Major case presentation on Acute Pulmonary Embolism with Deep Vein
13 Slides63.14 KB
Major case presentation on Acute Pulmonary Embolism with Deep Vein Thrombosis By
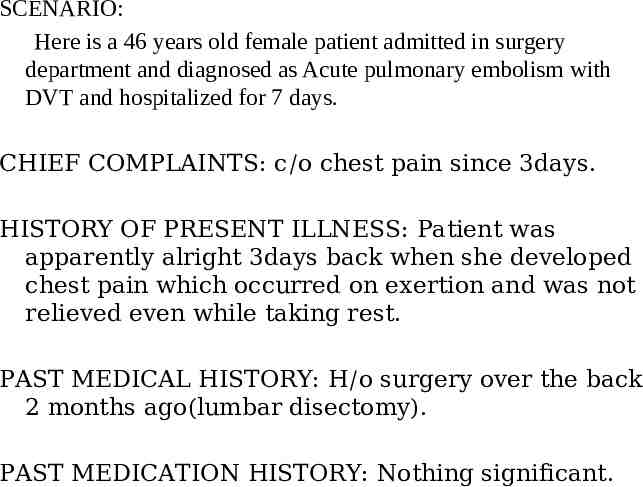
SCENARIO: Here is a 46 years old female patient admitted in surgery department and diagnosed as Acute pulmonary embolism with DVT and hospitalized for 7 days. CHIEF COMPLAINTS: c/o chest pain since 3days. HISTORY OF PRESENT ILLNESS: Patient was apparently alright 3days back when she developed chest pain which occurred on exertion and was not relieved even while taking rest. PAST MEDICAL HISTORY: H/o surgery over the back 2 months ago(lumbar disectomy). PAST MEDICATION HISTORY: Nothing significant.
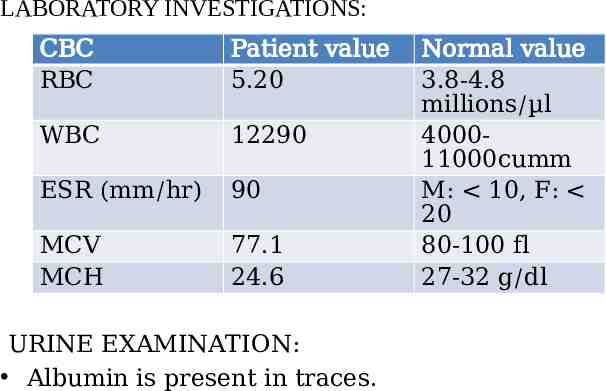
LABORATORY INVESTIGATIONS: CBC RBC Patient value 5.20 WBC 12290 ESR (mm/hr) 90 MCV MCH 77.1 24.6 URINE EXAMINATION: Albumin is present in traces. Normal value 3.8-4.8 millions/µl 400011000cumm M: 10, F: 20 80-100 fl 27-32 g/dl
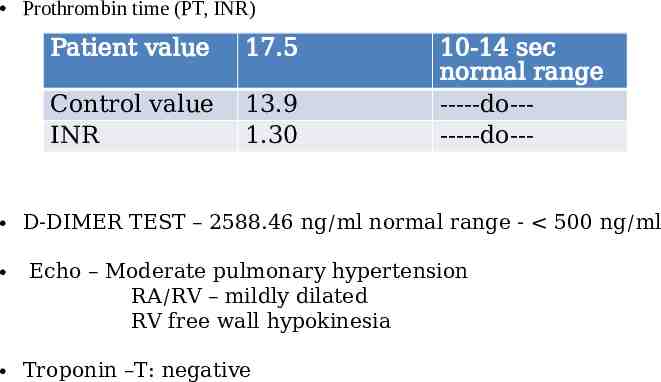
Prothrombin time (PT, INR) Patient value 17.5 Control value INR 13.9 1.30 10-14 sec normal range -----do-------do--- D-DIMER TEST – 2588.46 ng/ml normal range - 500 ng/ml Echo – Moderate pulmonary hypertension RA/RV – mildly dilated RV free wall hypokinesia Troponin –T: negative
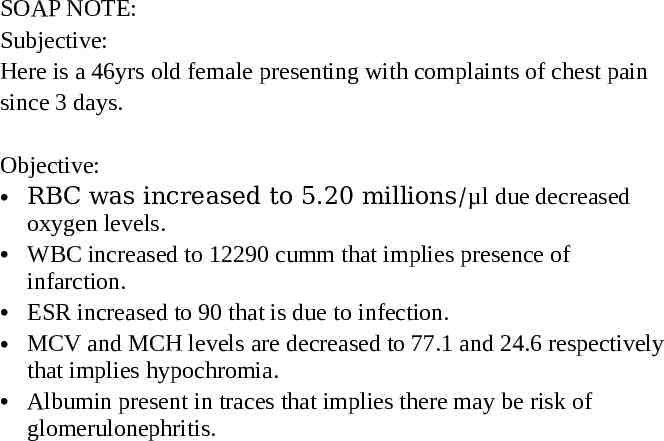
SOAP NOTE: Subjective: Here is a 46yrs old female presenting with complaints of chest pain since 3 days. Objective: RBC was increased to 5.20 millions/µl due decreased oxygen levels. WBC increased to 12290 cumm that implies presence of infarction. ESR increased to 90 that is due to infection. MCV and MCH levels are decreased to 77.1 and 24.6 respectively that implies hypochromia. Albumin present in traces that implies there may be risk of glomerulonephritis.
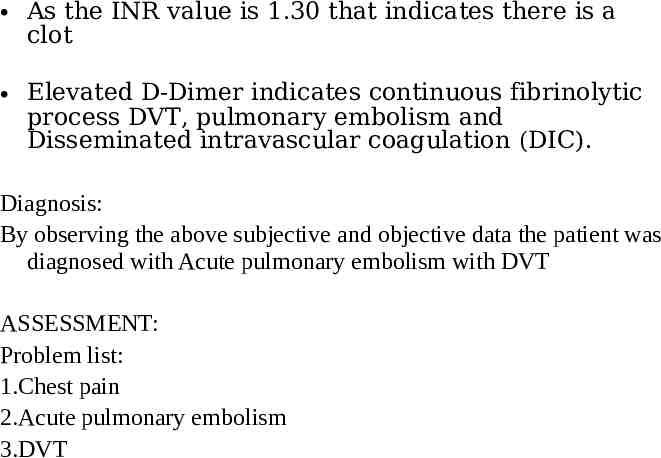
As the INR value is 1.30 that indicates there is a clot Elevated D-Dimer indicates continuous fibrinolytic process DVT, pulmonary embolism and Disseminated intravascular coagulation (DIC). Diagnosis: By observing the above subjective and objective data the patient was diagnosed with Acute pulmonary embolism with DVT ASSESSMENT: Problem list: 1.Chest pain 2.Acute pulmonary embolism 3.DVT
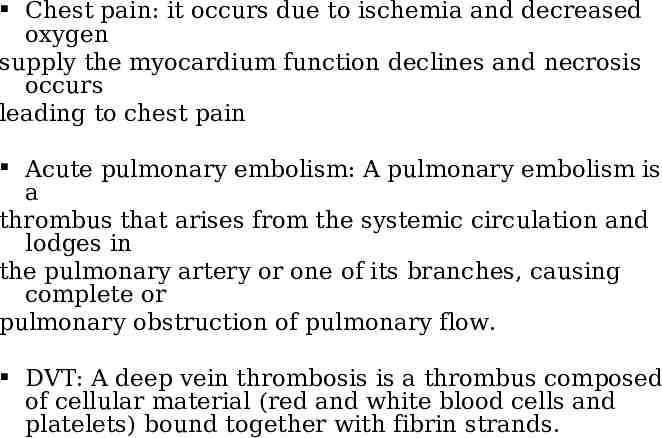
Chest pain: it occurs due to ischemia and decreased oxygen supply the myocardium function declines and necrosis occurs leading to chest pain Acute pulmonary embolism: A pulmonary embolism is a thrombus that arises from the systemic circulation and lodges in the pulmonary artery or one of its branches, causing complete or pulmonary obstruction of pulmonary flow. DVT: A deep vein thrombosis is a thrombus composed of cellular material (red and white blood cells and platelets) bound together with fibrin strands.
PLAN OF CARE: GOALS OF THERAPY: To prevent the development of pulmonary embolism and the post thrombotic syndrome To reduce morbidity and mortality from the acute event To minimize the adverse effects and the cost of treatment
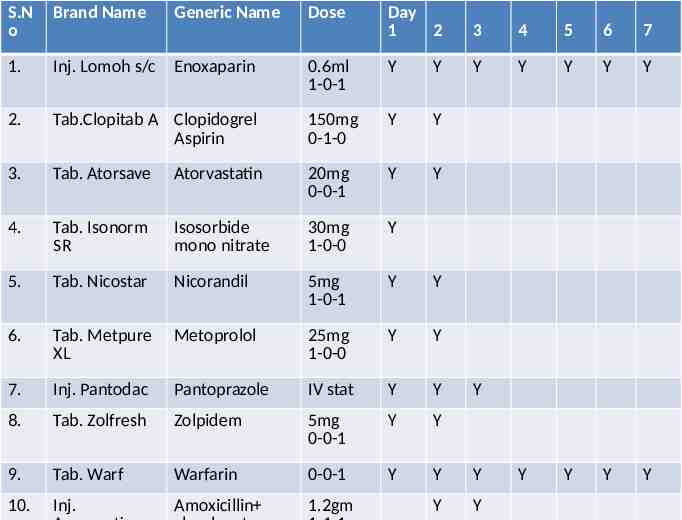
S.N o Brand Name 1. Inj. Lomoh s/c 2. Generic Name Day 1 2 3 4 5 6 7 0.6ml 1-0-1 Y Y Y Y Y Y Y Tab.Clopitab A Clopidogrel Aspirin 150mg 0-1-0 Y Y 3. Tab. Atorsave Atorvastatin 20mg 0-0-1 Y Y 4. Tab. Isonorm SR Isosorbide mono nitrate 30mg 1-0-0 Y 5. Tab. Nicostar Nicorandil 5mg 1-0-1 Y Y 6. Tab. Metpure XL Metoprolol 25mg 1-0-0 Y Y 7. Inj. Pantodac Pantoprazole IV stat Y Y 8. Tab. Zolfresh Zolpidem 5mg 0-0-1 Y Y 9. Tab. Warf Warfarin 0-0-1 Y Y Y Y Y Y Y 10. Inj. Amoxicillin 1.2gm Y Y Enoxaparin Dose Y
11. Tab. Dolo 12. 15. 16. Inj. STK 1amp in 5ml Syp. Neogadine elixir Cap. Recovit total Inj Tramadol T. Calcimox 17. T. Ultra D3 18. Inj. Emset IV 19. Inj. Pan IV 20. 21. Tab. Zerodol MR Cap. Cyra D 22. Cap. Lycoprez 13. 14. Paracetamol 650mg Sos Bolus 30ml 2ml/hr Y Y 2tsp 1-1-1 Y Y Glutamic acid In 100ml NS Calcium corbonate Vit D, Cholecalcifer ol ondansetron 0-1-0 Y Y 1-0-1 500mg 0-1-0 0-1-0 Y Y Pantoprazol e Aceclofenac Domperidon 1-0-0 Rabeprazole 0-1-0 Y Y Y Y Y Y Y Y Neogadine 4mg 1-1-1 40mg 1-0-0 1-0-1 Y Y Y Y Y Y Y Y Y
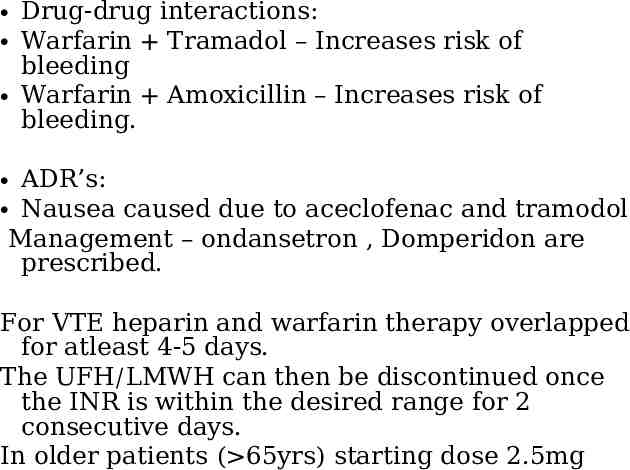
Drug-drug interactions: Warfarin Tramadol – Increases risk of bleeding Warfarin Amoxicillin – Increases risk of bleeding. ADR’s: Nausea caused due to aceclofenac and tramodol Management – ondansetron , Domperidon are prescribed. For VTE heparin and warfarin therapy overlapped for atleast 4-5 days. The UFH/LMWH can then be discontinued once the INR is within the desired range for 2 consecutive days. In older patients ( 65yrs) starting dose 2.5mg
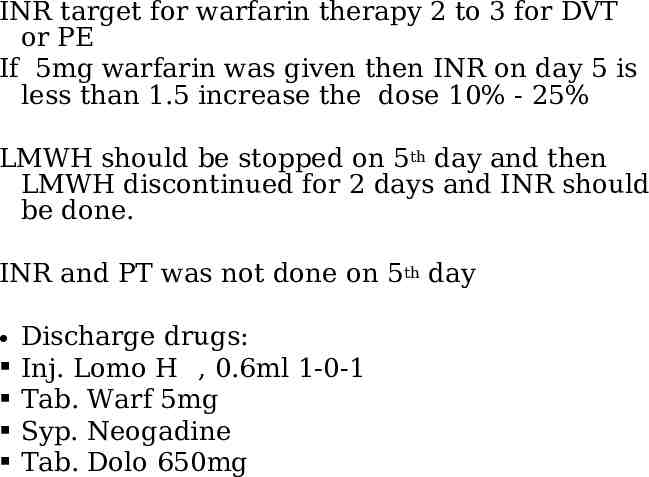
INR target for warfarin therapy 2 to 3 for DVT or PE If 5mg warfarin was given then INR on day 5 is less than 1.5 increase the dose 10% - 25% LMWH should be stopped on 5th day and then LMWH discontinued for 2 days and INR should be done. INR and PT was not done on 5th day Discharge drugs: Inj. Lomo H , 0.6ml 1-0-1 Tab. Warf 5mg Syp. Neogadine Tab. Dolo 650mg

THANKYOU