Perioperative Surgical Home Model Julie Sheedy DNP, MSN, NE-BC,RN
46 Slides6.35 MB
Perioperative Surgical Home Model Julie Sheedy DNP, MSN, NE-BC,RN Administrator March 9, 2019
Agenda Welcome Overview of TriHealth TriHealth Surgical Home Data Collection Lessons Learned Future state Closing

TriHealth At A Glance Four acute-care hospitals with 900 adult-staffed beds One short-stay surgical hospital Two free-standing outpatient surgery centers Over 140 outpatient service locations Over 150 physician practice locations Over 850 employed physicians Over 1,800 physicians on medical staff Over 12,000 employees

TriHealth Awards for Clinical Quality, Technical Excellence and Employee Engagement

TriHealth Awards for Clinical Quality, Technical Excellence and Employee Engagement Healthcare Information and Management System Society (HIMSS) Analytics Electronic Medical Record (EHR) Adoption Model Stage 7 Awarded to TriHealth successfully TriHealth July 2014 recertified as HIMSS Stage 7 in December 2017

TriHealth Surgical Optimization Center Recognition Nationally Recognized by ASA as Industry Leading Innovator Award Nationally Recognized by Studer Group What’s Right in Healthcare Nationally Recognized by ASPAN as First Place Winners

Local Problem Increased LOS Patient outcomes were being impacted due to: Clinical variation Lack of coordinated care Patient disconnected from primary care provider Causing: Increased costs Inconsistent patient experience Surgery Delays /Cancellation s Increased Readmissions Preventable Complications Lower Patient Satisfaction Higher Cost Per Care
Perioperative Learning Collaborative Premier Learning Collaborative is physician-led that brings health systems and clinical leaders together to challenge perceptions and practices related to improvement solutions. Leveraging the power of peer-to-peer learning, data-enabled decision making and innovation to evaluate new cost and quality improvements. Over 80 hospitals are participating and sharing best practices TriHealth chose to participate in the National Perioperative Learning Collaborative and pilot a perioperative surgical home program. 8
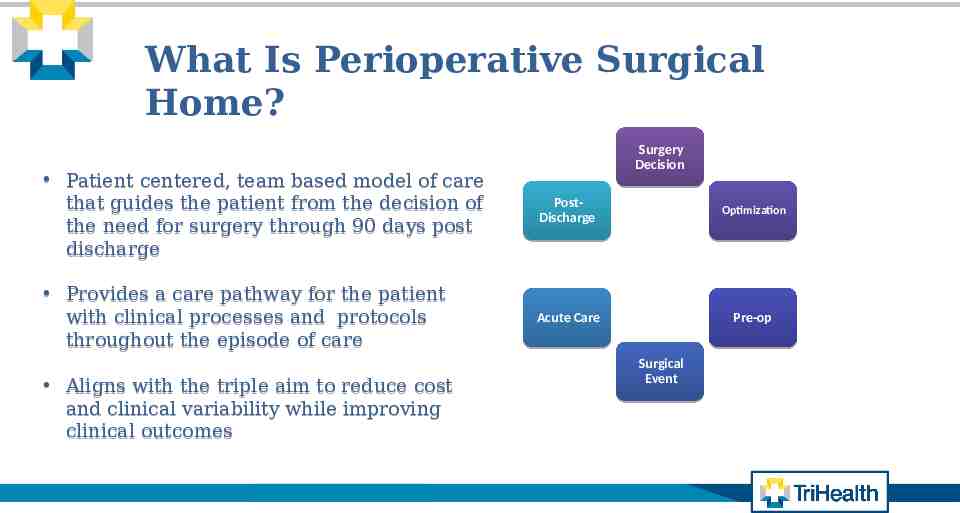
What Is Perioperative Surgical Home? Surgery Decision Patient centered, team based model of care that guides the patient from the decision of the need for surgery through 90 days post discharge PostDischarge Optimization Provides a care pathway for the patient with clinical processes and protocols throughout the episode of care Acute Care Pre-op Aligns with the triple aim to reduce cost and clinical variability while improving clinical outcomes Surgical Event

Transforming Pre-Surgical Services Surgical cases account for 50% of readmissions Current state contributes to excessive expenditures (labs, cardiac clearance, productivity) Duplicate and unnecessary testing Fragmentation falls short of meeting patients needs

PSH Perioperative Clinic Patient Reported Outcomes (PROs)* Identification of risk through screening Chronic disease Management Holistic Management of the patient

TriHealth Surgical Optimization Center (TSOC) Admission through a centralized clinic Early preadmission assessments/risk stratification Centralized systems to gather health information “Prehabilitation” programs Multidisciplinary team based care to coordinate/navigate complex patients prior to surgery Support healthy surgical candidate with a standardized process

Solution Selection Process Colorectal as the Preferred Service Line Manageable volume ( 3oo patients) Cohesive and collaborating group of physicians and team members Looking for an engaged service line that would allow us to stand up a successful model that could be extended and repeated across the enterprise. 13

Where We Started March 2016 – February 2017 Average Length of Stay 8.2 Days Surgical Site Infections 21 Delayed Cases 9 % Readmission 14.00% Average Cost Per Case 11,693 Overall Patient Experience (Top Box) 72.50%

Governance and Clinical Decision PSH Core Group Making Dr. Matt Schantz, Dr. Elsass, Dr. Kirkpatrick, Dr. Guend, Mary Pat Gilligan, Julie Sheedy, Diana Smith, Judie Conley Surgery Decision Optimization Preop Day of Surgery Intraoperative PACU Acute Phase of Care Discharge Data Analytics Education Communication Anesthesia : Dr. Schantz/Dr. Elsass Anesthesia : Dr. Schantz/Dr. Elsass Anesthesia: Dr. Burgess Anesthesia : Dr. Schantz/Dr. Elsass Surgeon: Dr. Kirkpatrick & Dr. Guend Surgeon: Dr. Maynard Surgeon: Dr. Kirkpatrick Surgeon: Dr. Guend Surgeon: Dr. Kirkpatrick Clinical Lead: Lisa Hess & Lori Vernon Clinical Lead: BN/GS SDS Managers & OR Managers Clinical Lead: Carolyn Hoenicke Clinical Lead: Lisa Hess & Lori Vernon IT Lead: Mufaddal Frosh & Diana Smith Clinical Lead: Sue Sandsone PSS/PAT RN: 2 BN & 2 –GS SDS/OR RN: 2 BN & 2 –GS PACU/IP RN: 2 BN & 2 –GS Care Coordinator: Heidi Loughran Data Analytic Lead: Patrick Haney Marketing & Communications IT: Lindsey Satterfield & Chris Cionni IT: Shara Jenkins & Jennifer Grice IT: Lindsey Satterfield & Chris Cionni IT: Thomas Hester IT: Lisa Sheppard & John Montavon IT: Lindsey Satterfield & Chris Cionni Clinical Informatics: Sharon Hafertepe & Meg Howes Clinical Informatics: Clinical Informatics Clinical Informatics: Tracey Bracke & Beth Angst Sherri Chenault & Patti Burke Anesthesia : Dr. Schantz/Dr. Elsass Anesthesia : Dr. Elsass Surgeon: Dr. Kirkpatrick Educators: Patrick Bobst & Amy Orr Educators

Intended Outcomes Preoperative - Improved patient experience - Managed comorbidities - Reduce clinical variation - Transitional Care Planning Reduc e Cancel s Intraoperative - Reduce clinical variation - Operational efficiencies Postoperative - Right level of care - Integrated pain management - Prevention of complications Long Term Recovery - Coordinated discharge plan - Educate patient and care givers - Transition to appropriate level of care - Rehabilitation and return to function

Intended Outcomes Preoperative - Improved patient experience - Managed comorbidities - Reduce clinical variation - Transitional Care Planning Reduc e Cancel s Intraoperative - Reduce clinical variation - Operational efficiencies Reduc e Cost Postoperative - Right level of care - Integrated pain management - Prevention of complications Long Term Recovery - Coordinated discharge plan - Educate patient and care givers - Transition to appropriate level of care - Rehabilitation and return to function

Intended Outcomes Preoperative - Improved patient experience - Managed comorbidities - Reduce clinical variation - Transitional Care Planning Reduc e Cancel s Intraoperative - Reduce clinical variation - Operational efficiencies Reduc e Cost Postoperative - Right level of care - Integrated pain management - Prevention of complications Reduc e SSI Long Term Recovery - Coordinated discharge plan - Educate patient and care givers - Transition to appropriate level of care - Rehabilitation and return to function

Intended Outcomes Preoperative - Improved patient experience - Managed comorbidities - Reduce clinical variation - Transitional Care Planning Reduc e Cancel s Intraoperative - Reduce clinical variation - Operational efficiencies Reduc e Cost Postoperative - Right level of care - Integrated pain management - Prevention of complications Reduc e SSI Long Term Recovery - Coordinated discharge plan - Educate patient and care givers - Transition to appropriate level of care - Rehabilitation and return to function Reduc e Readm it

Optimization Phase Surgeon referral to TSOC Nurse Practitioner identify for pre-risk screening Obtain anesthesia consults Perform H&P’s when necessary Determine course of treatment based on labs and EKG

Optimization Phase Nurse Navigators obtain surgical referral Perform chart review within 48-72 hours Phone encounter to determine clinical needs Conduct Optimization protocols Perform optimization visit for education and necessary services Follow-up with surgical patients 6 days out

Optimization Protocols Anemia Protocol Anticoagulation Pathway Diabetes Protocol Enhance Recovery Protocol Fraility Nutritional Pathway Obstructive Sleep Apnea Smoking Cessation

Implications of Frailty for the Surgical Patient - Frailty in non emergent surgery predicts: - 2.5 fold increased risk of postop complications 1.7 fold increase in LOS 20 fold increase in discharge to not home Frailty in emergency surgery: 11 fold increase in mortality Makary J Am Coll Surg 2010 Farhat J Trauma Acute care Surg 2012 Kim JAMA Surg 2014 23

Therapy order management 24

Referral for Diabetes Education 25

TSOC Communication Tools 26

Intraoperative Phase Multi-modal pain management Fluid management Standardization of surgical technique

Postoperative Phase Pain management plan of care Early mobilization Care transition to home Discharge protocols Multi-disciplinary approach with patient and family

Post-Discharge Phase Nurse Care Guide established to care manage patient 90-days post-discharge Developed registries to identify patients Utilized EMR documentation to standardize follow-up care Patient Experience Survey at day two and day 10

TSOC Inclusion TSOC Inclusion Patient Flagging BPAs Clinical Workflow Optimization Clinical Pathway Pathway Review Physician Workflow Optimization Documentation Reporting Tools

Flagging Patient As TSOC TSOC Inclusion Patient Flagging BPAs Clinical Workflow Optimization Clinical Pathway Pathway Review Physician Workflow Optimization Documentation Reporting Tools

Best Practice Alerts TSOC TSOC Inclusion Inclusion Patient Patient Flagging Flagging BPAs BPAs Clinical Clinical Workflow Workflow Optimization Optimization Clinical Clinical Pathway Pathway Pathway Pathway Review Review Physician Physician Workflow Workflow Optimization Optimization Documentation Documentation Reporting Reporting To Tools ols

Post-Discharge Documentation TSOC Inclusion Patient Flagging BPAs Clinical Workflow Optimization Clinical Pathway Pathway Review Physician Workflow Optimization Documentation Reporting Tools

TSOC Dashboard Reports TSOC Inclusion Patient Flagging BPAs Clinical Workflow Optimization Clinical Pathway Pathway Review Physician Workflow Optimization Documentation Reporting Tools

TSOC Dashboard Reports TSOC Inclusion Patient Flagging BPAs Clinical Workflow Optimization Clinical Pathway Pathway Review Physician Workflow Optimization Documentation Reporting Tools

TSOC Dashboard Reports TSOC Inclusion Patient Flagging BPAs Clinical Workflow Optimization Clinical Pathway Pathway Review Physician Workflow Optimization Documentation Reporting Tools

TSOC Dashboard Reports TSOC Inclusion Patient Flagging BPAs Clinical Workflow Optimization Clinical Pathway Pathway Review Physician Workflow Optimization Documentation Reporting Tools

Quality Outcomes Response rate: 84% 218/260 returned survey Compliance with IT Tools: 100% of Colo-rectal patients followed the TSOC clinical pathway Total volume: 260 cases Increased Overall Patient Satisfaction 76% to 83% No Case Cancellations

Quality Outcomes 67% overall reduction in SSI Source: HDM – Clinical Quality Dept 5.8% overall reduction in ALOS Source: TH TSOC Dashboard & Decision Support Financial Data Warehouse
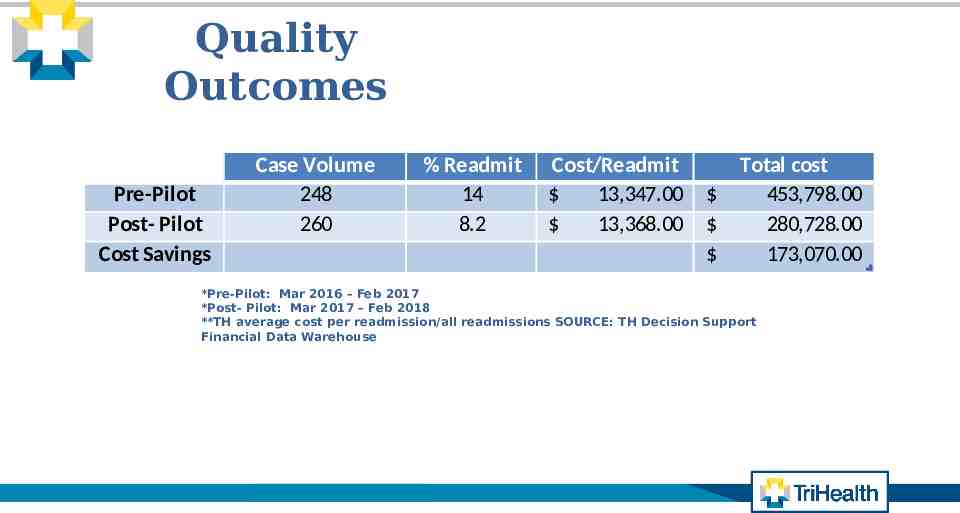
Quality Outcomes Column1 Pre-Pilot Post- Pilot Cost Savings Case Volume 248 260 % Readmit 14 8.2 Cost/Readmit 13,347.00 13,368.00 Total cost 453,798.00 280,728.00 173,070.00 *Pre-Pilot: Mar 2016 – Feb 2017 *Post- Pilot: Mar 2017 – Feb 2018 **TH average cost per readmission/all readmissions SOURCE: TH Decision Support Financial Data Warehouse

Overall Project Outcomes 2017 2018 Length of Stay 8.2 4.8 Surgical Site Infection 21 8 9 0 14% 8.2% Patient Experience Survey 72.5% 83% Financial 11,693 10,586 Delayed Cases Readmission (Average cost per patient)

Soft & Hard ROI for TSOC Reduced Readmission 173,070 Reduced SSI Cost 14,365 Cost Avoidance for Canceled Cases1 66,960 Reduced Cost Per Case 287,820 Total ROI 542,215

Keys to Success Team Member Engageme nt Culture of Partnershi p Keys to Succes s Informatio n System is Seen as Part of the Care Team MultiDisciplinar y care team 43

Lessons Learned Establish a steering group to oversight of the program. Keep the scope tight and cohesive. Select strong operational team members. Ongoing meetings to identify progress, barriers and challenges. Collaboration and team work respect and appreciation for all perspectives. Delivering a product that is a patient centered and a multidisciplinary approach. Celebrate wins! 44

What’s Next Expanding TSOC and Clinical Pathways Additional service lines: o o o o Ventral Hernias went live November 2018 Spine scheduled late spring Urologic Gynecology Urology Future Increase patient engagement via MyChart questionnaires Improve patient experience through text-messaging Enhance data collection Integrate Clinical Pathways into the Discharge Care Guide’s role Refine and expand implications in addressing patients at risk for readmission to the hospital

QUESTIONS 46