MassHealth: The Basics FACTS AND TRENDS UPDATED OCTOBER 2023 Robert W.
43 Slides1.63 MB
MassHealth: The Basics FACTS AND TRENDS UPDATED OCTOBER 2023 Robert W. Seifert Consultant OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE

TABLE OF CONTENTS GLOSSARY OF ACRONYMS 2 INTRODUCTION 3 ELIGIBILITY AND ENROLLMENT 7 BENEFITS AND DELIVERY SYSTEMS 16 SPENDING AND COST DRIVERS 25 REFORMS 35 CONCLUSION 39 DESIGN: www.StudioADesign.com OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 2

GLOSSARY OF ACRONYMS ACA Affordable Care Act FSP Flexible Services Program ACS American Community Survey HCBS Home- and Community-Based Services ACO Accountable Care Organization LTSS Long-Term Services and Supports CHIP Children’s Health Insurance Program MCO Managed Care Organization CMS Centers for Medicare and Medicaid Services PACE Program of All-Inclusive Care for the Elderly CBHC Community Behavioral Health Center PCC Primary Care Clinician Plan CP Community Partner Per Member Per Month CSP Community Support Program PMP M FBR Federal Benefit Rate SCO Senior Care Options FFS Fee-For-Service SFY State Fiscal Year (July 1–June 30; for example, SFY22 runs from July 1, 2021– June 30, 2022) STPH H Short-Term Post-Hospitalization Housing SNAP Supplemental Nutrition Assistance Program SSI Supplemental Security Income FMAP Federal Medical Assistance Percentage FPL OCTOBER 2023 Federal Poverty Level MASSACHUSETTS MEDICAID POLICY INSTITUTE 3

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION INTRODUCTION OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 4

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION INTRODUCTION: THE IMPORTANCE OF MASSHEALTH MassHealth is Massachusetts’ name for its Medicaid program and Children’s Health Insurance Program (CHIP). MassHealth is a cornerstone of the health insurance landscape in Massachusetts and critical to the state’s high rates of coverage and ongoing efforts to improve equity. The program is jointly funded and administered by state and federal governments. COVERAGE Nearly one in three Massachusetts residents is covered by MassHealth over 2 million people including low-income children, seniors, and people with disabilities. EQUITY MassHealth members are representative of the diversity of the Commonwealth and so the program is positioned to help address disparities for people across disability status, racial and ethnic identities, sexual orientation, and gender identities. OCTOBER 2023 SAFETY NET Enrollment typically grows during recessions when people are losing jobs. MassHealth helps keep Massachusetts’ coverage rates high through crises such as the COVID-19 pandemic. INNOVATION MassHealth is implementing health policy reforms including new service models that address social determinants of health and payment models that reward performance over volume. MASSACHUSETTS MEDICAID POLICY INSTITUTE 5

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH: THE BASICS KEY FINDINGS ENROLLMENT 2020 2022 Enrollment grew sharply during the COVID-19 pandemic but is expected to shrink by about 300,000 in the coming year Children, seniors, and people with disabilities make up 57% of MassHealth members SPENDING 2020 * 2022 Total MassHealth spending increased as enrollment increased from SFY 2021 to SFY 2022*, but the cost per member did not increase BENEFITS AND DELIVERY More SYSTEMS than two-thirds of MassHealth members are enrolled in managed care, with over half of members enrolled in Accountable Care Organizations (ACO) For some members, ACOs offer housing and nutrition supports through the Flexible Services Program and care coordination though Community Partners 61% of spending on Long Term Services and Supports (LTSS) is for community-based care, helping MassHealth members remain in their homes REFORMS MassHealth is pursuing new approaches for improving health equity, including holding hospitals financially accountable for measuring and reducing disparities MassHealth continues to improve the member experience for those with the most complex needs and to address certain health related social needs (such as food security) known to impact health MassHealth has expanded its range of behavioral health services, including access to urgent behavioral health care and supportive services provided by people with lived experience State Fiscal Year (SFY) 2021 starts 7/1/2020 and ends on 6/30/2021. SFY 2022 starts on 7/1/2021 and ends on 6/30/2022. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 6

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION ELIGIBILITY AND ENROLLMENT OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 7

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH IMPROVES ACCESS TO COVERAGE AND HEALTH OUTCOMES Massachusetts expanded MassHealth over the course of decades. These expansions have given researchers opportunities to study the effects of MassHealth on access to coverage, care, and health outcomes. In 1997, Massachusetts expanded MassHealth eligibility to more adults and children. 1997 IMPACTS: A dramatic drop in the uninsured rate, for both adults and children.1 The percentage of people entering substance use disorder treatment programs with MassHealth coverage rose 21%.2 1 2 3 4 In 2006 a comprehensive package of reforms expanded MassHealth eligibility again. These reforms also made subsidized coverage available through the Health Connector (Massachusetts’ statebased health insurance marketplace) and implemented insurance mandates for individuals and employers. 2006 2018 IMPACTS OF MASSHEALTH EXPANSION ASSOCIATED WITH: A more than 5 percentage point drop in the uninsured rate among children eligible for MassHealth.3 IMPACTS OF MASSHEALTH EXPANSION, IN COMBINATION WITH OTHER 2006 REFORMS, ASSOCIATED WITH: A drop of 50%, or almost 3 percentage points, in the uninsured rate for all Massachusetts children.3 Massachusetts becoming the state with the highest rate of insurance among all states.4 Measurable improvements in physical and mental health for adults and children.4 Increased use of preventive care for Zuckerman, S., Kenney, G.M., Dubay, L., Haley, J., & Holahan, J. (2001). Shifting Health Insurance Coverage, 1997–1999. Health Affairs, (1). adults and children (pap 20 screening, Zur, J. & Moitabai, R. (2013). Medicaid Expansion Initiative in Massachusetts: Enrollment Among Substance-Abusing Homeless Adults. AJPH, 103 (11). cholesterol testing, colonoscopies, pediatric Kenney, G. M., Long, S. K., & Luque, A. (2010). Health reform in Massachusetts cut the uninsurance rate among4children in half. Health Affairs, 29 (6), 1242–1247. checkups). Love, K.A. & Seifert, R.W. (2016). 10 Years of Impact: a Literature Review of Chapter 58 of the Acts of 2006. Blue Cross Blue Shield Foundation of Massachusetts; LOOKING AT THE MASSACHUSETTS POPULATION IN MORE RECENT YEARS, MASSHEALTH COVERAGE IS ASSOCIATED WITH: Financial protection and increased affordability for health insurance and care.5 Miller, S. (2012). The Impact of the Massachusetts Health Care Reform on Health Care Use among Children. American Economic Review, 102 (3). 5 Long, S.K., Aarons, J. (2018). Massachusetts Health Reform Survey. Blue Cross Blue Shield Foundation of Massachusetts. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 8

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH INCOME LIMITS VARY FOR DIFFERENT AGES AND ELIGIBILITY GROUPS1 MassHealth Standard MassHealth CommonHealth FPL2 MassHealth CarePlus MassHealth Family Assistance ConnectorCare (state supplement to federal subsidy for insurance purchased through Health Connector) 400% MAY BE ELIGIBLE FOR ADVANCE PREMIUM TAX CREDITS FOR A QUALIFIED HEALTH PLAN 300% 250% 223% 200% 300% 300% 300% 200% 150% 133% 0% NO UPPER LIMIT NO UPPER LIMIT 200% 1–18 19–20 DISABLED CHILDREN & YOUNG ADULTS THROUGH AGE 20 AGE IN YEARS NO UPPER LIMIT 300% FORMER FOSTER CARE YOUTH UP TO AGE 26 300% 300% 250% 300% 223% 200% 133% 133% 133% 133% MEDICALLY FRAIL CAREPLUS WHO ELECT STANDARD HIV POSITIVE DISABLED PARENTS AND CARETAKER RELATIVES OF CHILDREN UP TO AGE 19 CHILDREN 1 300% 200% 150% 150% 0 300% 133% ALL PREGNANT INDIVIDUALS HOME- AND ALL AGES WITH COMMUNITYOTHER BREAST OR BASED (DO NOT MEET CERVICAL SERVICES CRITERIA FOR CANCER (HCBS) OTHER WAIVER GROUPS) GROUP 3 ADULTS AGES 21 THROUGH 64 MassHealth eligibility includes nuances not included in this chart; MassHealth staff can help determine eligibility. Additional information can be found at https://www.mass.gov/service-details/masshealth-coverage-types-for-individuals-and-families-including-people-with. 2 FPL income as percent of federal poverty level; in 2023, 100% FPL for an individual was 14,580 annually. 3 Eligibility for all Home- and Community-Based Waivers except one (the waiver for Young Children with Autism) is based on 300% of the Supplemental Security Income (SSI) Federal Benefit Rate (FBR). FBR is a metric used by the Social Security Administration and tied to the consumer price index. In 2023, 300% SSI FBR for an individual was 32,911 annually (226% FPL for an individual). NOTES: MassHealth Limited, not shown in this chart, provides emergency health services to people who, under federal law, have an immigration status that keeps them from receiving more services. Income eligibility for this population is similar to MassHealth Standard: 200% FPL for pregnant women and children up to age 1; 150% FPL for children ages 1–20 years; 133% FPL for adults ages 21–64. SOURCES: 130 C.M.R. §505; 130 C.M.R. §519; MassHealth (2023). Member Booklet for Health and Dental Coverage and Help Paying Costs. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 9
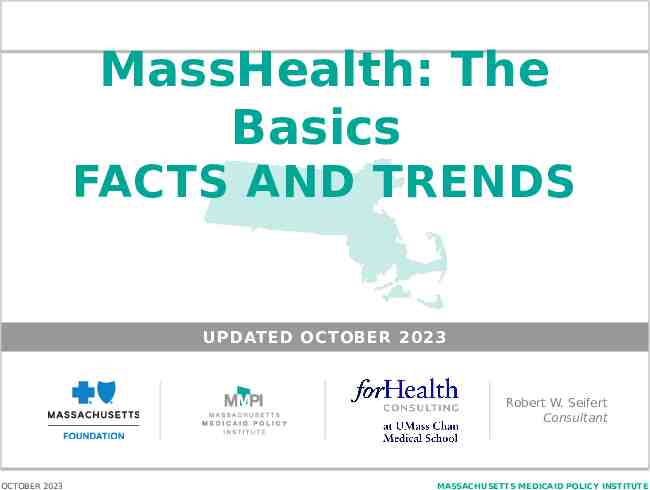
INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION ELIGIBILITY FOR SENIORS AGE 65 AND OLDER GENERALLY INCLUDES AN ASSET TEST AND LOWER INCOME THRESHOLDS; MOST SENIORS ALSO HAVE MEDICARE1 POPULATION INCOME/ASSETS2 COVERAGE Living in community, with or without Medicare eligibility, citizen or lawfully present immigrant 100% Federal Poverty Level (FPL) 2,000 Assets (for an individual) Comprehensive coverage through MassHealth Standard or Family Assistance (based on immigration status). For those with MassHealth Standard, MassHealth also pays their Medicare cost-sharing and premiums. Living in community, certain noncitizens 100% FPL 2,000 Assets (for an individual) MassHealth Limited — Emergency services only. Living in community, eligible for Medicare 190% FPL4 MassHealth Senior Buy-In — Covers Medicare premiums, co-pays, and deductibles. Does not cover other MassHealth Standard services. Living in community, eligible for Medicare 190% and 225% FPL Living in or waiting for facility-based long-term care No specific income limit 2,000 Assets (for an individual) MassHealth Buy-In — Covers Part B premiums only. 4 MassHealth Standard — Including LTSS. Member must pay income minus monthly allowances3 toward nursing facility care. 1 MassHealth eligibility includes nuances not included in this chart; for example, parents of minors and seniors who work have different eligibility requirements. MassHealth staff can help determine eligibility. 2 Certain assets are excluded from the asset test; these include principal home (in most cases), one vehicle, any loan or grant, life insurance cash-surrender value up to 1,500, and reserved funeral and burial funds up to 1,500. In certain cases, asset spend-down is available. Income and asset considerations are based in part on federal law. 3 Allowances include personal need allowance and spousal maintenance allowance, among others. 4 The SFY24 state budget eliminated an asset test that had previously applied to both MassHealth buy-in programs; this change will be effective following federal approval and issuance of state regulations. NOTES: Asset limits listed are for individuals; the amounts for couples are higher. Seniors (age 60 or older) can qualify for MassHealth through the Frail Elder Waiver with income up to 300% of the Supplemental Security Income (SSI) federal benefit rate (FBR) ( 32,911 for an individual in 2023). Other Home- and Community-Based Services (HCBS) waivers are available as well. Seniors may also be eligible for ConnectorCare and Advance Premium Tax Credits for insurance purchased through the Health Connector. SOURCES: 130 C.M.R. §519; MassHealth (2023). Senior Guide to Health Care Coverage, OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 10

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION THERE ARE MANY DOORS INTO MASSHEALTH Individuals apply directly, by phone, on paper form, in person with assistance at a MassHealth Enrollment Center or Health Connector walk-in center, or through the online application, an integrated eligibility system that allows users to shop and apply for MassHealth and other health insurance programs. Appeals and Grievances Health care providers assist patients with applications. Hospitals Community health centers Nursing facilities Other providers State agencies facilitate applications. Department of Developmental Services Department of Mental Health Massachusetts Rehabilitation Commission Department of Transitional Assistance Department of Children and Families Other agencies Community organizations and advocacy groups provide health care referrals and access to MassHealth. My Ombudsman. This nonprofit organization answers questions, provides information, and works with health plans and MassHealth to ensure members can access their benefits. Community action programs Community development corporations Aging services access points Health Care For All Other community organizations designated as Enrollment Assisters Typically, if an applicant disagrees with MassHealth’s denial of coverage, the applicant can appeal the decision within 30 days using the Fair Hearing Request Form. Applicants and members can also file grievances at any point for any type of problem, including issues with the quality of care, wait times, or customer service. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 11
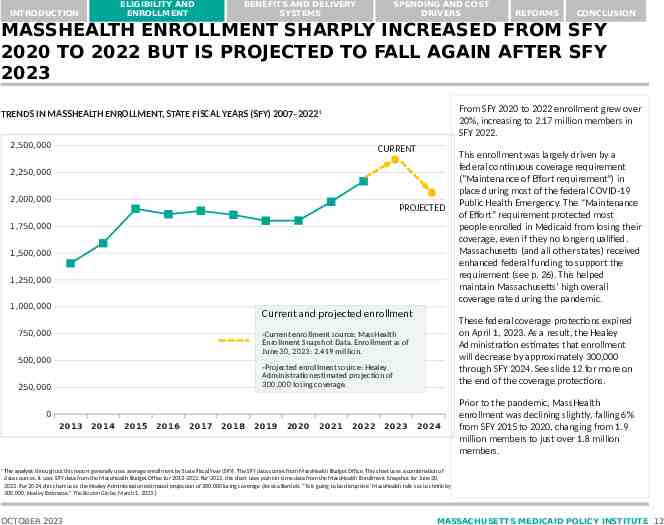
ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH ENROLLMENT SHARPLY INCREASED FROM SFY 2020 TO 2022 BUT IS PROJECTED TO FALL AGAIN AFTER SFY 2023 From SFY 2020 to 2022 enrollment grew over 20%, increasing to 2.17 million members in SFY 2022. TRENDS IN MASSHEALTH ENROLLMENT, STATE FISCAL YEARS (SFY) 2007–20221 2,500,000 CURRENT 2,250,000 2,000,000 PROJECTED 1,750,000 1,500,000 1,250,000 1,000,000 Current and projected enrollment 750,000 These federal coverage protections expired on April 1, 2023. As a result, the Healey Administration estimates that enrollment will decrease by approximately 300,000 through SFY 2024. See slide 12 for more on the end of the coverage protections. -Current enrollment source: MassHealth Enrollment Snapshot Data. Enrollment as of June 30, 2023: 2.419 million. 500,000 -Projected enrollment source: Healey Administration estimated projection of 300,000 losing coverage. 250,000 0 2013 1 2014 2015 2016 2017 2018 2019 2020 2021 2022 2023 This enrollment was largely driven by a federal continuous coverage requirement ("Maintenance of Effort requirement“) in place during most of the federal COVID-19 Public Health Emergency. The “Maintenance of Effort” requirement protected most people enrolled in Medicaid from losing their coverage, even if they no longer qualified. Massachusetts (and all other states) received enhanced federal funding to support the requirement (see p. 26). This helped maintain Massachusetts’ high overall coverage rate during the pandemic. 2024 Prior to the pandemic, MassHealth enrollment was declining slightly, falling 6% from SFY 2015 to 2020, changing from 1.9 million members to just over 1.8 million members. The analysis throughout this report generally uses average enrollment by State Fiscal Year (SFY). The SFY data comes from MassHealth Budget Office. This chart uses a combination of data sources. It uses SFY data from the MassHealth Budget Office for 2013-2022. For 2023, this chart uses point-in-time data from the MassHealth Enrollment Snapshot for June 30, 2023. For 2024, this chart uses the Healey Administration estimated projection of 300,000 losing coverage (Jessica Bartlett, “’It is going to be disruptive.’ MassHealth rolls set to shrink by 300,000, Healey Estimates.” The Boston Globe, March 1, 2023.) OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 12

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH RESUMED ELIGIBILITY REDETERMINATIONS IN APRIL 2023 IN RESPONSE TO THE END OF THE PUBLIC HEALTH EMERGENCY During the COVID-19 public health emergency (PHE), the federal government offered enhanced funding to support states’ Medicaid programs. As a condition of receiving these funds, states were required to provide continuous coverage to members. These federal coverage protections ended on April 1, 2023, and MassHealth is currently redetermining eligibility for all members. This process has the potential to result in coverage loss even for people who should still be eligible, and in response MassHealth has developed a robust strategy to try to minimize coverage disruption. MASSHEALTH’S STRATEGIES FOR REDUCING COVERAGE LOSS To reduce coverage loss among eligible members, MassHealth developed a multi-prong approach, which includes: Taking the full amount of time allowed by the federal government (12 months) to process all pending redeterminations. This spreads out redeterminations to ensure more availability of oneon-one support. Increasing staff to support redetermination efforts, implementing system improvements, and collecting updated contact information to streamline the renewal process. Creating an interactive public dashboard to track changes in member enrollment. Renewing coverage automatically for more members (no paperwork required) by verifying income using existing data sources. HEALTH EQUITY FOCUS Those with limited English proficiency and those with unstable housing are at increased risk of losing coverage during the renewal process. To help reach those at increased risk for coverage loss, MassHealth is partnering with Health Care For All and the Health Connector on the “Your Family. Your Health” campaign. The campaign is a collaboration with community-based organizations in 15 priority communities that have the highest overall populations of MassHealth members. These communities also have high concentrations of immigrants, refugees, and people of color. Strategies include: On-the-ground outreach (canvassing and providing information at local events and community spaces). A multilingual media campaign with messages in nine languages. SOURCES: MassHealth. MassHealth Eligibility Redeterminations(April 2023). MassHealth Redeterminations Resources. Redeterminations Outreach Toolkit: Phase 1. https://www.mass.gov/info-details/masshealth-eligibility-redetermination-outreach-toolkit. Redeterminations Outreach Toolkit: Phase 2. https://www.mass.gov/info-details/redeterminations-outreach-toolkit-phase-2 MassHealth. MassHealth Redetermination Dashboard. https://www.mass.gov/info-details/masshealth-redetermination-dashboard Health Care for All. MassHealth Redetermination Campaign. https://hcfama.org/policy campaigns/redeterminationcampaign/ OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 13

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION CHILDREN, SENIORS, AND PEOPLE WITH DISABILITIES MAKE UP 57% OF MASSHEALTH MEMBERS PERCENT OF TOTAL MASSHEALTH ENROLLMENT (2.17 MILLION), SFY 2022 SENIORS IN COMMUNITY 188,161 1% 9% SENIORS IN NURSING FACILITIES 20,824 NON-DISABLED ADULTS 93610326% 936,103 NON-DISABLED CHILDREN1 719,753 33% 26087290% ADULTS WITH DISABILITIES 260,873 2% MassHealth members range from the very young to the very old. Children comprise 35% of MassHealth members. Adults with disabilities (under age 65) and children with disabilities represent 14% of membership. Nearly one out of 10 MassHealth members is age 65 or over. Most of these seniors also have Medicare coverage, and most live in their communities (not in nursing facilities.) This chart includes MassHealth members (of all ages) who also have coverage through Medicare, an employer-sponsored plan, or student health insurance. In those cases, MassHealth acts as secondary coverage.2 In some circumstances, MassHealth also pays members’ premiums and cost sharing for their employer-sponsored insurance or Medicare coverage. CHILDREN WITH DISABILITIES1 38,794 1 Children defined as under age 21. 2 MassHealth may provide additional or augmented covered services when a member has primary insurance that does not provide coverage for certain needed services. SOURCE: MassHealth Budget Office. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 14

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH IS IMPORTANT TO MANY POPULATION GROUPS PERCENT OF SELECT MASSACHUSETTS POPULATIONS COVERED BY MASSHEALTH Almost half of children in Massachusetts and almost one-third of adults under age 65 are MassHealth members. MassHealth is an especially important source of coverage for people with low incomes and people with disabilities. Almost four in ten births are covered by MassHealth. All children (ages 0–20) 29% All non-elderly adults (ages 21–64) All seniors (ages 65 ) 17% 37% Births (child born in last 12 months) 69% Nursing facility residents 66% People in families earning 133% FPL People with disabilities (broad definition *) 24% 59% People with disabilities (require assistance with self-care) Medicare beneficiaries Two-thirds of people with incomes below 133% of the federal poverty level (about 19,391 annually for a oneperson household in 2023) and more than half of all Massachusetts residents with disabilities who need assistance with self-care (dressing, bathing, or getting around inside the home) receive coverage from MassHealth. Almost seven out of 10 nursing facility residents are MassHealth members. 19% *Deaf or serious difficulty hearing; blind or serious difficulty seeing; cognitive, ambulatory, self-care, or independent living difficulty. SOURCES: Authors’ calculations for “all children,” “all non-elderly adults,” and “all seniors” calculated using the 2017-2021 American Community Survey (ACS) 5-Year Estimates and data from MassHealth Budget Office. “Nursing Facility Residents” calculation uses Nursing facility data from Massachusetts Center for Health Information and Analysis. Baseline Report: Trends in the Massachusetts Nursing Facility Industry 2013–2017 November 2019), accessed at Massachusetts Nursing Facilities (chiamass.gov) OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 15

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH PLAYS A KEY ROLE IN SUPPORTING THE LOW-INCOME WORKFORCE Nearly three quarters of MassHealth members under the age of 65 live in working families. MassHealth provides health insurance coverage to low-income workers across a wide range of industries: SALES (cashiers, retail salespeople, retail supervisors) TRANSPORTATION (movers, drivers, stockers) FOOD SERVICE (fast food workers, cooks, waiters) OFFICE AND ADMINISTRATIVE SUPPORT (customer service representatives, secretaries, receptionists) HEALTH CARE SUPPORT (nursing assistants, personal care aides, home health aides) CLEANING AND MAINTENANCE (janitors, maids, landscapers) CONSTRUCTION (laborers, carpenters, painters) PRODUCTION (butchers, laundry workers, tailors) MANAGERS (managers in sales, retail, operations, food service) PERSONAL CARE AND SERVICES (childcare workers, nail technicians, hairstylists) 0 10 20 30 40 50 60 70 80 90 NUMBER OF WORKERS (THOUSANDS) SOURCES: Kaiser Family Foundation. Distribution of the Nonelderly with Medicaid by Family Work Status, 2021. Accessed at: Distribution of the Nonelderly with Medicaid by Family Work Status KFF. Authors’ industry calculations using the American Community Survey (ACS) 2022 1-Year Public Use Microdata Samples. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 16

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION BENEFITS AND DELIVERY SYSTEMS OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 17

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH PROVIDES COVERAGE SIMILAR TO COMMERCIAL INSURANCE, PLUS SOME ADDITIONAL BENEFITS TYPICAL COMMERCIAL INSURANCE COVERAGE Hospital services Physician services Well child visits Ancillary services (lab tests, radiology, etc.) Prescription drugs Mental health/substance use disorder treatment Vision, hearing, medical equipment ADDITIONAL BENEFITS Long-term services and supports (communityand facility-based)1 Diversionary behavioral health services (to avert hospitalization) Enhanced mental health/substance use disorder treatment 2 Dental services Transportation to medical appointments1 1 LTSS and transportation to medical appointments are available to most but not all MassHealth members. 2 See Massachusetts Division of Insurance, The Catalogue of Carrier Coverage of Inpatient, Outpatient and Community Behavioral Health Services (November 10, 2017), Excel sheet available at https://www.mass.gov/info-details/health-care-access-bureau. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 18

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION LONG-TERM SERVICES AND SUPPORTS THAT KEEP PEOPLE IN THEIR HOMES WHAT IS LTSS AND WHO USES IT Seniors and people with disabilities of all ages can access LTSS. LTSS includes both facility-based services, such as nursing facilities, and home and community-based services (HCBS) such as personal care and in-home supports designed to help people to remain in their homes and communities. Given the complex needs of this population, MassHealth spends more to serve members who need LTSS, on average, than any other group. This is especially true for those who receive facility-based care. BENEFITS OF REMAINING IN THE COMMUNITY Most seniors and people with disabilities greatly prefer remaining in their homes, with support, to institutional long-term care. They are less at risk of infectious disease, are able to maintain independence, and stay more connected with friends and family. In addition, with the high cost of nursing care, it is cost effective to provide the services people need to remain in their home. The tragic toll that the COVID-19 pandemic had on many nursing facilities across the country highlighted the continued importance of strengthening home- and community-based service options. WHAT ARE HOME AND COMMUNITYBASED LTSS MassHealth HCBS is provided through several avenues. Community-based services available to all MassHealth members with disabilities who meet medical necessity criteria include personal care attendants (professionals who assists with performing day-to-day activities) and adult day health (services like supervision, recreation, social activities, meals, and varying levels of medical services provided at a day health facility). Massachusetts also provides services through 10 Home and Community-based Services waivers for specific populations. Examples of HCBS waiver services include residential services, in-home supports such as personal care, home delivered meals, day and employment services, therapies, assistive technology and specialized medical equipment, home and vehicle modifications, and transportation services.1 COSTS OF COMMUNITY BASED LTSS Massachusetts has one of the highest levels of HCBS use among states, as a proportion of its total Medicaid LTSS spending. In 1980, nearly all of Massachusetts’ LTSS spending was for facility-based care. By 2010, about 50% of the spending was for community-based care2 and today, 61% of the spending is for community-based care ( 2 billion out of the 3.4 billion total for Massachusetts’ LTSS spending.)3 1 Medicaid.gov. Massachusetts Waiver Factsheet. (2023). https://www.medicaid.gov/medicaid/section-1115-demo/demonstration-and-waiver-list/Waiver-Descript-Factsheet/MA 2 Blue Cross Blue Shield of Massachusetts Foundation. Massachusetts Medicaid 50th Anniversary Timeline. (2015). https://www.bluecrossmafoundation.org/publications/ma-medicaid-50th#. 3 MassHealth Budget Office OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 19

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH DELIVERY SYSTEM OVERVIEW Originally payment for all Medicaid services was made directly to providers by MassHealth on a fee-for-service (FFS) basis. Over the years, Massachusetts has moved more members to managed care (health care delivery systems organized to manage cost, utilization, and quality) to provide more coordinated and efficient care. Some MassHealth members are required to enroll in a managed care program, some are not eligible for managed care, and others can choose between managed care or the original Medicaid. The chart below provides more details on these different groups and the programs they can choose. Mandatory Managed Care Optional Managed Care These plans all include robust care coordination with a care coordinator assigned to every member. Under 65, no other insurance, living in community Older adult or Disabled, may have Medicare Those with Original FFS other insurance or in Medicaid institutions PCC Plan A primary care clinician coordinates medical care, behavioral health is provided through a managed BH Plan. Medical services are paid FFS. 1 MCOs MCOs are paid a capitated2 rate to provide medical and behavioral health care, through their provider networks. ACOs ACOs are based in provider systems and have enhanced care coordination (see slide 21). PACE A capitated inclusive plan with many services provided at PACE Centers (sites that offer adult day care services, a health clinic, physical and occupational therapy, and common room(s) for social and recreational activities). For people age 55 with clinical need. SCO One Care MassHealth FFS Like an MCO, but includes both Medicaid and Medicare services, including LTSS and dental. For people age 65 . Like a SCO for people with disabilities ages 21–64 Medicare and Medicaid. 3 with No entity is charged with coordinating a member’s care. Most seniors and others with Medicare remain in FFS. Fee-for-service (FFS) payment: A payment made to providers for each service delivered. a capitated rate is a monthly payment per member to cover all services If a member enrolled in One Care turns 65 and is still eligible for One Care, they may elect to stay enrolled in One Care. SOURCES: 130 C.M.R . §450; 130 C.M.R §508. 1 2 3 OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 20

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION AMONG MASSHEALTH MEMBERS WHO ARE ALSO ENROLLED IN MEDICARE, FEWER THAN ONE THIRD ARE ENROLLED IN MANAGED CARE PLANS SFY 2022 MASSHEALTH MEMBERS NOT ENROLLED IN MEDICARE Nearly one in five MassHealth members is also enrolled in Medicare. Most of these members have two insurance cards and must navigate two distinct enrollment processes, provider networks, and sets of covered services. These misalignments can cause confusion, suboptimal care, and poorer health outcomes. 84% 1,825,827 16% 344,339 Massachusetts has developed three managed care options — One Care, PACE, and SCO (see slide 19 for more detail on these option) — to align Medicare and Medicaid services through a single program and provide coordinated care.¹ More than two-thirds of “dual eligible” people remain outside these plans. MASSHEALTH MEMBERS ENROLLED IN MEDICARE BUY IN 10% 1% FEE-FOR-SERVICE 61% (EXCLUDING BUY IN) 209,049 19% 9% 34,050 PACE 4,603 SCO 64,463 ONE CARE32,173 1 Massachusetts Executive Office of Health and Human Services. (2023). One Care Homepage. 2 Massachusetts Executive Office of Health and Human Services. (2023). One Care Transition Planning. NOTES: The bottom pie chart only shows members who are enrolled in Medicare and Medicaid. In addition, there are SCO and PACE enrollees who are not enrolled in both MassHealth and Medicare. The MassHealth buy-in covers Medicare premiums, co-pays, and deductibles, but does not cover other MassHealth Standard services. Eligibility for the buy-in program was expanded in January 2020, increasing buy-in enrollment SOURCE: MassHealth Budget Office. OCTOBER 2023 One Care is planning for change. The federal government has updated the rules under which the program operates, effective in 2026. MassHealth is engaging with stakeholders to ensure the required updates will maintain a program with robust service coordination and a consumer focus.² MASSACHUSETTS MEDICAID POLICY INSTITUTE 21

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION AMONG ALL MASSHEALTH MEMBERS, 69% WERE ENROLLED IN MANAGED CARE IN SFY 2022, WITH OVER HALF OF ALL MEMBERS IN ACOs MASSHEALTH ENROLLMENT BY PAYER TYPE, SFY 2022 Most MassHealth Members are enrolled in some form of managed care, with more than half of members enrolled in an ACO. See Slide 19 for program descriptions. ACCOUNTABLE CARE PARTNERSHIP PLAN 676,662 31% ACOs 21% PRIMARY CARE ACO 460,907 MANAGED CARE NONMANAGED CARE FFS, PREMIUM ASSISTANCE, AND LIMITED1 673,795 1 5% 31% 6% 3 % MCOs 112,876 1% ONE CARE 32,209 SCO AND PACESCO: 69,988 PACE:4,902 PCC PLAN133,168 Premium assistance includes premium subsidies from MassHealth for employer-sponsored health insurance. MassHealth Limited provides coverage for emergency medical services for about 243,822 noncitizens (for SFY 2022). SOURCE: MassHealth Budget Office. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 22

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH ACCOUNTABLE CARE ORGANIZATIONS (ACOS) ACCOUNTABLE CARE PARTNERSHIP PLAN PRIMARY CARE ACO Contract between MassHealth and Accountable Care Partnership Plan Capitation payment Contract between MassHealth and ACO Shared savings and losses 15 ACOs SELECTED BY THE STATE STATE 350,000 MEMBERS 880,000 MEMBERS ENROLLED 2 ACOs SELECTED BY THE ENROLLED 1 1 With the selection of new ACOs in April 2023, an estimated 525,000 members joined one of the new ACO plans.2 ACO enrollment has shifted from SFY 2022 (slide 21) to 2023 because there are two more Accountable Care Partnership Plans and one less Primary Care ACO than in SFY 2022. Members are assigned to ACOs based on the affiliation of their primary care provider. These numbers represent estimates as of April 2023 1 2 MassHealth presentation on ACO Relaunch for Advocates Meeting Presentation, February 2023 SOURCES: Massachusetts Health Policy Commission. February 2023. Care Delivery Transformation meeting presentation. Available from: https://www.mass.gov/doc/presentation-02152023-cdt-meeting Executive Office of Health and Human Services. March 2023. All Provider Bulletin 363. Available from: https://www.mass.gov/doc/all-provider-bulletin-363-accountable-care-organization-program-updates-0 OCTOBER 2023 Accountable Care Organizations (ACOs) are organized groups of doctors, hospitals and other health care providers held accountable for their member populations’ health and health care costs. There are two types of MassHealth ACOs, with different payment and contracting structures. For members enrolled in Accountable Care Partnership Plans, MassHealth makes capitation payments (a set amount per member per month.) Accountable Care Partnership Plans must use these payments to pay for comprehensive health services, including both physical and behavioral health, for their enrollees. For Primary Care ACOs MassHealth pays providers directly for most services. These costs are then compared to a spending target, and the ACO and MassHealth share in any savings or losses. MassHealth recently selected a new set of ACOs for a new five-year contract beginning April 1, 2023. The new lineup resulted in many members changing ACOs (most commonly because their primary care provider’s ACO affiliation changed.) Beginning in 2023, all ACOs will pay primary care providers via capitation rather than fee-for-service, to allow more flexibility and innovation in primary care. MASSACHUSETTS MEDICAID POLICY INSTITUTE 23

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH COMMUNITY PARTNERS (CP) ACCOUNTABLE CARE PARTNERSHIP PLAN PRIMARY CARE ACO MCO Behavioral Health Community Partners and Long Term Services and Supports Community Partners Agreements between ACOs/MCOs and Community Partners Per Member Per Month payment ACOs and MCOs pay CPs directly 12 BH CPs SELECTED BY THE 8 LTSS CPs SELECTED BY THE STATE STATE 31,000 TOTAL MEMBERS 10,500 TOTAL MEMBERS ENROLLED ENROLLED SOURCES: MassHealth. Payment and Care Delivery Innovation (PCDI) Initiative for Providers. Available: https://www.mass.gov/payment-care-delivery-innovation-pcdi-for-providers Massachusetts Health Policy Commission. February 2023. Care Delivery Transformation meeting presentation. Available from: https://www.mass.gov/doc/presentation-02152023-cdt-meeting OCTOBER 2023 MassHealth’s focus on accountable care includes an increased focus on care coordination for its most complex members. Each ACO and MCO contracts with community organizations to be MassHealth Community Partners (CPs). CPs work with members with serious mental illness and addiction (Behavioral Health CPs), and adults and children with physical and developmental disabilities and brain injuries (Long-Term Services and Supports CPs). CPs promote the integration of care through outreach and engagement, person-centered treatment planning, service coordination, health and wellness coaching, and facilitation of access to social and community-based supports. For a member involved with multiple health care providers, which members with complex needs frequently are, the CP is the lead care coordinator. A lead care coordinator ensures that all providers’ care plans are in alignment. MassHealth recently selected a new lineup of CPs for a new five-year contract, beginning April 1, 2023. There are now 20 CPs providing services to ACO and MCO members, down from 27 previously. MASSACHUSETTS MEDICAID POLICY INSTITUTE 24

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION FLEXIBLE SERVICES PROGRAM (FSP) ACCOUNTABLE CARE PARTNERSHIP PLAN PRIMARY CARE ACO MCO MCOs do not currently include Flexible Services Social Service Organizations Partnerships between ACOs and Social Service Organizations to provide FSP 82 FSPs APPROVED BY THE STATE 2 ALL ACOs HAVE AN APPROVED FSP 41 NUTRITION FSPs SINCE 2020, MORE THAN 20,000 ACO MEMBERS HAVE RECEIVED 40 HOUSING FSPs APPROXIMATELY 50 MILLION IN 1 JOINT NUTRITION/HOUSING FSPs HOUSING OR NUTRITION SUPPORTS MassHealth Health Plan Contracts. ACPP Model Contract section 2.22 and PCACO Model Contract section 2.13. (2023). https://www.mass.gov/masshealth-health-plan-contracts 1 SOURCES: Massachusetts Health Policy Commission. February 2023. Care Delivery Transformation meeting presentation. Available from: https://www.mass.gov/doc/presentation-02152023-cdt-meeting OCTOBER 2023 The Flexible Services Program (FSP), launched in 2020, provides some ACO members with services not typically covered by MassHealth. FSP addresses members’ health-related social needs (HRSN) by providing nutrition and housing supports, aimed to improve members’ health and potentially reducing an ACO’s total cost of care. Examples of housing supports include housing application assistance, and home modifications like air conditioners or grab bars in showers. Examples of nutrition assistance are medically-tailored and home-delivered meals and food vouchers. ACOs can partner with social service organizations to provide these services, or they can provide the services directly to their members. A member may be eligible for FSP if they have 1) behavioral or complex physical health needs and 2) housingor nutrition-related risk factors. Each ACO further defines the eligibility for their FSP programs. As of April 2023, MassHealth requires ACOs to offer at least one nutrition and one housing program. In addition, they must provide FSP services to a minimum numbers of members. 1 MASSACHUSETTS MEDICAID POLICY INSTITUTE 25

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION SPENDING AND COST DRIVERS OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 26

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION NEARLY EVERY DOLLAR IN MASSHEALTH SPENDING IS REIMBURSED BY AT LEAST 50 CENTS IN FEDERAL REVENUE TO THE STATE FEDERAL AND STATE SHARES OF MASSHEALTH EXPENDITURES, TYPICAL LEVELS CHIP ACA EXPANSION POPULATION MOST OTHER MASSHEALTH SERVICE EXPENDITURES Federal funds pay Federal funds pay Federal funds pay 65% 90% 50% of CHIP expenditures. of Medicaid expansion expenditures. of most other MassHealth service expenditures. 1 FEDERAL FUNDS STATE FUNDS Centers for Medicare and Medicaid Services. CMS Waivers, Flexibilities, and the Transition Forward from the COVID-19 Public Health Emergency. (February 2023). https ://www.cms.gov/newsroom/fact-sheets/cms-waivers-flexibilities-and-transition-forward-covid-19-public-health-emergency The federal government reimburses Massachusetts for a portion of MassHealth spending. During the pandemic, the federal government increased Medicaid expenditure reimbursements by 6.2 percentage points, and CHIP expenditure reimbursements by 4.3 percentage points. With the end of the public health emergency, this enhanced federal reimbursement is being phased out between April and December of 2023. By January 1, 2024, the federal reimbursement levels will have returned to the typical levels shown in the chart.1 The CHIP federal matching assistance percentage was 69.34% in SFY22 and is returning to 65%. The federal match for the Affordable Care Act (ACA) expansion population is 90%, which did not increase during the public health emergency. Most other MassHealth service expenditures had their federal match increased to 56.2% during the public health emergency, and this is returning to 50%. SOURCES: Kaiser Family Foundation. State Health Facts, Enhanced Federal Medical Assistance Percentage (FMAP) for CHIP. Kaiser Family Foundation. State Health Facts, Federal Medical Assistance Percentage (FMAP) for Medicaid and Multiplier. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 27

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION THE MAIN SOURCE OF FEDERAL REVENUES TO MASSACHUSETTS IS MASSHEALTH MASSACHUSETTS STATE BUDGET ( 53.9 BILLION), SFY 2022 STATE PORTION 39.8B 74% Federal revenues supply about one-quarter of the funding for the state budget, and about 89% of that revenue is generated by Medicaid, CHIP, and ConnectorCare expenditures. Approximately 12.5 billion, or 89%, of all federal revenue 14.1B in SFY22 budget 26% is generated by Medicaid/CHIP/ ConnectorCare FEDERAL REVENUE NOTE: Medicaid in this context includes MassHealth, Commonwealth Care (prior to 2014), and ConnectorCare premium and cost-sharing subsidies (post-2014); additional MassHealth 1115 waiver spending; and spending on some programs and facilities that serve people eligible for MassHealth and are administered by the Departments of Developmental Services, Mental Health, and Public Health, and the Massachusetts Rehabilitation Commission. SOURCE: Massachusetts Budget and Policy Center. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 28

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH ACCOUNTS FOR APPROXIMATELY 22% OF THE STATE BUDGET, NET OF FEDERAL REVENUES MASSACHUSETTS TOTAL STATE SPENDING NET OF FEDERAL REVENUES ( 39 BILLION), SFY 2022 Massachusetts’s SFY 2022 budget was approximately 53.9 billion, of which about onequarter was supplied by federal revenues. Medicaid/CHIP/ConnectorCare spending generated the vast majority (89%) of those federal revenues (see slide 27). To understand the true cost of MassHealth to the state, it is instructive to look at the expected state spending net of those federal revenues; this net state budget totaled 39 billion in SFY 2022. The state’s share of MassHealth costs is approximately 22% ( 8.5 billion) of the state budget net of federal revenues. 8.5B 22% OTHER 30.5B (non-MassHealth budget items) 78% SOURCES: Massachusetts Budget and Policy Center (2022). What is the Actual State Cost of MassHealth in State Fiscal Year 2022? Blue Cross Blue Shield of Massachusetts Foundation. See also: Massachusetts Budget and Policy Center (2019). What is the Actual State Cost of MassHealth in 2019? Blue Cross Blue Shield of Massachusetts Foundation. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 29

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION TOTAL MASSHEALTH SPENDING HAS RISEN SINCE THE BEGINNING OF THE PANDEMIC, DRIVEN LARGELY BY ENROLLMENT MASSHEALTH TOTAL PROGRAMMATIC SPENDING, SFY 2013–2022 21 (BILLIONS OF DOLLARS) 19 18.1 18 16.5 17 14.6 15 13 10 15.0 15.2 13.5 14 11 17.0 15.8 16 12 19.9 CURRENT DOLLARS 20 11.9 10.8 13.0 13.5 13.8 14.2 14.3 15.9 14.2 INFLATION-ADJUSTED DOLLARS2 11.8 10.8 9 8 7 6 5 SFY 2013 2014 2015 2016 2017 2018 2019 2020 2021 2022 NOTE: This analysis reflects gross spending amounts, which includes both state and federal shares. The spending amounts include claim and capitation payments for medical benefits provided by MassHealth, and do not include the cost of Medicare or commercial premiums, Medicaid-reimbursable services from other state agencies, administrative spending, or risk corridor payments to managed care plans, or supplemental payments to providers. Note that this slide contains actual programmatic spending data while the previous slide contains budgeted state spending net of federal revenues. 1 Medical cost inflation is based on the consumer price index specifically for medical care. 2 Inflation adjustment uses the Medical Consumer Price Index for the Boston area, from the U.S. Bureau of Labor Statistics. 3 Massachusetts Budget and Policy Center (2022) What is the Actual State Cost of MassHealth in 2022? Blue Cross Blue Shield of Massachusetts Foundation SOURCES: MassHealth Budget Office and authors’ calculations. OCTOBER 2023 Total MassHealth program spending has nearly doubled in 10 years, from 10.8 billion in SFY 2013 to 19.85 billion in SFY 2022. When adjusted for medical cost inflation,1 the average annual increase from SFY 2013 to SFY 2022 was less than 4.5%. The average inflation-adjusted increase was particularly low in the years between SFY 2016 and SFY 2020, with growth averaging 2%. Since the start of the pandemic in 2020 inflation-adjusted spending has increased, by 6.8% in SFY 2021 and 4.2% in SFY 2022. This growth was largely driven by increases in enrollment related to the COVID-19 Public Health Emergency (see slide 12). With the resumption of eligibility redeterminations in April 2023, it is expected that spending growth will slow in SFY 2024, in line with projected enrollment changes. The increased spending in SFY 2021 and SFY 2022 was offset by the enhanced federal match during the pandemic, reducing the impact on the state budget.3 Prior to the COVID-19 pandemic, the most significant annual increases in spending occurred from SFY 2013 to SFY 2015. Most of that growth is attributable to enrollment increases resulting from the ACA expansion. MASSACHUSETTS MEDICAID POLICY INSTITUTE 30

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION WHILE ENROLLMENT AND OVERALL PROGRAM SPENDING INCREASED DURING SFY 2021-2022, SPENDING PER MEMBER REMAINED STEADY GROWTH IN MASSHEALTH TOTAL SPENDING, ENROLLMENT, AND PER MEMBER PER MONTH (PMPM) COSTS1 AS COMPARED TO SFY 2013 (SFY 2013 100%) 200% (PERCENTAGE OF 2013 LEVEL) TOTAL SPENDING 180% 160% ENROLLMENT 140% 120% 100% 80% 2014 2015 2016 2017 2018 2019 2020 2021 2022 1 This PMPM drop was a result of temporary Medicaid coverage that was initiated in 2014 at the start of the ACA expansion. The temporary members caused some of the spike in enrollment, as well as the declining PMPM, as these members used fewer health care services. 2 Blue Cross Blue Shield of Massachusetts Foundation. (2021). SFY2021 Budget for MassHealth and Other Health Reform Programs. SOURCES: MassHealth Budget Office (total date of service spending and enrollment) and authors’ calculations. OCTOBER 2023 Since SFY 2013, PMPM spending increased 19%, with a dip from SFY 2013 to 20151, and a rapid increase between SFY 2017 and 2020. PMPM spending is determined by two factors: rates paid to providers and utilization of services by members. The increase in PMPM spending from SFY 2017 to 2020 is largely driven by provider and capitation rate increases during this time frame. PMPM SPENDING SFY 2013 Total MassHealth spending typically tracks with enrollment - when enrollment increases (such as during the pandemic or when the ACA expanded eligibility for the program), spending typically increases at a faster than average rate. From SFY 2021 to 2022, member enrollment increased by 9.8%, driving the increase in total spending, while spending per member (PMPM) was unchanged. PMPM spending leveled off during the pandemic, from SFY 2020 to 2022, coincident with rapid enrollment growth. This is because most of this enrollment growth occurred among non-disabled children and adults, whose relatively low service utilization had little effect on overall per member spending. MASSACHUSETTS MEDICAID POLICY INSTITUTE 31

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MOST MASSHEALTH DOLLARS ARE SPENT ON SERVICES FOR A MINORITY OF MEMBERS DISTRIBUTION OF MASSHEALTH ENROLLMENT AND SPENDING BY VARIOUS POPULATIONS, SFY 2022 100% 10% 90% 14% 80% 23% SENIORS 32% ADULTS AND CHILDREN WITH DISABILITIES 31% NON-DISABLED ADULTS 15% NON-DISABLED CHILDREN MassHealth spending is not spread evenly across the various categories of members. More than half (55%) of spending in SFY 2022 was for services to people with disabilities and seniors. These groups make up only a quarter (24%) of the MassHealth membership. 70% 60% 43% 50% 40% 30% 20% 33% 10% 0% Enrollment Spending SOURCE: MassHealth Budget Office. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 32

ELIGIBILITY AND ENROLLMENT INTRODUCTION BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION TRENDS IN MASSHEALTH SPENDING PER MEMBER VARIED ACROSS SUB-GROUPS IN RECENT YEARS MASSHEALTH PAYMENTS PER MEMBER PER YEAR, SFY 2020-2022 21,000 0 Total (All Members) Non-Disabled Children Non-Disabled Adults Adults with Disabilities Seniors 18,878 18,257 18,254 Children with Disabilities SOURCE: Calculations based on total spending and member months from the MassHealth Budget Office. Based on date of service spending. Excludes spending and enrollment for the Temporary Medicaid category. OCTOBER 2023 16,650 5,861 5,819 5,564 3,541 3,337 3,210 8,081 7,877 7,000 8,081 14,000 16,481 16,993 17,038 SFY 2022 18,558 SFY 2021 19,704 SFY 2020 Over a three-year period from SFY 2020 to SFY 2022 per member spending, unadjusted for inflation, remained flat for the MassHealth population as a whole. Per member spending over this period, however, increased for all population groups except seniors. These increases can be explained by several factors: 1) a significant increase in capitation rates paid by MassHealth beginning midway through SFY 2020; 2) significant workforce investments in services utilized by people with disabilities and seniors; and 3) rebounding utilization in SFY 2022, following a drop during the early phase of the COVID-19 pandemic. Per member spending for seniors declined 7% from SFY 2020 to 2021, owing in large part to a reduction in service utilization early in the pandemic. The spending per member for seniors increased in SFY 2022 as utilization recovered, resulting in a net 4% reduction over the three-year period. MASSACHUSETTS MEDICAID POLICY INSTITUTE 33

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION OVER HALF OF MASSHEALTH SPENDING IN SFY 2022 WAS ON CAPITATION PAYMENTS TOTAL MASSHEALTH SPENDING 17.54 BILLION, SFY 2022 CAPITATION PAYMENTS, including payments to Accountable Care Partnership plans; Primary Care ACOs’ administrative payments 1 MCOs; SCO plans; One Care plans; PACE organizations; and The PCC plan’s behavioral health carve-out vendor OTHER PAYMENTS 9.23B 8.31B including PCC plan payments; Primary Care ACO payments; and Fee-for-service payments MassHealth spent 17.54 billion 2 on services for its members in SFY 2022. Over half of that spending ( 9.23 billion) was capitation payments to ACOs, MCOs, the PCC plan’s behavioral health carve-out vendor, SCO plans, One Care plans, and PACE providers. With the focus on accountable, integrated, and coordinated care, an increasing portion of MassHealth enrollees are members of an ACO and other types of managed care. In SFY 2022, approximately 69% of MassHealth members were enrolled in one of these managed care arrangements. For members enrolled in ACOs and MCOs, some services are paid for under fee-for-service arrangements, including the majority of LTSS provided to managed care members. As a result, forty-two percent of all MassHealth feefor-service payments went to Community and Institutional LTSS (data not shown in chart.)³ 1 Primary Care ACO administrative payments are made on a per enrollee, per month basis. Primary Care ACOs are primarily paid on a shared savings / shared loss model that is not considered to be a capitated payment. 2 This total does not include spending on Medicare premiums. The figures also do not include Medicaid-reimbursable services from other state agencies, administrative spending, or supplemental payments to hospitals. 3 MassHealth Budget Office. SOURCE: MassHealth Budget Office. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 34

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH SPENDING IS IMPORTANT TO MANY TYPES OF PROVIDERS MASSHEALTH REVENUE AS A PERCENTAGE OF PROVIDERS’ TOTAL PATIENT REVENUES NURSING FACILITIES (2019) MassHealth represents a significant portion of health care providers’ revenues. This is especially the case for nursing facilities, community LTSS providers, and community health centers, which on average receive more than forty-five percent of their total patient revenues from MassHealth. COMMUNITY HEALTH CENTERS (2021) 54% 45% LTSS1 (2020) PRENATAL CARE2 (2019) HOSPITALS (2021) 46% 38% 17% MassHealth covers the prenatal care for more than a third of all births in Massachusetts. Prenatal care is delivered by a mix of providers. MassHealth dollars Includes spending for private sector establishments primarily engaged in providing skilled nursing services in the home along with a range of the following: personal care services; homemaker and companion services; physical therapy; medical social services; medications; medical equipment and supplies; counseling; 24-hour home care; occupation and vocational therapy; dietary and nutritional services; speech therapy; audiology; and high-tech care, such as intravenous therapy. 2 Percentage of births whose prenatal care was paid for by MassHealth SOURCES: Center for Health Information and Analysis (CHIA) (2021), Massachusetts Hospital Profiles (SFY 2021 data); CHIA Cost Reports (Nursing Facilities — Calendar Year 2019); Health Resources and Services Administration, Bureau of Primary Health Care, Uniform Data System Report (CHCs — federal FY 2021 data) (limited to HRSA-funded CHCs); CMS National and State Health Expenditure Accounts (LTSS); MA DPH; Massachusetts Births 2019, Table 1. Trends in Birth Characteristics. 1 OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 35

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION REFORMS OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 36

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSACHUSETTS ADMINISTERS MOST OF MASSHEALTH THROUGH WAIVERS WHAT IS A STATE Medicaid state plans reflect an agreement between a state and the federal government PLAN? regarding how the state Medicaid program will operate. Amendments to Medicaid state plans are frequent and may be large or small. WHAT IS A WAIVER? States may request approval from the federal government to waive certain parts of federal Medicaid law to test program innovations or gain more flexibility than state plans allow in how they deliver and pay for Medicaid services. An important condition of 1115 demonstration waivers is that they be “budget neutral,” meaning the federal government will contribute no more to a waiver program than it would to a Medicaid program operating under standard rules. MASSHEALTH’S 1115 DEMONSTRATIO N WAIVER MassHealth operates under the authority of an 1115 demonstration waiver for almost all members. The waiver took effect in 1997 and has evolved through seven extensions to expand coverage, support the safety net, and provide incentives for delivery system innovations. In the 2017-2022 extension, MassHealth introduced Accountable Care Organizations (ACOs) and new models of addressing member needs using Community Partners and flexible services. The latest extension, approved in September 2022 and effective through December 31, 2027, builds on past demonstrations and adds a sharper focus on health equity (see slide 37 for more information). MassHealth has other waivers to permit the state to provide LTSS in a home or HOMEAND community setting to members whose disabilities qualify them for an institutional level COMMUNITYof care. See slide 18 for more details. BASED SERVICES WAIVERS SOURCES: 130 C.M.R. §519.007; 1915(c) waiver approval documents; Gershon, R. (2019) Deciphering State Medicaid Programs. ForHealth Consulting Publications. 1115 MassHealth Demonstration ("Waiver") Approval. OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 37

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION LATEST EXTENSION OF MASSHEALTH’S 1115 DEMONSTRATION WAIVER ADVANCES REFORMS, FOCUSES ON EQUITY On September 28, 2022, CMS approved Massachusetts’ request for a five-year extension of its MassHealth Section 1115 Demonstration waiver. This new waiver will be in effect from October 1, 2022 through December 31, 2027, and includes features that: Continue and build on the ACO, Community Partners (CP), and Flexible Services (FSP) programs. IMPROVE Enhance care coordination and support members’ health-related social needs (HRSN). DELIVERY SYSTEM REFORMS UPDATE ELIGIBILITY POLICIES Extend CommonHealth eligibility (for people with disabilities) to maintain coverage for older adults and people with unsteady or less than full-time employment. Make coverage retroactive to three months prior to application for pregnant people and children Guarantee continuous coverage for people experiencing homelessness (for 24 months) and for people transitioning from incarceration back to the community (12 months). ADVANCE HEALTH EQUITY Address HRSN for people experiencing homelessness, transitioning from incarceration to the community, or at risk of eviction because of a disability caused by substance use disorder or mental illness. Expand FSP to include household-level nutrition supports if qualifying member is a child or pregnant person. Introduce payment incentives for hospitals to collect social risk factor data, to implement interventions that improve quality and reduce inequities, and to improve workforce capacity and collaborations to reduce inequities. INVEST IN PRIMARY CARE AND BEHAVIORAL HEALTH Implement a value-based capitation payment for ACO-affiliated primary care practices, to provide practices with flexibility and promote care coordination and integration of behavioral health care. Make workforce investments, including loan repayment programs for primary care and behavioral health providers and a family nurse practitioner residency program in community health centers. Continue the Safety Net Care Pool, a key source of funding for hospitals and other facilities that CONTINUE TO treat populations with limited access to care. SUPPORT SAFETY SOURCES: Massachusetts Executive Office of Health and Human Services. (2023). 1115 MassHealth Demonstration ("Waiver"). https://www.mass.gov/service-details/1115-masshealth-demonstration-waiver. NET CARE Cross Blue Shield of Massachusetts Foundation. (2023). The MassHealth Demonstration Extension 2022–2027: Building on Success, Focusing on Equity. HOSPITALS https://www.bluecrossmafoundation.org/publication/masshealth-demonstration-extension-2022-2027-building-success-focusing-equity. OCTOBER 2023 Blue MASSACHUSETTS MEDICAID POLICY INSTITUTE 38

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH HAS PROPOSED ADDITIONAL COVERAGE AND SERVICE EXPANSIONS On October 16, 2023, MassHealth proposed a waiver amendment to CMS to advance health equity by expanding coverage and further addressing members’ health-related social needs. The proposed waiver includes the following provisions: MASSHEALTH SERVICES FOR PEOPLE WHO ARE INCARCERATED Federal law generally prohibits states from using federal Medicaid dollars to cover people who are incarcerated in jails or prisons or residing in public institutions. To address health inequities experienced by justice-involved populations, MassHealth has requested to cover certain MassHealth services for 90 days before release for all Medicaid-eligible people in County Correctional Facilities and state Department of Corrections facilities and for Medicaid-eligible youth committed to the care and custody of the state Department of Youth Services. COVERAGE CONTINUITY FOR ADDITIONAL MASSHEALTH MEMBERS Under MassHealth’s proposed waiver amendment, once an adult (age 21 , inclusive of seniors) is established eligible for MassHealth, their eligibility would stay in place for 12 months, regardless of changes in circumstances that may occur in the interim. This policy makes retention of eligibility easier by reducing the chance of disenrollment because of a failure to comply with an administrative request. Federal law already requires all states to implement 12-month continuous eligibility for children beginning in 2024, and members who are experiencing homelessness are already provided 24-months of continuous eligibility in MassHealth. COVERAGE THAT EXTENDS BACKWARDS IN TIME, PRIOR TO APPLICATION DATE Federal law requires states to extend most Medicaid coverage backwards in time, to three months prior to the application date. However, for many years MassHealth has had a waiver to limit retroactive eligibility to ten days. As part of its most recent waiver renewal, Massachusetts eliminated the waiver of retroactive eligibility for pregnant people and children, thus extending eligibility for these members to three months prior to the date of application if they would have met eligibility requirements during that period. Under MassHealth’s proposed waiver amendment, MassHealth would restore 3-month retroactivity for everyone on MassHealth – not just pregnant people and children. COVERAGE FOR POSTHOSPITALIZATION HOUSING To ensure that MassHealth members experiencing homelessness are discharged from hospitals to a safe space, MassHealth’s proposed waiver amendment would cover up to six months of Short-Term PostHospitalization Housing (or STPHH, also known as medical respite) for certain MassHealth members who meet certain risk-based and clinical criteria. STPHH would also include medical services such as monitoring of vital signs, assessments, wound care, medication monitoring and reminders, and 24-hour on-call medical support. SOURCE: Massachusetts Executive Office of Health and Human Services. (2023). Amendment Request of 1115 MassHealth Demonstration ("Waiver"). https://www.mass.gov/doc/masshealth-section-1115-demonstration-amendment-request-2/download OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 39

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION MASSHEALTH HAS ENHANCED ITS BEHAVIORAL HEALTH BENEFITS As the Commonwealth institutes broad reforms to the behavioral health system through the “Roadmap for Behavioral Health Reform,” MassHealth plays a central role. MassHealth’s coverage of new services and providers are important components of the state’s overall efforts to improve access to timely behavioral health care. COMMUNITY BEHAVIORAL HEALTH CENTERS (CBHC) CBHCs are a new type of provider, with integrated mental health and substance use care, available on a same day basis for urgent needs or for ongoing care using evidence-based practices. They provide Mobile Crisis Intervention for both adults and children in the community, which is designed to reduce the reliance on emergency departments for behavioral health crises. MassHealth reimburses CBHCs using bundled service payments, and more robust payments support previously non-reimbursable services such as care coordination. EXPANDED PROVIDER TYPES IN FFS PROGRAM Massachusetts updated provider regulations to add coverage for Licensed Independent Social Workers in the FFS system, previously only covered in managed care. MassHealth expanded its scope of service regulations for psychologists to include psychotherapy. MassHealth added Community Support Programs1 services, to the FFS system, as well as Certified Peer Specialists, services, Recovery Coaches, and Recovery Support Navigators.2 BEHAVIORAL HEALTH URGENT CARE MassHealth offers higher rates of payment to mental health centers that can provide access to urgent behavioral health care on the same or next day, to incentivize them to build this capacity into their clinics. MASSHEALTH ROLE IN BROADER REFORMS MassHealth’s creation of the CBHCs has provided the infrastructure in which to offer these services, especially urgent care, which CBHCs are required to provide to any Massachusetts resident in crisis.3 The MassHealth 1115 demonstration waiver includes loan forgiveness programs for behavioral health clinicians, an important element of efforts to expand the behavioral health workforce. CSP provides an array of services that can help a member live in the community, such as service planning and coordination, assisting with obtaining benefits, or helping members their activities of daily living. Certified Peer Specialists are people with lived experience of a mental health disorder trained to mentor a member experiencing a mental health disorder. Recovery Coaches are people with lived experience of substance use disorders and recovery trained to help peers explore recovery. Recovery Support Navigators are paraprofessionals, who provide care coordination, case management and motivational support. 3 Mass.gov. Community Behavioral Health Centers. (2023). https://www.mass.gov/community-behavioral-health-centers Sources: MassHealth provider regulations, 130 CMR 448 Community Behavioral Health Centers, Services 130 CMR 462 Licensed Independent Clinical Social Worker Services, 130 CMR 429 Mental Health Center Services, 130 CMR 411 Psychologist Services, 101 CMR 305: Rates for Behavioral Health Services Provided in Community Behavioral Health Centers; 130 CMR 461.000: Community Support Program Services. MassHealth Managed Care Entity Bulletin 76, December 2021 https://www.mass.gov/doc/managed-care-entity-bulletin-76-behavioral-health-urgent-care-providers/download 1 2 OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 40

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION CONCLUSION OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE 41

INTRODUCTION ELIGIBILITY AND ENROLLMENT BENEFITS AND DELIVERY SYSTEMS SPENDING AND COST DRIVERS REFORMS CONCLUSION LOOKING TO THE FUTURE OF MASSHEALTH COVERAGE Federal policy protected most Medicaid members from being disenrolled during the COVID-19 pandemic. MassHealth resumed eligibility redeterminations on April 1, 2023, a process expected to decrease enrollment in MassHealth. MassHealth is working to minimize the risk of coverage loss for eligible members. EQUITY MassHealth is making several policy changes to improve health equity, including creating financial incentives for hospitals to measure and reduce health inequities and broadening its focus on health-related social needs. OCTOBER 2023 SAFETY NET MassHealth continues to be a cornerstone of a system that provides near-universal coverage, and it provides support to hospitals that care for a disproportionate share of MassHealth members and patients without insurance. INNOVATION MassHealth is implementing health policy reforms that invest in primary care and behavioral health and that stabilize eligibility for members for whom access to care is crucial and often interrupted. MASSACHUSETTS MEDICAID POLICY INSTITUTE 42

OCTOBER 2023 MASSACHUSETTS MEDICAID POLICY INSTITUTE