Neonatal Abstinence Syndrome Diana Frankenburger, MSN, RNC-OB, CCE,
29 Slides1.26 MB
Neonatal Abstinence Syndrome Diana Frankenburger, MSN, RNC-OB, CCE, CLS [email protected]
Learning Objectives Participants will be able to define Neonatal Abstinence Syndrome (NAS) as it compares to typical infant development. Participants will be able to list common behaviors in infants and newborns with NAS. Participants will be able to state 3 potential supportive measures for infants experiencing NAS and their families.
The Opioid Crisis: Background 2017: US Department of Health and Human Service (HHS): opioid crisis in America is a public health emergency 11.1 million Americans misused prescription meds 47,872 deaths from unintentional overdose 2.6 million had opioid use disorder Use of heroin and pain medications by women nearly doubled since 2009 Delivery records indicate quadrupling of opioid use disorder since 1999 (Kondili & Duryea, 2019)
Results of Opioid Exposure Increase in health care spending for prolonged hospitalizations 50-80% of infants exposed to substances develop NAS symptoms Symptoms begin 24-72 hours Symptoms can last up to 60 days Long term effects
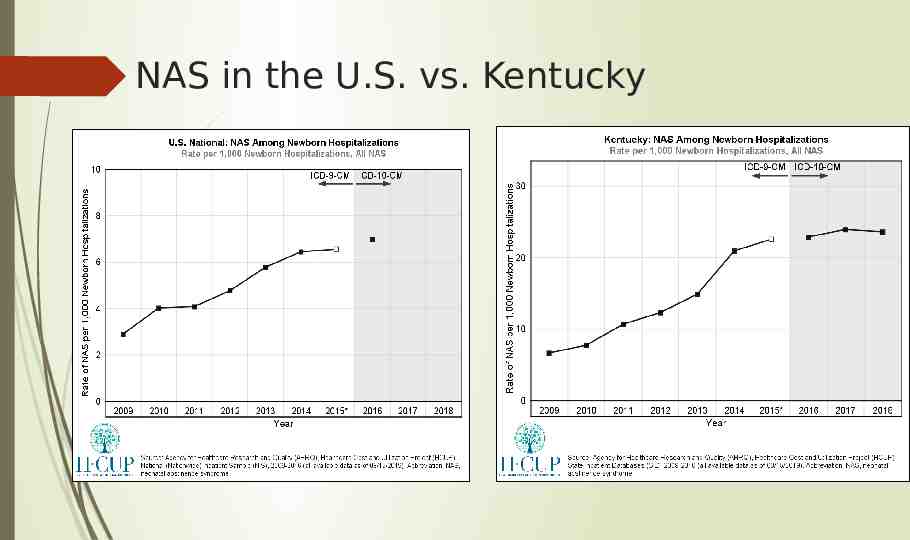
NAS in the U.S. vs. Kentucky
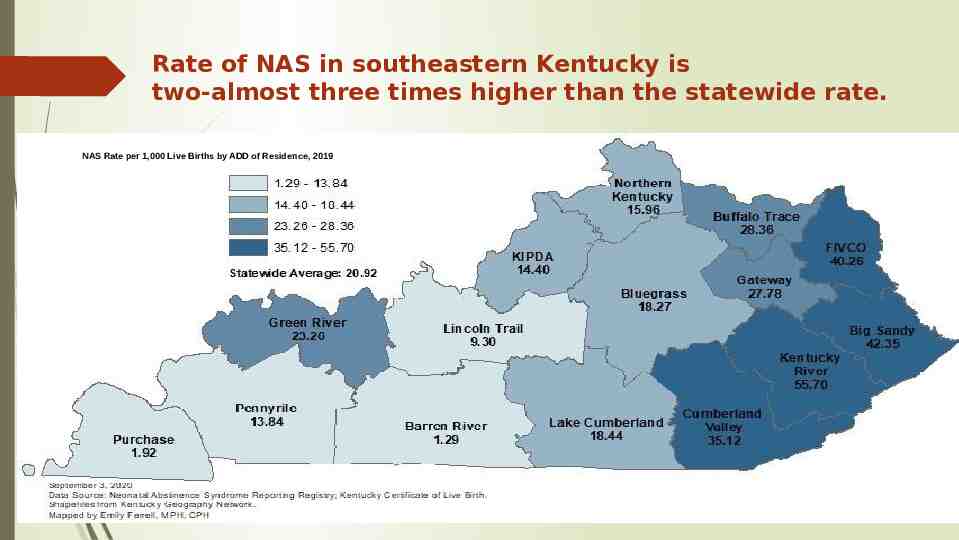
Rate of NAS in southeastern Kentucky is two-almost three times higher than the statewide rate. NAS Rate per 1,000 Live Births by ADD of Residence, 2019
Question 1: True or False Infants born to women addicted to substances are also born addicted to substances.
Definition of NAS (Neonatal Abstinence Syndrome) An infant’s response to withdrawal of prescribed or illicit medications or substances they were exposed to before birth. Withdrawal may be increased by other medications or substances including nicotine and caffeine. Infants are born withdrawing, not addicted. Addiction is the inability to stop using a substance despite it’s harmful consequences. Withdrawal is the effect of stopping the use of a substance or behavior; often involves physical symptoms, sometimes severe enough to cause death. (Felman, 2018) (Reddy, et al., 2017)
How to tell an infant has NAS Infants are identified through mother’s health information, history, and infant’s behavior after birth. Drug screening of urine and stool help determine drugs. Most commonly used: Finnegan Neonatal Abstinence Scoring Tool to measure infant’s degree of withdrawal Scoring concentrates on specific body systems (see next slide) Number assigned is associated with severity of symptoms
Baby’s Systems Affected Central Nervous System (high pitched cry, irritability, high muscle tone, highly reflexive, difficulty sleeping) Autonomic Nervous System (high temperature, nasal stuffiness, sweating, sneezing, splotchy skin, yawning, rapid breathing) Gastrointestinal System (disorganized swallow and suck, poor feeding, weight loss, loose stools, spitting up)
NAS Crying
When Should Assessment for NAS Begin? Within 3-6 hours after birth Symptoms usually appear within 72 hours of birth Scoring every 3-4 hours Scoring 8 in 3 consecutive scorings or 12 in two consecutive scorings Length of stay for evaluation: 5 days in many facilities If treatment with medication is required, stay may be 14 days or longer (Kondili & Duryea, 2019) (ACOG, 2017) (Kondili & Duryea, 2019) (ACOG, 2017)
Question 2: True or False Women in a treatment program receiving medication for their substance use do not have to worry about their babies experiencing withdrawal.
Why Treat Pregnant Women with Drugs (Subutex, Suboxone, Methadone)? Prevents opioid withdrawal symptoms Decreases use of drugs off the street Improves prenatal care In combination with prenatal care, decreases risk of complications Decreases participation in high-risk behaviors, violence Decreases risk of relapse during pregnancy (ACOG Committee Opinion Number 711, 2017)

In the Hospital: Non-Medical Support Breastfeeding when appropriate Rooming in Mom’s bonding and attachment Skin to skin (Kangaroo Care) Infant massage, positioning 5 Ss Soothing Techniques (works with all babies) https://www.youtube.com/watch?v 6OtPSfyZXNw&t 2s (Kondili & Duryea, 2019)
How can you help infants? Swaddling through 3 months (or until baby shows signs of turning over) White noise (no time limit) Rocking or swinging Holding close Pacifier Extra time with feeding, smaller amounts and more frequent burping(Pace) More subject to skin breakdown: use water/water wipes for cleaning Aquaphor for diaper area irritation Eye contact Conversation Infant Massage
KEY STRATEGIES FOR HELPING INFANTS 5 Ss Pace Feeding Communication: verbally, through eye contact, and touch
How can you help families? Children with NAS more likely to die between 28 days of life and 1 year; most common cause of death: Sudden Infant Death Syndrome. Model and Teach ABCDs of SAFE SLEEP; ask caregivers where baby sleeps-What is a safe sleep surface? Discourage co-sleeping Post information about smoking reduction or stopping, and effects of 2nd and 3rd hand smoke for children Use TEN-4 to evaluate for abuse; Bruising anywhere on baby who is not pulling up or taking steps Accept families without judgment
Helping Families cont’d Some children exposed to substances often do not receive health care in their first 2 years of life; results in hospitalizations for infections; other childhood problems left untreated. Help moms recognize when medical attention is needed Children of parents abusing drugs usually receive less attention, direction, often live in chaos; increases physical and mental stressors; can lead to negative behaviors including drug abuse or crime. Any attention may seem better than no attention! Mom’s bonding with her child is influenced by many factors- her own experience as a child or with her own mother; her feelings of guilt and remorse for what has happened with her children. Look for ways to praise what the caregiver is doing right!
KEY STRATEGIES FOR HELPING FAMILIES ABCDs of Safe Sleep Know Signs of Abuse (TEN-4) Help caregivers recognize when medical attention is needed Share things their child enjoys and successful ways for redirection/ coping with acting out.
Question 3: Name 3 supportive measures for infants with NAS and their families.
References ACOG Committee Opinion (2017). Opioid use and opioid disorder in pregnancy, Number 711. Retrieved from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/08/opioid-use-andopioid-use-disorder-in-pregnancy Adams, E. (2017). PATHways program demonstrates success of evidence-based, collaborative approaches to perinatal opioid treatment. UKnow: University of Kentucky News. Retrieved from: https://uknow.uky.edu/uk-healthcare/pathways-program-demonstrates-success-evidence-based-coll aborative-approaches . Casper, T., & Arbour, M. (2014). Evidence-based nurse-driven interventions for the care of newborns with neonatal abstinence syndrome, Advances in Neonatal Care, 14(6): p. 376-380. doi: 10.1097/ANC.0000000000000118. Felman, A. (2018). What is addiction? Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/323465 Highleyman, L. (2017). New approaches help babies get through opioid withdrawal, MedPage Today, May 12, 2017. Retrieved from: http://www.medpagetoday.com/meetingcoverage/pas/65259. Knopf, A. (2018) More research needed on NAS, but evidence for breastfeeding and rooming in is clear, Alcoholism and Drug Abuse Weekly, 30(15): 1-3. Retrieved from: http://dx.doi.org.ezproxy.uky.edu/10.1002/adaw.31921 Kocherlakota, P. (2014). Neonatal Abstinence Syndrome, Pediatrics, 134(2): p.e-547-e-561. doi:10.1542/peds.2013-3524 .
More References Kondili,E. & Duryea,D. (2019) The role of mother-infant bond in neonatal abstinence syndrome (NAS) management, Archives of Psychiatric Nursing, 33(3): p. 267-274. McQueen, K. (2018). Rooming-in could be an effective non-pharmacological treatment for infants with neonatal abstinence syndrome, Evidence Based Nursing. doi: 10.1136/eb-2018-102948. Oei, J.L.(2019). After NAS, Seminars in Fetal and Neonatal Medicine, 24(2019): 161-165. Retrieved from https://doi.org/10.1016/j.siny.2019.01.012 Reddy, U., Davis, J., Ren, Z., & Green, M. (2017). Opioid use in pregnancy, neonatal abstinence syndrome, and childhood outcomes, Obstetrics & Gynecology, 130:1, p. 10-27. Reece-Stremtan, S., Marinelli, K. (2015). ABM clinical protocol #21: Guidelines for breastfeeding and substance use or substance use disorder, revised 2015, Breastfeeding Medicine, 10(3): 135141. doi: 10.1089/bfm.2015.9992 Saia,K., Schiff, D., Wachman, E., Mehta, Pl., Vilkins, A., Sia, M., Price, J., Samura, T., DeAngelis, J., Jackson, C., Emmer, S., Shaw, D., & Bagley, S. (2016). Caring for pregnant women with opioid use disorder in the USA: Expanding and improving treatment, Current Obstetrics and Gynecology Report, 5:257-263. doi: 10.1007/s13669-016-0168-9.
24 Team KY SCOPE Child Challenge Diana Frankenburger, Prenatal Education Coordinator UK HealthCare PATHways
25 Background on Case Annie: Age 6 weeks (treated for NAS on Morphine for 2 weeks) Mother Michelle (in a treatment program) and works at a convenience store. First time parenting for Michelle- other 2 children removed. Annie cries for long periods at daycare, and, per Michelle, for long periods each evening. Annie spits up frequently and has had formula changed twice by pediatrician. Michelle’s mother has custody of other children and sometimes picks Annie up.
26 Child and Family Strengths A mom who has worked hard to parent. A mom who does show initiative in taking Annie to the pediatrician. A mom who continues to have a relationship with her mother and appears to have her support. A child born at term while Michelle was stable in her recovery. A child who is able to maintain weight. A child who has successfully been weaned off Morphine for withdrawal symptoms.
27 Primary Areas of Challenge Annie has difficulty with feeds- spits up frequently and takes longer Annie has long periods of crying and short periods of sleep Michelle is a single parent/ few supports available What coping skills does Michelle have? Who would Michelle reach out to if she needed assistance? What comfort measures does Michelle know/ practice with Anne?
Barriers and Goals for this Challenge Barriers: Annie: potential for lingering withdrawal symptoms and poor feeding. Michelle: limited interaction, parenting experience, few supports Goals: Annie will keep 90% of her feeds down during the day; Annie will be soothed by comfort measures and these will be shared with Michelle to use at home 28
29 Small Group Discussion Questions 1) List strengths of the child 2) List strengths of the family 3) List strategies to address these challenges discussed 4) List some resources for this child and family (websites, agencies, training opportunities) 5) List some offices in your region or in KY that can assist this child and family