NHS Continuing Healthcare Strategic Improvement Programme CHC
6 Slides555.11 KB

NHS Continuing Healthcare Strategic Improvement Programme CHC SIP Programme Update Regional Roadshows Jim Connolly National Director CHC SIP Programme June 2018 1 1
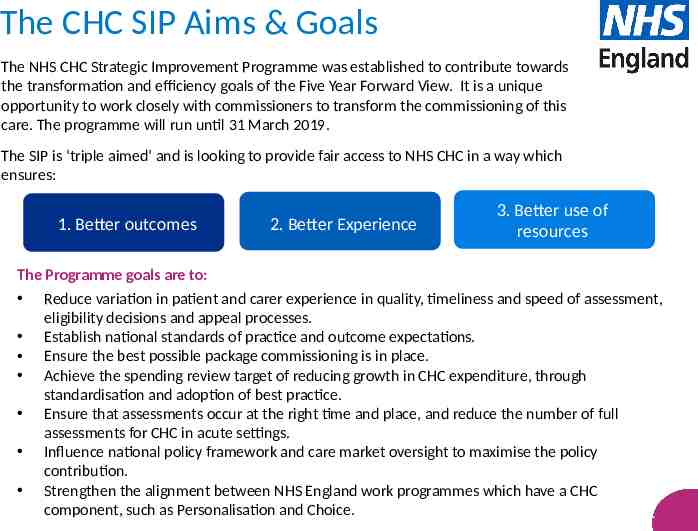
The CHC SIP Aims & Goals The NHS CHC Strategic Improvement Programme was established to contribute towards the transformation and efficiency goals of the Five Year Forward View. It is a unique opportunity to work closely with commissioners to transform the commissioning of this care. The programme will run until 31 March 2019. The SIP is ‘triple aimed’ and is looking to provide fair access to NHS CHC in a way which ensures: 1. Better outcomes 2. Better Experience 3. Better use of resources The Programme goals are to: Reduce variation in patient and carer experience in quality, timeliness and speed of assessment, eligibility decisions and appeal processes. Establish national standards of practice and outcome expectations. Ensure the best possible package commissioning is in place. Achieve the spending review target of reducing growth in CHC expenditure, through standardisation and adoption of best practice. Ensure that assessments occur at the right time and place, and reduce the number of full assessments for CHC in acute settings. Influence national policy framework and care market oversight to maximise the policy contribution. Strengthen the alignment between NHS England work programmes which have a CHC component, such as Personalisation and Choice. 2 2
Finance and Information Aiming to improve understanding of NHS CHC information, including both reported expenditure and activity data. The main focus areas are: Improving the accuracy, timeliness, breadth and completeness of CHC financial and activity information. Improving the understanding of the drivers of unwarranted variation in CHC. Challenging CCGs and Regional teams to deliver a decrease in growth against the projected increase in CHC expenditure of over 1bn by 2020/21. Working with CHC systems suppliers to support CCGs to improve the way they manage and understand CHC data. Workforce Helping to professionalise the CHC workforce, supporting the development of the standard operating model (Better CHC Manual) to help underpin outcomes. Key outputs include: Publication of competency framework, endorsed by RCN, RCOT, COP, CSP, ADASS – August 2018 Core CHC training (reflecting revised national framework) available via e-learning tool – August 2018 Supplementary CHC training catalogue – September 2018 Workforce Modelling toolkit – November 2018 Communications & Engagement Ensuring continued programme communications and engagement, both internally and externally. Outputs including: Developing and implementing communications and engagement strategies Coordinating programme enquiries and handling media issues Capturing patient, family and carer experiences of CHC to aid training and awareness. 3 3
Business Change and Delivery This workstream is wide ranging, looking at a number of specific projects, plus the overarching consideration of programme delivery assurance to March 2019 and sustainability post March 2019. Specific projects are looking at: The CHC Initial Care Pathway (ICP) Digital CHC These are aimed at improving both efficiency and effectiveness of the CHC process, allowing greater consistency between decisions, achieved faster The Collaborative Aims to bring together the CHC community to facilitate co-production and test and implement CHC service improvement. Areas of work include: Continued engagement of CCGs and LAs through regular interactive WebEx’s and Development events with the Development Group, Test and Scale Group and full community. Creation of a patient and sector/ third sector collaborative. ‘Better Continuing Healthcare Manual’ – Accessible online and housing best practice, improvement tools, patient experience films, staff competencies, training tools etc. Aiming to assist CCGs in streamlining process and improving patient experience. Commissioning Strategy Exploring standardisation across a number of commissioning areas such as Care Homes and Domiciliary Care. Exploring best practice for procurement when commissioning external providers. Developing standard specifications and one IPA which can be used across the country. 4 4
Programme Progress Programme is currently on track and all workstreams are geared up to delivery. Excellent progress being made on: CHC Delivery Model Joint statements being developed with ADASS. Positive, helpful feedback from Collaborative Development Day 30 May Workforce Competency Framework & training tools Positive, helpful feedback from the Collaborative Development Day 30 May Commissioning Commissioning documents/specs to be made available for review and comment - Dom Care, Nursing Home Care, IPAs. Initial Care Pathway project is identifying some interesting questions. The Finance and Information workstream will be re-running the variation information for publication later in the spring. Understanding and tackling the cause of unwarranted variation remains key for both the programme and CCGs. 5 5
Assurance Recognition of the work undertaken by CCGs in hitting the location of assessment, and the support through the assurance process from the CHC Business Unit. Still more work to do on prolonged waits. PHBs Letter regarding mainstreaming PHBs has now gone out to CCGs. This is fully supported by the SIP programme from both an individual perspective, (more choice and control over how their care needs are met) and an efficiency perspective; it is estimated that package costs could reduce by up to 17%. All Dom Care to go to PHBs by March 2019. Implementation to be managed by PHB Team. CHC Connect Online SharePoint resource for the SIP – Launch earlier this year was delayed due to a technical issue. Should be available for use in early June. Slight access issue for Local Authority colleagues, but a work around is available. 6 6