Mental Health in Adolescence Mary Dobbins, MD
65 Slides5.08 MB
Mental Health in Adolescence Mary Dobbins, MD

CME Accreditation Statement The Illinois Chapter, American Academy of Pediatrics is acc redited by the Illinois State Medical Society (ISMS) to provide continuing medical education for physicians. The Illinois Chapter, American Academy of Pediatrics des ignates each enduring activity for a maximum of 1 AMA PRA Category 1 Credit(s) . Physicians should claim only the credit commensurate with the Nurses and Nurse Practitioners canactivity. submit Certificates of extent of their participation in the Attendance to their accrediting board for credit for participation in the live webinars.

CE Accreditation Statement One (1) continuing education hour (CE) is approved for this live webinar ”Mental Health in Adolescence" on March 27, 2020 by the Illinois Department of Human Services, Division of Developmental Disabilities for one continuing education credit for the following licensed professionals: Licensed Clinical Professional Counselors (LCPC) Licensed Clinical Psychologists (LCP) Licensed Clinical Social Workers (LCSW) Licensed Nursing Home Administrators (LNHA) Licensed Occupational Therapists (OT) and Occupational Therapy Assistants (OTA), Licensed Physical Therapists (PT) and Physical Therapy Assistants (PTA) Licensed Professional Counselors (LPC) Licensed Social Workers (LSW) Registered Nurses (RN) Licensed Practical Nurses (LPN) Advanced Practice Nurses (APN)

ADOLESCENT HEALTH WEBINAR SERIES: PART 2 Introduction to Vaping Available at https://illinoisaap.org/adolescent-health/ Welcome Marijuana: Medical and Recreational Use Available at https://illinoisaap.org/adolescent-health/ Mental Health March 27, 2020, 12-1 PM CT HAPPENING NOW! Aiding Adolescents to Take Control of Their Health April 24, 2020, 12-1 PM CT Registration: https://bit.ly/2D6CdZ8

Planning Group Sara Parvinian, MD, FAAP Rachel Caskey, MD, MaPP, FAAP Kathy Sanabria, MBA Olyvia Phillips, MPH/MBA Candidate Webinar Planning Group CME APPLICATION REVIEWERS Karen Judy, MD, FAAP Matthew Leischner, MD, FAAP CONTENT REVIEWER Rachel Caskey, MD, MaPP, FAAP

Webinar Information RECORDING DURING THE WEBINAR The webinar will be recorded and made available at illinoisaap.org. The webinar will be made available for CME/CE credit on ICAAP's LMS in Spring/Summer 2020! Participants will be muted during the webinar. Please type questions or comments into the chat box and they will be answered at the conclusion of the presentation.

Webinar Information Continued. At the conclusion of the Attendees will be emailed a link to complete an online evaluation. webinar. Once the evaluations are submitted, Olyvia Phillips will send participants a certificate of participation for CME/CE records.

Presenter: Dr. Mary Dobbins Dr. Dobbins is an associate professor at Southern Illinois University School of Medicine, where she is the Director of Integrated Care Initiatives in the Department of Family and Community Medicine. A pediatrician and psychiatrist, she has worked extensively with child and family development, the developmental effects of trauma and stress, and the social determinants of health. She is a frequent consultant for the integration of preventative, treatment, and restorative practices for children in educational, medical, and community settings. She has been involved with national initiatives through the American Academy of Pediatrics, and is currently the President Elect of ICAAP.

NO FINANCIAL CONFLICT OF INTEREST OFF-LABEL USE OF MEDICATIONS IN PEDIATRICS Disclosures LIMITATIONS OF CURRENT EVIDENCE TRIGGER WARNING CREDITS

Discuss the types of mental health problems presenting in adolescents Discuss management and prevention Objectives Intentionally and comfortably adapt practice Identify resources for practice

I. Development and Mental Health

Developmental period (preteen years through early 20s) “Adolescence” Competence Sense of self Independence / adult transition Puberty Context / sexuality

Optimal adjustment and daily functioning “Mental Health” Emotional and “behavioral” health Absence of mental illness

The acquisition of the abilities to successfully navigate the demands of daily living “Develop – Mental Health” Adaptability Perspective - cognitive skills, self-regulation (psychological adjustment) – sense of self, others, locus of control, expectations Neurodevelopment, experiences, genetics Environment – family, activities, social, community / society, inner self

Develop-Mental Health Take Home points Is there a problem? If so: What are they bothered by ? Why can’t they handle it ?

II. Presentations

Presenting complaint (importance of assessment) Presentations “Door-knob comment” (time management) Presenting as another problem (importance of spotting “red flags”) Hidden (importance of screening)

DEPRESSION / SUICIDAL IDEATION SUBSTANCE USE Screening / Assessment ANXIETY / TRAUMA ENVIRONMENTAL SAFETY SOCIAL DETERMINANTS OF HEALTH GENERAL FUNCTIONING PROTECTIVE FACTORS

Pediatric Symptom Checklist (PSC) Child Symptoms Inventories (CSI) Common Validated Tools Achenbach (ASEBA) Child Behavior Checklist (CBCL) Columbia Impairment Scale Screen for Child Anxiety Related Emotional Disorders (SCARED) Ask Suicide-Screening Questions (asQ) PHQ-9 Modified for Adolescents (PHQ-A) Columbia Suicide Severity Risk Scale (CSSRS)

Interview Patient alone Confidential - with limits Language – “stress”, “hurt”/ “kill” General approaches

Youth’s perspective “Measure your mood” General Approaches BATHE How have you been? How does that make you feel? (affect) What troubles you the most about that? What are you doing to handle the situation? Affirmation (empathy)

Protective Factors RELATIONSHIPS MEANINGFUL ACTIVITIES / INVOLVEMENT SPIRITUAL BELIEFS / RELIGIOUS AFFILIATION

Three Levels of Stress Positive Brief increases in heart rate, mild elevations in stress hormone levels. Tolerable Serious, temporary stress responses, buffered by supportive relationships. Toxic Prolonged activation of stress response systems in the absence of protective relationships.

Keep Keep stress within healthy levels Mitigate Mitigate effects of stress Interventions Treat Treat effects of stress individual resilience / resistance to Increase Increase effects of stress

Take Home Points Presentations Everyday functioning (external) Mood (internal) Coping strategies (substance use, selfharm) Stressors / protective factors

III. Symptoms and Disorders

Categories of Symptoms Resistant behavior, school refusal Disruptive, aggressive behavior Mood (anxiety, depression, irritability) Change in behavior / level of functioning (sleep, grades, interpersonal interactions, substance use)

“Disorders” Under-recognized, under-treated (autism, ADHD) Common (depression, anxiety / PTSD variants) “Marker misdiagnosis” (ODD, IED, DMD, BPD, BD) Serious but uncommon (bipolar disorder, psychosis) Chronic and complex (eating disorders, addiction)

Problematic/dangerous behaviors indicate a child is overwhelmed. What causes problems? Intrinsic disorders (psychotic and bipolar disorders) are uncommon. (although can begin to emerge in adolescence) Problems with adaptability are common. (autism spectrum, social immaturity) Problems with self-regulation are common. (ADHD and trauma) Mood problems are common, and usually secondary.

COGNITIVE ABILITIES / FLEXIBILITY SOCIAL COMMUNICATION Adaptability: Intrinsic and Extrinsic Factors SOCIAL MATURITY EXECUTIVE FUNCTION SLEEP SENSORY PROCESSING EXTERNAL STRESSORS AND SUPPORTS

Poor Adaptability Misdiagnosis Missed diagnoses Stubborn, bossy, difficult Sensory Processing Disorder Attention seeking Bad Social Communication / Autism Spectrum Disorders Unmotivated, lazy Cognitive inflexibility Oppositional Defiant Disorder Inability / immaturity Conduct Disorder Stress / trauma Personality Disorder

ADHD Selfregulation Sensory processing Poor sleep Anxiety Trauma
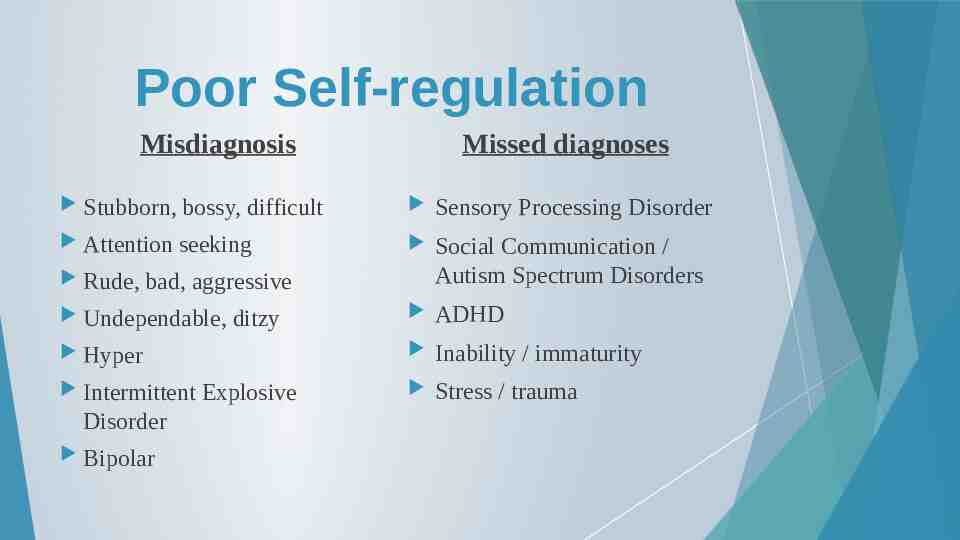
Poor Self-regulation Misdiagnosis Missed diagnoses Stubborn, bossy, difficult Sensory Processing Disorder Attention seeking Social Communication / Autism Spectrum Disorders ADHD Inability / immaturity Stress / trauma Rude, bad, aggressive Undependable, ditzy Hyper Intermittent Disorder Bipolar Explosive

Anxiety Mood Presentations Depression Irritability, temper

Adjustment and Mood Problems Misdiagnosis Stubborn, bossy, difficult Attention seeking Missed diagnoses Poor adaptability / functioning Drama queen Anxiety Amotivated, weak, absent Depression Rude, bad Trauma Personality disorder Drug use Anger management problem Bipolar

Pearls for “Diagnosis” Focus on “stress” (most problems are Chronic Adjustment Disorders) Determine “why” as well as “what”(Why can’t child adapt? What is overwhelming them?) Specifically consider trauma, executive function, social atypicality Screen for maladaptive coping mechanisms Consider impact on developmental tasks (sense of competency and worth, ability to form healthy relationships, vision for future)

Take Home Points Symptoms and Disorders The Importance of “Why” (not just volitional) Understanding is more important than formal diagnosis. “Mental Health” problems do not always need “mental health” treatments.

IV. Management

Personal Resilience and Readiness Vulnerability Support Knowledge Skills Expectations

Complex / Chronic patients Diagnostic ambiguity Realistic Expectations Treatment uncertainty Care is “messy” Engagement and progress are key
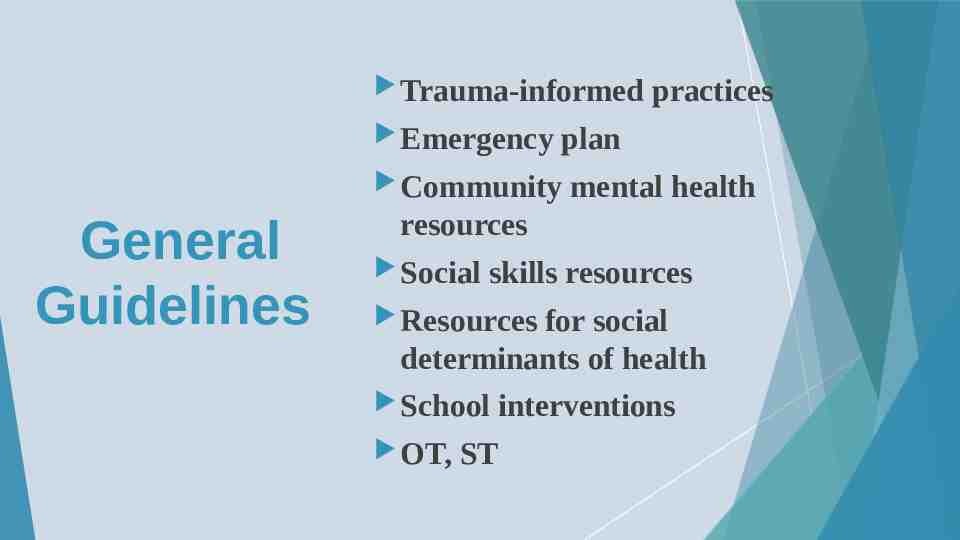
Trauma-informed Emergency plan Community General Guidelines practices mental health resources Social skills resources Resources for social determinants of health School OT, interventions ST

Screening opportunity Emergency procedures Patient presentations in the medical setting Clinical Strategies Medical services – assessment, treatment Care coordination “Anticipatory Professional guidance” influence on environment Relationship as a protective factor

Management Assessment of distress Proactive followup / therapeutic relationship Assessment of contributing factors Identification / reinforcement of strengths Linkage to resources Communication with / assistance for family

Anxiety Specific Disorders Depression Bipolar Disorder Psychosis

Emergency Rare, usually secondary to reactivity / impulsivity or drug use Treat Anxiety Disorders Be assertive, utilize a variety of approaches, avoid benzodiazepines Specialty Care Coordinate with therapist (and a variety of environmental supports) Psychiatrist if complex with multiple medication changes or resistant Pearls Look for underlying disorder (trauma, decreased adaptability, medical causes) and maladaptive coping behaviors

Emergency Active suicidality, especially with plan and means, needs ED assessment for hospitalization Higher risk if prior attempt, humiliated, impulsive, psychotic, or using drugs (Passive suicidality or SIB doesn’t mean acute danger, but does mean serious distress) Depression Treat SSRI medication if over 3 weeks (differentiates from normal sadness) Specialty Care Coordinate with therapist (and a variety of environmental supports) Pearls Usually occurs when patient has become hopeless of alleviating stress

Suicide Prevention Campaign and Toolkit

Assess Managing a Positive Screen for Suicide: Counsel Moderate Counsel Assess level of risk and intervene accordingly Low Risk: counsel, refer, follow-up Moderate Risk: counsel, refer, develop Safety Plan, follow-up Severe Risk: counsel, ensure parents/caregivers closely monitor child, remove lethal means, develop Safety Plan, make a crisis referral, follow-up

National Suicide Prevention Lifeline Emergency Contacts 24 / 7 1-800-273-TALK (8255) Text HELLO to 741741 Illinois Warm Line IDHS, Illinois Mental Health Collaborative Monday - Friday, 8 am - 5 pm 1- 866 - 359 – 7953

Emergency Bipolar Disorder (Manic Depression) Check for drug use, medical disorder (delirium) If risk for self-harm, need ED assessment for hospitalization Treat If obvious mania, will need mood stabilizer started to prevent deterioration Specialty Care Until stable Pearls Commonly misdiagnosed, symptoms overlap with many disorders / drug side effects. NOT just “mood swings” (spontaneous, discrete, uncharacteristic pattern of change)

Emergency Psychosis (hallucinations , disorganized thought) Check for drug use, medical disorder (delirium) Commands to harm self or others need ED assessment for hospitalization Treat Most commonly secondary to anxiety disorder (especially PTSD) – treat that! Specialty Care If sensory or bizarre, more likely to be true emerging psychosis Pearls Autism spectrum / exceptionally creative individuals may be misinterpreted May be normal if related to beginning or end of sleep

Take Home Points Management Care is “messy” Engagement and progress are key Emergencies are not common Relationships are of utmost importance

V. Pharmacotherapy

Medication Management Anxiety, Depression Sleep Sympathetic nervous system hyper activation Impulsivity Other (psychosis, mood swings)

Reassurance for Families Use to “make child healthier”, not “alter” them. A medication trial does not mean a lifelong need. Most are very safe and well-tolerated if “customized” gradually and taken as prescribed. Discuss “what we typically see in practice” (risks and benefits). Not a “magic wand” Stimulants are not intrinsically addictive or zombiogenic. Many medications have multiple uses.

Therapeutic doses often are not based on weight. Adjustments need to be small, but timely. Pearls for Providers Children tend to be more sensitive if they are young, have atypical neurodevelopment, or have a family history of sensitivity. FDA approval is used for marketing purposes. Benzodiazepines have a poor benefit: risk ratio. Become familiar with a few favorite medications.

Anti-histamine UrgentEmergency Aid: Hydroxyzine Useful for overwhelming peaks of distress, PTSD, sleep Peaks in 20-30 minutes (non-addictive alternative to benzodiazepines) Often sedating, especially if used “as needed” Use assertively for PTSD, may be adjusted dose to dose Adolescent dose typically 10 mg – 25 mg Maximum adult dose 100 mg four times per day Pamoate form preferred for anxiety, but HCL acceptable

Alpha-2 agonists Useful for “inflexibility”, reactive aggression, ADHD, sleep Jack-of-alltrades: Guanfacine and Clonidine Rare cardiovascular concern (don’t stop abruptly) Common anti-histamine effect (step up gradually) Guanfacine- Usual starting dose 0.5 mg (0.1 mg preschool age) Maximum dose 4 mg daily, divided into bid-tid dosing Liquid and extended-release forms available

Sympathetic hyperactivity – propranolol or guanfacine Inflammatory messaging – hydroxyzine Combinations for PTSD Nightmares- prazosin Flashbacks / derealization – neuroleptics aripiprazole (starting dose 2.5 mg - 5 mg) quetiapine (starting dose 12.5 mg- 25 mg) Sleep aid – trazodone Quality of mood – SSRI Look for mania / hypomania, monitor “ADHD”

Monitor sedation, light-headedness for antihistamines, beta blockers, alpha agonists, and prazosin. Medication Pearls SSRIs / SNRIs are very safe despite black box warning, but need very slow adjustment. Main risk is agitation (may unmask true mania in those predisposed). Neuroleptics, lithium and valproate require lab work and, along with lamotrigine, have more specific side effect profiles. Avoid benzodiazepines.

Take Home Point Pharmacotherapy Familiarity with a few medications across categories will suffice for the management of most conditions

VI. Resilience

Resilience Relationships Realistic sense of self-worth Practice in selfefficacy Development of interpersonal skills Authoritative yet flexible parenting for exploration within safe boundaries Realistic understanding of world around them Safe and gradual introduction into broader society

Anticipatory Guidance Support for parents Self-care (sleep) Self-regulation, mindfulness Self-efficacy (chores, failures and mistakes) Interpersonal skills (limit use of social media) “Background” stressors (media, politics)

You as a Protective Factor ! “You don’t have to be a therapist to be therapeutic.” - M. Dobbins