Quarterly Provider Office Staff Meeting March 3, 2021
40 Slides274.60 KB
Quarterly Provider Office Staff Meeting March 3, 2021 Physicians, Hospitals and Health Plans working together for the patient

Agenda Introductions Overview Department Process Review Updates Questions

Introductions Sonya Araiza, CEO Michael Swartout, MD – Medical Director Carl Constantine, MD – Associate Medical Director Veronica Vasquez, CIO/COO Linda Viles, CFO Dione Webster, Director of Operations, Payer Risk Management (Provider Relations, Contracting, Customer Service) Anastajia Navarro, Supervisor, Provider Network Development (Provider Relations/Contracting) Lisa Macias, Supervisor, Customer Service Lisa Tran, Provider Relations Brandee Ball, Provider Relations Arlene Prado, Provider Relations/Contracting Jeremiah Chandler, Contracting Kimberly Baldwin, BSN, RN, Director of Health Services Brianne Rodriguez, RN, Manager, Utilization Management Cecille Luna, LVN, Manager, Case Management Linda Lopez, Supervisor, Case Management Jamie Schaub, Supervisor, Utilization Management Stephanie Eugenio, Controller Bret Trubey, MBA, Financial Analyst Mary Berlin, Claims Manager Robin Grimm, RN, Manager, Quality Management Traci Mackey, Credentialing & Compliance Supervisor Andrea Barrios, EDI Supervisor Armina “Nina” Huzbasic, Manager, IT Apps & Analytics Anissa Campos, IT Applications Manager, Clinical Programs Karen Sauer, Marketing

Contracting New Providers CV and Letters of Interest (LOIs) to be sent to [email protected] LOI must include office location and hours, provider degree, provider specialty and limitations, if any Provider Status Change (i.e., leave of absence, terminations, demographic changes, tax ID change, etc.) Send to [email protected]

Contracted Health Plans Commercial Plans: Aetna Anthem Blue Cross Blue Shield (including TRIO product) Health Net United Healthcare Senior Plans: Alignment Anthem Blue Cross Blue Shield Central Health Plan Humana SCAN United Healthcare

Customer Service Contracted providers are to use EZ-NET portal for claim and auth inquiries prior to Customer Service outreach Customer Service documents calls; incident remains open until resolution is made Telephone Numbers: Provider Line: (805) 604-3308 Member Line: (805) 604-3332 Customer Service Center Hours: Monday-Thursday 8a-5p; Friday 9a-5p Customer Service Support: Authorizations - Authorization extensions; submit request via email to [email protected] (only applicable to authorizations not yet expired and not previously been extended) Claims - direction on who to bill; claim status Eligibility – Eligibility should be reviewed through the health plan websites directly. Member adds or issues should be reported to Customer Service. Member bills - Customer Service team to obtain copies of member bills and forwards to IPA Provider Relations team to work with provider to resolve issue (incident remains open until resolution is made) Provider network questions

Provider Relations The Provider Relations team provides support to educate the network on policies/procedures, perform office training, assist providers with EZ-NET set up and work as a liaison between IPA Departments for escalated issues or trends. Email: [email protected] Your PR Team: Lisa Tran & Brandee Ball VCIPA Website & Provider Portal: The site contains important memos, network information, provider rosters, UM guidelines, COVID-19 information, Health Plan website links, clearing house information, fee schedule & payment policies, various forms, provider manual, etc. Website: www.valleycareipa.com Log in information: User: vcipa Password: vcprovider EZ-NET: Quick link is available on the Valley Care Website Each employee needs unique log-on For access, email [email protected] Provides status of claims, authorizations and for PCPs to submit referral requests

Primary Care Physicians, Specialty Network, Urgent Care & After Hour Care Provider rosters can be found on the Valley Care IPA website. PCP: https://valleycareipa.com/valley-care-ipa-primary-care-physicians.html Specialty Network: https://valleycareipa.com/valley-care-ipa-specialty-care-physicians.html Urgent Care Locations: Valley Care IPA has “10” contracted urgent care locations available to members. For the most current list, please visit the website at: https://valleycareipa.com/affiliated-health-plans-and-hospitals.html#urgent -care-centers After Hours Care: Members can obtain after hours care through an affiliated urgent care or a hospital emergency room. Participating hospitals with Valley Care IPA are: Community Memorial Hospital, Ventura County Medical Center, Santa Paula Hospital, St. John’s Regional Medical Center & St. John’s Pleasant Valley Hospital
Urgent Care Process Members can access urgent care without a prior authorization outside of normal business hours (before 8a or after 5p M-F or anytime Sat and Sun). If a member presents to an urgent care during normal hours, the Urgent Care contacts Valley Care IPA requesting an authorization. Below are the steps that take place: UM team reviews for medical necessity. If medically necessary, UM issues authorization. If not deemed urgent in nature, UM requests the Provider Relations Department to contact the member’s PCP to identify appointment availability. Provider Relations must provide feedback to UM within 30 minutes of request. If Provider Relations is unable to get a response from the office, PCP will be potentially cap deducted for the urgent care visit. If PCP can accommodate, the Urgent Care is notified and member is redirected to their PCP office. If PCP cannot accommodate, the UM team issues an authorization and the PCP is set up for potential cap deduct. County assigned members may access County urgent cares during normal business hours without a prior authorization; this will be considered covering PCP services.

Laboratory & Radiology Providers Laboratory: Valley Care IPA’s capitated laboratory is Quest Diagnostics. For a current listing of Quest draw sites, please visit the website at: https://valleycareipa.com/laboratories.html Radiology: Valley Care IPA is capitated with two different radiology providers. 1. County of Ventura (for members assigned to a County Primary Care Physicians) 2. County PCPs are identified in the system as having “VCMC” after provider’s last name (i.e., Lyons (VCMC), Morgan) – and can be identified as such on the provider roster Beverly Radiology aka RadNet (for members not assigned to a County Primary Care Physicians For a current listing of radiology locations, please visit the website at: https://valleycareipa.com/radiology-valley-care-ipa.html
Behavioral Health Valley Care IPA is not delegated to manage behavioral health, effective 1/1/19, with the exception of Anthem Blue Cross Senior. Members other than Anthem Blue Cross Senior must be directed to the health plan to access the Plans carve-out network. Anthem Blue Cross Seniors should continue to be submitted to VCIPA for behavioral health services.

Eligibility Eligibility Eligibility Team membership verifies and provided update the records from Membership loaded intoeach EZCAP/EZNET each health continuously plan month month New for 2021 – Blue Shield Trio Plan All Blue Shield members who are patriciate with a TRIO Plan (non-exchange) will have an EZ-Alert#2 added to their account. ( MEMBER IS ASSIGNED TO BLUESHIELD TRIO PLAN. BLUESHIELD TRIO PLANS ARE CURRENTLY EXCLUDED FROM THE DIRECT REFERRAL AND INTERNAL PROCESSING. UM TO REVIEW PROVIDER NOTES FOR FINAL DETERMINATION). Blue Shield members who are patriciate with Exchange plans are on a month to month premium plan. Members who have not paid their monthly dues will enter into a grace period. Once the member enters the second month of the grace period and dues are still not paid, the member will be termed in EZ-NET on the last day of the month following the month of dues not paid. See below example (once member pays their dues, they will be reinstated.

Referral/Authorization Process All routine referrals go through the PCP for submission into the EZ-NET system, with exception of the following: Continuation of DME, Oxygen, Tertiary Care, Total OB or Behavioral Health (these can be submitted directly to the IPA via fax at (805) 278-6815) Urgent & STAT referrals must be called into the UM Department: (805) 918-4179 Urgents must be called in by PCP; STATs can be called in by specialist or PCP PCP & specialist upload all supporting documentation into the EZ-NET system County County providers are entered as an internal referral and most are autoapproved upon submission – priority status “0” in EZNET (REMINDER: County PCPs are identified in system as having “VCMC” after their last name; some County providers excluded from internal referral) – new document will be available and shared soon identifying County providers included in the Internal Referral Program Contracted providers can view authorization status by logging into the EZ-NET system IMPORTANT: Providers are encouraged to review submitted referrals daily for potential pends and additional information requests. The UM team no longer places call outs for additional information.

Referral/Authorization Process – cont’d If change requests are needed on an existing referral, the Authorization Inquiry Form must be used and submitted directly to the UM team for processing. This form is on the VCIPA website. Form should uploaded to EZ-NET and emailed to the UM team (email address provided on the form). Inquiries can be submitted by PCP and specialty offices; please avoid submitting multiple inquiries for same issue by same office staff. Contracted specialists are required to obtain authorizations for continuing care prior to services being rendered. Requests must be sent to the PCP to submit to the IPA via EZ-NET. PCPs are required to submit the specialist requests to the IPA via EZNET within 2-business days of receipt. Specialists should be checking EZ-NET 2-days after submission to PCP to ensure auth was entered. If not entered, specialist to follow up with PCP office. If PCP office is unresponsive, please advise [email protected].
Referral/Authorization General Rules Members seen in the ER require PCP follow up prior to being referred back to an attending specialist. If need is urgent or STAT in nature, those referral requests need to be called into the Urgent/STAT Huntline. Otherwise, PCP to see member, then submit for referral as indicated. PCPs must sign ALL referral submissions (electronic signatures accepted) If a member is out of network and PCP is wanting to refer back into network, a chart note signed by the PCP is required when submitting for the referral. This will avoid cancelled referrals. Submission of a referral to a specialist requires PCP signature

Referral/Authorization Turn Around Times Referral processing timeframes are as follows: Routine: Commercial: 5 days business days 45 days if missing information to make a decision Senior: 14 calendar days Urgent: 72 hours (medically urgent indications only; not scheduling reasons) STAT: 24 hours Drugs: 24 hours It is recommended to schedule member once authorization is approved. Once a referral has been finalized, it’s set to fax out to the requesting provider, rendering provider and member’s PCP (and facility, if one exists on the auth). Faxes are generated every three (3) hours. Real-time status can be obtained via the EZ-NET system.

Utilization Review/Authorization Tips Attach documentation that supports the authorization request (upload via EZ-NET) Diagnosis entered must support the service being requested Referral Form is complete and identifies what is being requested and why Submit authorizations with turn-around-times considered; upgrading the request to urgent status due to scheduling purposes is not appropriate Pended auths – viewable in EZ-NET for quicker response time; the sooner we receive the needed information, the sooner your request will be processed Prevent Cancelled Authorizations! Be sure physician has signed and all required elements are provided with supporting documentation!
Urgent/STAT Requests Expedited/urgent reviews will be performed for sensitive situations when the routine review timeframe could seriously jeopardize the life or health of the member’s ability to regain maximum function. Examples: 1. Member’s need for treatment is imminent due to the emergent or urgent nature of the illness, injury or condition requiring the treatment 2. Member has a life or limb threatening condition 3. Routine review would seriously jeopardize the life or health of the member or would jeopardize the member’s ability to regain maximum function
Urgent/STAT Huntline Urgent/STAT Line: (805) 918-4179 Not to be used for inquiries on referral status, provider to use EZ-NET for auth and claim status The Urgent/STAT Huntline is often used as a direct line to Utilization Review – that is not the purpose of this phone line Callers without Urgent or STAT authorization requests will be directed back to Customer Service for appropriate call handling Messages left on the Urgent/STAT line are transcribed into an email for the UM Coordinators within 10 minutes of the message being left.

Direct Referral Program Valley Care IPA has several specialties on the Direct Referral Program. What this means is a Primary Care Physician can submit for an authorization for a provider specialty on the Direct Referral Guideline for the specified type of service and the authorization will auto-approve upon submission Direct Referral Guidelines can be found under the Provider Portal on the Valley Care IPA website Be sure when submitting referral for a provider under the Direct Referral Program that you flag the referral with Priority Status “0”

Case Management Inpatient concurrent review of: Hospital Admissions Skilled Nursing Facility Admissions Durable Medical Equipment (DME) Authorization Reviews Transition Care Measures Coordinate discharge needs with Care Coordination Participates in Interdisciplinary Team Meetings with the Health Plans and Medical Directors to address gaps in care and follow up needs

Care Coordination Care Coordination Team: Doug McClatchey, RN Liza Torres, MA, Health Coach Joanna Cardenas, Social Worker Care Coordination follows member outpatient to address: Gaps in Care Chronic Disease Management Healthcare Navigation PCP Coordination Hours of operation are M-F 8a-5p Care Coordination Referrals may be received via fax, secure email, shared electronic medical record (EMR), telephonically by providers, care managers, payer sources or direct member referral. Direct Line: (805) 918-5299 Direct Fax: (805) 856-0385 Email: [email protected]

Quality Management Responsible for writing denial letter language per MDR Investigates appeals & grievances Health Plan audits Compliance

Quality Management – cont’d Commercial Non-Emergent Medical Appointment Access Standards Appointment Type Time-Elapsed Standards Urgent Care appointments that require prior authorization (PCP) do not Must offer the appointment within 48 hours of request Urgent Care appointments with SCP that require prior authorization Must offer the appointment within 96 hours of request Non-Urgent Care appointments for Primary Care (PCP) Must offer the appointment within 10 business days of the request Non-Urgent Care appointments Specialists Physicians (SCP) Must offer the appointment within 15 business days of the request with Non-Urgent Care appointment with nonphysician mental health provider Within 10 business days of the request Non-Urgent Care appointments for ancillary services (for diagnosis or treatment of injury, illness or other health condition) Must offer appointment within 15 business days of the request In-office wait time for appointments (PCP and SCP) Not to exceed 15 minutes First prenatal visit Well-child visit Wellness check scheduled Within 10 business days of request Within 10 business days of request Within 30 calendar days of request

Quality Management – cont’d Senior Non-Emergent Medical Appointment Access Standards Appointment Type Time-Elapsed Standards Urgent Care appointments that require prior authorization (PCP) do not Must offer the appointment within 48 hours of request Urgent Care appointments with SCP that require prior authorization Must offer the appointment within 96 hours of request Urgent Care appointment with physician mental health provider Within 10 business days of request. non- Non-Urgent Care appointments for Primary Care (PCP) Must offer the appointment within 10 business days of the request Non-Urgent Care appointments Specialists Physicians (SCP) Must offer the appointment within 15 business days of the request with Non-Urgent Care appointment with nonphysician mental health provider Within 10 business days of the request Non-Urgent Care appointments for ancillary services (for diagnosis or treatment of injury, illness or other health condition) Must offer appointment within 15 business days of the request In-office wait time for appointments (PCP and SCP) Not to exceed 30 minutes Wellness check scheduled Within 30 calendar days of request

Quality Management – cont’d Behavioral Health Emergent & Non-Emergent Appointment Access Standards Appointment Type Time-Elapsed Standards Non-Urgent appointments for with a mental health care provider Must offer the appointment business days of the request Non-Urgent Care appointments with a nonphysician mental health care provider Must offer the appointment within 100 business days of the request Urgent Care appointments Must offer the appointment within 48 hours of request Access to Care for Non-Life Threatening Emergency Within 6 hours Access to Life-Threatening Emergency Care Immediately Access to Follow Up Care Hospitalization for mental illness One follow-up provider within Plus One follow-up provider within after within 10 encounter with a mental health 7 calendar days after discharge encounter with a mental health 30 calendar days after discharge
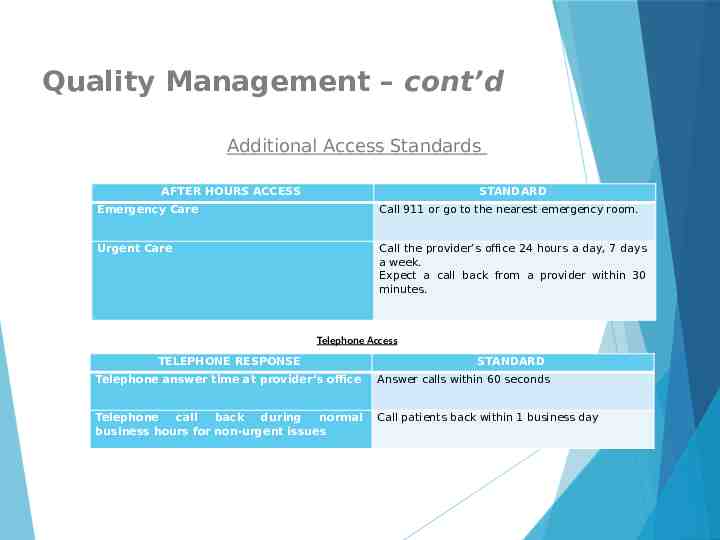
Quality Management – cont’d Additional Access Standards AFTER HOURS ACCESS STANDARD Emergency Care Call 911 or go to the nearest emergency room. Urgent Care Call the provider’s office 24 hours a day, 7 days a week. Expect a call back from a provider within 30 minutes. Telephone Access TELEPHONE RESPONSE STANDARD Telephone answer time at provider’s office Answer calls within 60 seconds Telephone call back during normal business hours for non-urgent issues Call patients back within 1 business day

Claims Claim status, payment information and/or denials can be viewed by a contracted provider via the EZ-NET system. Standard claims processing timeframe is 60-days, but IPA processes 98% of clean claims within 30 days. Providers are encouraged to submit claims electronically via Office Ally: Clearinghouse: www.OfficeAlly.com Payer ID: VCIPA Contact Information: [email protected] / telephone (866) 575-4120 Practice may use alternate clearinghouse, but must use payer ID VCIPA to route claims to Valley Care IPA for processing.

Finance Claims payments All claim payments are processed by ECHO Health, Inc. www.providerpayments.com Available documents: RA 1099s EOB Payment Options – contact ECHO to change payment method @ (866) 686-3260 Virtual Credit Card (default payment) EFT Paper check MPX (formerly MedPay) Printable check (e-check) Capitated Provider Payments Coming Soon! ACH electronic payments Payment details to be emailed Vendor ACH Form needed for setup Confirm email address for payment detail Attach a VOID check to ensure correct account number

New Members Welcome Letters are mailed to members new to IPA. They are encouraged to contact their PCP to be seen within 90-days of enrollment Members are directed to the IPA Website for important information (i.e., provider rosters, urgent care facilities, lab and radiology locations, etc.) New Member Packets are available upon request for members without internet or computer access If member requires coordination of care for a previously established specialty provider, provider is to contact the UM team and the UM team works directly with the Plan to facilitate coverage PCP assignment changes or demographic changes should be made directly with health plan

Incentives/Quality Program Primary Care Physicians: Annual Wellness Visits (AWV) – Medicare Advantage members HCC Recapture – Medicare Advantage members Quarterly/Monthly Reports Care Gap Reports All Physicians: CAHPS Survey – New – Webex Trainings Coming Soon! Getting needed care Care Coordination Doctor/Patient Conversations Prescriptions

Updates

Marketing Covered California Special Enrollment Period (SEP) Extension – Feb 1 through May 15 Information will be posted to the VCIPA website Health Plan Broker Update Community Sales IPA Coordination Health Plan News Alignment Anthem Blue Shield Central Health Humana SCAN United Healthcare

COVID-19 Various sites are performing vaccine clinics. These are available through the County of Ventura (Public Health) and through some IDMG clinics. CDC posts updates on the following site to keep the community apprised on the eligible age groupings: www.venturacountyrecovers.org

Resources

Health Education, Community Health Centers & Social Services Health Education: Valley Care IPA partners with various community centers that offer health education Community Health Centers & Social Services: Camarillo Healthcare District (adult daycare, sponsored and private pay): https://www.camhealth.com/ or (805) 388-1952 Senior Concerns (currently virtual only; align seniors with care giving, meals on wheels): https://www.seniorconcerns.org/ or (805) 497-0189 Focus on Seniors: (805) 322-8822 Ventura County Homecare Association: http://vchainc.org/ or (805) 363-2533 Alzheimer Association (AA): https://www.alz.org/cacentralcoast or (805) 494-5200 American Red Cross (ARC): https://www.redcross.org/local/california/central-california/about-us/locations/pacific-coast.html ?CID organic gmb listings or (805) 987-1514 Cancer Support Community: https://www.cancersupportvvsb.org/ or (805) 379-4777 Social Services: Adult daycare, health and awareness, food share (weekly), reasonably priced senior lunches ( 2-5), health fairs throughout the year, coordinate DME services and assisted living, supportive nursing services, health education for debilitating diseases and how to function through these, ARC helps with re-housing during disasters, AA offers respite care, etc. Transportation is offered through Camarillo Healthcare District via bus

Starbucks Drawing – Question #1! Who can call in Urgent & STAT referral requests?

Starbucks Drawing – Question #2 Name our two capitated Radiology Provider groups for County assigned members and non-County assigned members.

Starbucks Drawing – Question #3! What is the group email address for Provider Relations?

Questions?