS: Diagnosed late adolescence LOS: Diagnosed 45 years
Maternal Risk Factors Prenatal poverty Poor nutrition Depression Exposure to influenza outbreaks War zone exposure Rh-factor incompatibility
Infant and Childhood Risk Factors Low birth weight Short gestation Early developmental difficulties CNS infections
Familial Differences First-degree biologic relatives have 10 times greater risk for schizophrenia. Other relatives have higher risk for other psychiatric disorders.
Comorbidity Increased risk of cardiovascular disorders Association between insulin-dependent diabetes and schizophrenia Depression and pseudodementia Increased substance abuse Cigarette smoking Fluid imbalance
Disordered Water Balance Prolonged periods of polydipsia, intermittent hyponatremia, polyuria Etiology – unknown Prevention of water intoxication Promotion of fluid balance
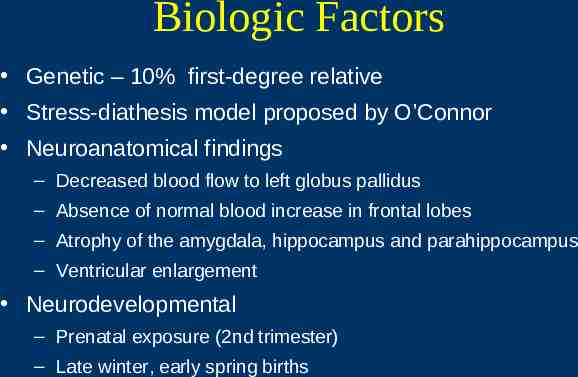
Biologic Factors Genetic – 10% first-degree relative Stress-diathesis model proposed by O’Connor Neuroanatomical findings – Decreased blood flow to left globus pallidus – Absence of normal blood increase in frontal lobes – Atrophy of the amygdala, hippocampus and parahippocampus – Ventricular enlargement Neurodevelopmental – Prenatal exposure (2nd trimester) – Late winter, early spring births
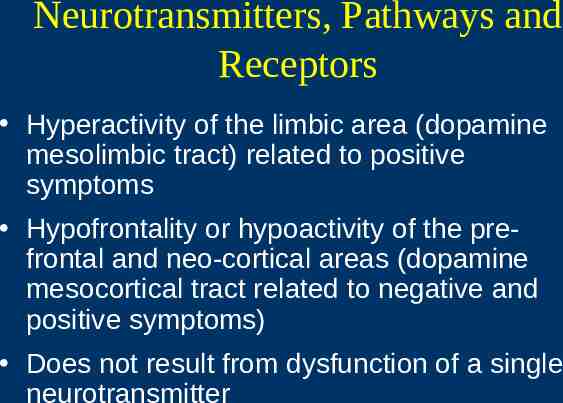
Neurotransmitters, Pathways and Receptors Hyperactivity of the limbic area (dopamine mesolimbic tract) related to positive symptoms Hypofrontality or hypoactivity of the prefrontal and neo-cortical areas (dopamine mesocortical tract related to negative and positive symptoms) Does not result from dysfunction of a single neurotransmitter
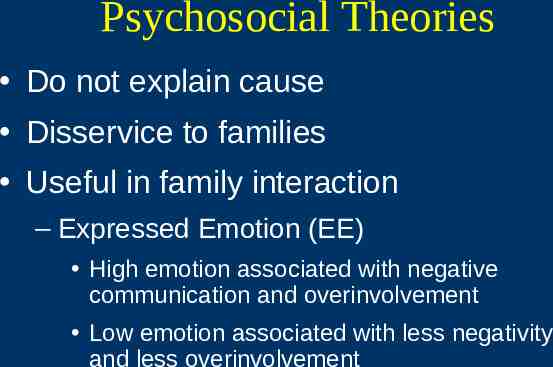
Psychosocial Theories Do not explain cause Disservice to families Useful in family interaction – Expressed Emotion (EE) High emotion associated with negative communication and overinvolvement Low emotion associated with less negativity and less overinvolvement
Priority Care Issues Suicide Safety of patient and others Initiate antipsychotic medications
Family Response to Disorder Mixed emotions – shock, disbelief, fear, care, concern and hope May try to seek reasons Initial period very difficult
Interdisciplinary Treatment The most effective approach involves a variety of disciplines. There is considerable overlap of roles and interventions. Nursing’s contribution is significant.
Nursing Management: Biologic Domain Assessment Present and past health status Physical functioning Nutritional assessment Fluid imbalance assessment Pharmacologic assessment Medications (prescribed, OTC, herbal, illicit) Abnormal motor movements – DISCUS – AIMS – Simpson-Angus Rating Scale
Nursing Diagnosis: Biologic Domain Self-care deficit Disturbed sleep pattern Ineffective therapeutic regimen management Imbalanced nutrition Excess fluid volume Sexual dysfunction
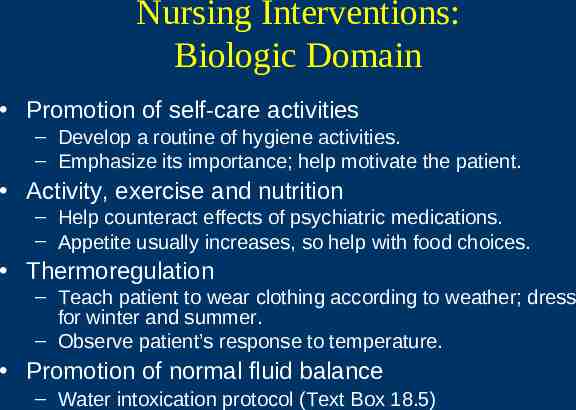
Nursing Interventions: Biologic Domain Promotion of self-care activities – Develop a routine of hygiene activities. – Emphasize its importance; help motivate the patient. Activity, exercise and nutrition – Help counteract effects of psychiatric medications. – Appetite usually increases, so help with food choices. Thermoregulation – Teach patient to wear clothing according to weather; dress for winter and summer. – Observe patient’s response to temperature. Promotion of normal fluid balance – Water intoxication protocol (Text Box 18.5)
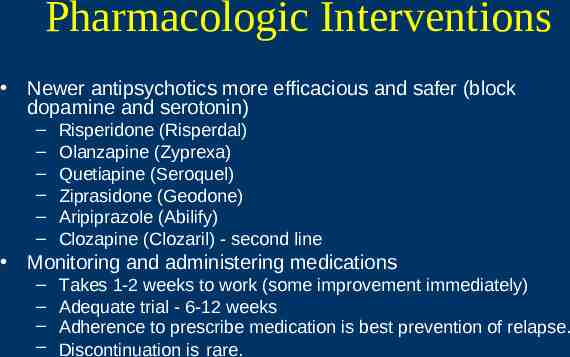
Pharmacologic Interventions Newer antipsychotics more efficacious and safer (block dopamine and serotonin) – – – – – – Risperidone (Risperdal) Olanzapine (Zyprexa) Quetiapine (Seroquel) Ziprasidone (Geodone) Aripiprazole (Abilify) Clozapine (Clozaril) - second line Monitoring and administering medications – – – – Takes 1-2 weeks to work (some improvement immediately) Adequate trial - 6-12 weeks Adherence to prescribe medication is best prevention of relapse. Discontinuation is rare.
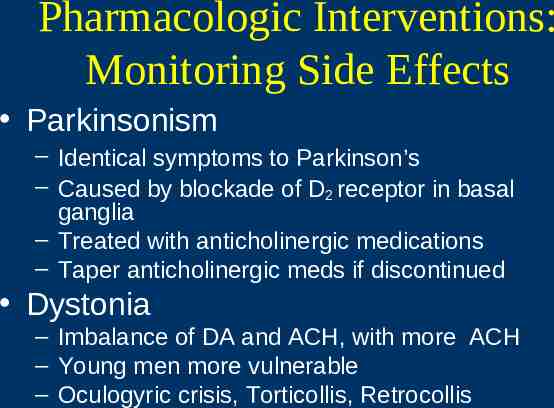
Pharmacologic Interventions: Monitoring Side Effects Parkinsonism – Identical symptoms to Parkinson’s – Caused by blockade of D2 receptor in basal ganglia – Treated with anticholinergic medications – Taper anticholinergic meds if discontinued Dystonia – Imbalance of DA and ACH, with more ACH – Young men more vulnerable – Oculogyric crisis, Torticollis, Retrocollis
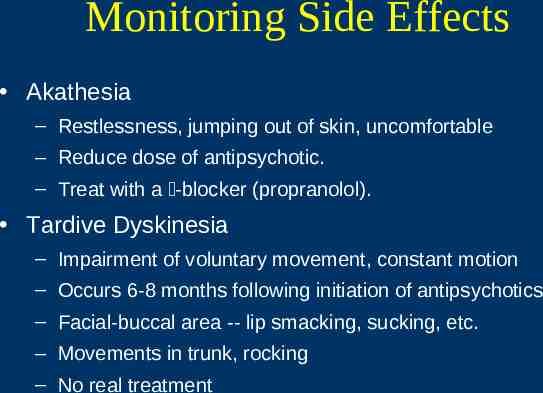
Monitoring Side Effects Akathesia – Restlessness, jumping out of skin, uncomfortable – Reduce dose of antipsychotic. – Treat with a -blocker (propranolol). Tardive Dyskinesia – Impairment of voluntary movement, constant motion – Occurs 6-8 months following initiation of antipsychotics – Facial-buccal area -- lip smacking, sucking, etc. – Movements in trunk, rocking – No real treatment
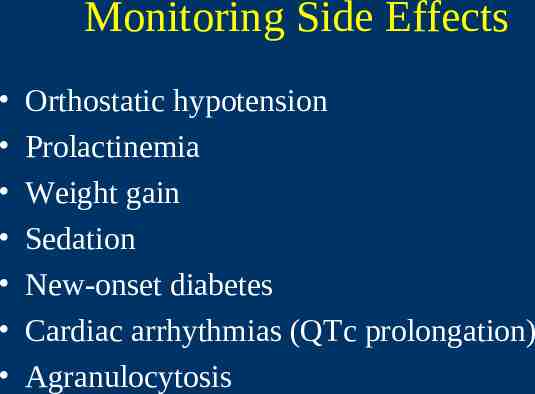
Monitoring Side Effects Orthostatic hypotension Prolactinemia Weight gain Sedation New-onset diabetes Cardiac arrhythmias (QTc prolongation) Agranulocytosis
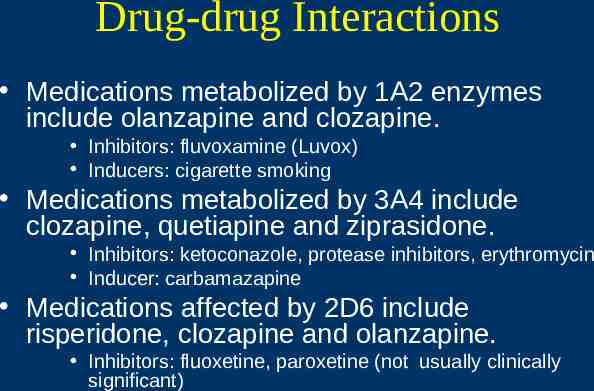
Drug-drug Interactions Medications metabolized by 1A2 enzymes include olanzapine and clozapine. Inhibitors: fluvoxamine (Luvox) Inducers: cigarette smoking Medications metabolized by 3A4 include clozapine, quetiapine and ziprasidone. Inhibitors: ketoconazole, protease inhibitors, erythromycin Inducer: carbamazapine Medications affected by 2D6 include risperidone, clozapine and olanzapine. Inhibitors: fluoxetine, paroxetine (not usually clinically significant)
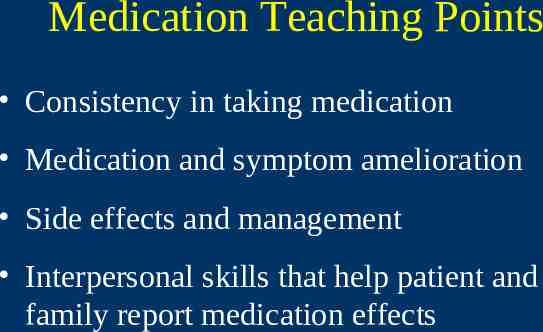
Medication Teaching Points Consistency in taking medication Medication and symptom amelioration Side effects and management Interpersonal skills that help patient and family report medication effects
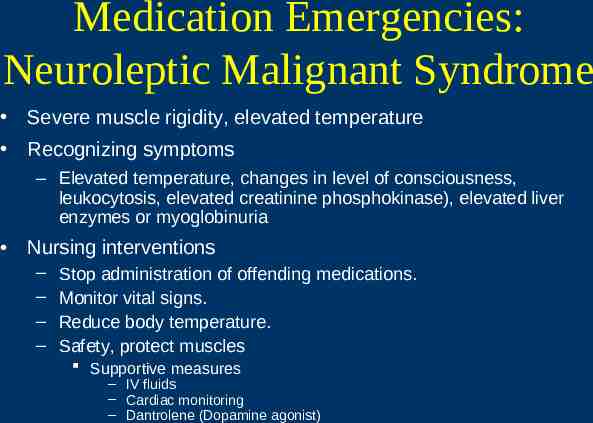
Medication Emergencies: Neuroleptic Malignant Syndrome Severe muscle rigidity, elevated temperature Recognizing symptoms – Elevated temperature, changes in level of consciousness, leukocytosis, elevated creatinine phosphokinase), elevated liver enzymes or myoglobinuria Nursing interventions – – – – Stop administration of offending medications. Monitor vital signs. Reduce body temperature. Safety, protect muscles Supportive measures – IV fluids – Cardiac monitoring – Dantrolene (Dopamine agonist)
Neuroleptic Malignant Syndromes Acute reaction to dopamine receptors blockers Prevalence 2 to 2.4% Death – 4 to 22%, mean 11% Etiology: – Drugs block striatal dopamine receptors; disrupt regulatory mechanisms in the thermoregulatory center in hypothalamus and basal ganglia; heat regulation fails and muscle rigidity
Medication Emergencies: Anticholinergic Crises Potentially life threatening, anticholinergic delirium Can occur in patients who are taking several medications with anticholinergic effects Elevated temperature, dry mouth, decreased salivation, decreased bronchial, nasal secretion, widely dilated eye Stop offending drug, usually self-limiting. May use inhibitor of anticholinesterase, physostigmine.
Anticholinergic Crisis Confusion, hallucinations Physical signs - dilated pupils, blurred vision, facial flushing, dry mucous membranes, difficulty swallowing, fever, tachycardia, hypertension decreased bowel sounds, urinary retention, nausea, vomiting, seizures, coma Atropine flush Hot as a hare, blind as a bat, mad as a hatter, dry as a bone
Treatment Self-limiting – three days Discontinuation of medication Physiostigmine 1-2 mg IV, an inhibitor of cholinesterase, improves in 24-36 hours Gastric lavage Charcoal, catharsis
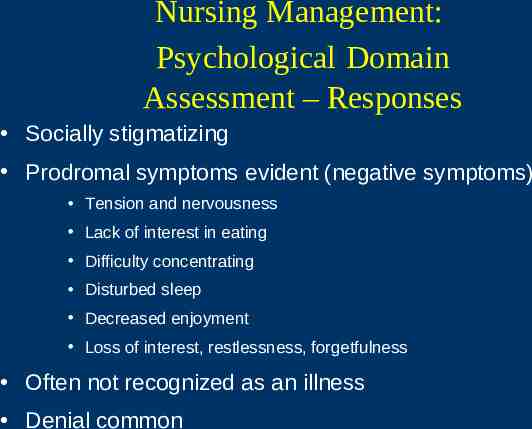
Nursing Management: Psychological Domain Assessment – Responses Socially stigmatizing Prodromal symptoms evident (negative symptoms) Tension and nervousness Lack of interest in eating Difficulty concentrating Disturbed sleep Decreased enjoyment Loss of interest, restlessness, forgetfulness Often not recognized as an illness Denial common
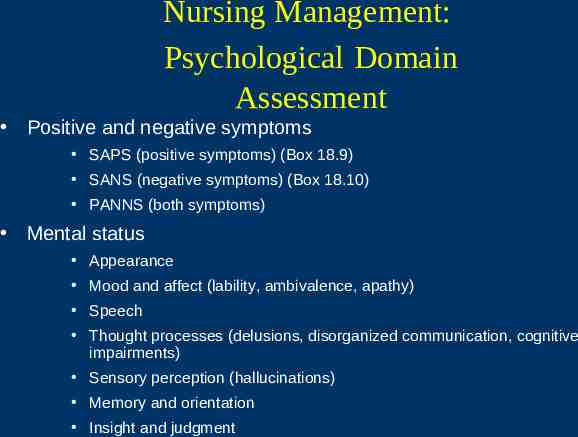
Nursing Management: Psychological Domain Assessment Positive and negative symptoms SAPS (positive symptoms) (Box 18.9) SANS (negative symptoms) (Box 18.10) PANNS (both symptoms) Mental status Appearance Mood and affect (lability, ambivalence, apathy) Speech Thought processes (delusions, disorganized communication, cognitive impairments) Sensory perception (hallucinations) Memory and orientation Insight and judgment
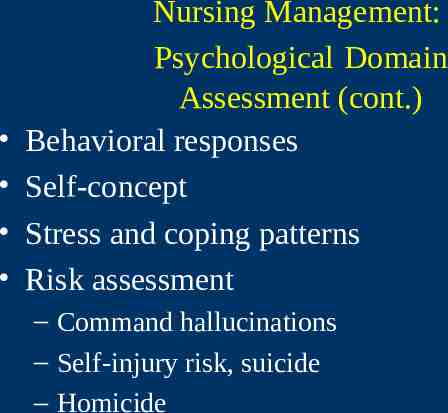
Nursing Management: Psychological Domain Assessment (cont.) Behavioral responses Self-concept Stress and coping patterns Risk assessment – Command hallucinations – Self-injury risk, suicide – Homicide
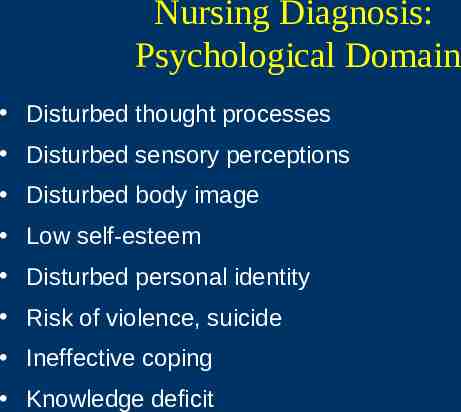
Nursing Diagnosis: Psychological Domain Disturbed thought processes Disturbed sensory perceptions Disturbed body image Low self-esteem Disturbed personal identity Risk of violence, suicide Ineffective coping Knowledge deficit
Nursing Interventions: Psychological Domain Counseling, conflict resolution, behavior therapy and cognitive interventions can be used. Development of nurse-patient relationship – Centers on the development of trust and acceptance of the persons – Critical for optimal treatment of schizophrenia
Nursing Interventions: Psychological Domain – Management of Disturbed Thoughts Assessment content of hallucinations/delusions Outcomes – Decrease frequency and intensity. – Recognize as symptoms of disorder. – Develop strategies to manage recurrence. Experiences real to the patient – Validate that experiences are real – Identify meaning and feeling that are provoked Teach patient that hallucinations and delusions are symptoms of illness.
Nursing Interventions: Psychological Domain Self-monitoring and relapse prevention – Monitor events, time, place, etc. of recurrence of symptoms. – Manage symptoms - getting busy, self-talk, change of activity. (Moller-Murphy Tool) Enhancement of cognitive functioning – Recognize difficulty in processing information. – Improve attention (computer programs, one-to-one). – Help memory (make lists, write down information). – Improve executive functioning-simulation.
Nursing Interventions: Psychological Domain Behavioral interventions – Organize routine, daily activities. – Reinforce positive behaviors. Stress and coping skills development – Counseling sessions – Teach and reward positive coping skills. Patient education – – – – Errorless learning environment Minimal distractions Clear visual aids Skills training
Family Interventions Family support Educate the family regarding lifelong disorder of schizophrenia. Emphasize consistent taking of medication.
Nursing Management: Social Domain Assessment Functional status – Assessed initially and at regular intervals – GAF usually used Social systems – Formal and informal support systems Quality of life Family assessment – Family assessment guide (Ch. 16) – Special consideration to the family where patient is the parent
Nursing Interventions: Social Domain Promotion of Patient Safety Monitoring for potential aggression Administering medication as ordered Reducing environmental stimulation Approach to individual patients – Thorough history of violence – Help patient to talk directly and constructively with those with whom they are angry. – Set limits. – Involve patients in formal contracting. – Schedule regular time-outs.
Nursing Interventions: Social Domain Support groups Milieu therapy Psychiatric rehabilitation Family interventions – Encourage to participate in support groups – Inform about local and state resources – Help negotiate provider system
Continuum of Care Treatment occurs across continuum. Patients are at high risk for getting lost in the system. Inpatient-focused care (stabilization) Emergency care (crisis) Community care (most of care) Mental health promotion