Respiratory System Diseases and Management Part IV Diana
26 Slides2.28 MB
Respiratory System Diseases and Management Part IV Diana Jones Paramedic

Respiratory System Many diseases affect the respiratory system. Covered in this lecture will be Asthma Pneumonia Pulmonary Edema Pulmonary Embolism COPD – chronic bronchitis and emphysema Trauma

Asthma Characterized by inflammation and narrowing of the airways and excess mucus production. Occurs primarily in two stages. Results in difficulty breathing and commonly associated with wheezing.

Asthma Stage II: Inflammatory Response Stage I: Hyper-reactivity Airways constrict and narrow in response to exposure from inhaled allergen or irritant Caused by smooth muscle contraction The airway does not relax and difficulty breathing results Airways swell Fill with fluid Excess mucus production Progress from wheezing to diminished breath sounds Difficulty exhaling – air trapping

Asthma Signs and Symptoms Difficulty breathing Shortness of breath Wheezing or diminished breath sounds Productive cough Cyanosis Tripod position, pursed lips/nasal flaring, accessory muscles, retractions
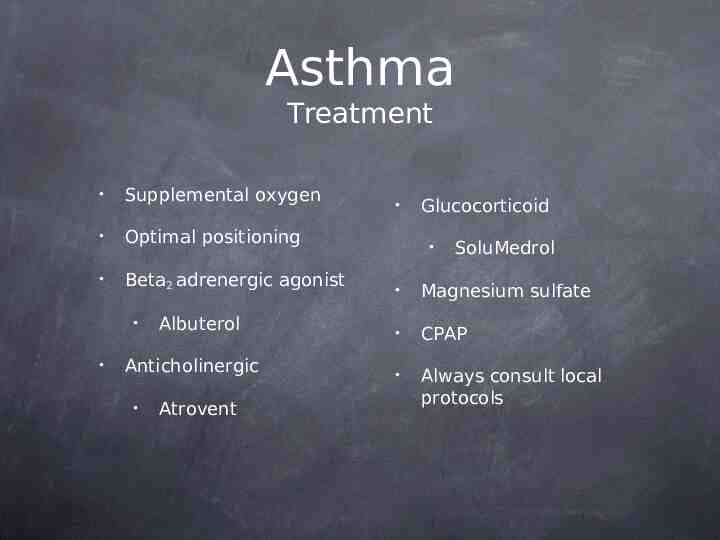
Asthma Treatment Supplemental oxygen Optimal positioning Beta2 adrenergic agonist Albuterol Anticholinergic Atrovent Glucocorticoid SoluMedrol Magnesium sulfate CPAP Always consult local protocols

Pneumonia An infection in the lung that may be caused by bacteria, virus, or fungus

Pneumonia Signs and Symptoms Cough, can be productive resulting in yellowish or greenish sputum Chest pain Shortness of breath Fever Altered mental status Loss of appetite

Pneumonia Treatment Position Supplemental Oxygen Bronchodilators (Albuterol) CPAP IV fluids If febrile, treat Always consult local protocols

Pneumonia *Remember your differential diagnosis* Pneumonia patients have been improperly treated because EMS providers believe they are CHF. What do you think would happen if a pneumonia patient were slammed with Lasix?

Pulmonary Edema Result of excess fluid in the lungs, collecting in the alveoli. Can develop from a number of causes, ranging from high altitude to chemical exposure. However, it is primarily cardiac in origin and what we will consider in this case.

Pulmonary Edema When the heart loses its ability to efficiently pump blood it results in congestive heart failure (CHF). CHF leads to a back up of blood in the veins and this high pressure system causes fluid to be shifted into the lungs

Pulmonary Edema Signs and Symptoms Difficulty breathing Cyanosis Shortness of breath Crackles or rales Tachycardia JVD Tachypnea Edema – pedal Pallor May be hypo or hypertensive Anxiety or restlessness Frothy sputum, can be bloody

Pulmonary Edema Treatment Patient position Supplemental oxygen IV fluid if hypotensive CPAP Consider Nitroglycerin if blood pressure parameters are met Lasix Consider Morphine

Pulmonary Embolism Pulmonary embolism is a blood clot lodged in the lung. Results in a V/Q mismatch. Clot typically originates from another site and migrates to the lung where it lodges.

Pulmonary Embolism What is a V/Q mismatch? To understand you must know the difference between perfusion and ventilation. Ventilation is the mechanical part of breathing, simple act of inhaling and exhaling. A PE does not affect this ability. Perfusion is the delivery of blood. So, in the case of a PE, blood is not delivered to the capillary beds of the alveoli, therefore gas exchange cannot take place. The result is a mismatch. Ventilation continues but perfusion is inhibited.

Pulmonary Embolism Signs and Symptoms Shortness of breath Tachypnea Tachycardia Chest pain that may migrate Anxiety/restlessness Cough, maybe bloody sputum

Pulmonary Embolism Treatment Patient position Supplemental oxygen IV access The main goal of field treatment is oxygenation and transport. Definitive care is provided by the hospital with rapid diagnosis and dissolving of the clot You may consider an anxiolytic if protocol allows

Chronic Obstructive Pulmonary Disease Umbrella term which includes chronic bronchitis and emphysema. By either mechanism, the result is decrease air flow.

COPD Chronic Bronchitis Airways are thick and inflamed Airways are clogged with excessive mucus production “Blue Bloaters”

COPD Emphysema Walls of alveoli become floppy Walls of alveoli may be destroyed Alveoli collapse “Pink Puffers”

COPD Regardless of the underlying cause of COPD, the result is the same. Decreased surface area for gas exchange. COPD is progressive and treatment is aimed at symptom management.

COPD Signs and Symptoms Shortness of breath Difficulty breathing Chronic cough Clubbing of fingers Cyanosis Wheezing Frequent infections

COPD Treatment Patient position Supplemental oxygen Bronchodilators Anticholinergics Glucocorticoid

Trauma The respiratory system can also be affected by trauma. Injury can lead to Pneumothorax Hemothorax Hemopneumothorax These will all be considered in a different lecture

Questions?