Rapid Sequence Intubation Drugs Ryan J. Fink, MD Raquel Bartz, MD Duke
30 Slides362.11 KB
Rapid Sequence Intubation Drugs Ryan J. Fink, MD Raquel Bartz, MD Duke University Medical Center Dept. of Anesthesiology
Learning Objectives At the completion of this module the learner should be able to: – Choose the appropriate induction agent and neuromuscular blocking agent for a given clinical situation – Calculate the appropriate dose of both induction agent and paralytic for a given patient and clinical situation – Understand relative and absolute contraindications for induction agents and paralytics – Choose the appropriate vasopressor if blood pressure decreases after induction/intubation
Administration of General Anesthetics for Rapid Sequence Intubation
Induction Agents: General Principles Choice of agent dependent on: – Clinical status of the patient – Clinicians familiarity with the agent Timing - Anesthetic agent should: – Have time to take effect – Be given before paralysis
Induction Agents: General Principles Primary concerns for agent choice: – Hemodynamic stability and risk of hypotension – Risk of additional respiratory depression – ICP and cerebral perfusion – History of ischemic heart disease – Rapidity of effect Secondary concerns for agent choice: – Amnestic properties – Emetic properties – Desired duration of effect
Induction Agents: General Principles Do no attempt intubation under suboptimal conditions! Patient is ready for intubation when: – Apneic – Unresponsive (no lid reflex) – Jaw is relaxed and mobile
Ideal Induction Agent - Promote amnesia - Hemodynamic stability - Short-acting - Minimal Side Effects - Reversible - Metabolized independent of liver or kidney

Potential Induction Agents Etomidate Propofol Ketamine
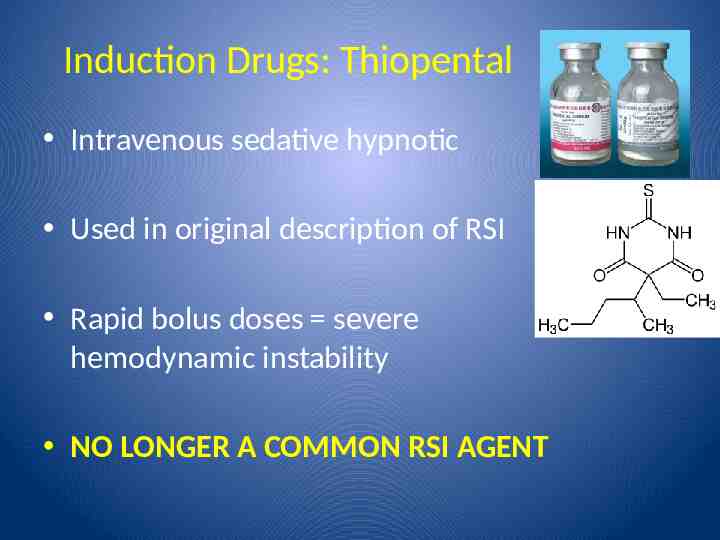
Induction Drugs: Thiopental Intravenous sedative hypnotic Used in original description of RSI Rapid bolus doses severe hemodynamic instability NO LONGER A COMMON RSI AGENT
Induction Agents: Etomidate Intravenous anesthetic Short-acting Hemodynamic response: – Minimal CV depression No major contraindications – Relative CI: adrenal insufficiency No analgesic activity
Induction Agents: Etomidate Intubating Dose: – 0.1 -0.2 mg/kg – i.e. 70 kg pt 7 - 14 mg Onset of Action: 1 min (one arm-brain circulation) T1/2: 10 – 20 min Hypnosis (duration of action): 3 - 5 min Side effects: – Myoclonus; burning – Nausea/vomiting – Reduce dose in the elderly – Adrenal suppression (inhibition of 11-beta-hydroxylation reduced cortisol and aldosterone)
Induction Drugs: Propofol Intravenous anesthetic Short-acting Hemodynamic response: SVR, contractility, and preload often leading to BP No analgesic activity Contraindications: Hypotension, hypovolemia
Induction Drugs: Propofol Intubating Dose: – 1 - 2 mg/kg – i.e. 70 kg pt 70 – 140mgmg Onset of Action: 1 min (one arm-brain circulation) Hypnosis (duration of action): 3 - 5 min T1/2: 3 – 12 hours (due to release from fat stores) Side effects: – Burning at injection site – Some anti-emetic effect
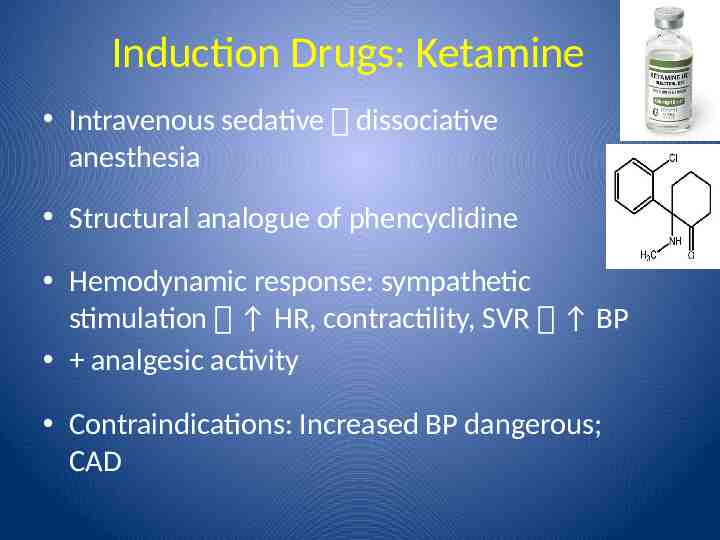
Induction Drugs: Ketamine Intravenous sedative dissociative anesthesia Structural analogue of phencyclidine Hemodynamic response: sympathetic stimulation HR, contractility, SVR BP analgesic activity Contraindications: Increased BP dangerous; CAD
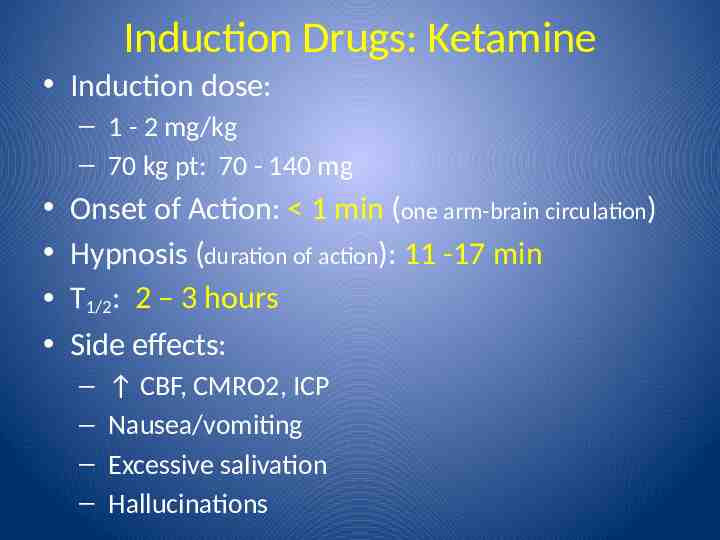
Induction Drugs: Ketamine Induction dose: – 1 - 2 mg/kg – 70 kg pt: 70 - 140 mg Onset of Action: 1 min (one arm-brain circulation) Hypnosis (duration of action): 11 -17 min T1/2: 2 – 3 hours Side effects: – – – – CBF, CMRO2, ICP Nausea/vomiting Excessive salivation Hallucinations
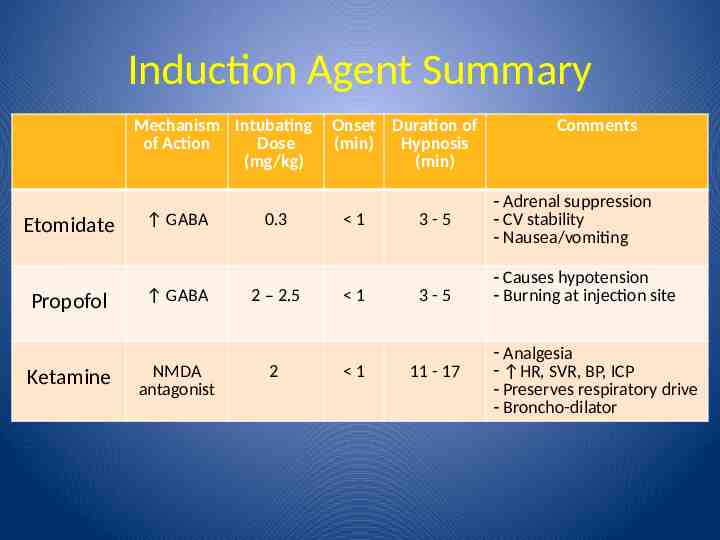
Induction Agent Summary Mechanism Intubating of Action Dose (mg/kg) Etomidate Propofol Ketamine GABA GABA NMDA antagonist 0.3 2 – 2.5 2 Onset Duration of (min) Hypnosis (min) 1 1 1 3-5 3-5 11 - 17 Comments - Adrenal suppression - CV stability - Nausea/vomiting - Causes hypotension - Burning at injection site - Analgesia - HR, SVR, BP, ICP - Preserves respiratory drive - Broncho-dilator
Neuromuscular Blocking Agents for Rapid Sequence Intubation
Neuromuscular Blocking Agents Advantages: – forceful regurgitation of gastric contents – Relaxation oral-pharyngeal muscles Easy distraction of mandible and tongue Disadvantages: – Apnea – Oral-pharyngeal soft tissue collapse Available agents: – Succinylcholine – Rocuronium
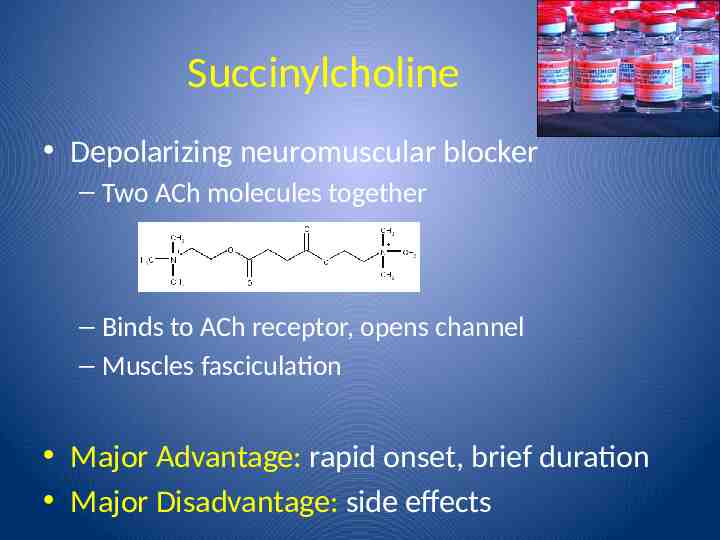
Succinylcholine Depolarizing neuromuscular blocker – Two ACh molecules together – Binds to ACh receptor, opens channel – Muscles fasciculation Major Advantage: rapid onset, brief duration Major Disadvantage: side effects
Succinylcholine Intubating dose: 0.6 – 1 mg/kg IV – 70 kg pt: 42 - 70 mg Onset of action: 30 – 60 seconds T ½: 10 – 15 minutes Metabolism: Plasma cholinesterase – 96% of pts have normal enzyme – Prolonged duration w/ atypical gene – Prolonged duration w/ conditions that PC Liver disease Pregnancy
Succinylcholine: Side Effects Bradycardia in adults after 2nd dose K ( 0.5 – 1.0 mEq/L) ICP Intraocular pressure Intra-gastric pressure Lower esophageal sphincter tone muscle tone in pts w/ myotonia congenita or dystrophica Myalgias
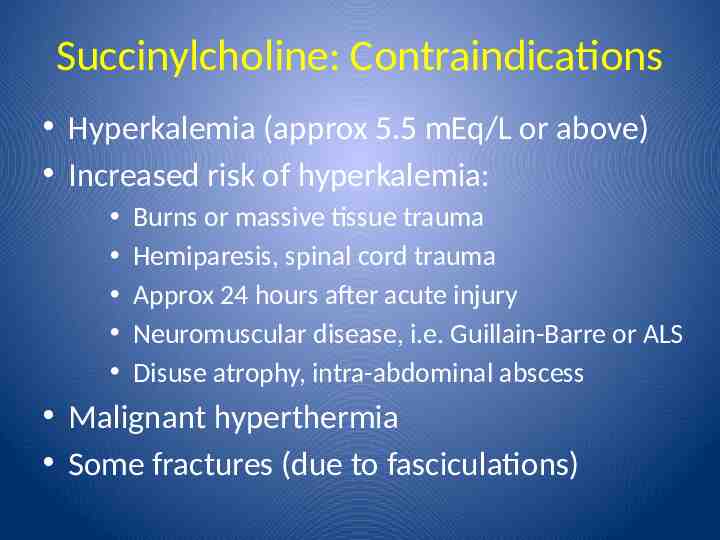
Succinylcholine: Contraindications Hyperkalemia (approx 5.5 mEq/L or above) Increased risk of hyperkalemia: Burns or massive tissue trauma Hemiparesis, spinal cord trauma Approx 24 hours after acute injury Neuromuscular disease, i.e. Guillain-Barre or ALS Disuse atrophy, intra-abdominal abscess Malignant hyperthermia Some fractures (due to fasciculations)
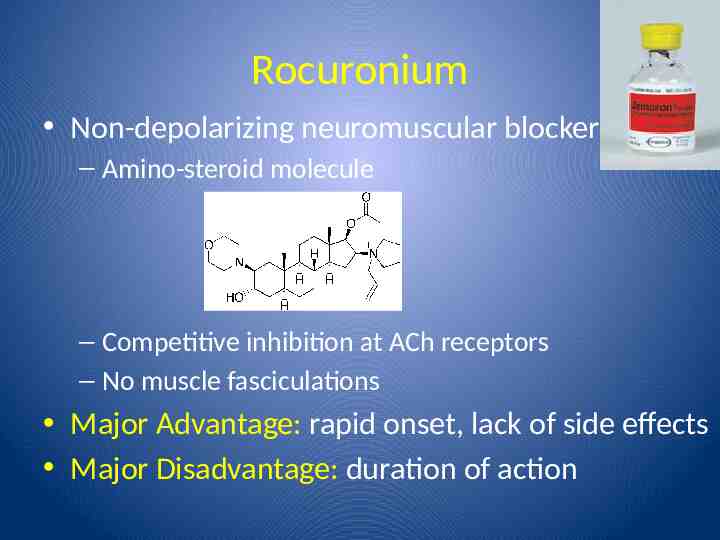
Rocuronium Non-depolarizing neuromuscular blocker – Amino-steroid molecule – Competitive inhibition at ACh receptors – No muscle fasciculations Major Advantage: rapid onset, lack of side effects Major Disadvantage: duration of action
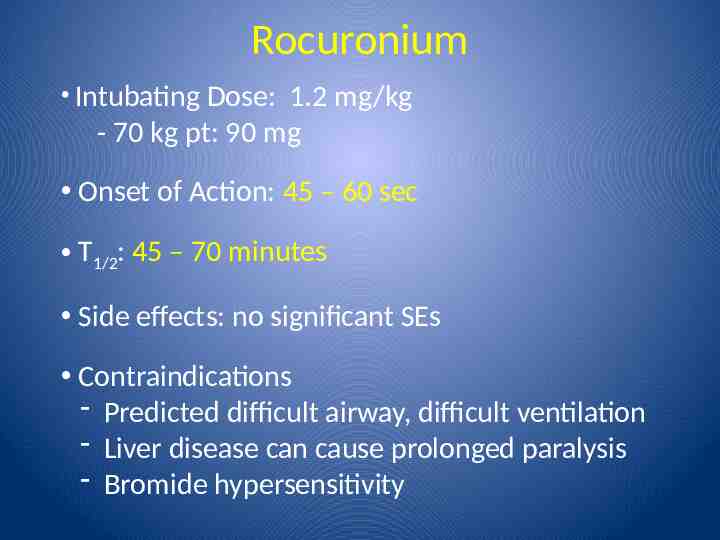
Rocuronium Intubating Dose: 1.2 mg/kg - 70 kg pt: 90 mg Onset of Action: 45 – 60 sec T1/2: 45 – 70 minutes Side effects: no significant SEs Contraindications - Predicted difficult airway, difficult ventilation - Liver disease can cause prolonged paralysis - Bromide hypersensitivity
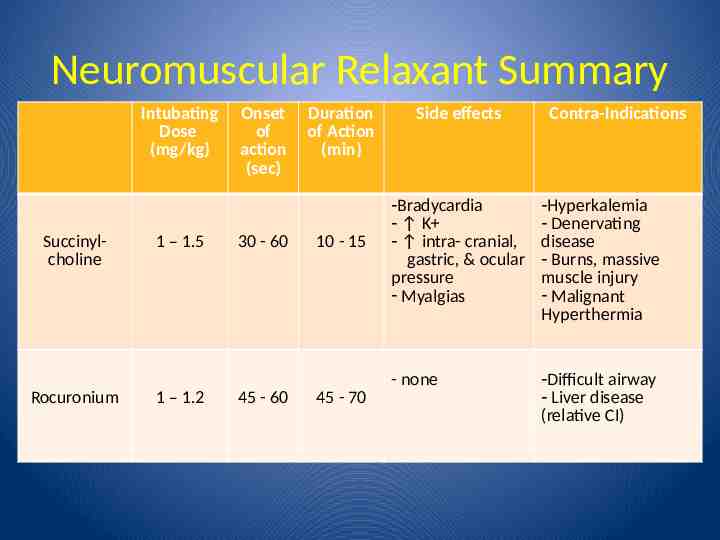
Neuromuscular Relaxant Summary Intubating Dose (mg/kg) Succinylcholine Rocuronium 1 – 1.5 1 – 1.2 Onset of action (sec) 30 - 60 45 - 60 Duration of Action (min) 10 - 15 45 - 70 Side effects Contra-Indications -Bradycardia - K - intra- cranial, gastric, & ocular pressure - Myalgias -Hyperkalemia - Denervating disease - Burns, massive muscle injury - Malignant Hyperthermia - none -Difficult airway - Liver disease (relative CI)
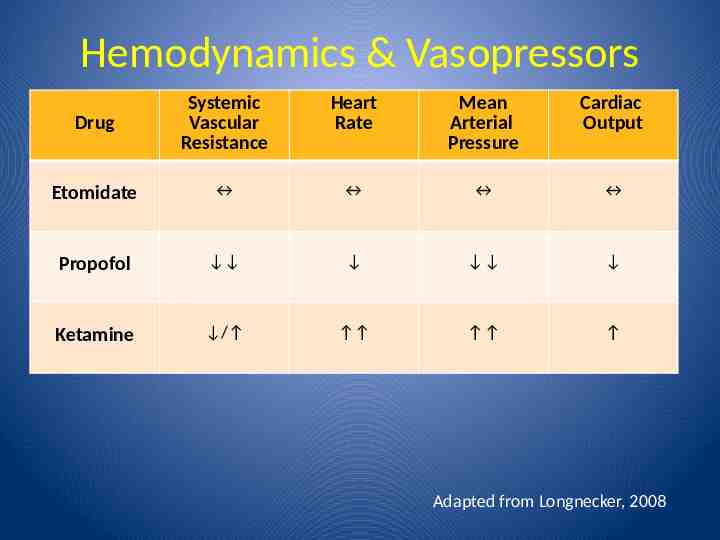
Hemodynamics & Vasopressors Drug Systemic Vascular Resistance Heart Rate Mean Arterial Pressure Cardiac Output Etomidate Propofol Ketamine / Adapted from Longnecker, 2008
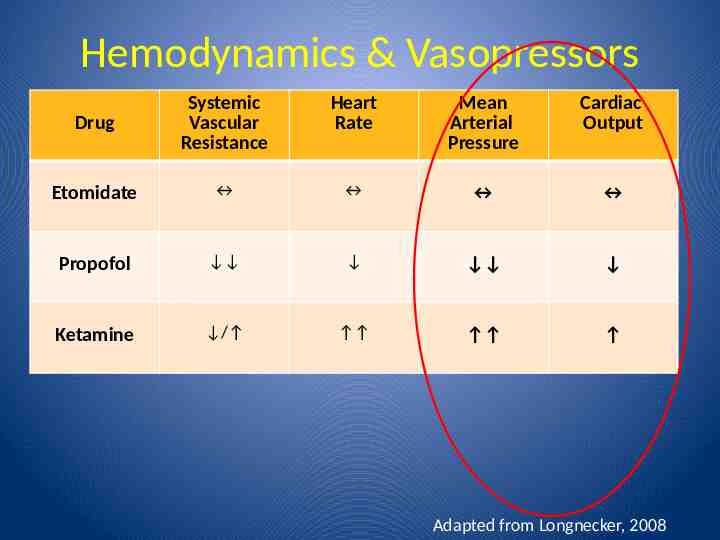
Hemodynamics & Vasopressors Drug Systemic Vascular Resistance Heart Rate Mean Arterial Pressure Cardiac Output Etomidate Propofol Ketamine / Adapted from Longnecker, 2008
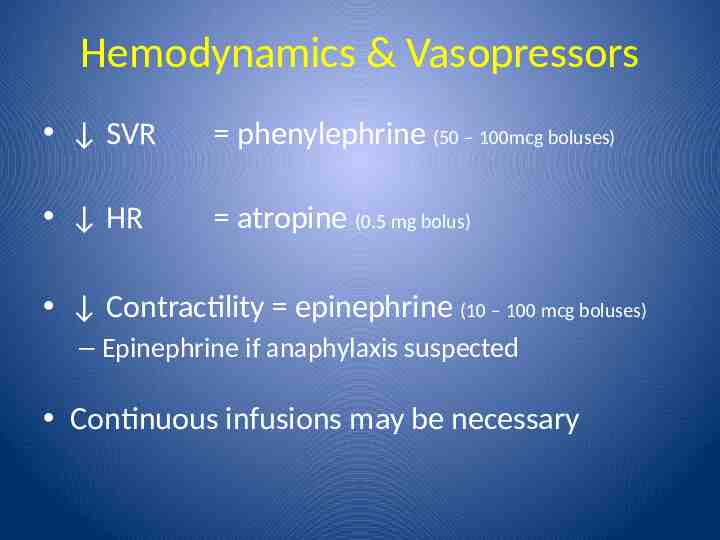
Hemodynamics & Vasopressors SVR phenylephrine (50 – 100mcg boluses) HR atropine (0.5 mg bolus) Contractility epinephrine (10 – 100 mcg boluses) – Epinephrine if anaphylaxis suspected Continuous infusions may be necessary
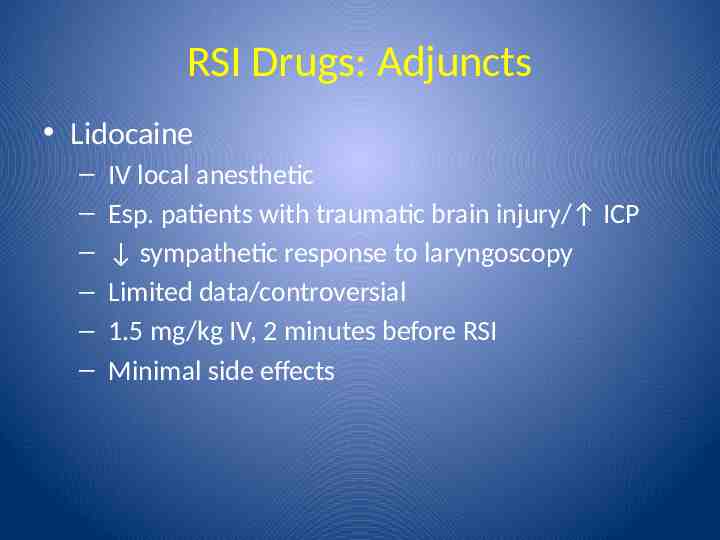
RSI Drugs: Adjuncts Lidocaine – – – – – – IV local anesthetic Esp. patients with traumatic brain injury/ ICP sympathetic response to laryngoscopy Limited data/controversial 1.5 mg/kg IV, 2 minutes before RSI Minimal side effects
Rapid Sequence Induction Drugs: Summary Main drug classes for RSI – General anesthetic – Neuromuscular blocking agent – Vasopressor – Possibly lidocaine (for brain injury patients) Choice of drug depends on: – Clinical situation and patient co-morbidities – Clinical judgment