LGBTQ HEALTH: WHO, WHAT, WHERE AND WHY WE SHOULD CARE LAURA C.
56 Slides6.46 MB

LGBTQ HEALTH: WHO, WHAT, WHERE AND WHY WE SHOULD CARE LAURA C. HEIN PHD, RN, FAAN

OBJECTIVES Introduce you to LGBTQ terminology Discuss historical and contemporary health concerns of the LGBTQ community Discuss facilitators and barriers to health Present current legal and regulatory standards related to LGBTQ health with recommended practice protocols Is your facility compliant?

DEFINITIONS LGBTIQ Gay, Lesbian Exclusive physical and emotional attraction to members of one’s own sex Bisexual Physical and emotional attraction to members of both sexes Transgender (gender identity) A person who feels his or her body is not the sex it should be, regardless of transformational hormone or surgical status Cis-Gender A person whose gender identity matches their sex at birth

Transgender (gender identity) LGBTIQ MtF Male-to-Female (she) transwoman Born with male anatomy, female gender FtM Female-to-Male (he) transman Born with female anatomy, male gender

Definitions LGBTIQ Intersex The vogue term for hermaphrodite. People born with the sexual characteristics of both sexes Questioning People who suspect they might be LGBT, but are not yet certain Queer Inclusive term of the LGBTIQ community Unique paradigm

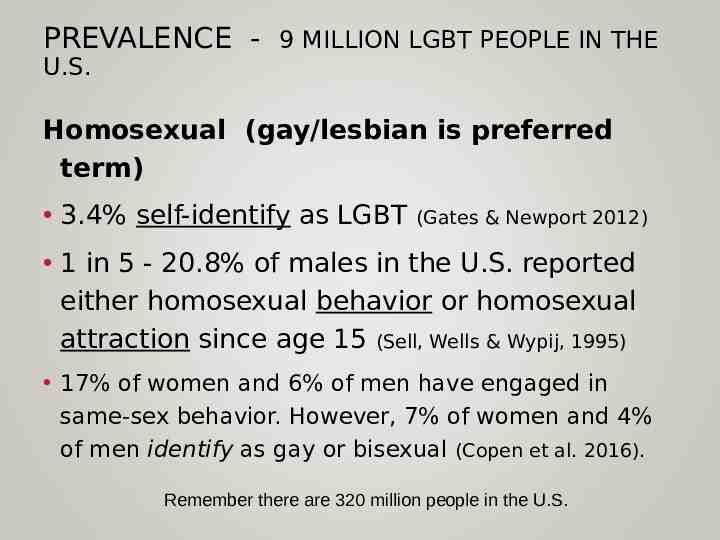
PREVALENCE - 9 MILLION LGBT PEOPLE IN THE U.S. Homosexual (gay/lesbian is preferred term) 3.4% self-identify as LGBT (Gates & Newport 2012) 1 in 5 - 20.8% of males in the U.S. reported either homosexual behavior or homosexual attraction since age 15 (Sell, Wells & Wypij, 1995) 17% of women and 6% of men have engaged in same-sex behavior. However, 7% of women and 4% of men identify as gay or bisexual (Copen et al. 2016). Remember there are 320 million people in the U.S.
TRANSGENDER POPULATION SIZE 1.4 million adults self-identify as trans in the U.S. Crissman et al. 2017; Flores et al., 2016; Meerwijk & Sevelius, 2017

GENDER NON-CONFORMITY OR GENDER DYSPHORIA GENDER NONCONFORMITY GENDER DYSPHORIA the extent to which a person’s gender identity, role, or expression differs from the cultural norms prescribed for people of a particular sex (IOM, 2011 definition) discomfort or distress that is caused by a discrepancy between a person’s gender identity and that person’s sex assigned at birth (and the associated gender role and/or primary and secondary sex characteristics) (WPATH, 2011)

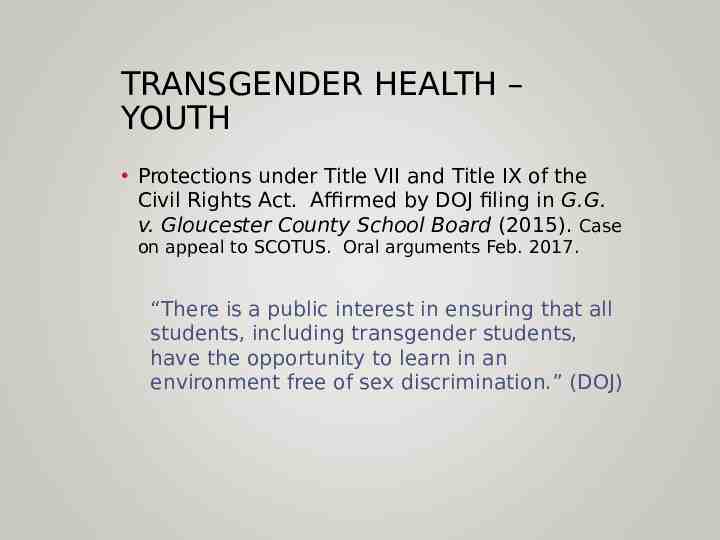
TRANSGENDER HEALTH – YOUTH Protections under Title VII and Title IX of the Civil Rights Act. Affirmed by DOJ filing in G.G. v. Gloucester County School Board (2015). Case on appeal to SCOTUS. Oral arguments Feb. 2017. “There is a public interest in ensuring that all students, including transgender students, have the opportunity to learn in an environment free of sex discrimination.” (DOJ)
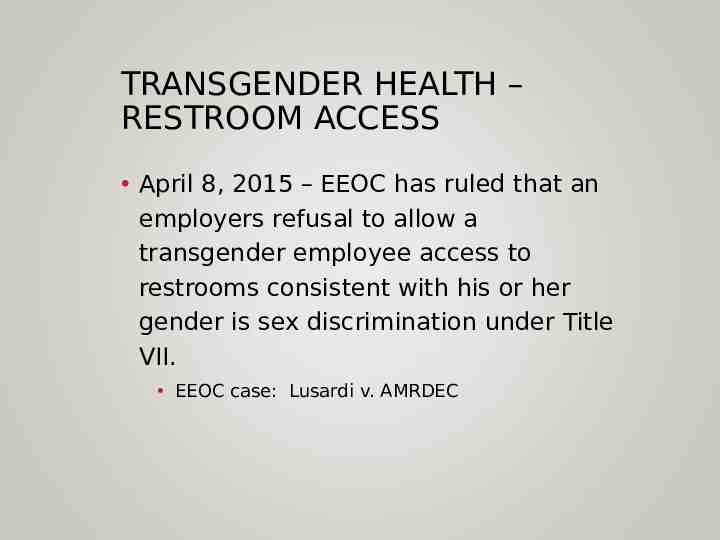
TRANSGENDER HEALTH – RESTROOM ACCESS April 8, 2015 – EEOC has ruled that an employers refusal to allow a transgender employee access to restrooms consistent with his or her gender is sex discrimination under Title VII. EEOC case: Lusardi v. AMRDEC
WHAT ABOUT SCHOOL? TITLE IX Title IX protects students, faculty and employees from sex discrimination in any federally funded education program or activity. However schools are still not safe.

EARLY SOCIAL TRANSITION Child lives as gender that matches their identity Trial run - name, attire, social roles at school, in community Reversible Family decision whether to disclose to others or not Approx. 25% of children who were assessed for gender dysphoria grew up to be cis-gender gay vs. transgender.

CHILDREN AND YOUTH EARLY medical and mental health services Family support is critical to positive health outcomes Puberty experienced congruent with gender (delay until sure) Reduces need for later medical interventions Prevents unwanted sex characteristics (i.e. breasts) Decreases stress, anxiety, depression

REPARATIVE THERAPY Efforts to change the sexual orientation or gender identity Condemned by all mainstream professional organizations as harmful including the APA, AMA, Am Acad of Pediatrics, AAN, ISPN etc. Related to depression, anxiety and suicide George Rekers (prof emeritus from USC SOM) – published case where he conducted reparative therapy. This is what he did .

PUBERTY BLOCKING – GNRH AGONISTS Ideally begun in Tanner 2 stage (early start of puberty). Can begin in Tanner 3-5 – goal is to stop puberty/ prevent secondary gender characteristics i.e. height, breasts etc. GnRH Agonists - Leuprorelin; Triptorelin; Goserelin; Histrelin implants Very expensive. Cost is between 500 and 1500 month. Insurance rarely covers this cost Effects are totally REVERSIBLE

IRREVERSIBLE HORMONE EFFECTS ESTROGEN TESTOSTERONE Breast development Uterine atrophy Nipple enlargement Facial and body hair Loss of erection Deepened voice Testicular atrophy Clitoral enlargement ? sterility ? sterility

FIRST DO NO HARM . There is harm related to NOT intervening Suicide 44% Depression Anxiety Homelessness ETOH, drug use Sex work HIV

OVERREPRESENTED HEALTH PROBLEMS HIV/ AIDS Trauma/ Victimization Mental Health Concerns Addictions Is this because they’re LGBT? –or- because of the context within which LGBT people must exist?

HIV/ AIDS A missing generation of gay men due to AIDS HIV the norm in some areas Homelessness/ poverty – survival sex Street hormones (trans)

TRAUMA/ VICTIMIZATION Parental abuse Increased prevalence of verbal and physical abuse and heightened suicidal ideation among those who disclosed their s.o. to their families Hate crimes

MENTAL HEALTH – DEPRESSION & ANXIETY Additional stress d/t image management related to s.o./g.i. LGBT children often grow up in a society that says that they should not exist and/or should not act on their feelings. These societal mores can be internalized internalized homophobia

DEPRESSION Prevalence of depression 17.2% higher than in U.S. adult men in general Distress & depression associated w/: lack of a partner; not identifying as gay, queer, or homosexual; experiencing multiple episodes of antigay violence in the previous 5 years; and very high levels of community alienation Mills 2004

LGBT YOUTH VICTIMIZATION 25% of gay youth (16% lesbian) have been threatened or injured with a weapon on school property. 3x higher than hetero rate for boys; 4x higher than hetero for girls. 13% gay (16% lesbian) youth didn’t go to school because of safety issues (O’Malley, 2014) 3x the hetero rate Sample was of YRBS HS students

MENTAL HEALTH - SUICIDE LGB youth 30% attempted suicide (double the hetero rate) School bullying increased the risk of suicide (Bouris et al, 2016)

TRANSGENDER SUICIDE U.S. TRANS/GQ DATA

ADDICTIONS Young LGBT (most prevalent) Lesbian/ female Bi – principally ETOH Gay/ MtF Transgender – Ecstasy (and other Rave drugs) Risk hyperthermia; Poppers (amyl nitrate) – enhanced sexual experience Risk an MI, priapism Ecstacy: MDMA

CDC RECOMMENDATIONS FOR SCHOOLS TO SUPPORT LGBTQ HEALTH 1. Identify “safe spaces” 2. Prohibit harassment and bullying 3. Facilitate access to health & psych providers not on school property who are LGBTQ affirming 4. Encourage professional development on safety for all students 5. Provide health education curricula with inclusive terminology Demisse et al., 2013

CASE 1 A 15yo questioning female student presents to the school nurse asking him to sponsor a Gay Straight Alliance (GSA) at their school. The best school nurse answer: A. “yes, of course I’ll sponsor a GSA” B.“I’d like to but I’ll need to talk to the principal first” C.“I think I’d like to talk to your parents first – we’ll be back in touch” D.“You really need to talk to our school psychologist about this”

SC CODE 59-32-30A(5) LOCAL SCHOOL BOARDS TO IMPLEMENT COMPREHENSIVE HEALTH EDUCATION PROGRAM; GUIDELINES AND RESTRICTIONS (5) The program of instruction provided for in this section may not include a discussion of alternate sexual lifestyles from heterosexual relationships including, but not limited to, homosexual relationships except in the context of instruction concerning sexually transmitted diseases.

CASE 2 30yo transman who initiated social gender affirmation 5 years ago, chest construction at 25yo, testosterone from 25-28yo. He grew a beard and stopped taking T. Beard growth persisted. No menstruation for 5 years. He would like the option to become pregnant in the future because he wants children but has legal concerns related to adoption. As the NP you first: A.Conduct an exam and draw labs B.Conduct an exam, draw labs and refer to endocrinology C.Conduct an exam, draw labs and refer to GYN

YOUR PATIENT WANTS TO TRANSITION – NOW WHAT?The pdf is free 1. Google “WPATH Guidelines” 2. Refer to a Psych NP or other mental health provider 3. Start hormone therapy www.wpath.org

RESEARCH ON HORMONES – IS IT SAFE? FTM MTF No increase in CAD found in 876 FTM pts (Gooren, 200) Increased risk of CAD at high doses. Increased risk of CA at low doses If prior MI – PO estradiol does not incr. or decr. risk for further emboli

WPATH Standards of Care The criteria for hormone therapy are as follows: Persistent, well-documented gender dysphoria; Capacity to make a fully informed decision and to consent for treatment; Age of majority in a given country (if younger, follow the Standards of Care outlined in section VI); If significant medical or mental health concerns are present, they must be reasonably well controlled

HORMONES Rx information taken from Cavanaugh 2016 FTM - OPTIONS Injectable Testosterone Testosterone Enanthate or Cypionate 100-200 mg IM q 2 wks (20 -22g x 1 ½” needles) Transdermal Testosterone Androderm TTS 2-8mg daily Topical testosterone gels in packets and pumps, multiple formulations (Testim, Androgel) 5 to 10 gm (50 to 100 mg of testosterone) applied topically daily Axiron 2% pump gel for axillary application 1 pump to each axilla daily Testosterone Pellet Testopel- implant 6-10 pellets q 3 to 6 months Buccal Testosterone Striant 30 mg buccal system q 12 hours

TESTOSTERONE RISKS HDL triglycerites insulin resistance sleep apnea Infertility Mental health changes MONITORING Baseline CBC, CMP, lipids, renal panel, fasting glucose 3 month, then Q 6-12 mo CBC, liver enzymes, serum testosterone Q 6-12 mo Lipid profile, HbA1c

HORMONES MTF OPTIONS Oral Estrogen Estradiol (estrace) 2-6mg PO or SL daily(can be divided into BID dosing) Premarin (conjugated estrogens) 1.25-10mg PO daily (can be divided into BID dosing) Transdermal estrogen (preferred for 40yo) Estradiol patch 0.1-0.4mg twice weekly Injectable Estrogens [NOTE – shortage right now] Estradiol valerate5-20mg IM q2 weeks Estradiol cypionate2-10mg IM weekly Antiandrogens Spironolactone (aldactone) 50-400mg PO daily (can be divided into BID dosing) Finasteride (Proscar) 2.5-5mg PO daily Progestins – increase breast development, but CV risk, weight gain & depression

MTF – ESTROGEN RISKS MONITORING CAD weight triglycerides Baseline – CBC, CMP, lipids, renal, fasting glucose, testosterone, prolactin libido glucose tolerance Gallbladder ds Infertility Mental health changes Spronolactone carries risks of hypotension, hyperkalemia and renal insufficiency 6mo. – serum testosterone & estradiol If on spironolactone 1 mo. then 3mo. – lipids, lytes, creatinine, glucose

MTF SURGICAL OPTIONS ( 30%) Removal of scrotum & penis Creation of vagina, labia, clitoris & mons Breast augmentation Tracheal shave Facial feminization Brow nose Taken from Schechter 2017 p.37

FTM SURGICAL OPTIONS ( 30%) Phalloplasty with urethral reconstruction & creation of scrotum (uncommon) Chest reconstruction
STAGED SURGERIES Genital FtM Tissue removal from donor site Urethral reconstruction Implant prosthesis Chest Contouring FtM Mastectomy Revision of prior surgery to decrease scarring and remove arm flaps

YOU’RE AN ORG LEADER/ MANAGER WHAT CAN YOU DO? Know the law and standards related to LGBTQ patients Train your staff – receptionist to CNO Work on the culture of your organization to make it safe.

Joint Commission Standards (2011) The patient-centered communication standards for Hospitals (CAMH). Elements of performance 28 and 29 under RI.01.01.01, require access to a support person and non-discrimination of care. The Joint Commission: Advancing Effective Communication, Cultural Competence, and Patient- and FamilyCentered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community: A Field Guide. Oak Brook, IL, Oct. 2011. LGBTFieldGuide.pdf.

RI.01.01.01 ELEMENT 29 “No longer considered to be simply a patient’s right, effective communication is now accepted as an essential component of quality care and patient safety.”

HOSPITAL VISITATION January 2010 Centers for Medicare and Medicaid Services (CMS) regulation required hospitals to permit patients to designate visitors & prohibits discrimination in visitation based on so/gi. 42 C.F.R. § 482.13 Compliance with requirements for Medicare Conditions of Participation (CoPs)

HOSPITAL VISITATION July 2011 Joint Commission standard – prohibition on discrimination based on orientation or gender identity. “Prohibit discrimination based on age, race, ethnicity, religion, culture, language, physical or mental disability, socioeconomic status, sex, sexual orientation, and gender identity or expression.” RI.01.01.01 EP29 (p.48 of Joint Commission LGBT doc).

CMS – EQUAL COVERAGE TO CARE IN THE SAME NURSING HOME AS A SPOUSE Aug. 29, 2013 - CMS announced the guarantee of Medicare coverage applies to ALL spouses regardless of sexual orientation. Prior to this same-sex spouses with Medicare Advantage plans were not eligible to live in the same nursing home as their spouse.

FMLA All spouses are now covered under FMLA if the employer is FMLA covered. (3/15 injunction against same sex spouses dissolved by SCOTUS Obergefell ruling) FMLA may be used for The birth of a child, adoption or foster parent; To care for a spouse, son, daughter, or parent who has a serious health condition; For a serious health condition that makes the employee unable to perform the essential functions of his or her job; or For any qualifying exigency arising out of the fact that a spouse, son, daughter, or parent is a military member on covered active duty or call to covered active duty status. http://www.dol.gov/whd/regs/compliance/whdfs28.pdf

AFFORDABLE CARE ACT Section 1557 – Civil Rights provisions of the Act. Applies civil rights protections to the Health Insurance Marketplace created by the ACA – and includes LGBT people

ACA & PREVENTIVE CARE May 2015 DOL Guidance on the ACA confirms Plans cannot limit sex-specific preventive services by gender identity. If a provider orders the service it is considered appropriate. http://www.dol.gov/ebsa/faqs/faq-aca26.html

THE LAW SC ANTI- TRANSGENDER BILL S.1203 defeated May 4, 2016 TITLE VII - EEOC Macy v. Holder (EEOC, 2012) – gender non-conformity gender. TITLE IX EDUCATION Grimm v. Glouchester (2015) Appealed to SCOTUS Administrative guidance

HOW DO I FIND AN AFFIRMING PROVIDER? GLMA.org Then click on: Resources – For Patients – Find a Provider A searchable provider directory (location, specialty, transition care etc.). Provider Directory at the Harriet Hancock LGBT Center

RESOURCES Locally Harriet Hancock LGBT Center IRIS LGBT group on campus Nationally The Trevor Project – suicide hotline for LGBT youth www.thetrevorproject.org 1-866-488-7386 Trans Lifeline http://www.translifeline.org 1-877-565-8860 Providers GLMA.org https://glmaimpak.networkats.com/members online new/members/dir prov ider.asp

HOW CAN AN LGBT PERSON KNOW IF SOMEONE IS SAFE TO TALK TO? Go with your instincts If you get a bad vibe from someone – trust your instincts and get out of there. Look for these symbols

WHAT WE CAN DO AS NURSES Be Authentic Encourage Authenticity in others Share Be flexible, scootch over a little, share the bench share the power

LAURA C. HEIN PHD, RN, FAAN [email protected]